CAPILLARIES MICROCIRCULATION AND LYMPHATIC SYSTEM Capillaries Are smallest
- Slides: 29
CAPILLARIES MICROCIRCULATION AND LYMPHATIC SYSTEM
Capillaries *Are smallest vessels with thin wall *Microscopic capillary networks are highly permeable to all water , cell nutrients and ell excreta between the tissues and circulating blood *Chemicals and gases diffuse across walls
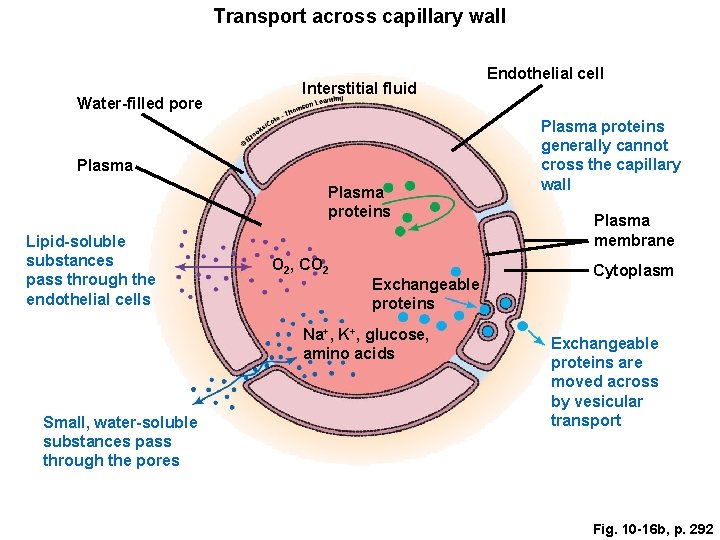
Functions of Capillaries *Permit diffusion of: water small solutes Lipid-soluble materials *Block: blood cells plasma proteins
