Capillary circulation Tissue fluid formation edema Dr Nermine

- Slides: 58
Capillary circulation Tissue fluid formation edema Dr Nermine Kamal 1
INTENDED LEARNING OBJECTIVES (ILO) By the end of this lecture the learner will be able to: a-Explain the factors affecting capillary blood pressure. b-Discuss the different forces acting in the tissue fluid formation. c -Define edema and explain the mechanism of its formation 2 PHYSIOLOGY department
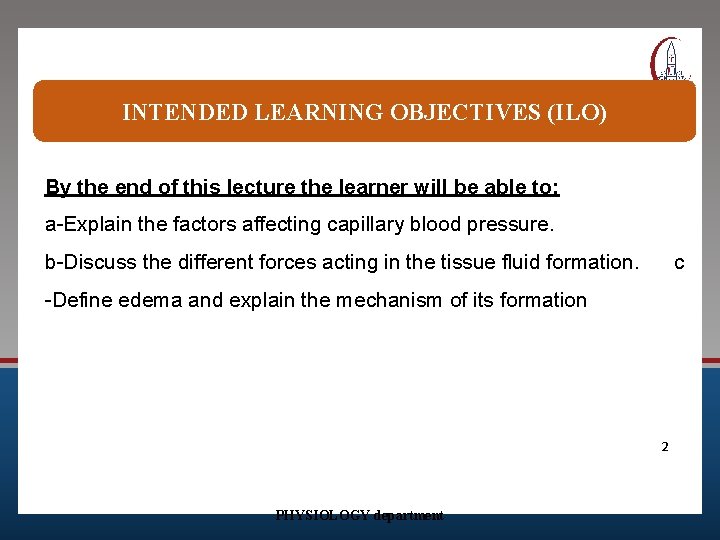
Outline the forces involved in tissue fluid formation. Explain mechanisms of edema in: Heart failure, renal failure, etc.
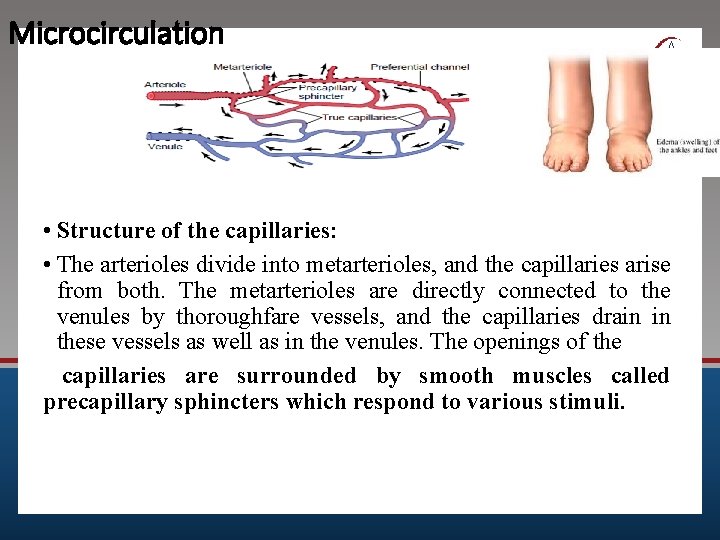
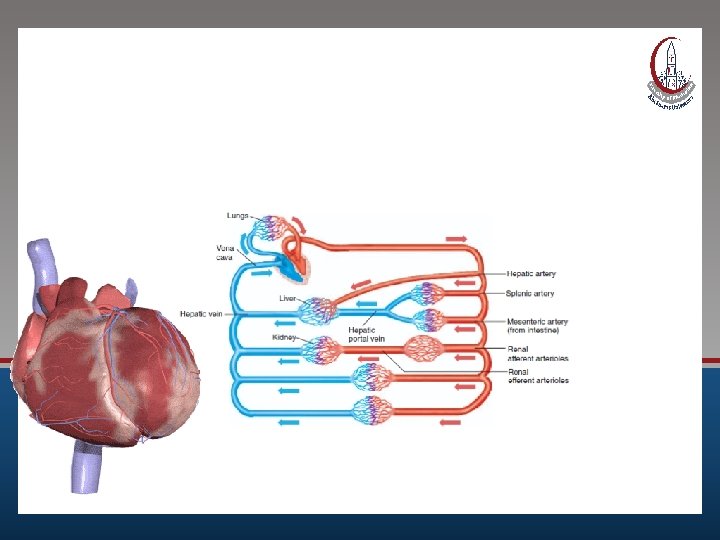
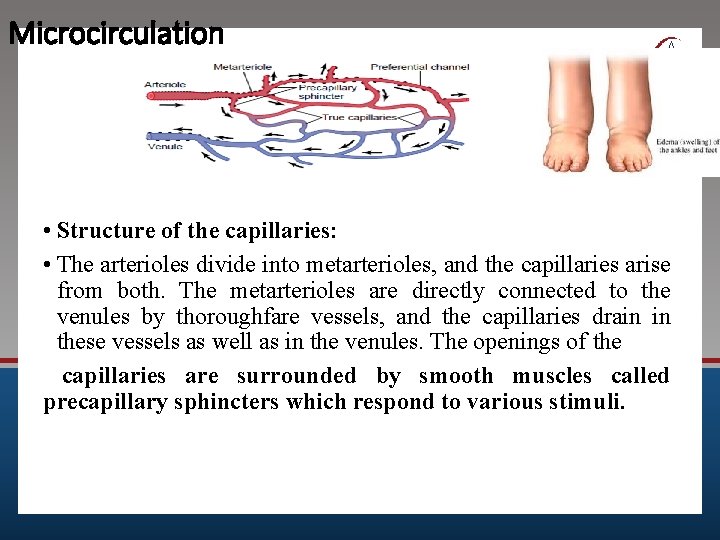
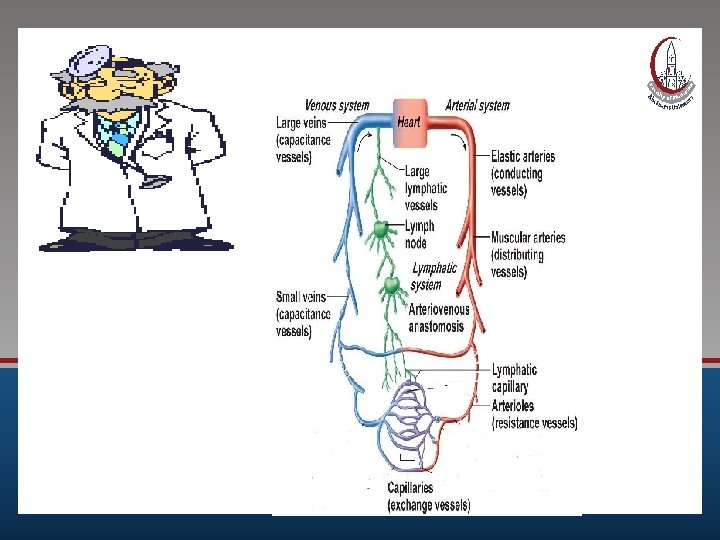
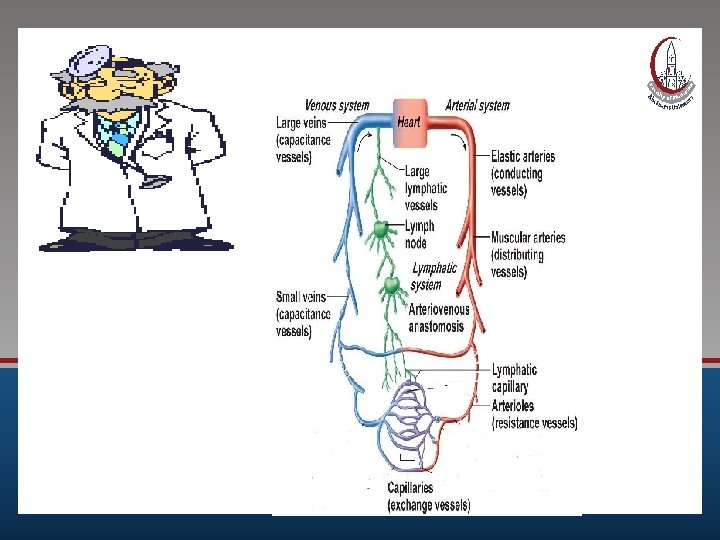
Microcirculation • Structure of the capillaries: • The arterioles divide into metarterioles, and the capillaries arise from both. The metarterioles are directly connected to the venules by thoroughfare vessels, and the capillaries drain in these vessels as well as in the venules. The openings of the capillaries are surrounded by smooth muscles called precapillary sphincters which respond to various stimuli.
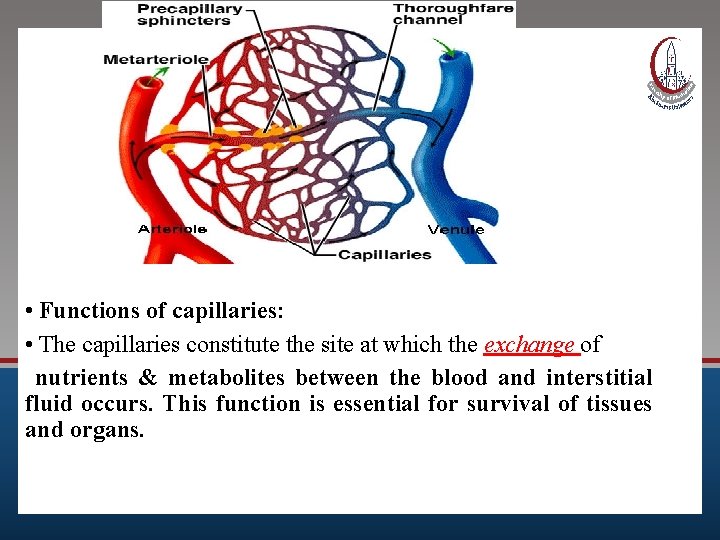
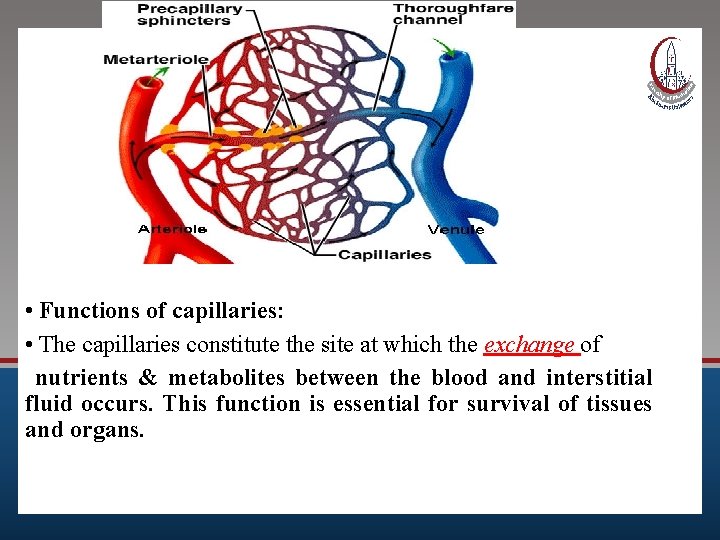
• Functions of capillaries: • The capillaries constitute the site at which the exchange of nutrients & metabolites between the blood and interstitial fluid occurs. This function is essential for survival of tissues and organs.
