Capsule and Ligaments of Talocrural Joint RIMT University



- Slides: 20
Capsule and Ligaments of Talocrural Joint RIMT University Department of Physiotherapy Prepared by: Dr. Navkaran Singh
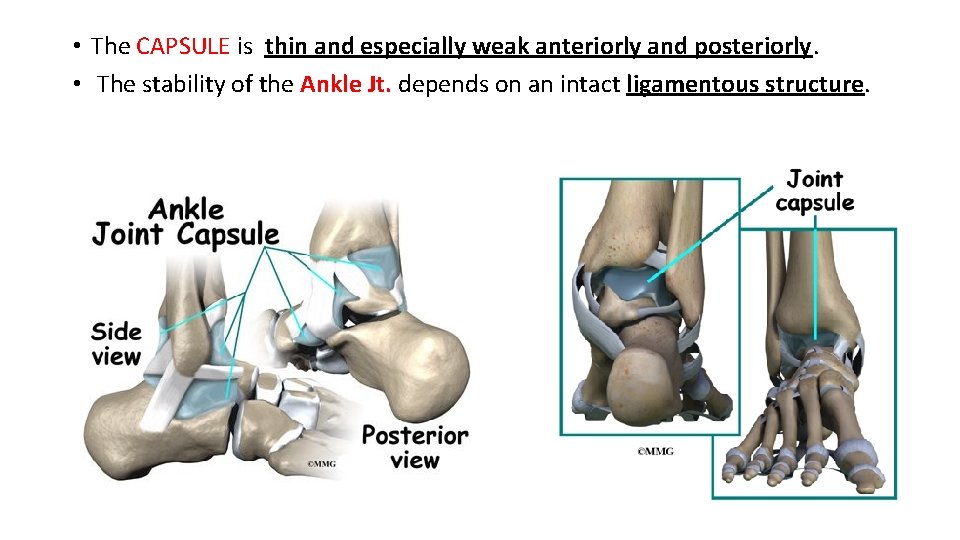
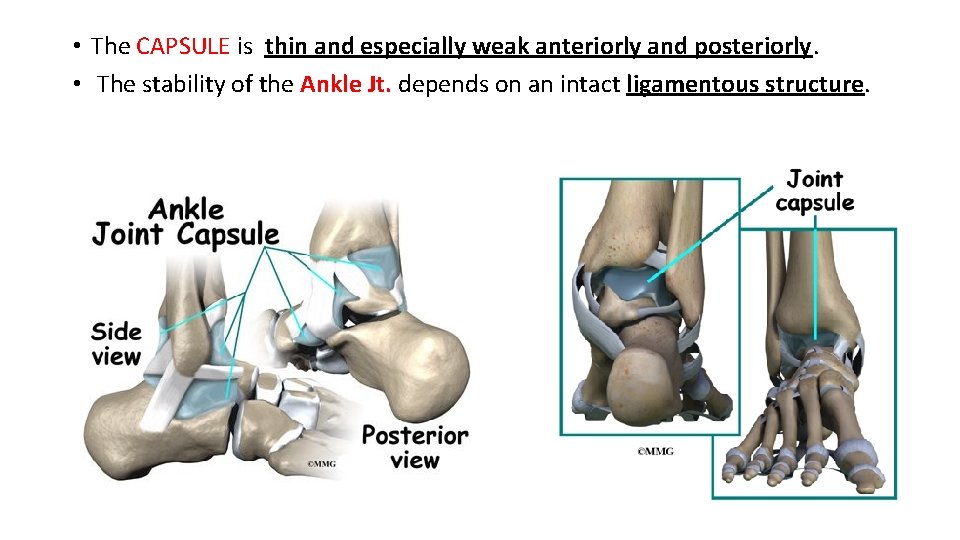
• The CAPSULE is thin and especially weak anteriorly and posteriorly. • The stability of the Ankle Jt. depends on an intact ligamentous structure.