Capillary Function *it’s the Location of all exchange functions of cardiovascular system *Materials diffuse between blood and interstitial fluid
Capillary Structure - Endothelial tube, inside thin basal lamina - No tunica media - No tunica externa *Diameter is similar to red blood cell
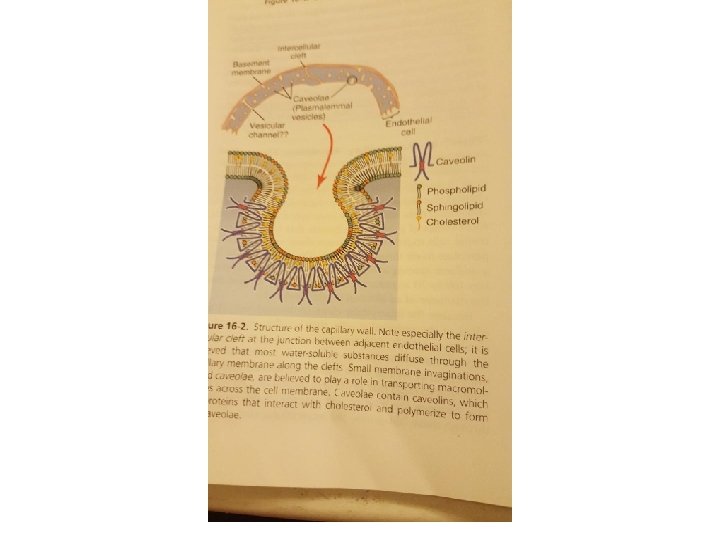
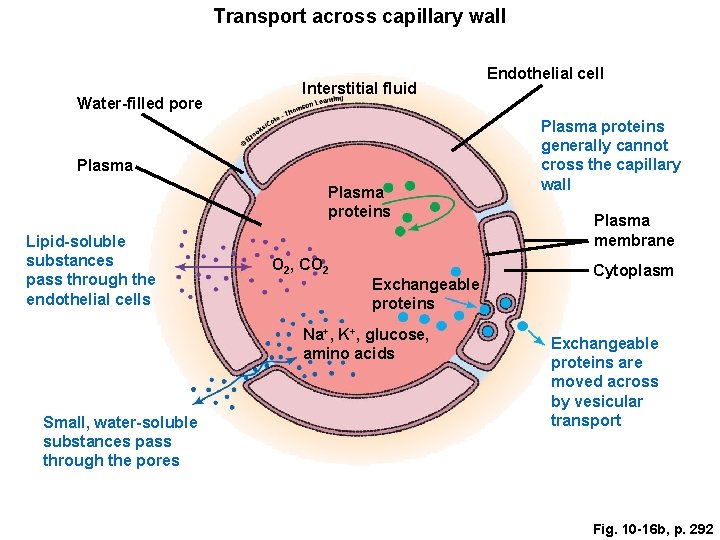
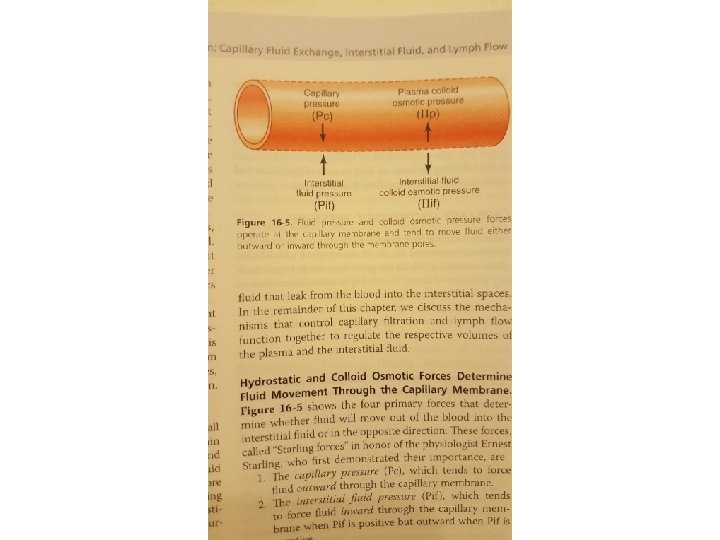