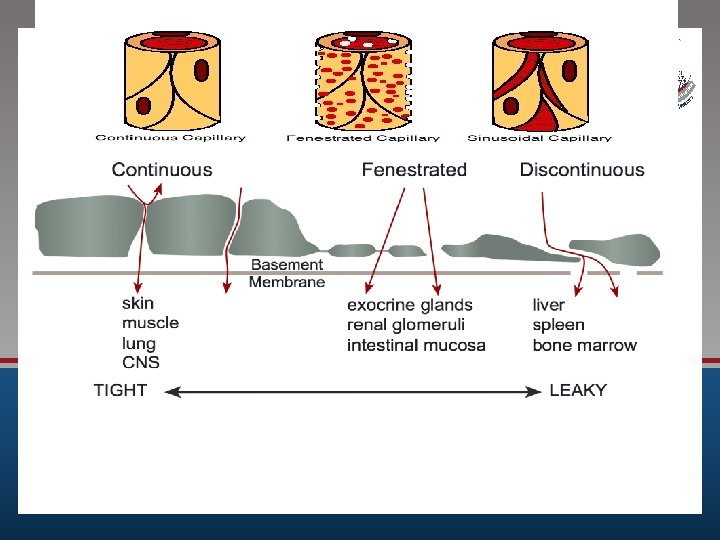
Types of capillaries
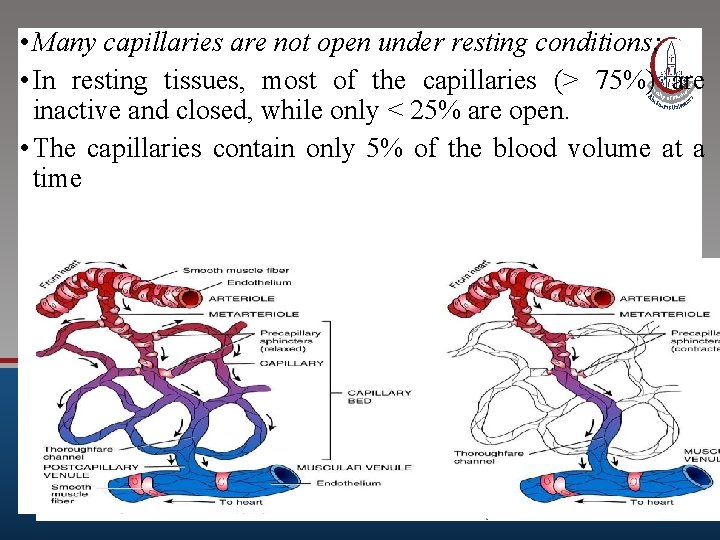
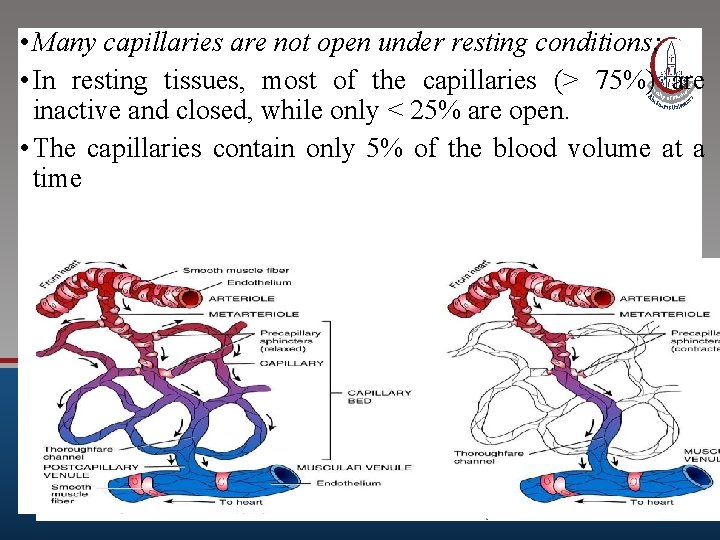
• Many capillaries are not open under resting conditions; • In resting tissues, most of the capillaries (> 75%) are inactive and closed, while only < 25% are open. • The capillaries contain only 5% of the blood volume at a time
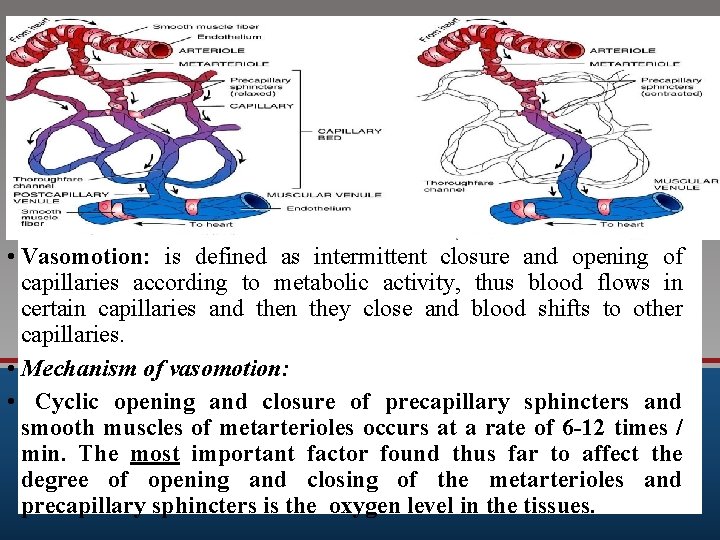
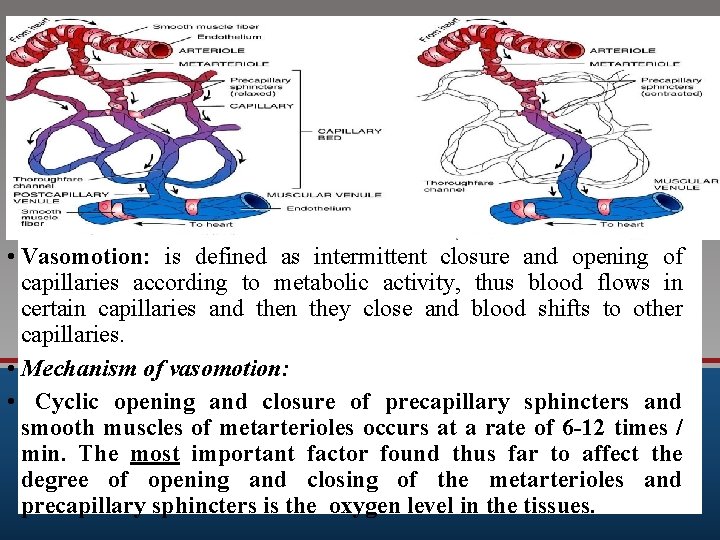
• Vasomotion: is defined as intermittent closure and opening of capillaries according to metabolic activity, thus blood flows in certain capillaries and then they close and blood shifts to other capillaries. • Mechanism of vasomotion: • Cyclic opening and closure of precapillary sphincters and smooth muscles of metarterioles occurs at a rate of 6 -12 times / min. The most important factor found thus far to affect the degree of opening and closing of the metarterioles and precapillary sphincters is the oxygen level in the tissues.
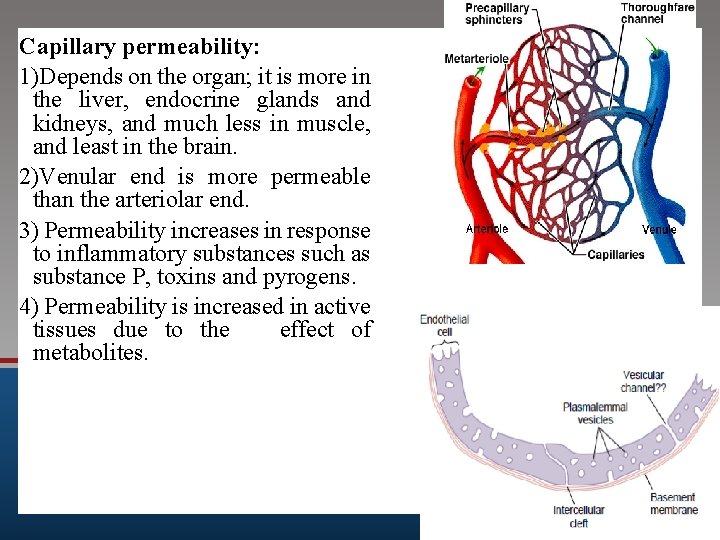
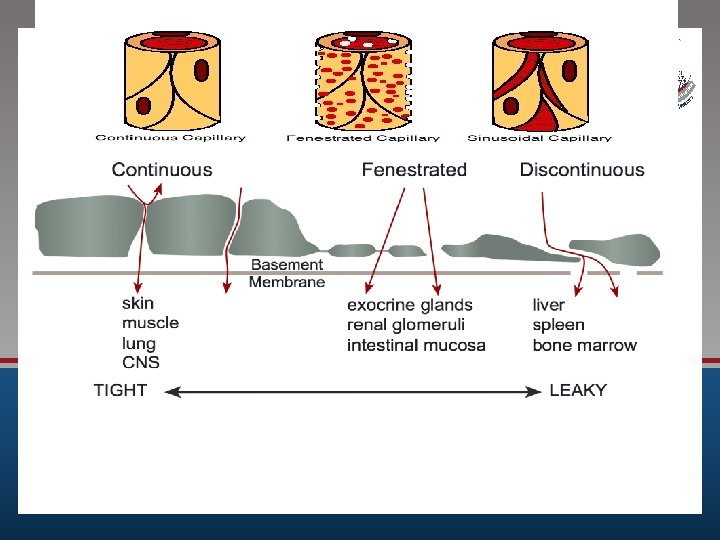
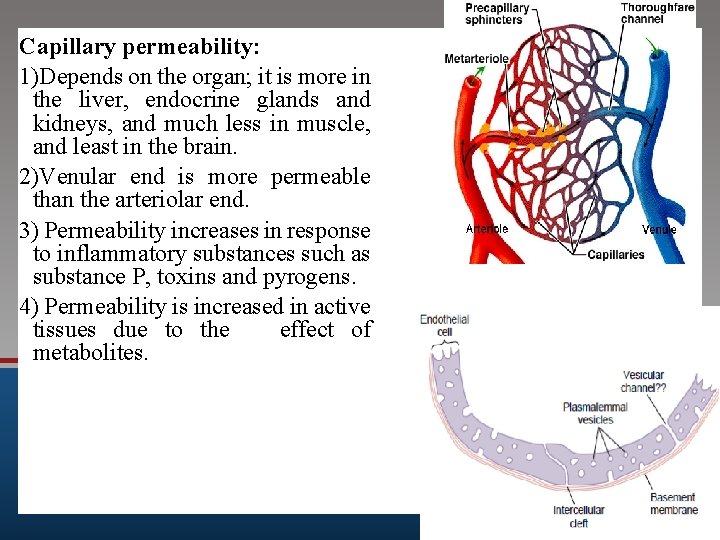
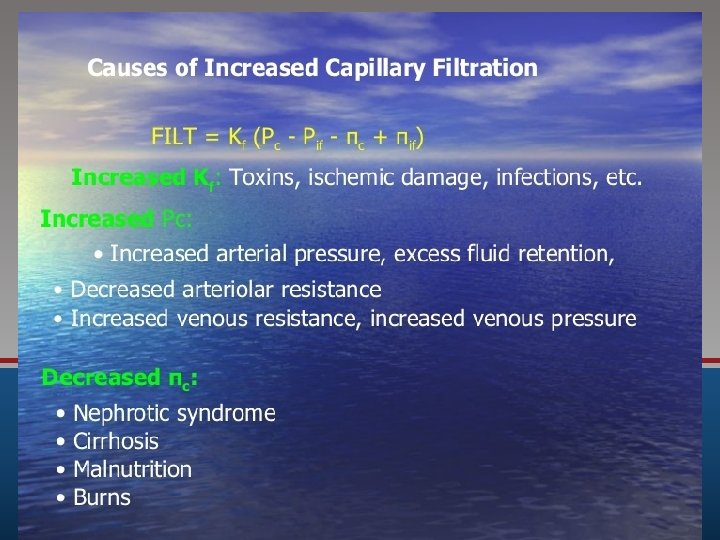
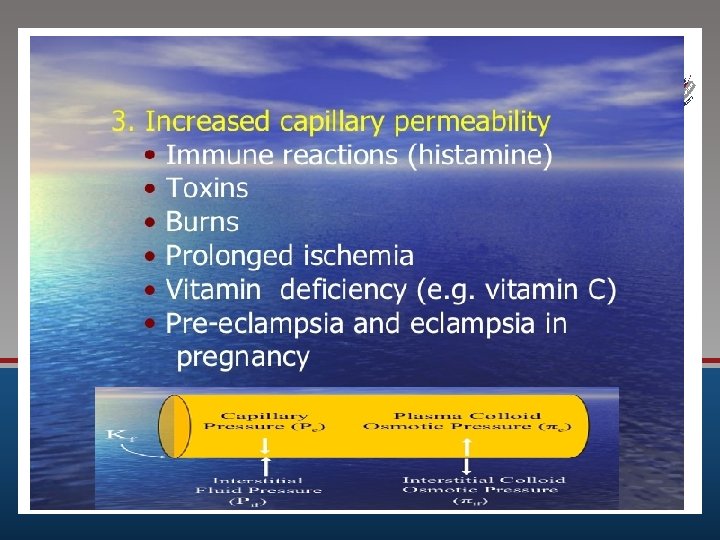
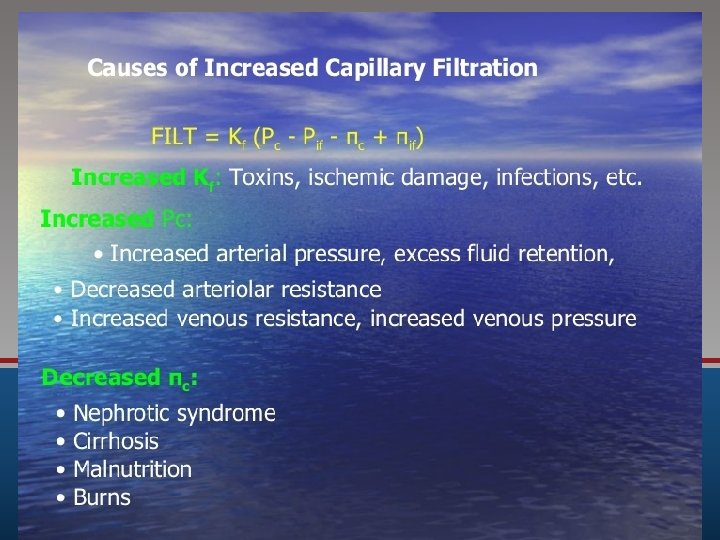
Capillary permeability: 1)Depends on the organ; it is more in the liver, endocrine glands and kidneys, and much less in muscle, and least in the brain. 2)Venular end is more permeable than the arteriolar end. 3) Permeability increases in response to inflammatory substances such as substance P, toxins and pyrogens. 4) Permeability is increased in active tissues due to the effect of metabolites. 5)Plasma proteins decrease permeability by closing capillary pores. In hypoproteinemia, as in liver disease or renal disease, the permeability increases.
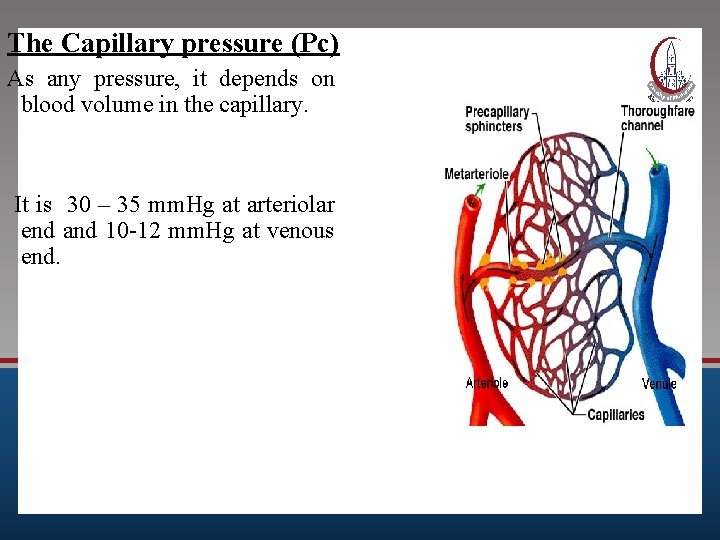
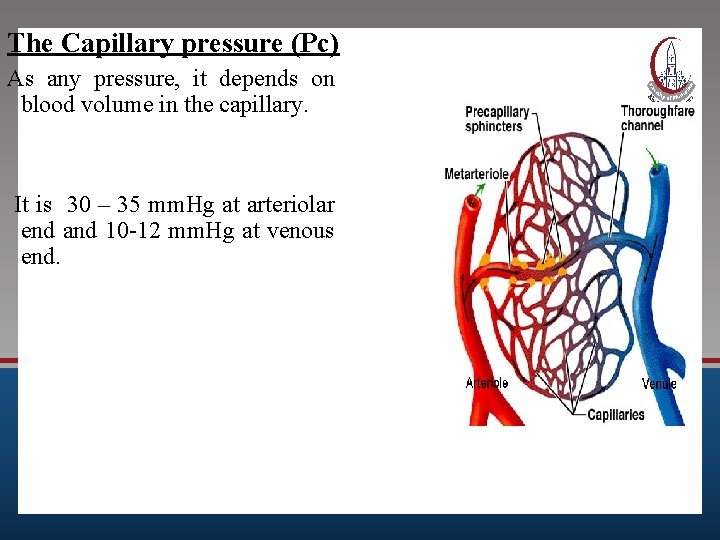
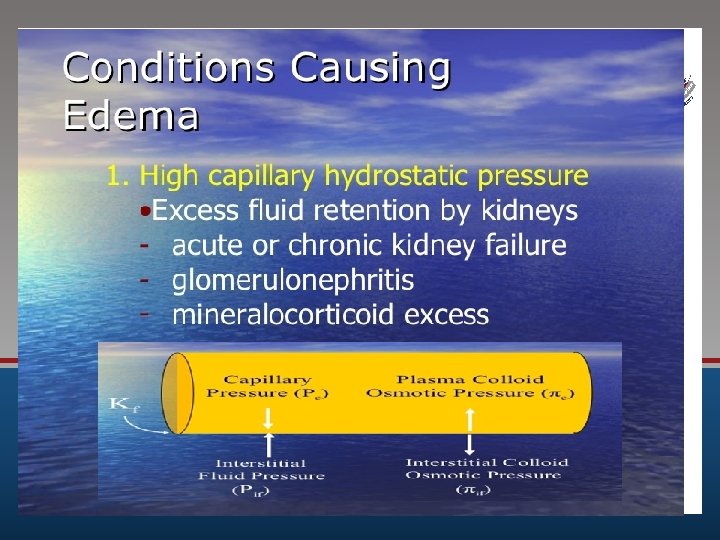
The Capillary pressure (Pc) As any pressure, it depends on blood volume in the capillary. It is 30 – 35 mm. Hg at arteriolar end and 10 -12 mm. Hg at venous end.