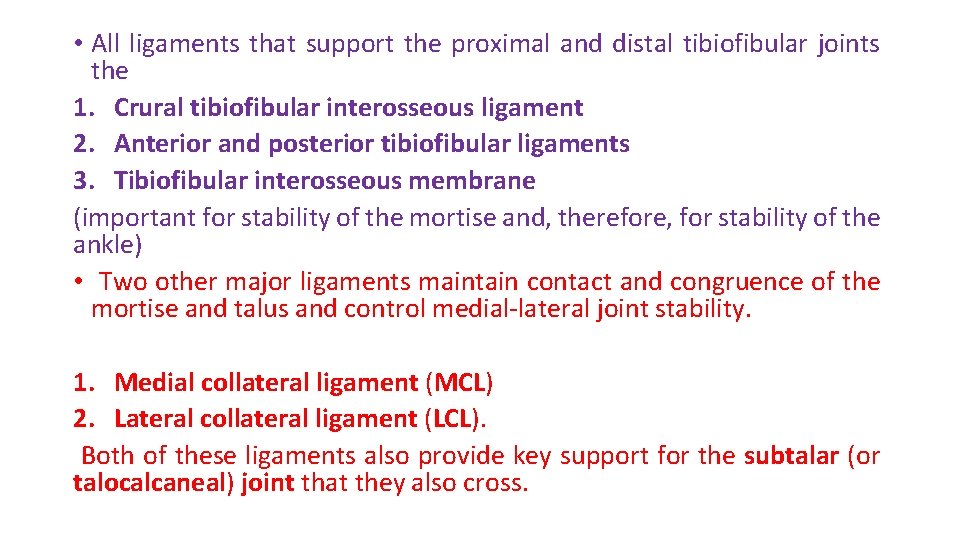
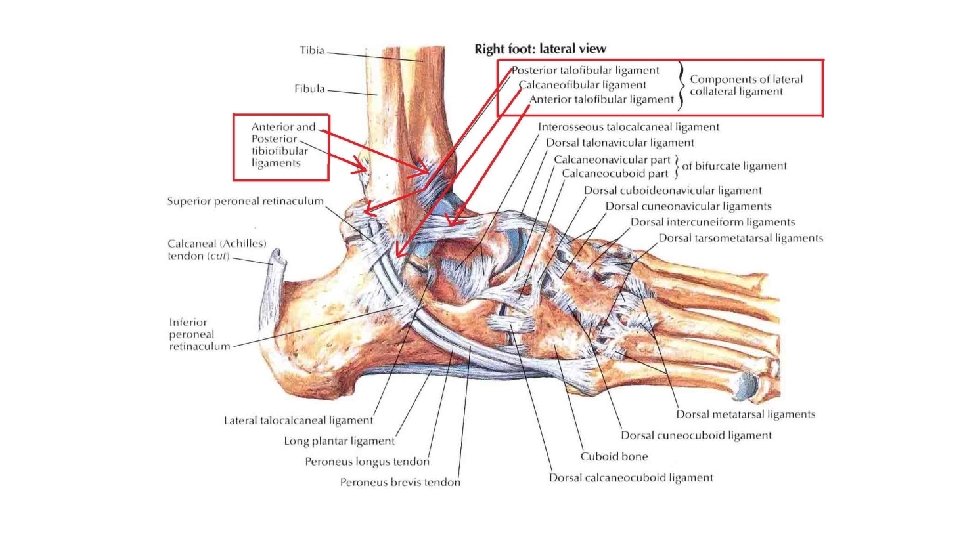
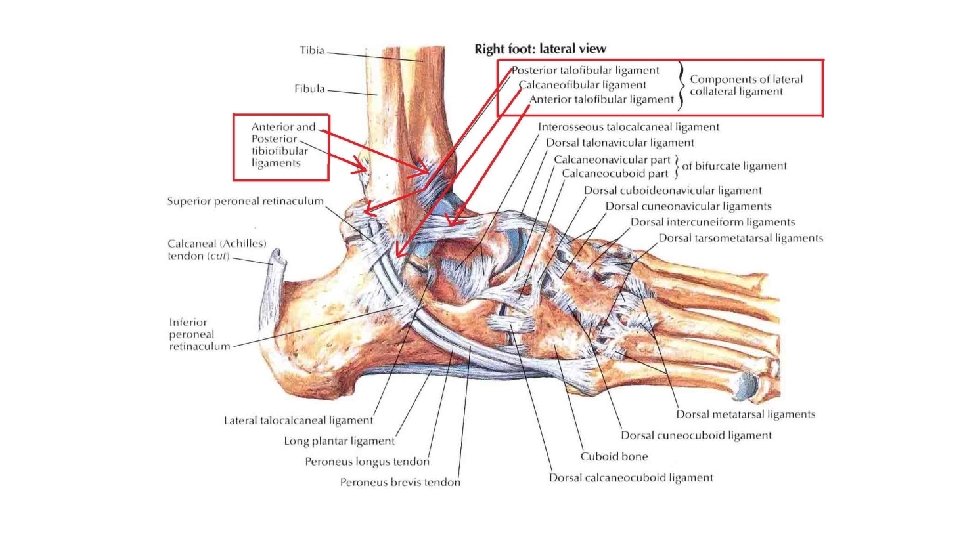
• All ligaments that support the proximal and distal tibiofibular joints the 1. Crural tibiofibular interosseous ligament 2. Anterior and posterior tibiofibular ligaments 3. Tibiofibular interosseous membrane (important for stability of the mortise and, therefore, for stability of the ankle) • Two other major ligaments maintain contact and congruence of the mortise and talus and control medial-lateral joint stability. 1. Medial collateral ligament (MCL) 2. Lateral collateral ligament (LCL). Both of these ligaments also provide key support for the subtalar (or talocalcaneal) joint that they also cross.