Transport across capillary wall Water-filled pore Interstitial fluid Plasma proteins Lipid-soluble substances pass through the endothelial cells O 2, CO 2 Exchangeable proteins Na+, K+, glucose, amino acids Small, water-soluble substances pass through the pores Endothelial cell Plasma proteins generally cannot cross the capillary wall Plasma membrane Cytoplasm Exchangeable proteins are moved across by vesicular transport Fig. 10 -16 b, p. 292
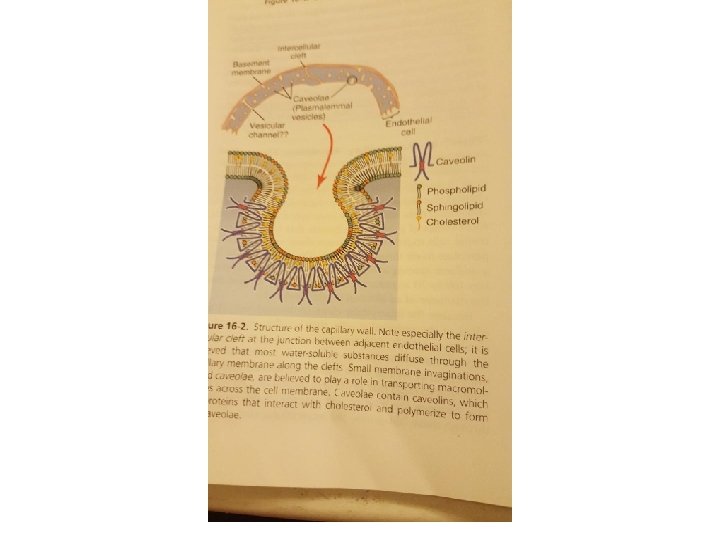
Capillary structure Capillary pores (Intercellular cleft) Plasmalemmal vesicles Vesicular channels