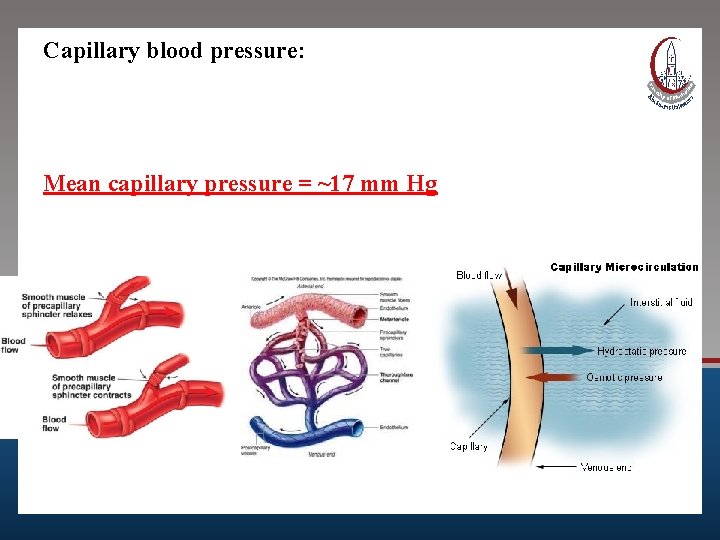
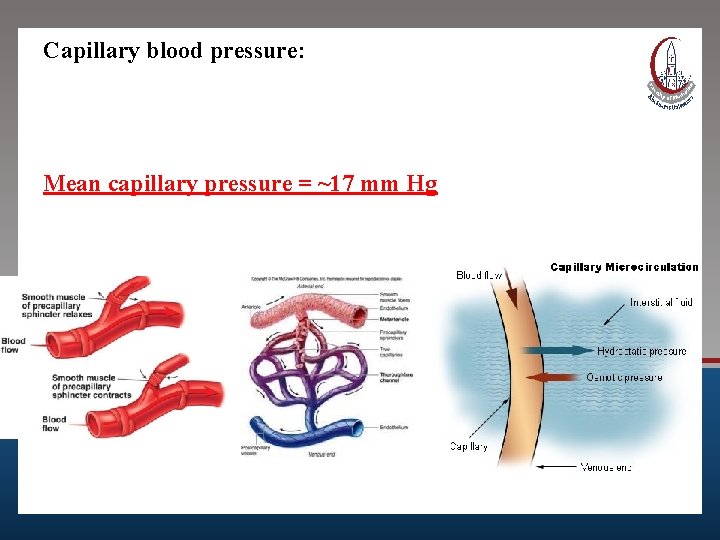
Capillary blood pressure: Mean capillary pressure = ~17 mm Hg
Factors affecting capillary pressure
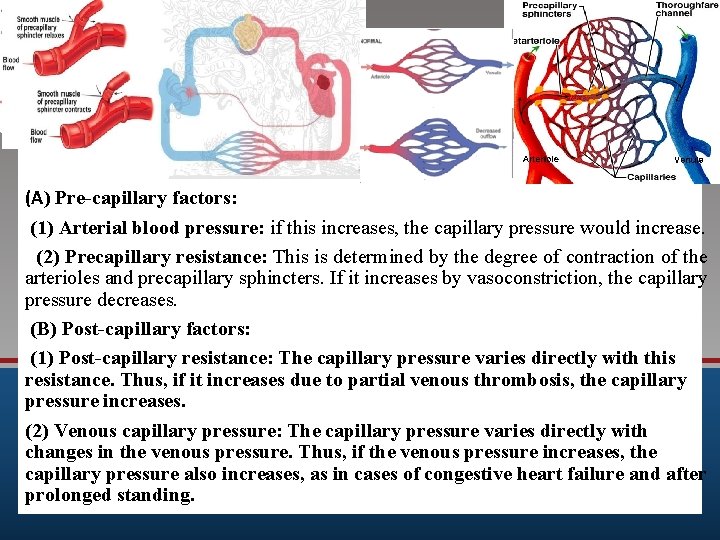
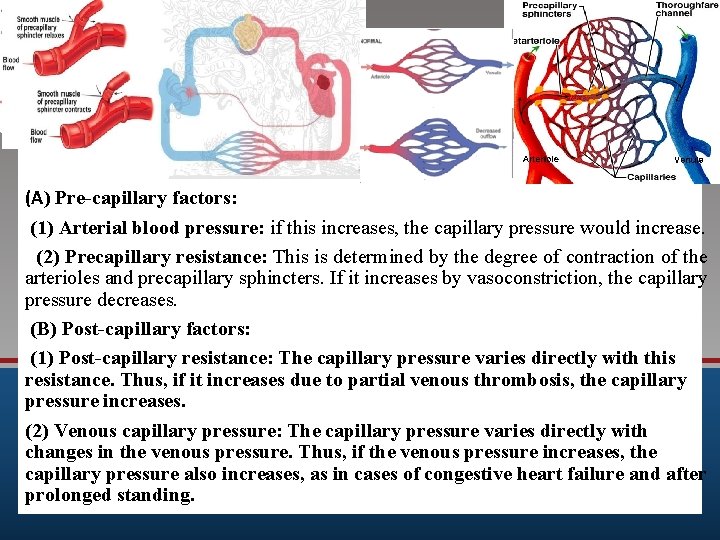
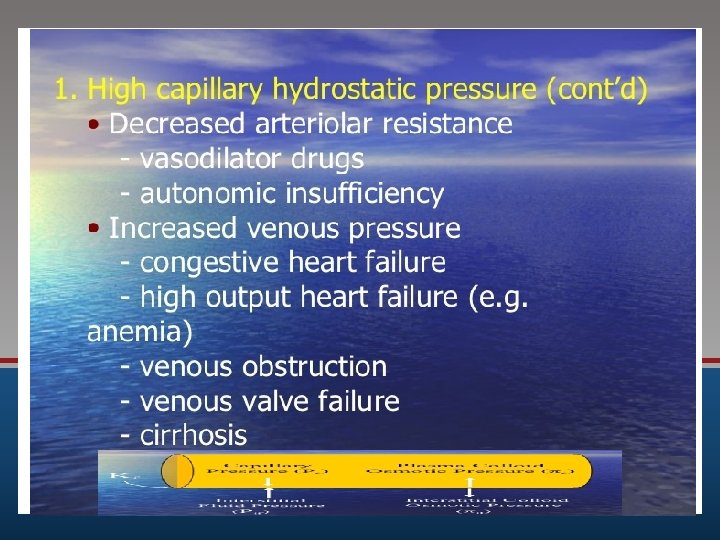
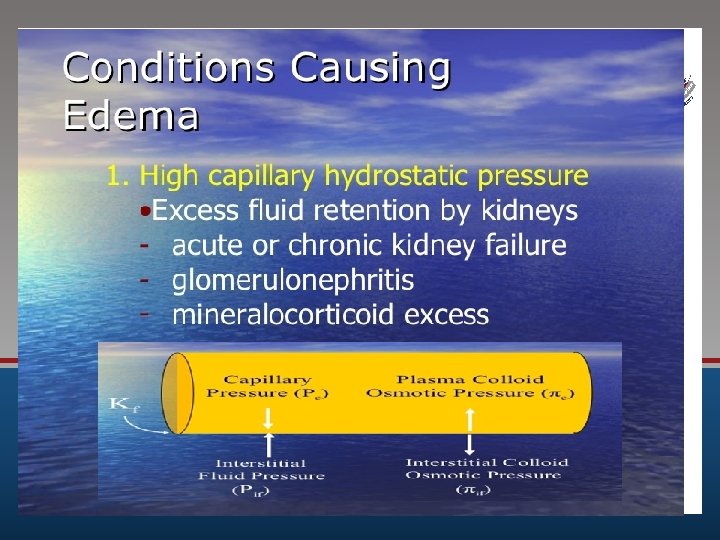
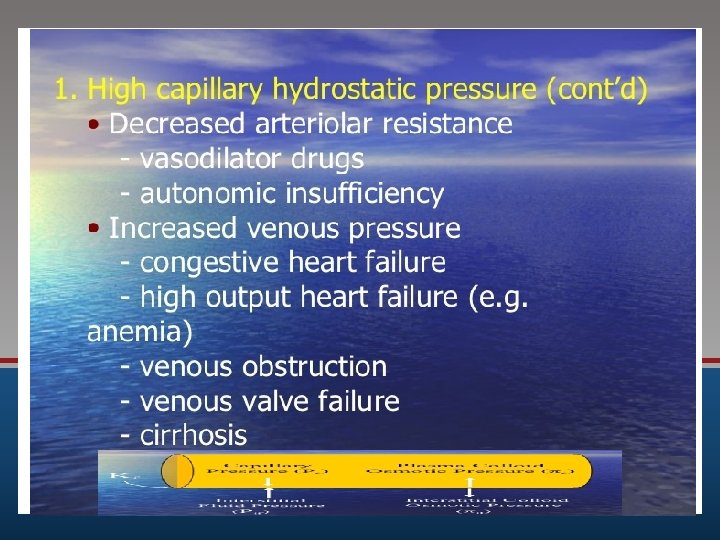
(A) Pre-capillary factors: (1) Arterial blood pressure: if this increases, the capillary pressure would increase. (2) Precapillary resistance: This is determined by the degree of contraction of the arterioles and precapillary sphincters. If it increases by vasoconstriction, the capillary pressure decreases. (B) Post-capillary factors: (1) Post-capillary resistance: The capillary pressure varies directly with this resistance. Thus, if it increases due to partial venous thrombosis, the capillary pressure increases. (2) Venous capillary pressure: The capillary pressure varies directly with changes in the venous pressure. Thus, if the venous pressure increases, the capillary pressure also increases, as in cases of congestive heart failure and after prolonged standing.
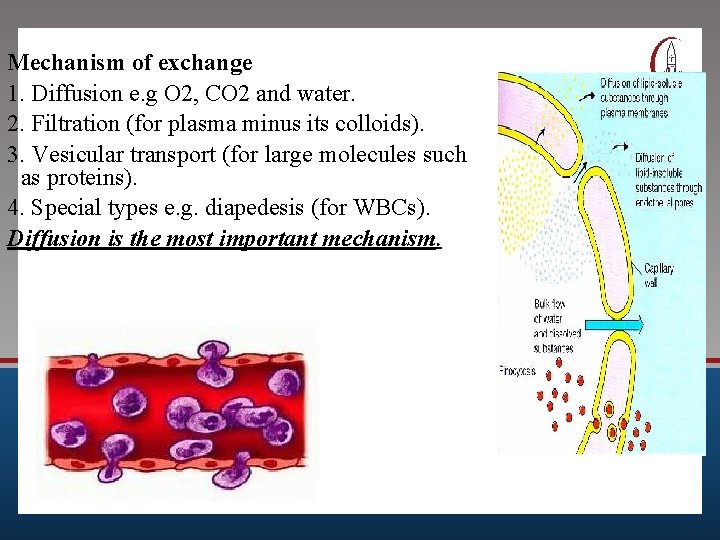
Mechanism of exchange
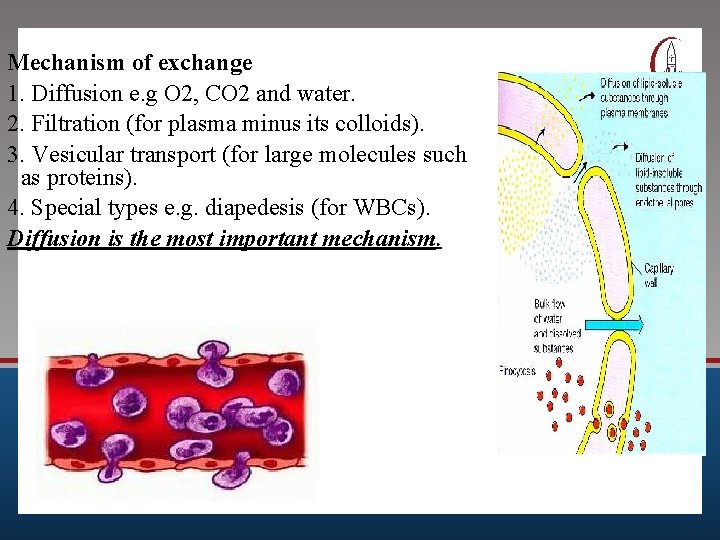
Mechanism of exchange 1. Diffusion e. g O 2, CO 2 and water. 2. Filtration (for plasma minus its colloids). 3. Vesicular transport (for large molecules such as proteins). 4. Special types e. g. diapedesis (for WBCs). Diffusion is the most important mechanism.
Outline the forces involved in tissue fluid formation. Explain mechanisms of edema in: Heart failure, renal failure, etc.