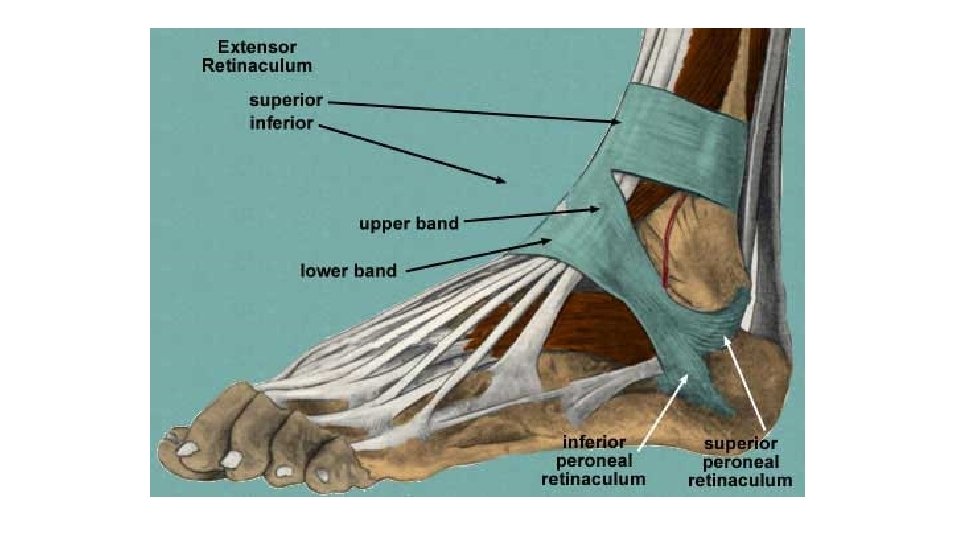
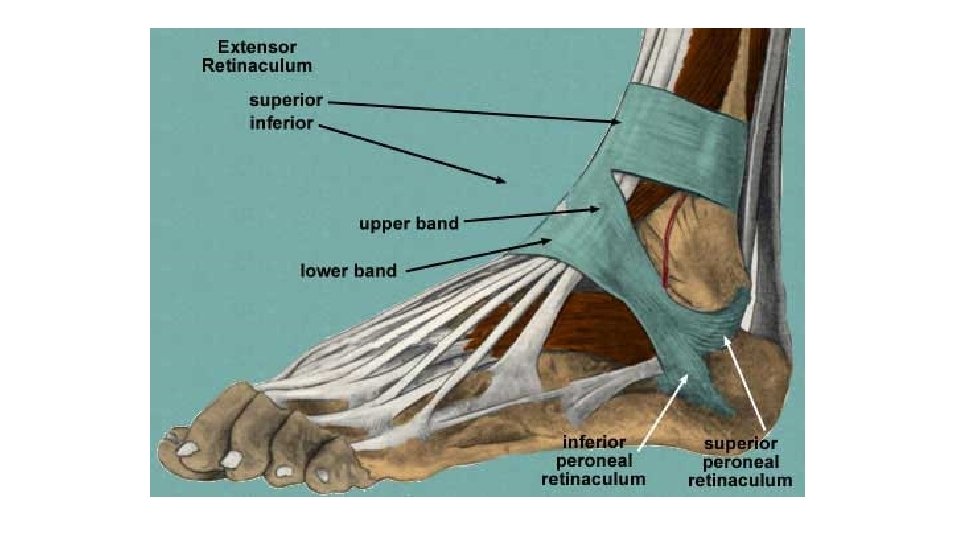
The function of the collaterals at the ankle joint, therefore, are difficult to separate from the function at the subtalar joint. Portions of the extensor and peroneal retinaculae of the ankle are also credited with contributing to stability at the ankle joint.