Special types of (pores) in certain organs 1. Brain , blood brain barriers tight junction 2. Liver very wide 3. GI capillaries, midway in size between muscles and liver 4. Glomerular capillaries of the kidney, Fenestrate ; small oval windows penetrate through middle of endothelial cells
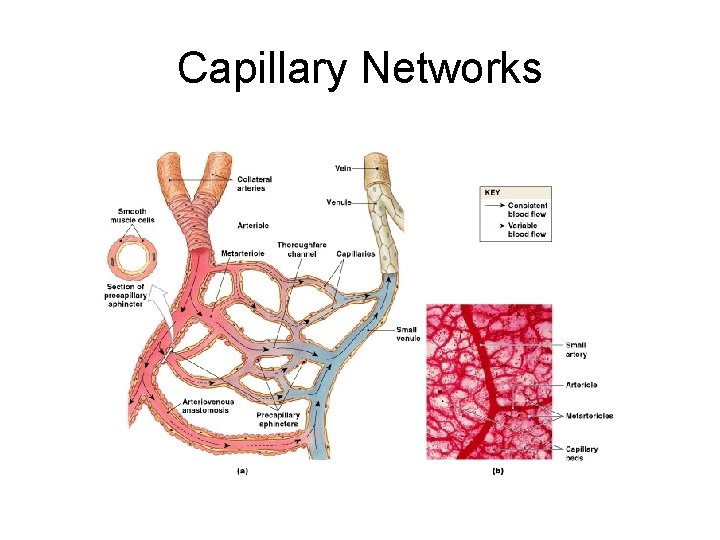
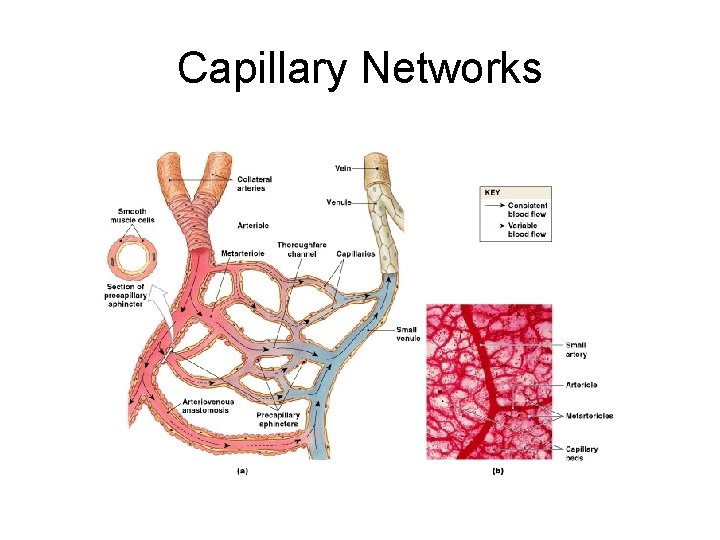
Capillary Networks Figure 21 -5
Capillaries Networks Capillary bed or capillary plexus Connect 1 arteriole and 1 venule