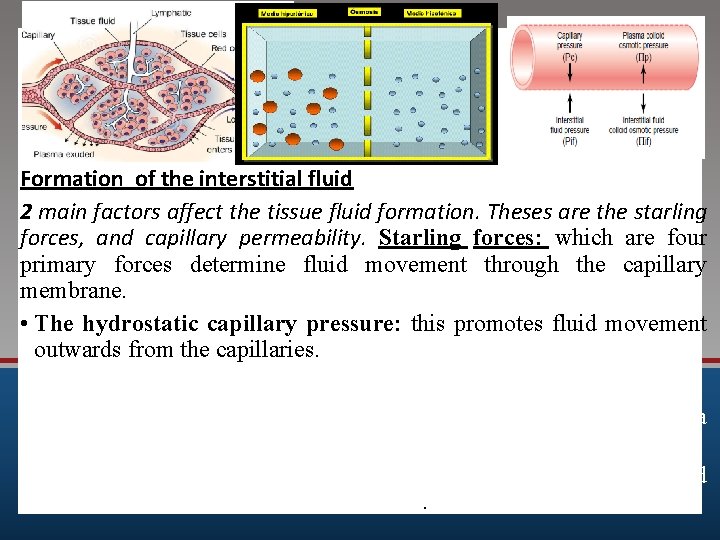
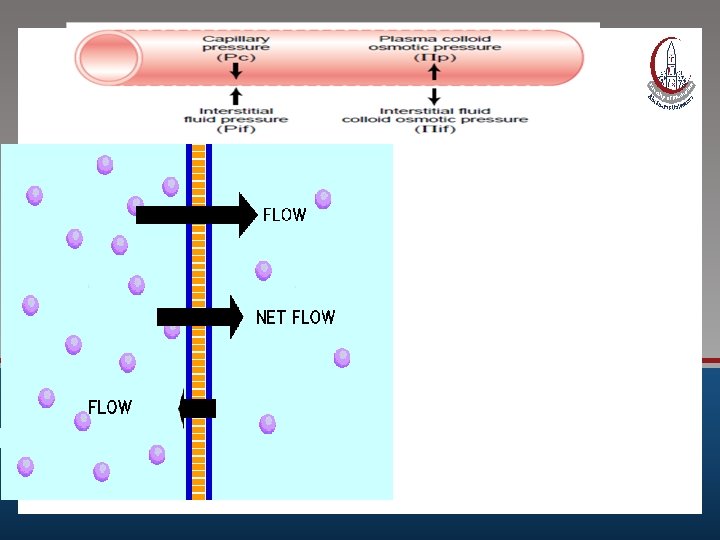
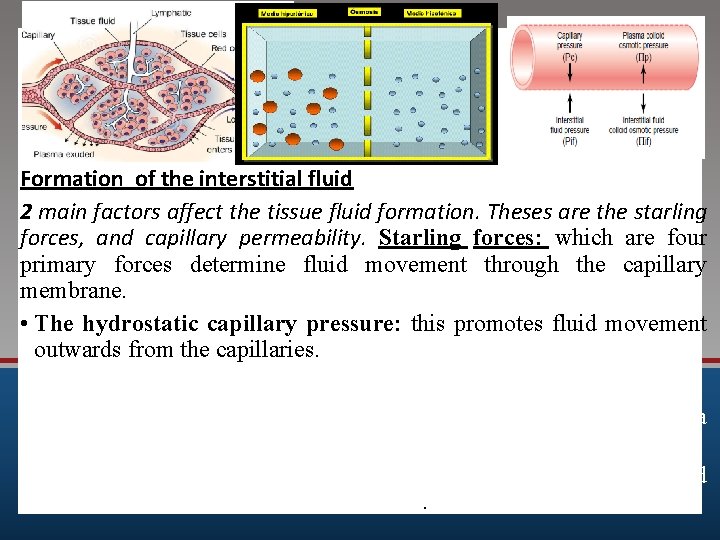
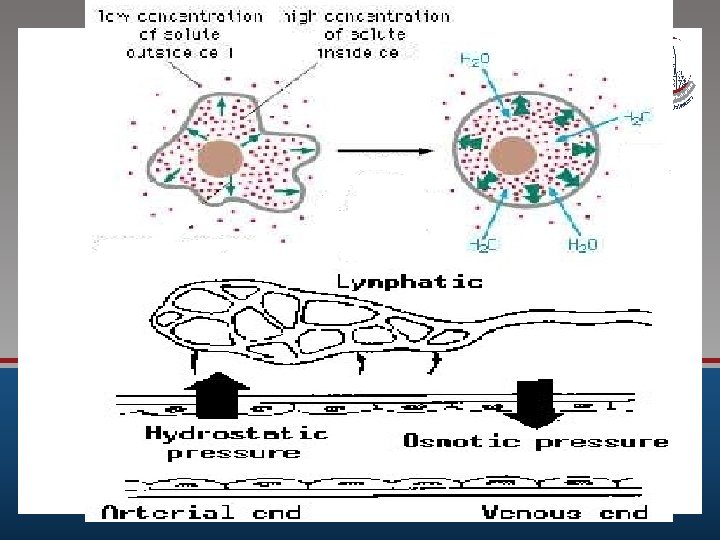
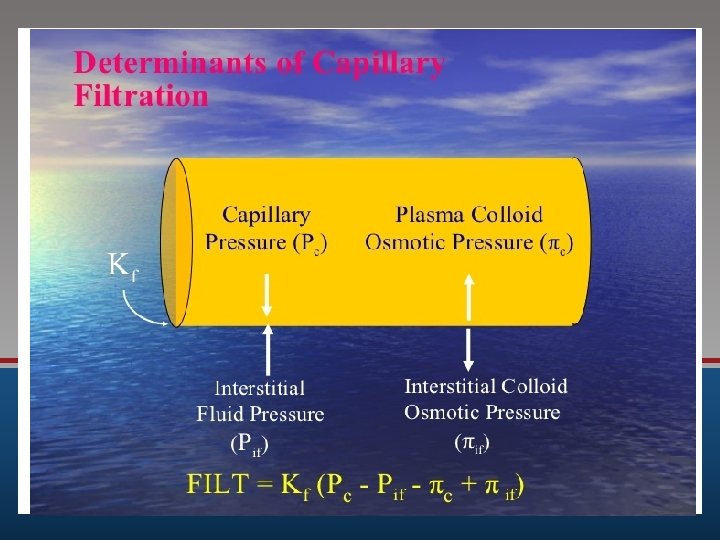
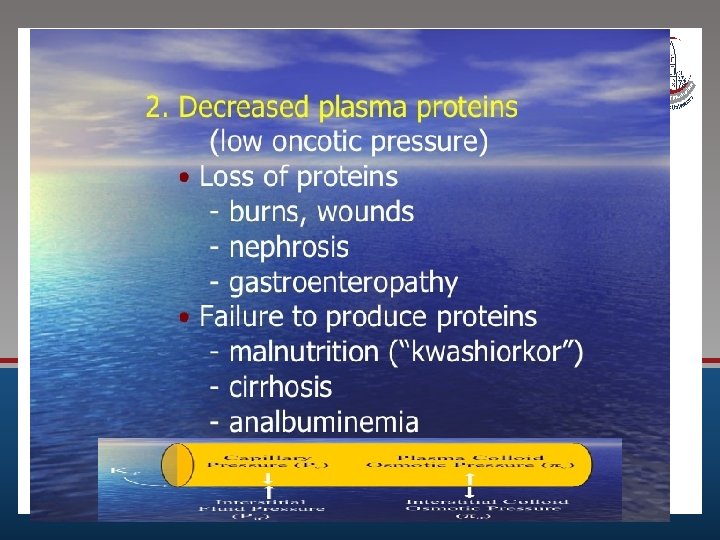
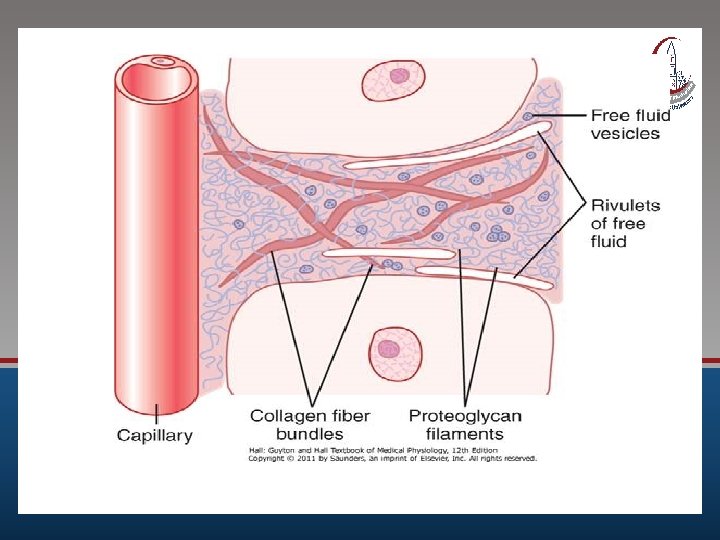
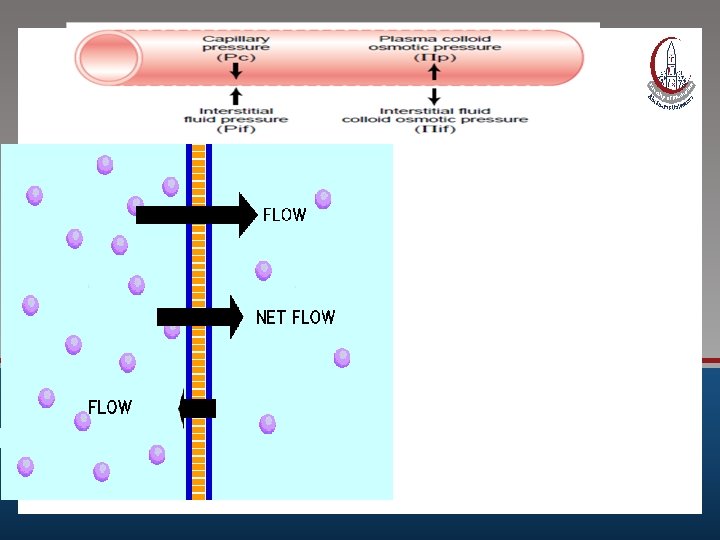
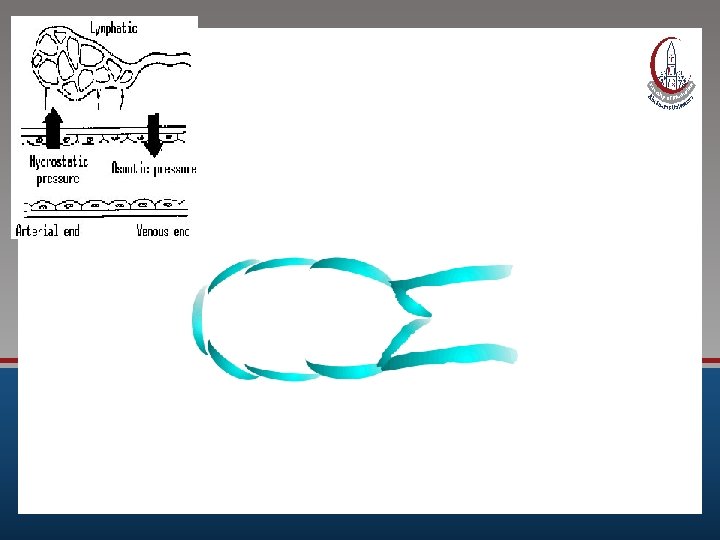
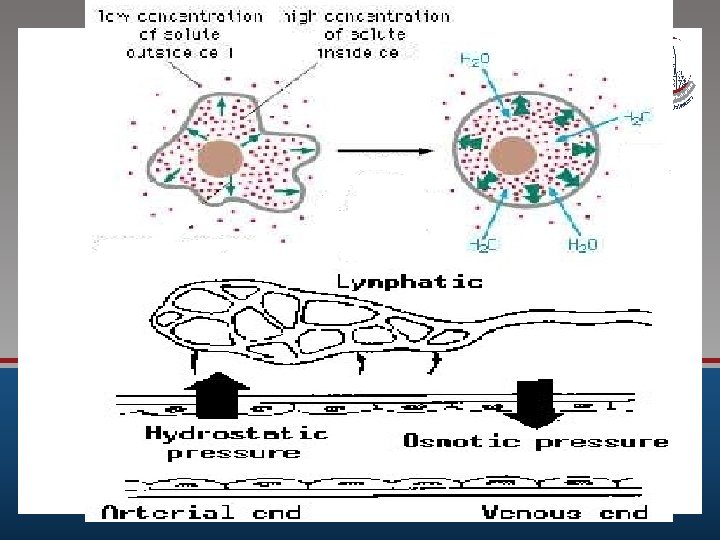
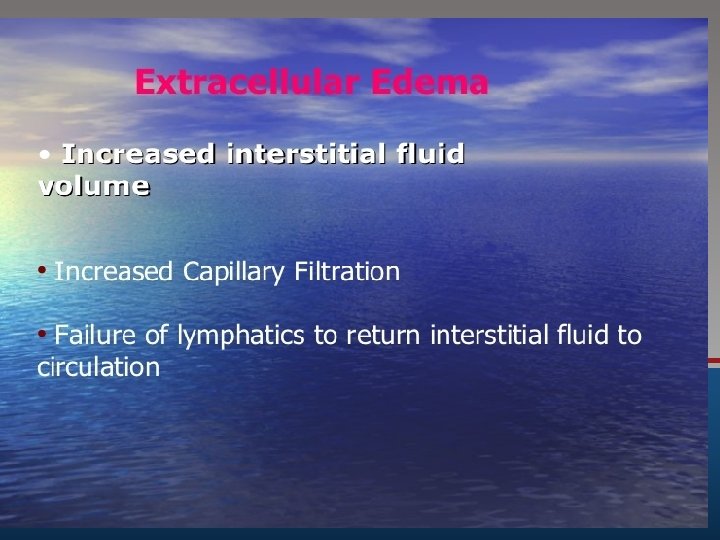
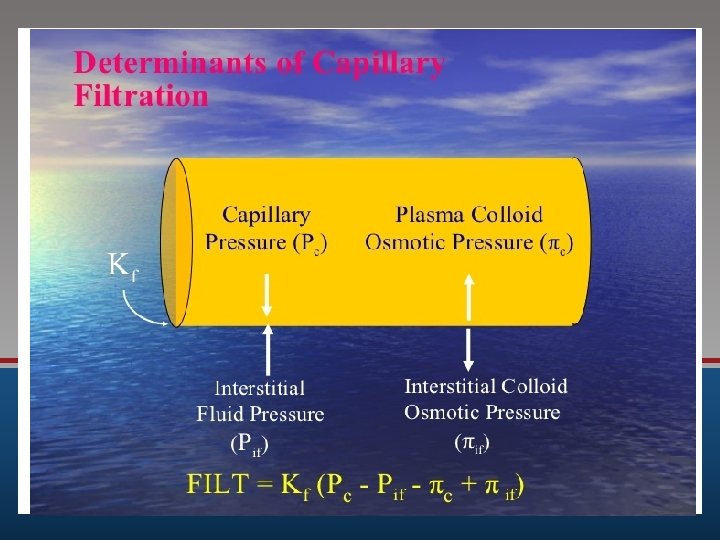
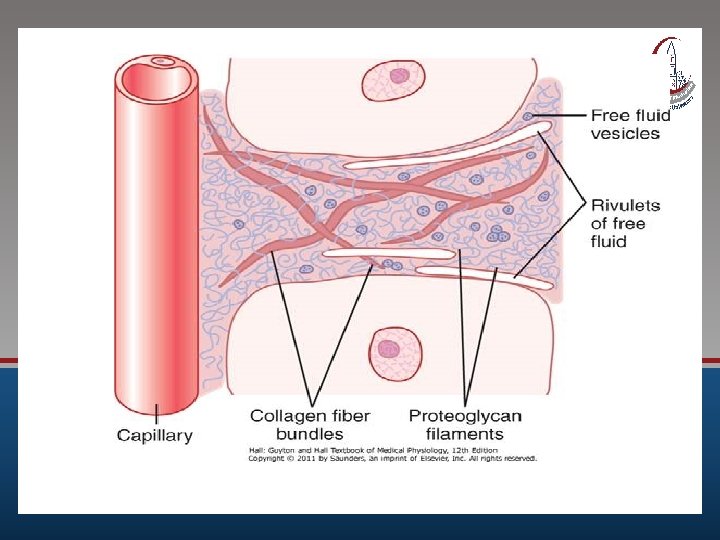
Formation of the interstitial fluid 2 main factors affect the tissue fluid formation. Theses are the starling forces, and capillary permeability. Starling forces: which are four primary forces determine fluid movement through the capillary membrane. • The hydrostatic capillary pressure: this promotes fluid movement outwards from the capillaries. • The interstitial fluid pressure. • The plasma osmotic pressure: This is produced mainly by plasma albumin, and it promotes fluid movement into the capillaries. • The interstitial fluid osmotic pressure: This promotes fluid movement outwards from the capillaries.