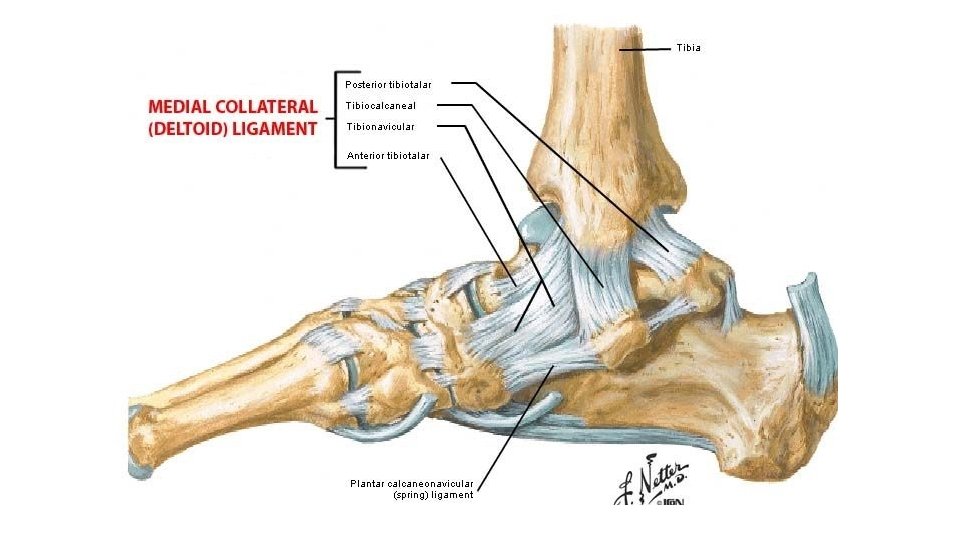
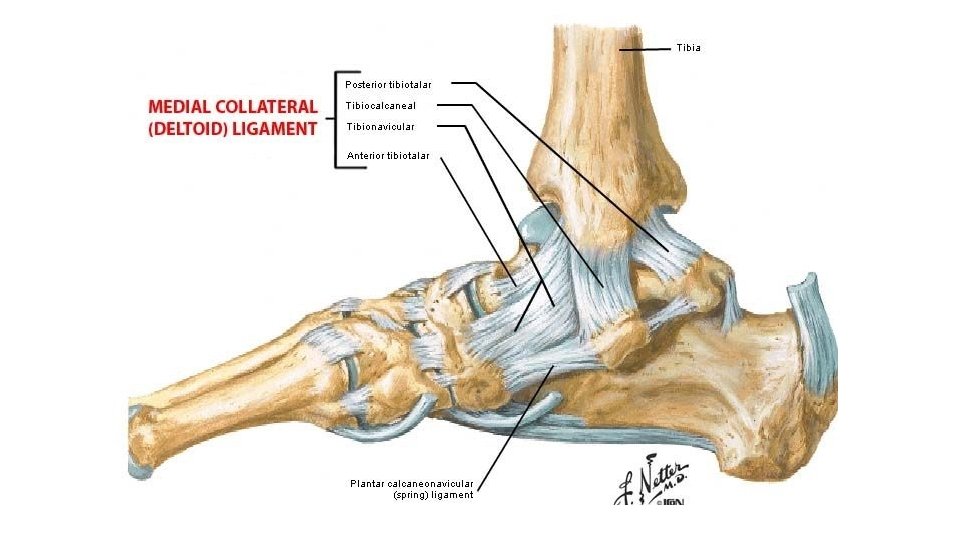
The MCL /deltoid ligament. 1. It is a fan-shaped. 2. It has superficial and deep fibers that arise from the borders of the tibial malleolus and insert in a continuous line on the navicular bone anteriorly and on the talus and calcaneus distally and posteriorly 3. It is extremely strong: Valgus forces that would open the medial side of the ankle may actually fracture and displace (avulse) the tibial malleolus before the deltoid ligament tears. 4. It helps control medial distraction stresses on the ankle joint and also helps check motion at the extremes of joint range, particularly with calcaneal eversion.