Collaterals *Multiple arteries that contribute to 1 capillary bed *Allow circulation if 1 artery is blocked Arterial anastomosis: => fusion of 2 collateral arteries
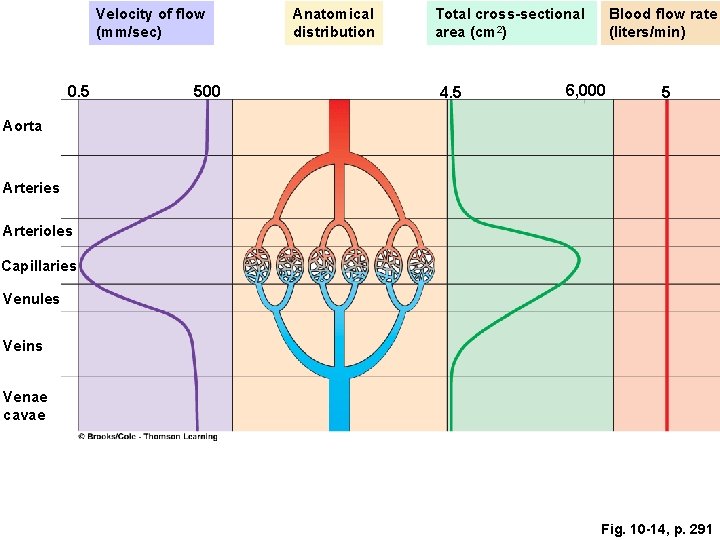
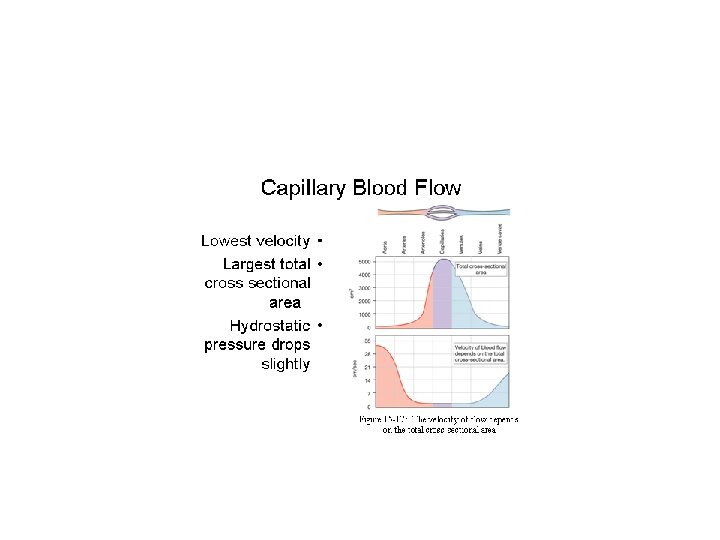
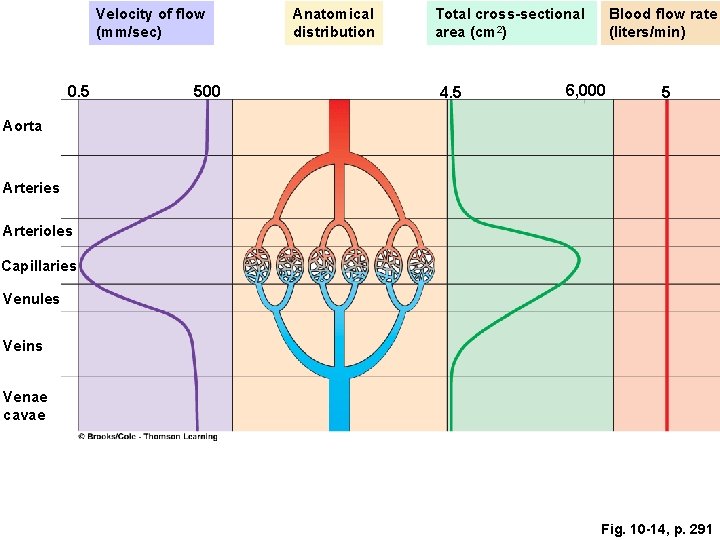
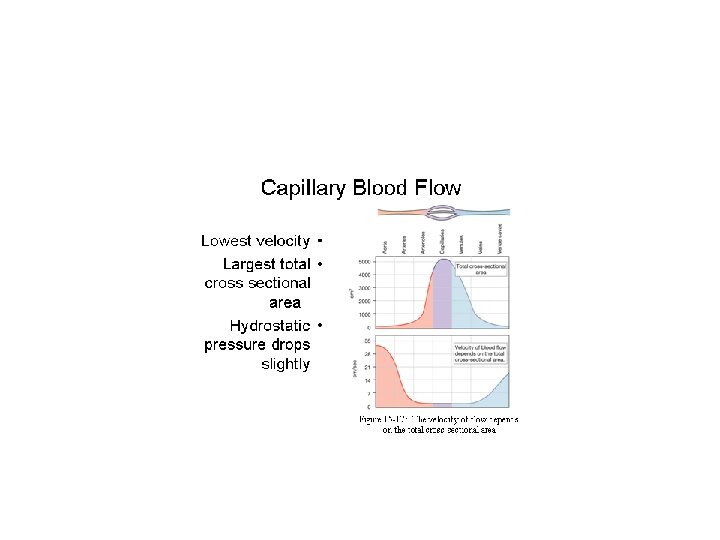
Velocity of flow (mm/sec) 0. 5 500 Anatomical distribution Total cross-sectional area (cm 2) 4. 5 Blood flow rate (liters/min) 6, 000 5 Aorta Arteries Arterioles Capillaries Venules Veins Venae cavae Fig. 10 -14, p. 291