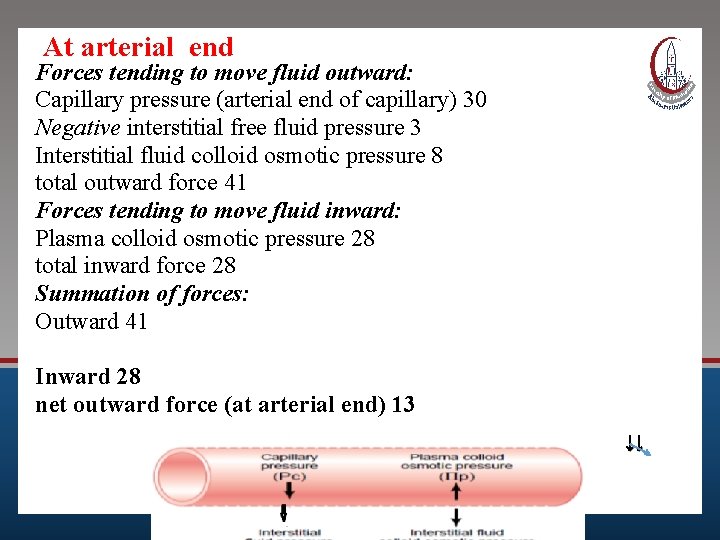
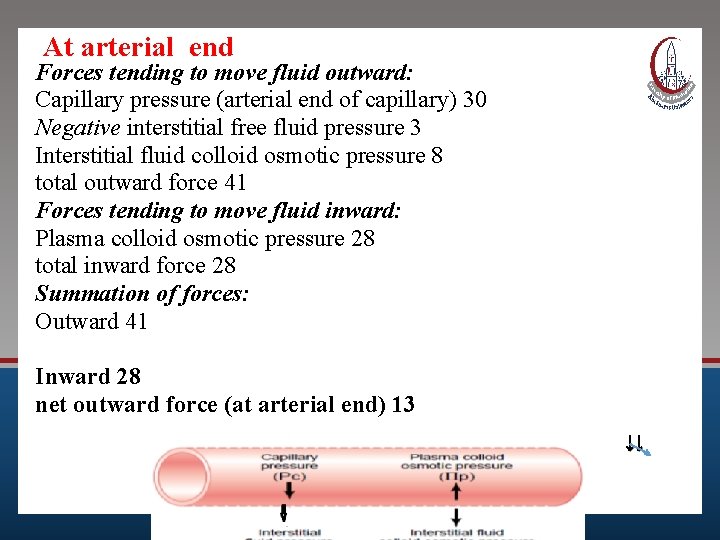
At arterial end Forces tending to move fluid outward: Capillary pressure (arterial end of capillary) 30 Negative interstitial free fluid pressure 3 Interstitial fluid colloid osmotic pressure 8 total outward force 41 Forces tending to move fluid inward: Plasma colloid osmotic pressure 28 total inward force 28 Summation of forces: Outward 41 Inward 28 net outward force (at arterial end) 13 ↓↓
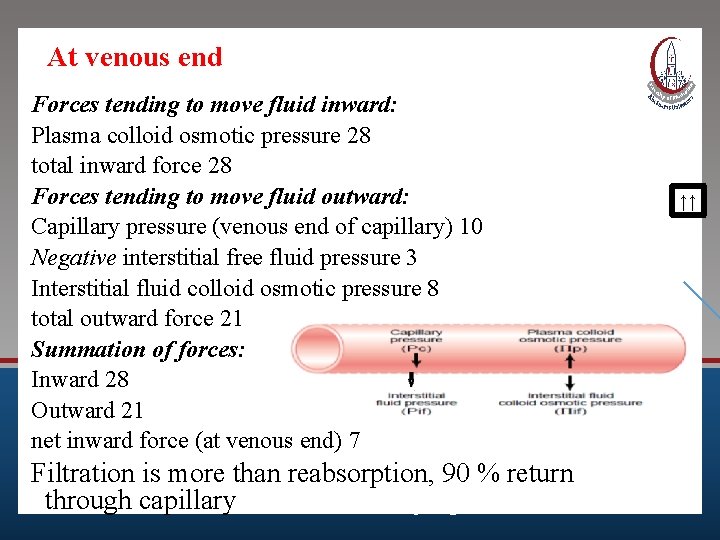
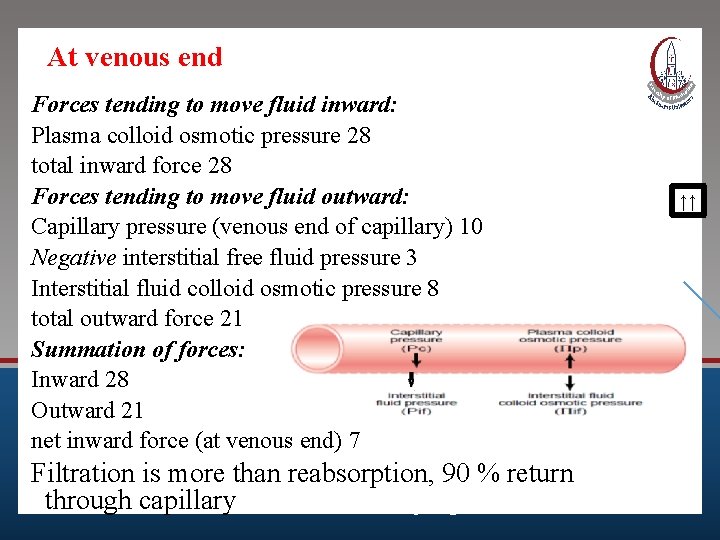
At venous end Forces tending to move fluid inward: Plasma colloid osmotic pressure 28 total inward force 28 Forces tending to move fluid outward: Capillary pressure (venous end of capillary) 10 Negative interstitial free fluid pressure 3 Interstitial fluid colloid osmotic pressure 8 total outward force 21 Summation of forces: Inward 28 Outward 21 net inward force (at venous end) 7 Filtration is more than reabsorption, 90 % return through capillary and 10% with lymph. ↑↑
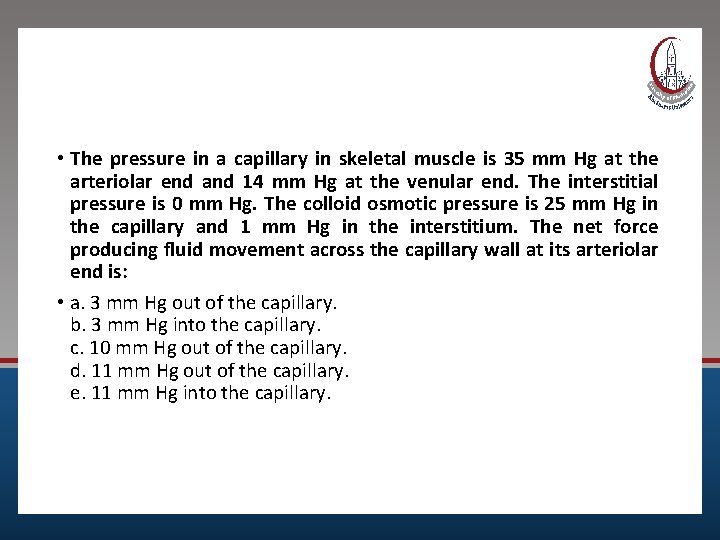
• The pressure in a capillary in skeletal muscle is 35 mm Hg at the arteriolar end and 14 mm Hg at the venular end. The interstitial pressure is 0 mm Hg. The colloid osmotic pressure is 25 mm Hg in the capillary and 1 mm Hg in the interstitium. The net force producing fluid movement across the capillary wall at its arteriolar end is: • a. 3 mm Hg out of the capillary. b. 3 mm Hg into the capillary. c. 10 mm Hg out of the capillary. d. 11 mm Hg out of the capillary. e. 11 mm Hg into the capillary.
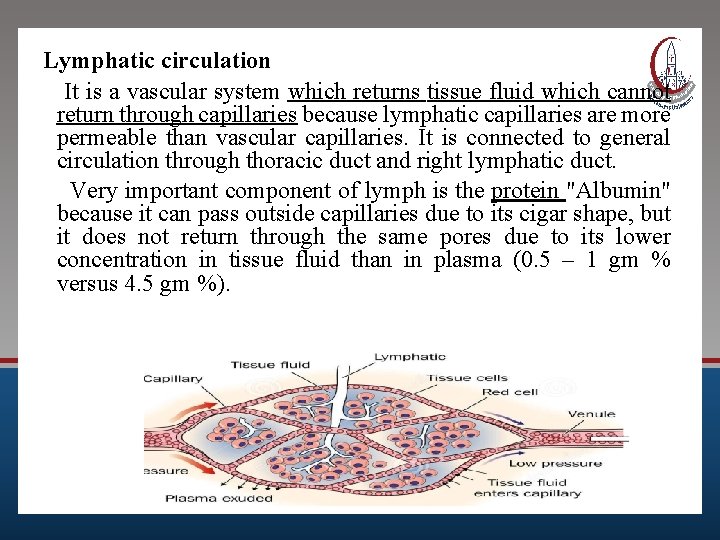
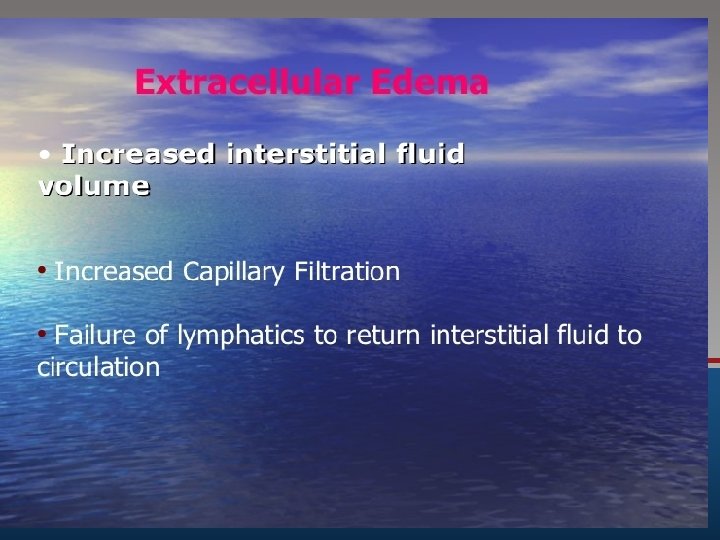
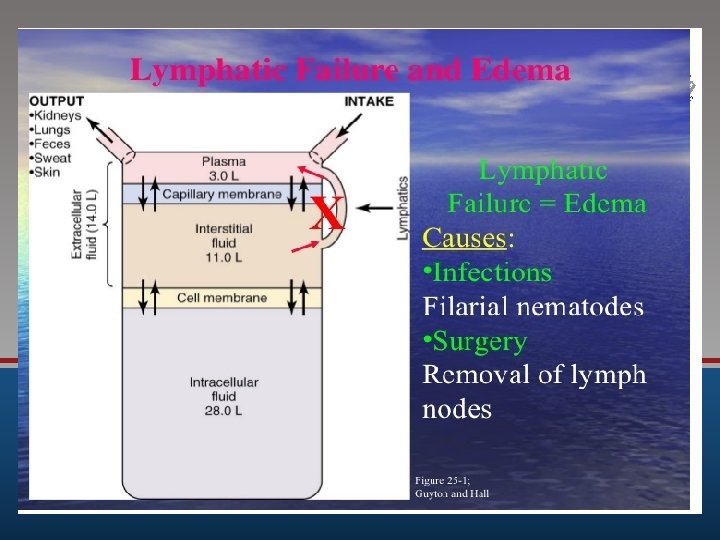
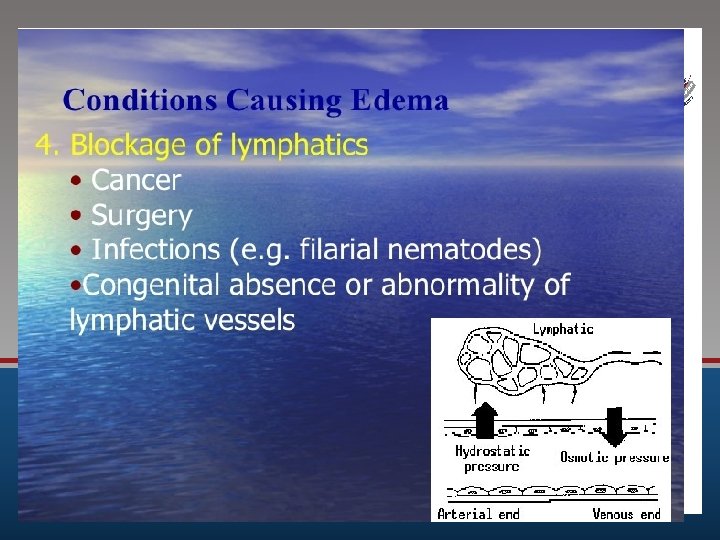
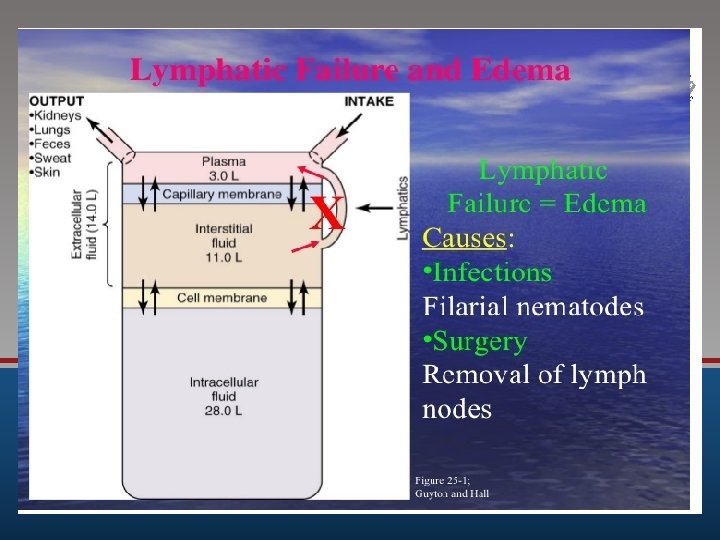
Lymphatic circulation It is a vascular system which returns tissue fluid which cannot return through capillaries because lymphatic capillaries are more permeable than vascular capillaries. It is connected to general circulation through thoracic duct and right lymphatic duct. Very important component of lymph is the protein "Albumin" because it can pass outside capillaries due to its cigar shape, but it does not return through the same pores due to its lower concentration in tissue fluid than in plasma (0. 5 – 1 gm % versus 4. 5 gm %).