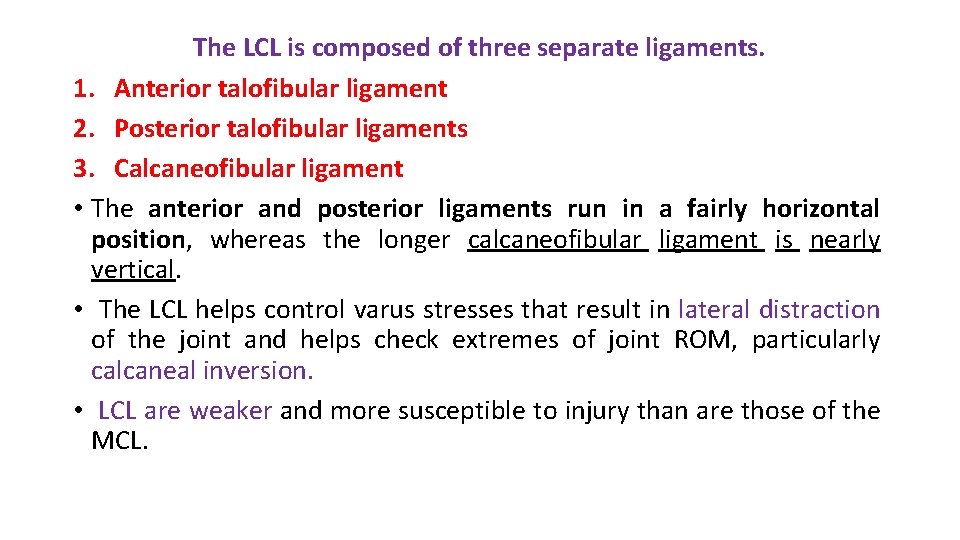
The LCL is composed of three separate ligaments. 1. Anterior talofibular ligament 2. Posterior talofibular ligaments 3. Calcaneofibular ligament • The anterior and posterior ligaments run in a fairly horizontal position, whereas the longer calcaneofibular ligament is nearly vertical. • The LCL helps control varus stresses that result in lateral distraction of the joint and helps check extremes of joint ROM, particularly calcaneal inversion. • LCL are weaker and more susceptible to injury than are those of the MCL.


The anterior talofibular ligament is the weakest and most commonly torn of the LCLs This ligament is most easily stressed when the ankle is in a plantarflexed and inverted position, such as when a basketball player lands on another player’s foot. Rupture of the anterior talofibular ligament often results in anterolateral rotatory instability of the ankle. The posterior talofibular ligament is the strongest of the collateral ligaments and is rarely torn in isolation.
• The inferior extensor retinaculum may also contribute to stability of the ankle joint. • Two additional structures that lie close and parallel to the calcaneofibular ligament appear to reinforce that ligament and serve a similar function. • These are the inferior band of the superior peroneal retinaculum and the much more variable lateral talocalcaneal ligament. • The ankle collateral ligaments and the retinaculae also contribute to stability of the subtalar joint.

• The ankle joint has one degree of freedom: with dorsiflexion/plantarflexion occurring between the talus and the mortise. 1. At the ankle, dorsiflexion refers to a motion of the head of the talus dorsally (or upward) while the body of the talus moves posteriorly in the mortise. 2. Plantarflexion is the opposite motion of the head and body of the talus.