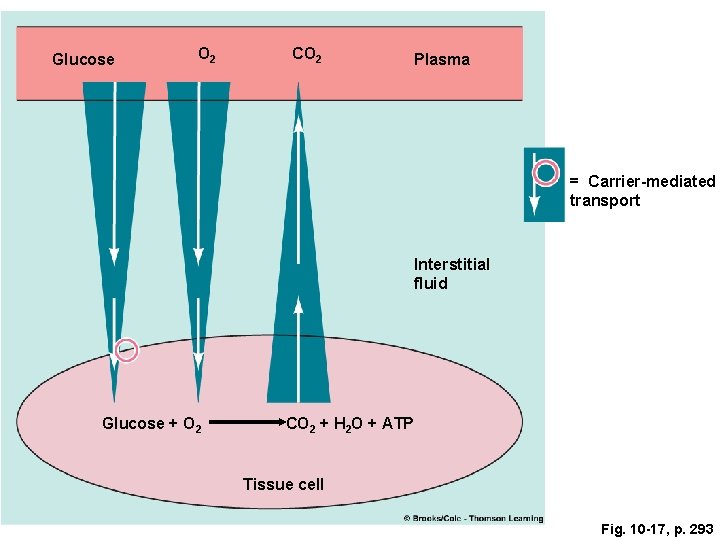
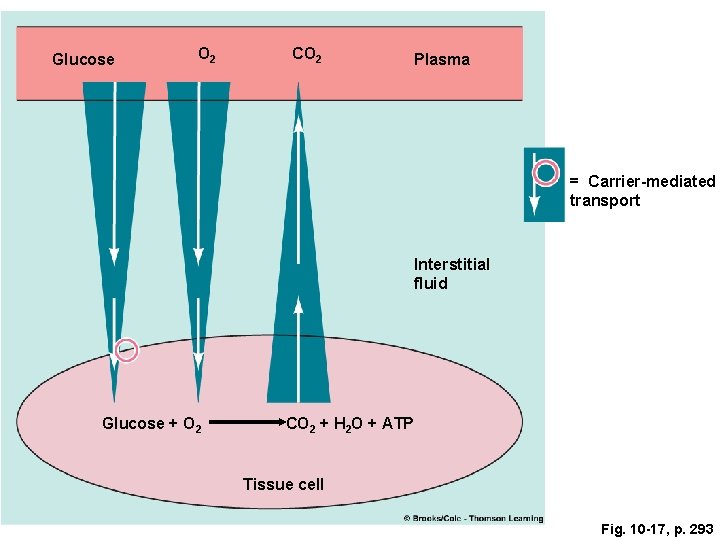
Glucose O 2 CO 2 Plasma = Carrier-mediated transport Interstitial fluid Glucose + O 2 CO 2 + H 2 O + ATP Tissue cell Fig. 10 -17, p. 293
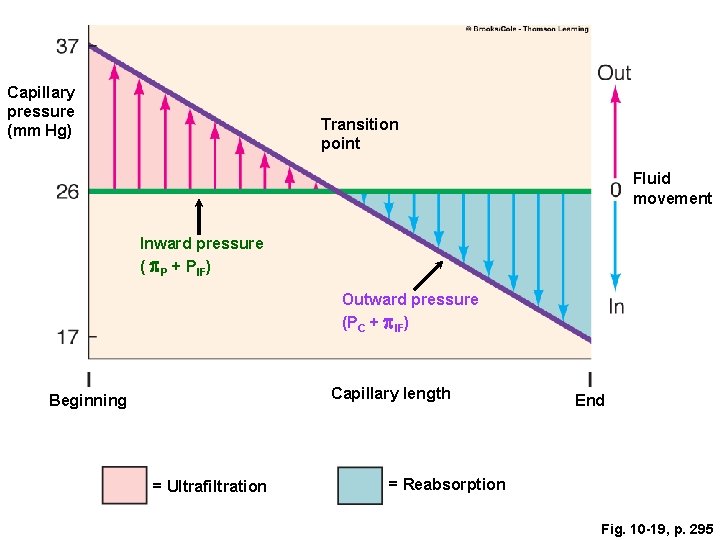
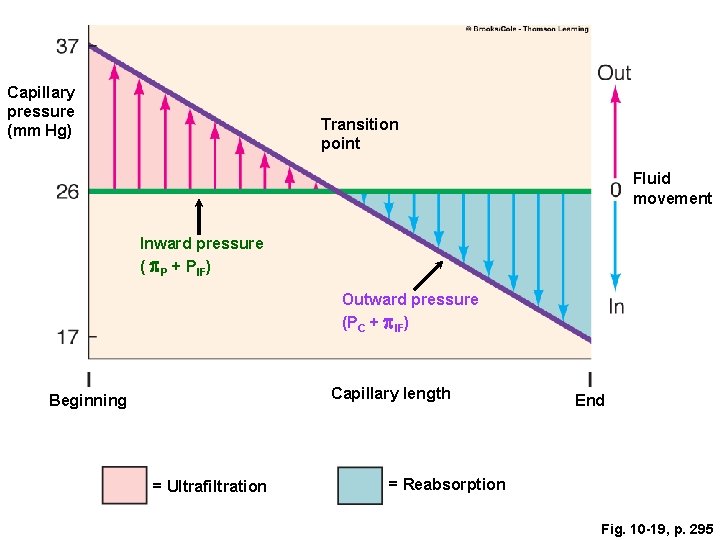
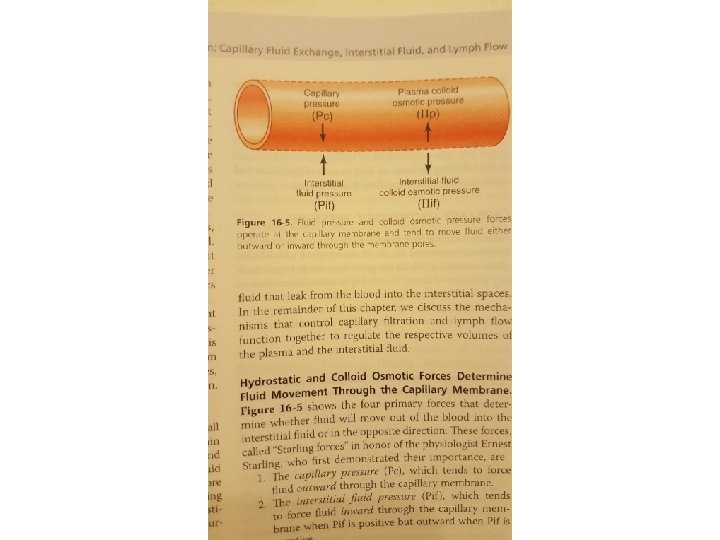
Capillary pressure (mm Hg) Transition point Fluid movement Inward pressure ( p. P + PIF) Outward pressure (PC + p. IF) Capillary length Beginning = Ultrafiltration End = Reabsorption Fig. 10 -19, p. 295
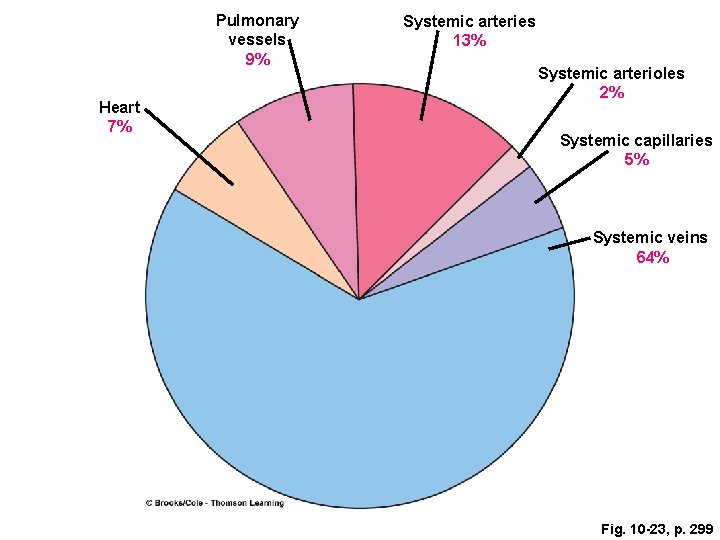
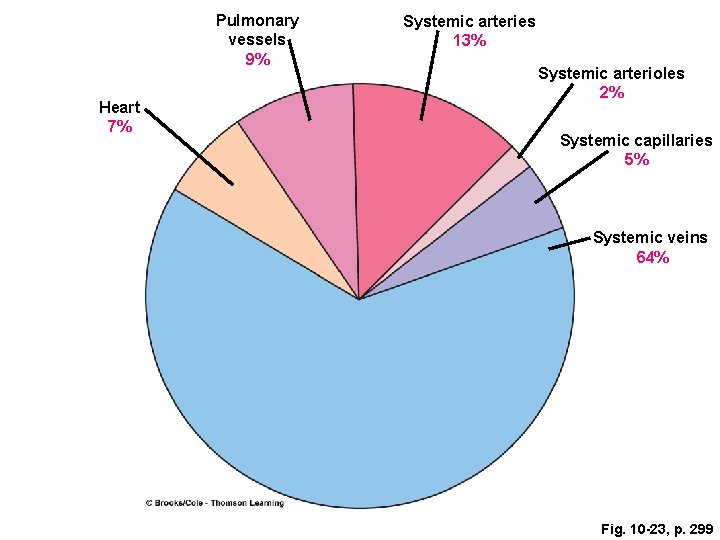
Pulmonary vessels 9% Heart 7% Systemic arteries 13% Systemic arterioles 2% Systemic capillaries 5% Systemic veins 64% Fig. 10 -23, p. 299
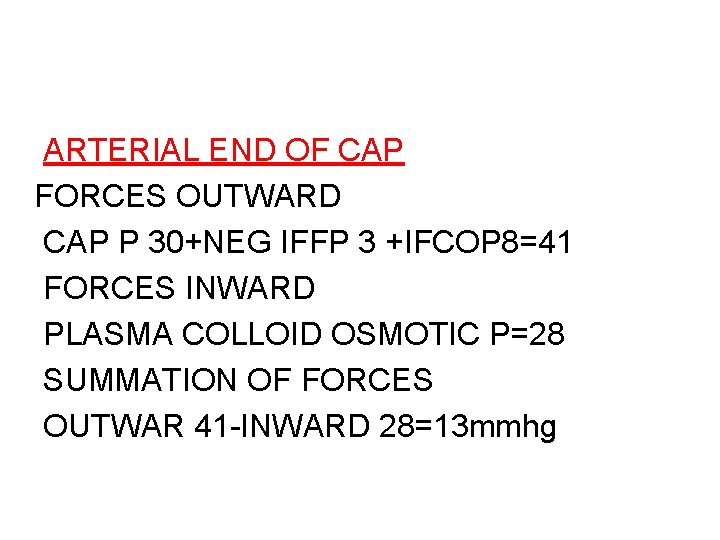
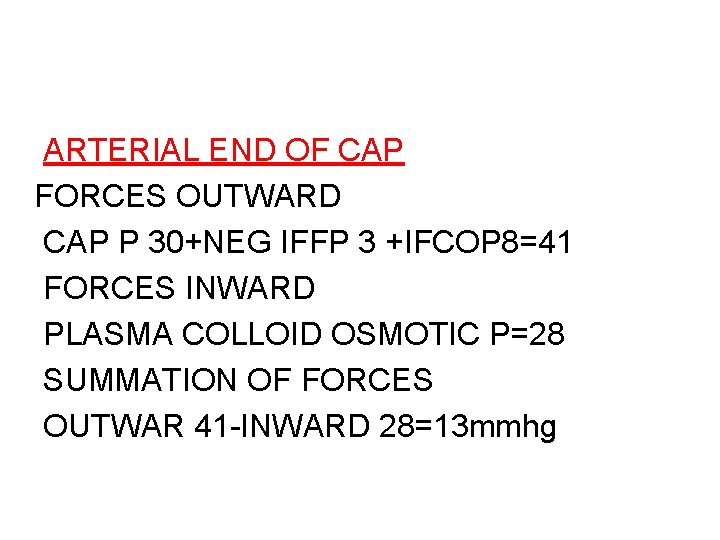
ARTERIAL END OF CAP FORCES OUTWARD CAP P 30+NEG IFFP 3 +IFCOP 8=41 FORCES INWARD PLASMA COLLOID OSMOTIC P=28 SUMMATION OF FORCES OUTWAR 41 -INWARD 28=13 mmhg