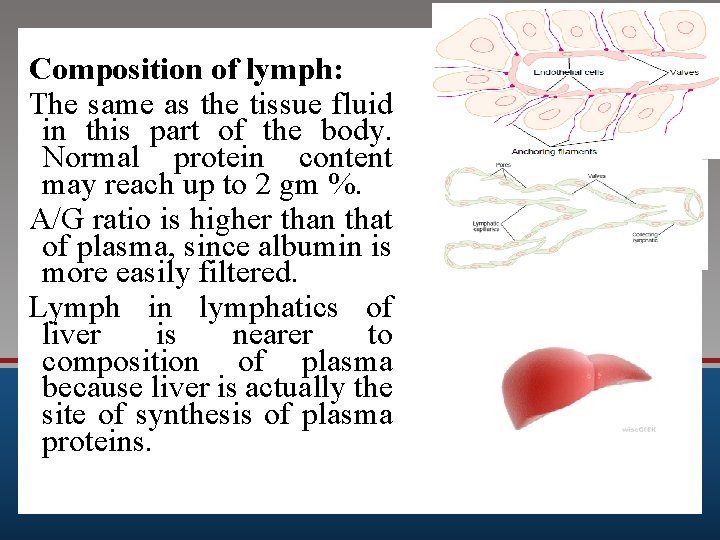
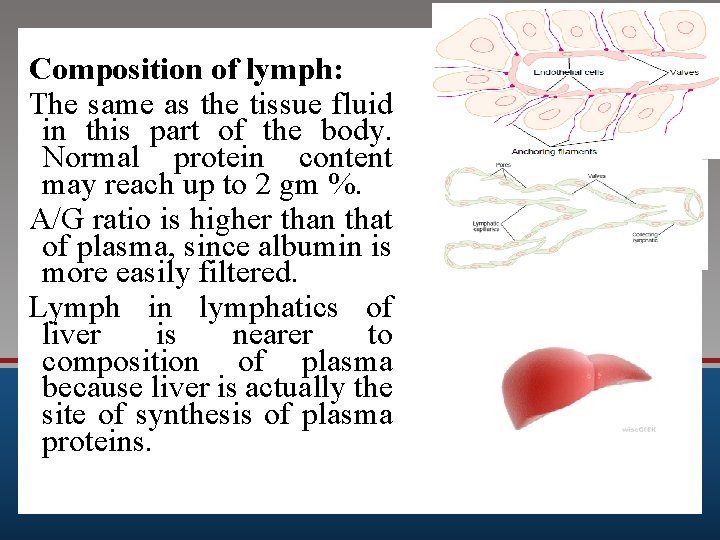
Composition of lymph: The same as the tissue fluid in this part of the body. Normal protein content may reach up to 2 gm %. A/G ratio is higher than that of plasma, since albumin is more easily filtered. Lymph in lymphatics of liver is nearer to composition of plasma because liver is actually the site of synthesis of plasma proteins.
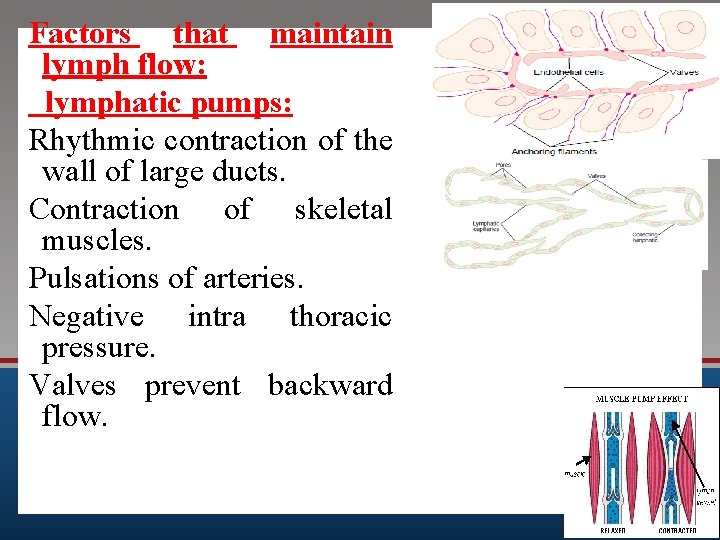
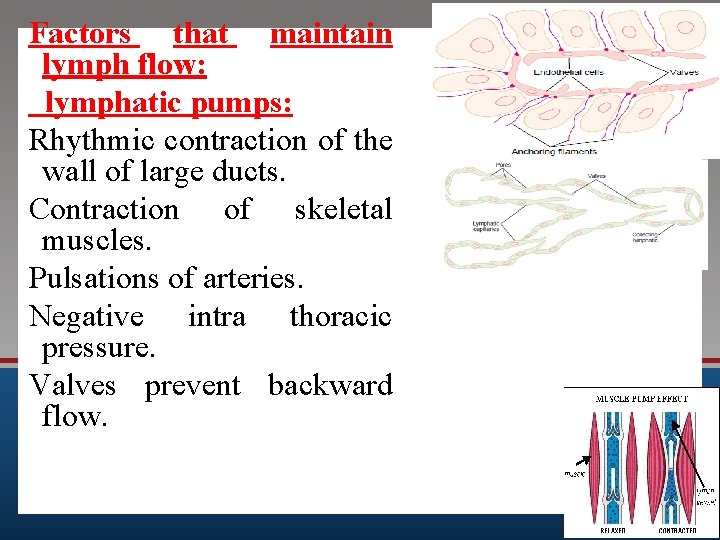
Factors that maintain lymph flow: lymphatic pumps: Rhythmic contraction of the wall of large ducts. Contraction of skeletal muscles. Pulsations of arteries. Negative intra thoracic pressure. Valves prevent backward flow.
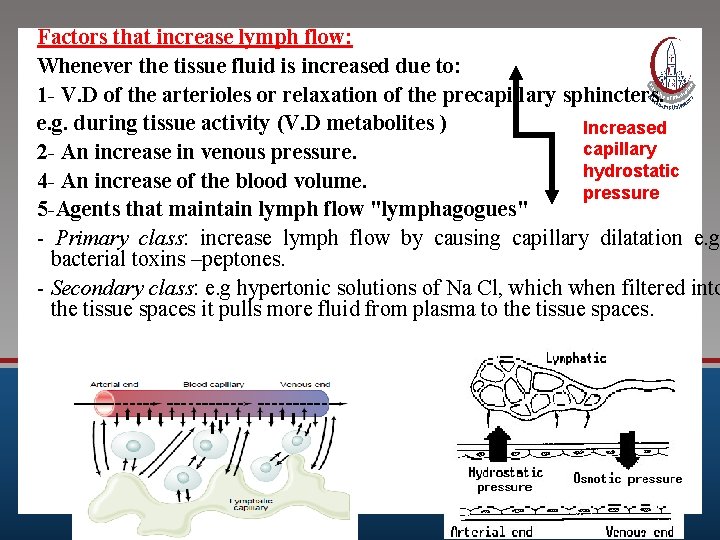
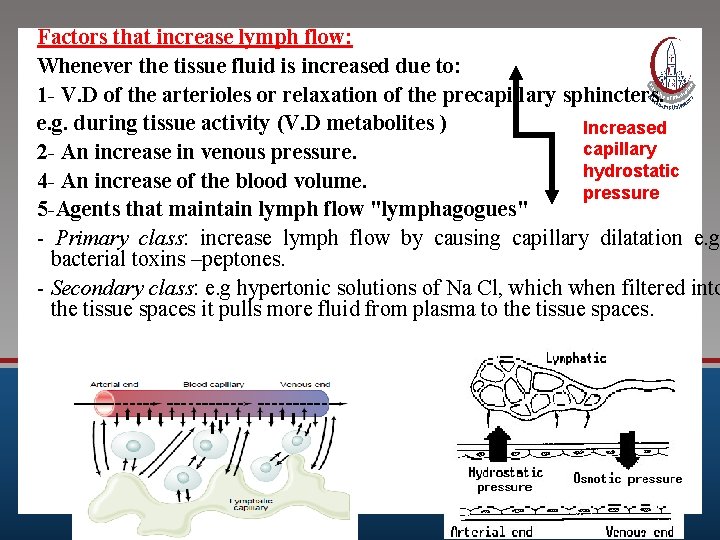
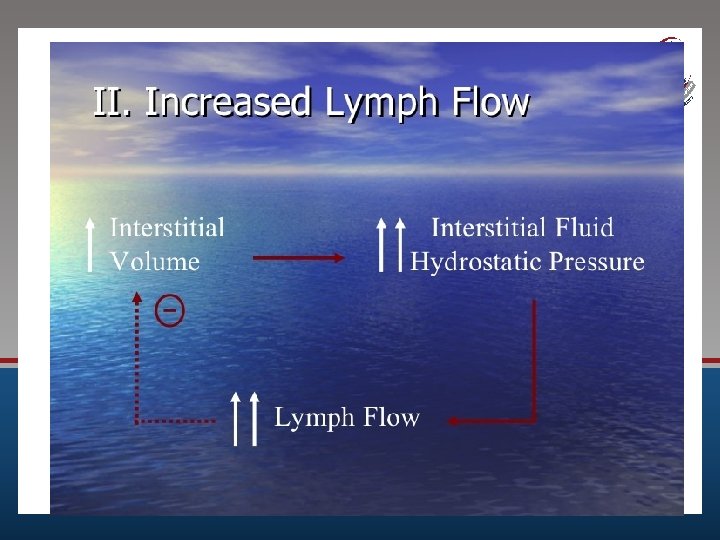
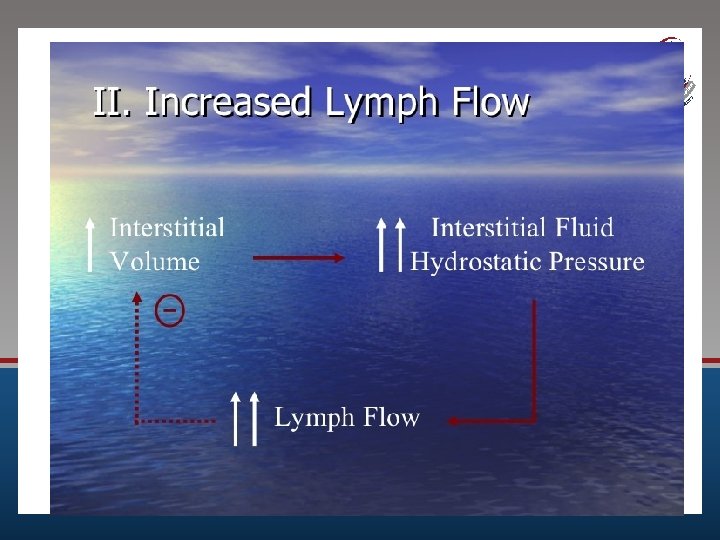
Factors that increase lymph flow: Whenever the tissue fluid is increased due to: 1 - V. D of the arterioles or relaxation of the precapillary sphincters. e. g. during tissue activity (V. D metabolites ) Increased capillary 2 - An increase in venous pressure. hydrostatic 4 - An increase of the blood volume. pressure 5 -Agents that maintain lymph flow "lymphagogues" - Primary class: increase lymph flow by causing capillary dilatation e. g. bacterial toxins –peptones. - Secondary class: e. g hypertonic solutions of Na Cl, which when filtered into the tissue spaces it pulls more fluid from plasma to the tissue spaces.
Clinical application ?