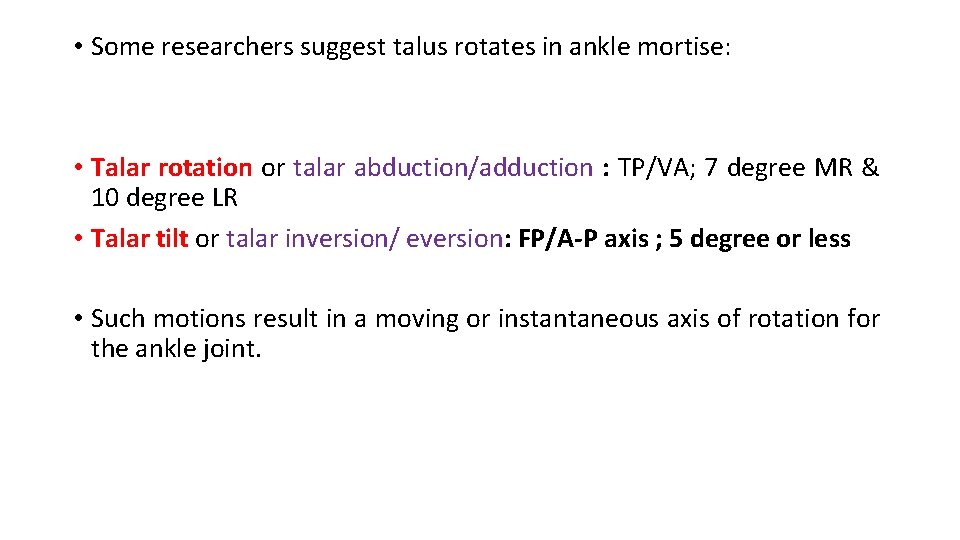
• Some researchers suggest talus rotates in ankle mortise: • Talar rotation or talar abduction/adduction : TP/VA; 7 degree MR & 10 degree LR • Talar tilt or talar inversion/ eversion: FP/A-P axis ; 5 degree or less • Such motions result in a moving or instantaneous axis of rotation for the ankle joint.
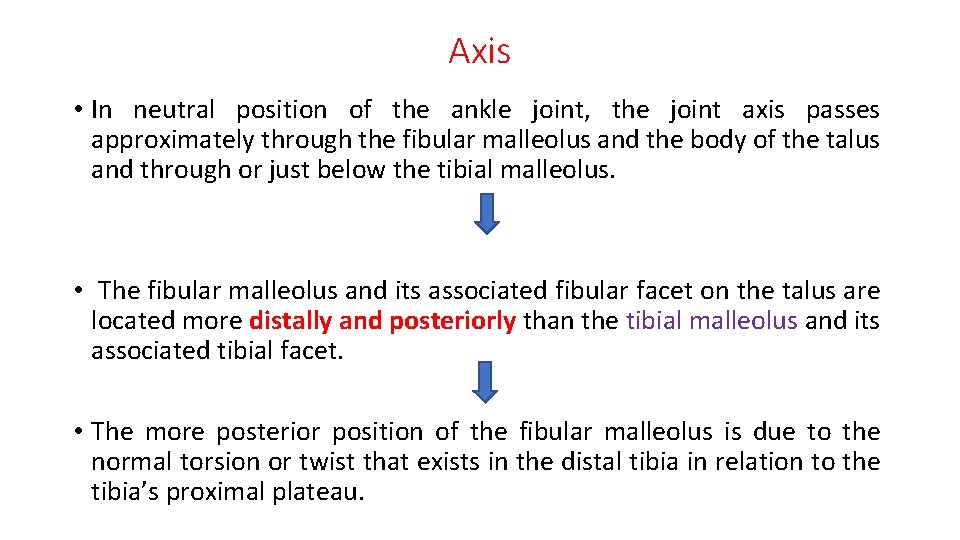
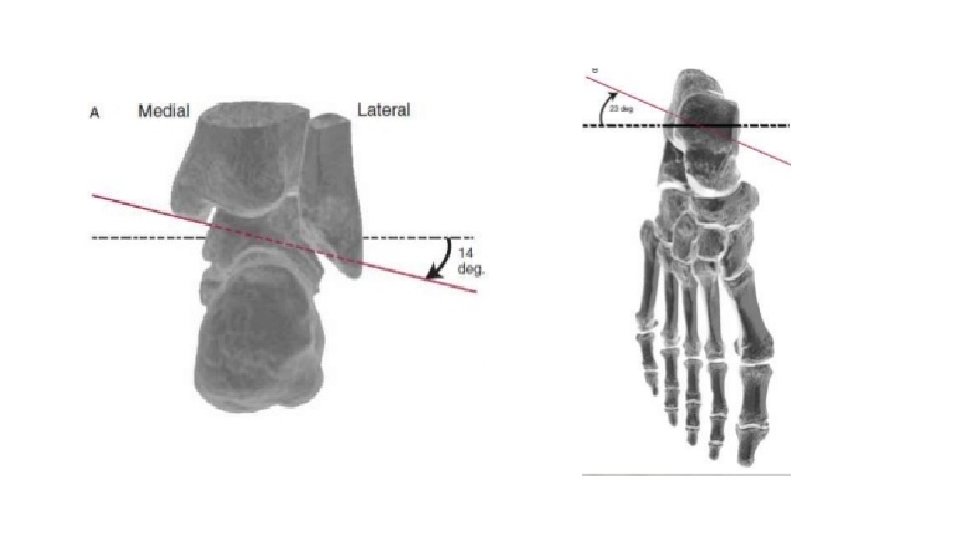
Axis • In neutral position of the ankle joint, the joint axis passes approximately through the fibular malleolus and the body of the talus and through or just below the tibial malleolus. • The fibular malleolus and its associated fibular facet on the talus are located more distally and posteriorly than the tibial malleolus and its associated tibial facet. • The more posterior position of the fibular malleolus is due to the normal torsion or twist that exists in the distal tibia in relation to the tibia’s proximal plateau.