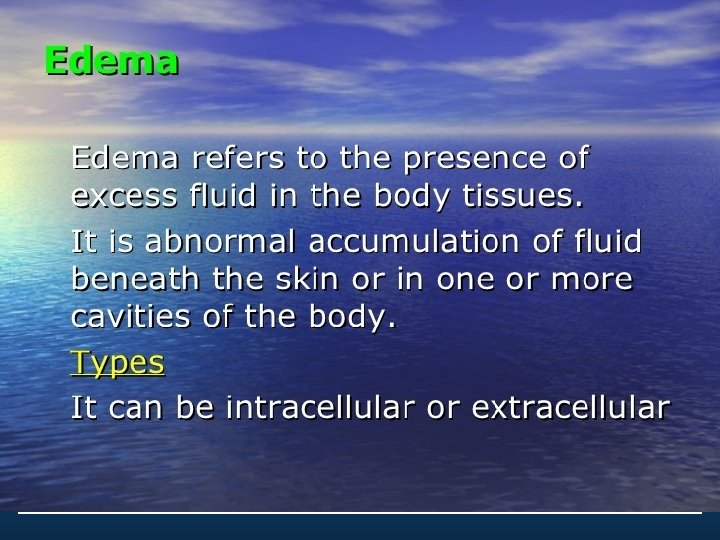
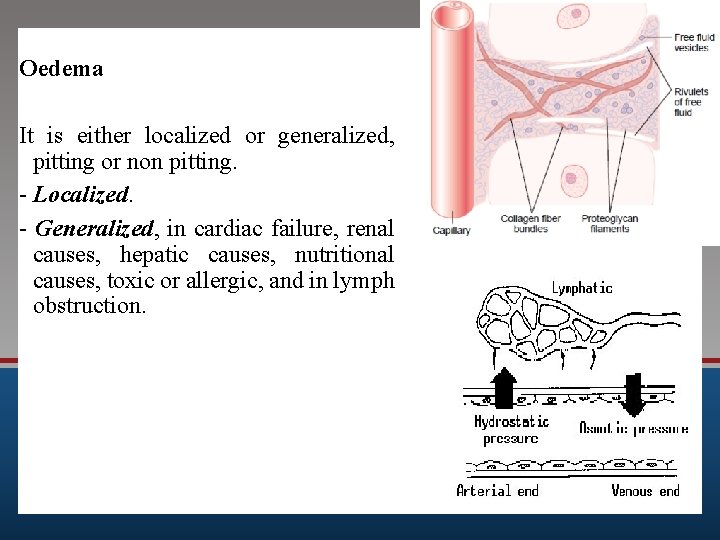
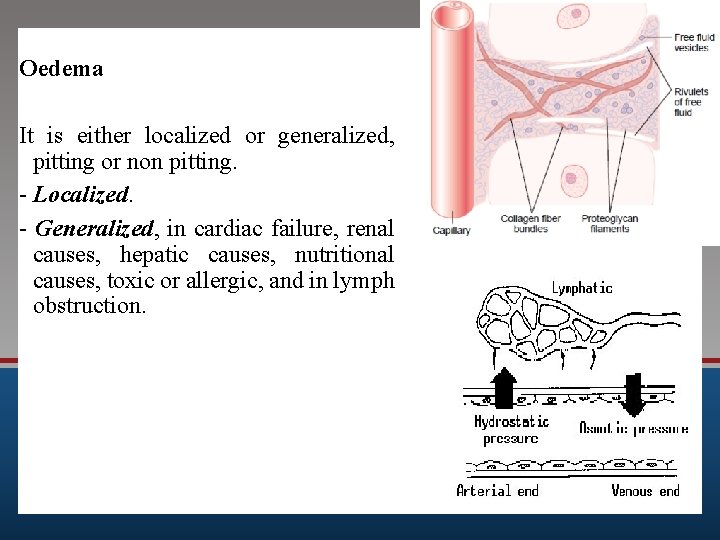
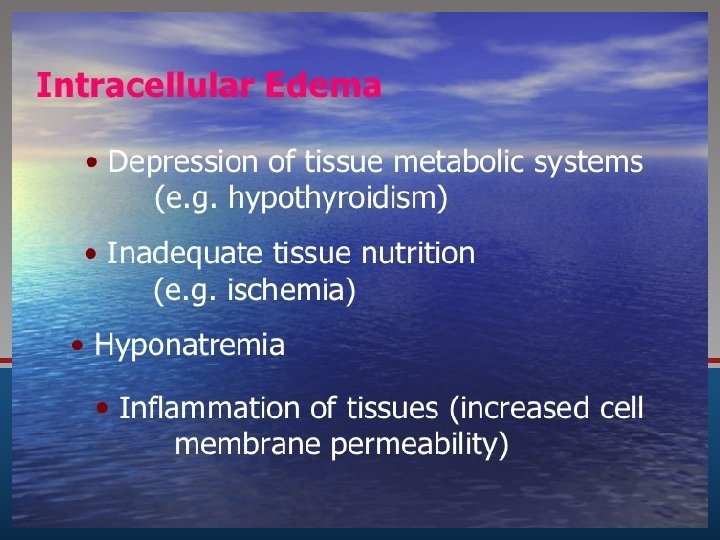
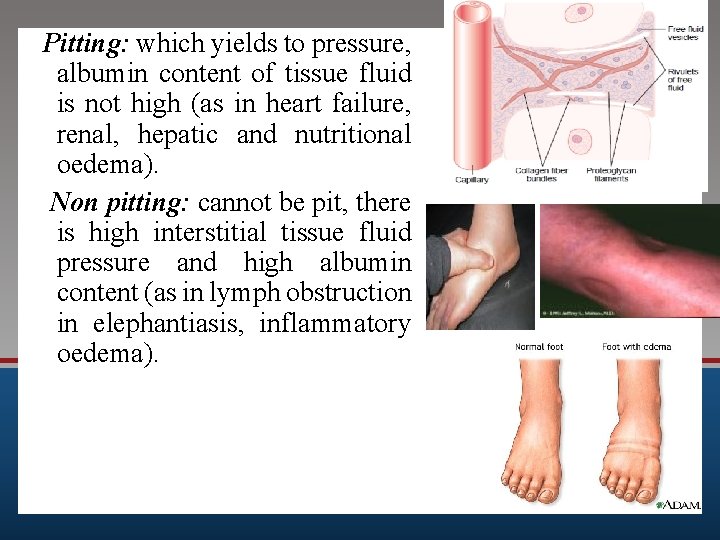
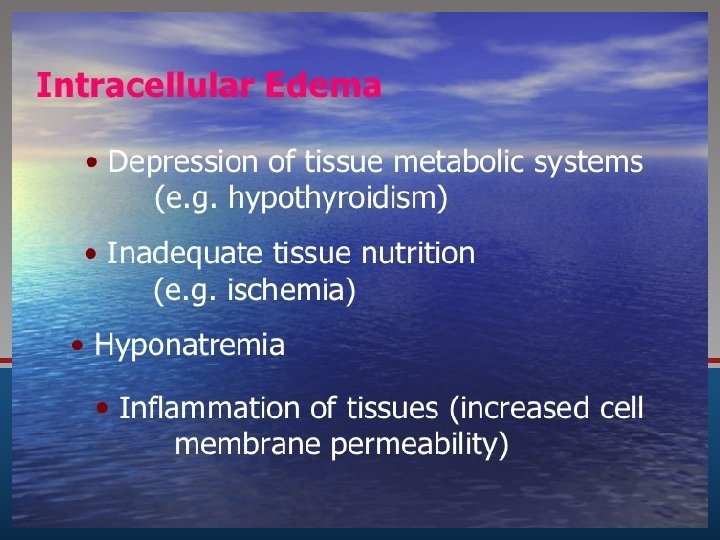
Oedema It is either localized or generalized, pitting or non pitting. - Localized. - Generalized, in cardiac failure, renal causes, hepatic causes, nutritional causes, toxic or allergic, and in lymph obstruction.
Heart failure ? Renal disease ?
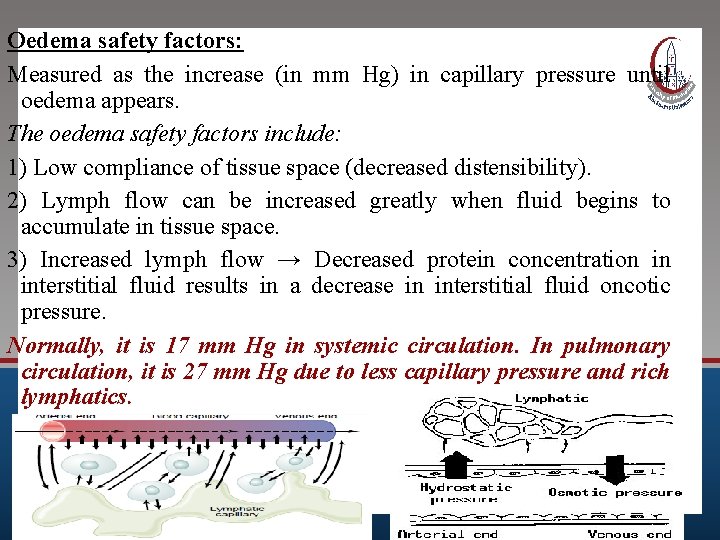
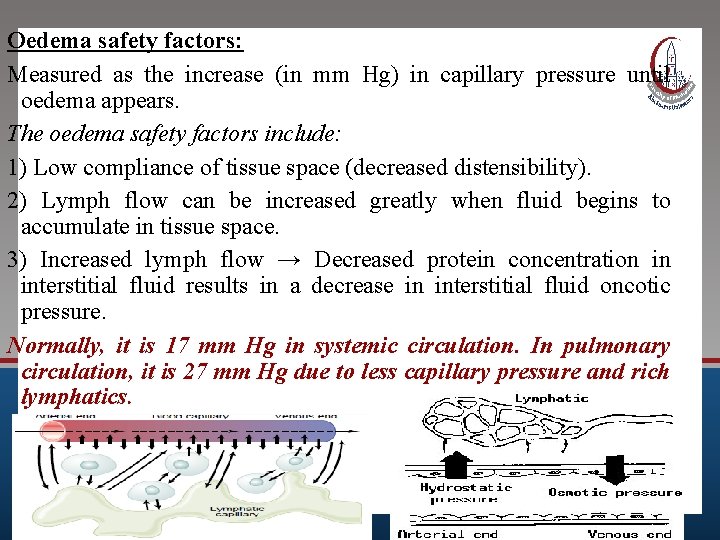
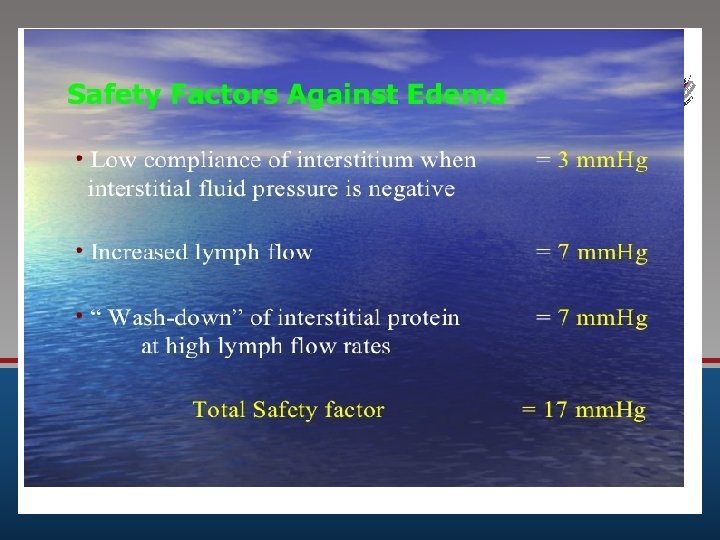
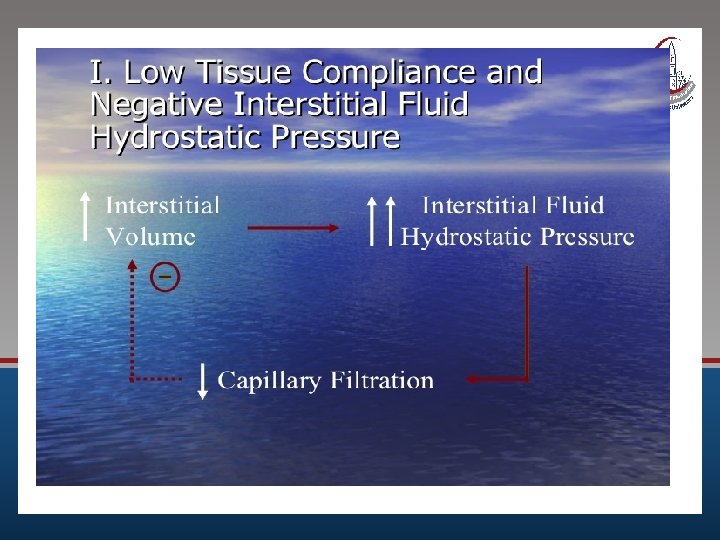
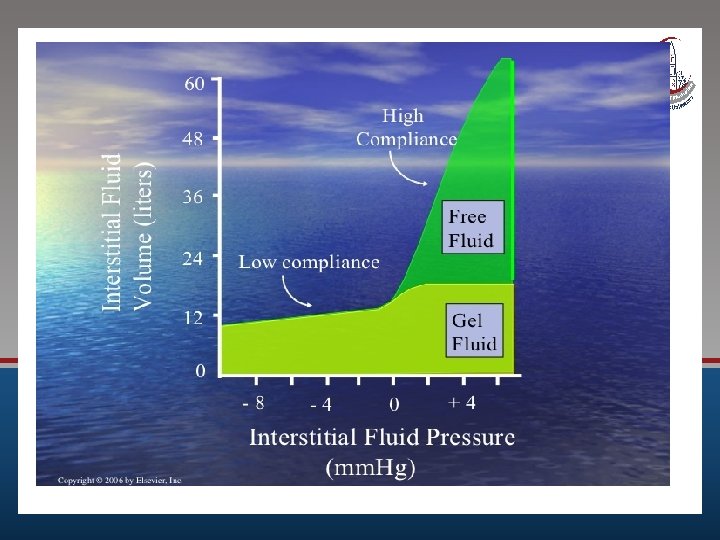
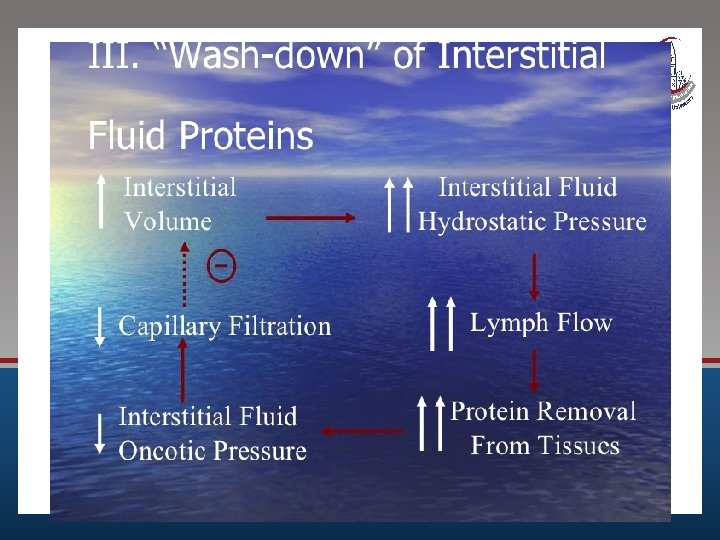
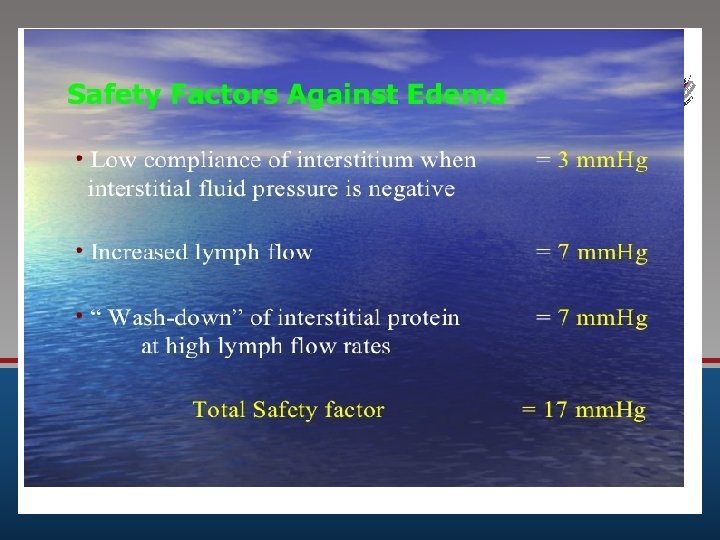
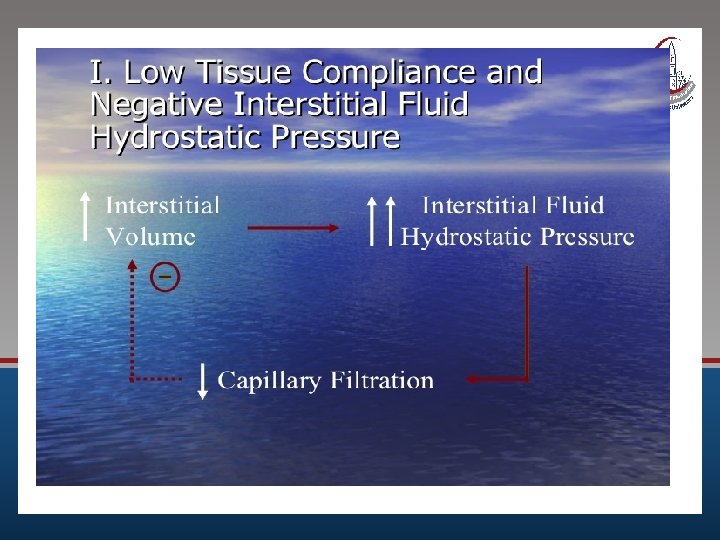
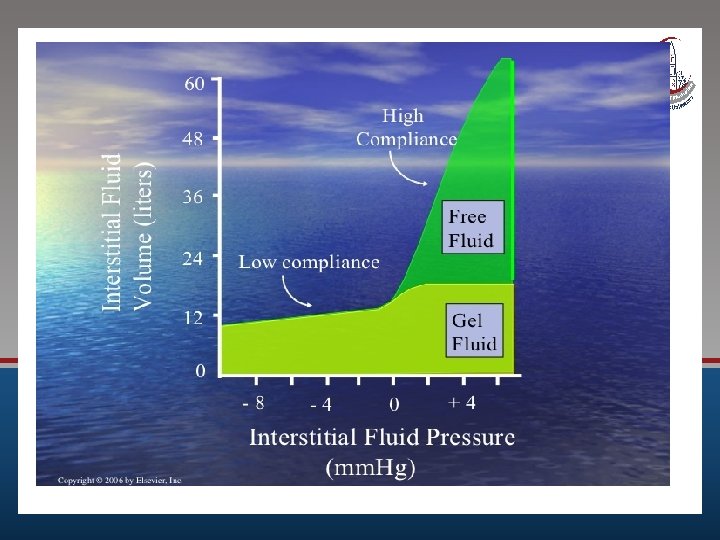
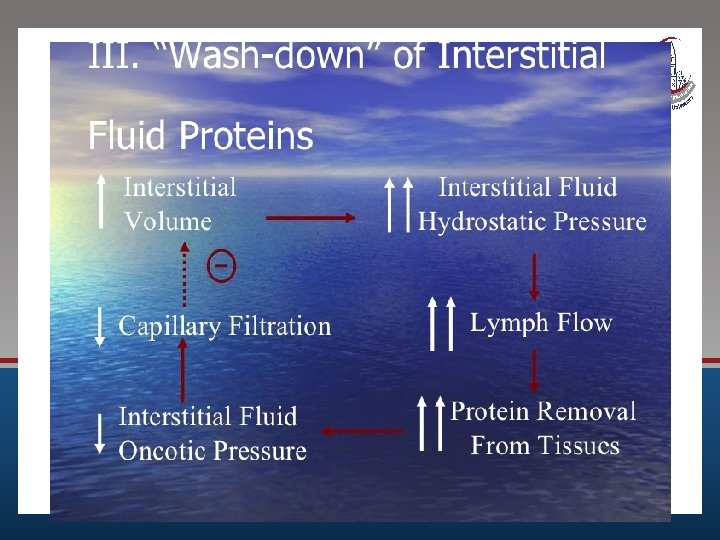
Oedema safety factors: Measured as the increase (in mm Hg) in capillary pressure until oedema appears. The oedema safety factors include: 1) Low compliance of tissue space (decreased distensibility). 2) Lymph flow can be increased greatly when fluid begins to accumulate in tissue space. 3) Increased lymph flow → Decreased protein concentration in interstitial fluid results in a decrease in interstitial fluid oncotic pressure. Normally, it is 17 mm Hg in systemic circulation. In pulmonary circulation, it is 27 mm Hg due to less capillary pressure and rich lymphatics.