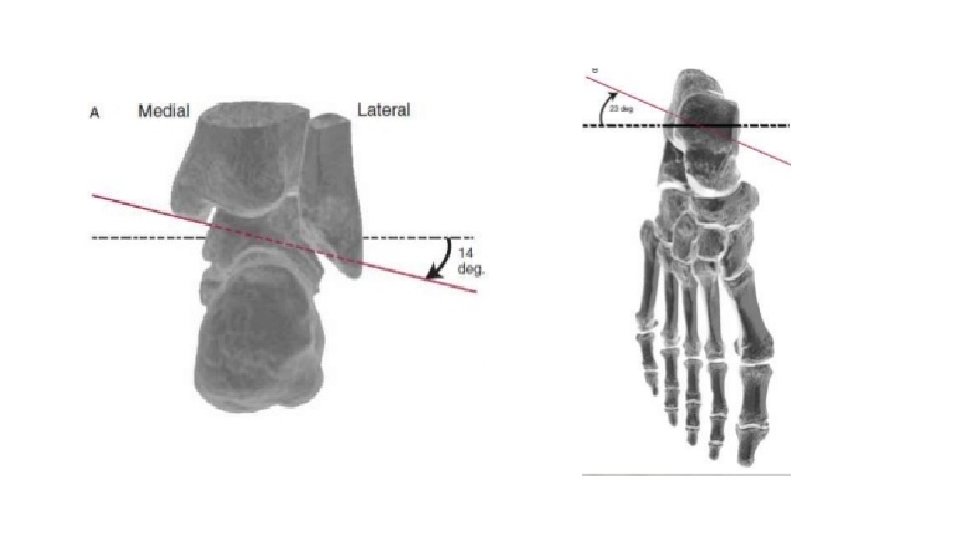
This twisting may be referred to as tibial torsion (or tibiofibular torsion because both the tibia and fibula are involved with the rotation in the transverse plane) and accounts for the toe-out position of the foot in normal standing. The torsion in the tibia is similar to the torsion found in the shaft of the femur, although normally reversed in direction. • An average value for this axis angle from frontal plane taken from several studies would be 23 degree. 9 • The lower position of the fibular malleolus, the axis of the ankle is inclined down on the lateral side which yields an average of 14 degree. 4 • Sagital plane 82 degree
In OKC • The DORSIFLEXION of the foot around a typically INCLINED ANKLE AXIS will not only bring the foot up but will also simultaneously bring it slightly lateral to the leg and appear to turn the foot longitudinally away from the midline. • Conversely, PLANTARFLEXION around the same SINGLE OBLIQUE ANKLE axis will result in the foot’s going down, moving medial to the leg and appearing to turn the foot longitudinally toward the midline.
In CKC • When the foot is in weight-bearing, the same relative pattern of motion exists when the tibia and fibular move on the foot. • In weight-bearing ankle dorsiflexion, the leg (tibia and fibula) will move toward and medial to the foot, as well as appear to rotate medially in the transverse plane. • The opposite occurs during weight- bearing ankle plantarflexion.
Thank YOU