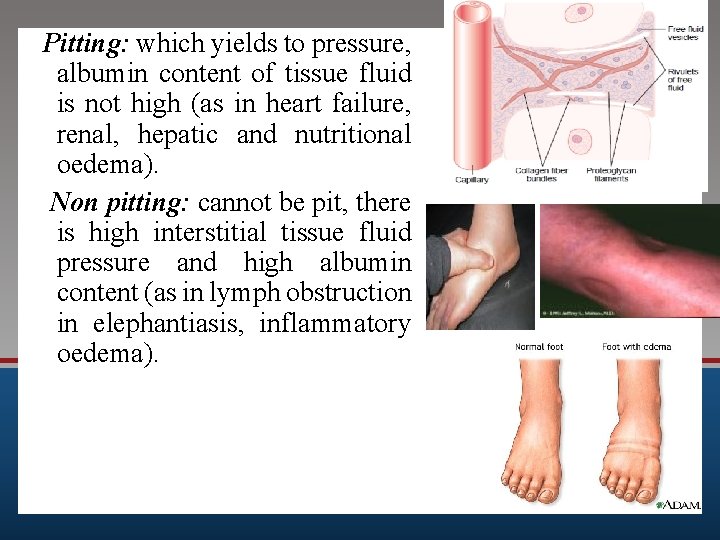
Pitting: which yields to pressure, albumin content of tissue fluid is not high (as in heart failure, renal, hepatic and nutritional oedema). Non pitting: cannot be pit, there is high interstitial tissue fluid pressure and high albumin content (as in lymph obstruction in elephantiasis, inflammatory oedema).

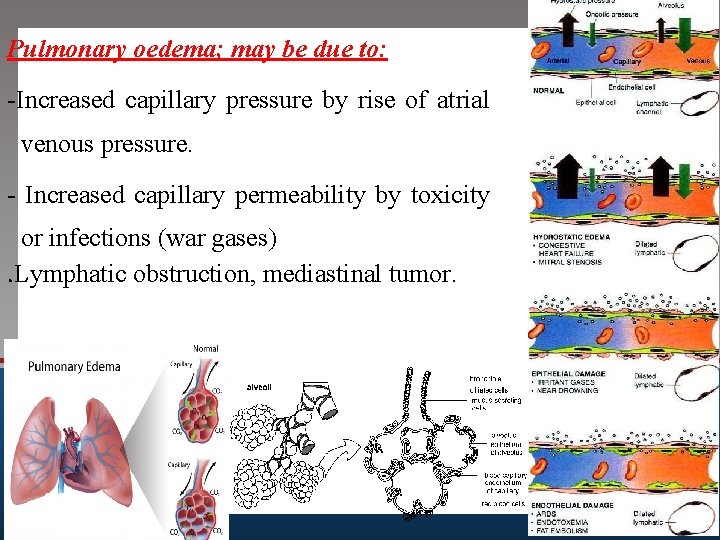
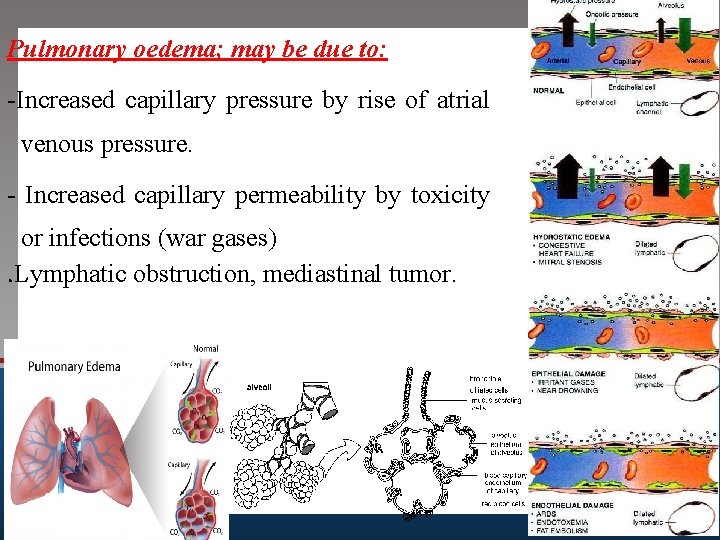
Pulmonary oedema; may be due to: -Increased capillary pressure by rise of atrial venous pressure. - Increased capillary permeability by toxicity or infections (war gases). Lymphatic obstruction, mediastinal tumor.
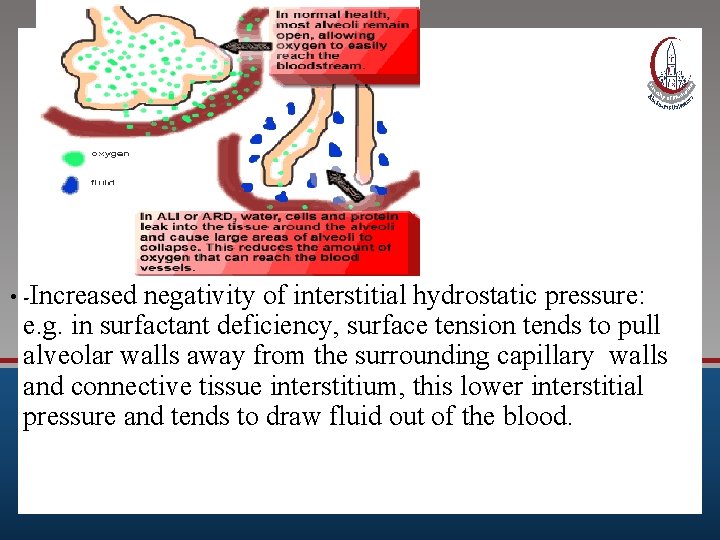
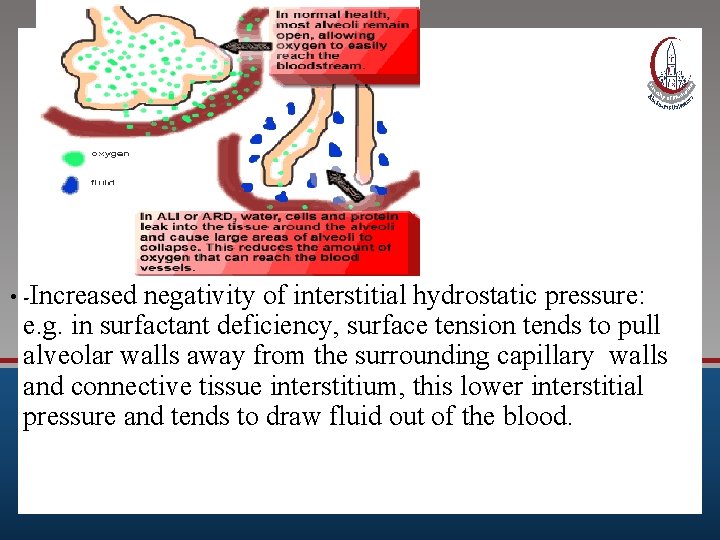
• -Increased negativity of interstitial hydrostatic pressure: e. g. in surfactant deficiency, surface tension tends to pull alveolar walls away from the surrounding capillary walls and connective tissue interstitium, this lower interstitial pressure and tends to draw fluid out of the blood.
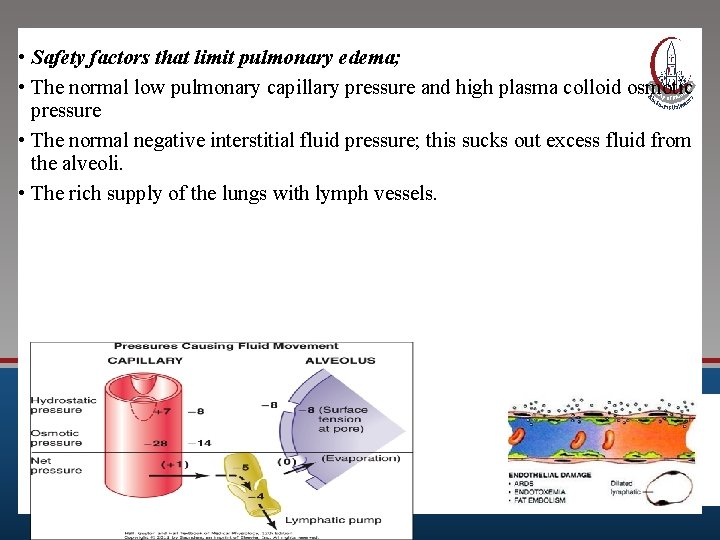
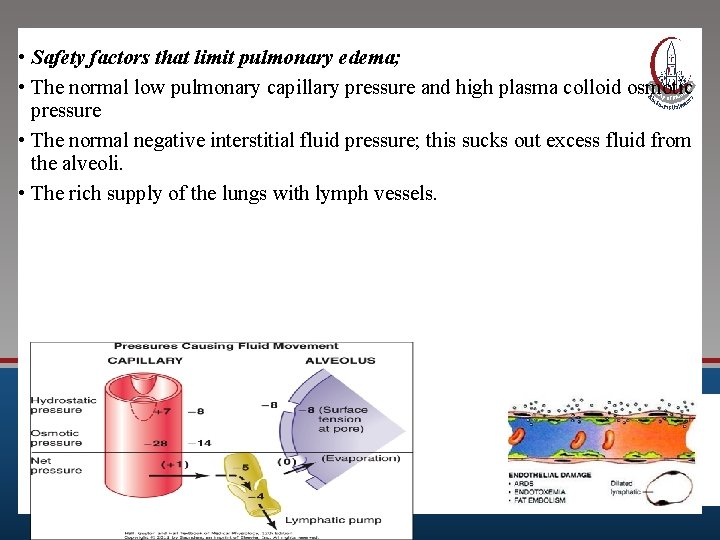
• Safety factors that limit pulmonary edema; • The normal low pulmonary capillary pressure and high plasma colloid osmotic pressure • The normal negative interstitial fluid pressure; this sucks out excess fluid from the alveoli. • The rich supply of the lungs with lymph vessels.
SUGGESTED TEXTBOOKS 1. Ganong’s Review of Medical Physiology. 2. Guyton and Hall; Textbook of Medical Physiology. ) 58