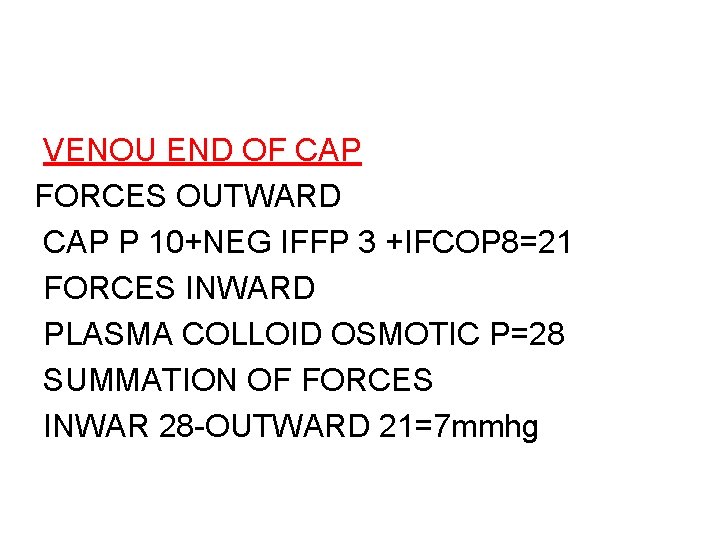
VENOU END OF CAP FORCES OUTWARD CAP P 10+NEG IFFP 3 +IFCOP 8=21 FORCES INWARD PLASMA COLLOID OSMOTIC P=28 SUMMATION OF FORCES INWAR 28 -OUTWARD 21=7 mmhg
STARLING EQUILIBRIUM FOR CAPILLARY PRESSURE OUTWAD FORCES MEAN CAP P=17. 3 NEG IFFP=3 IFCOP=8 TOTAL=28. 3 mmhg INWARD FORCES PLASMA COLL OSM PRES=28 mmhg RESULT(OUTWARD 28. 3 -INWARD 28=0. 3
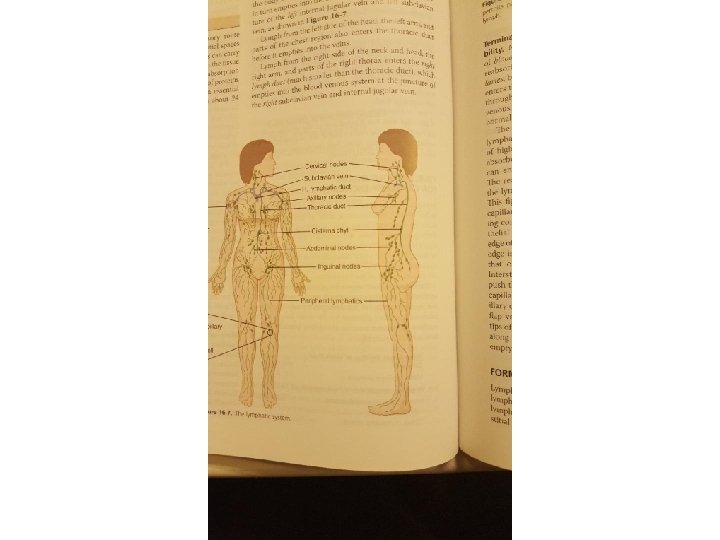
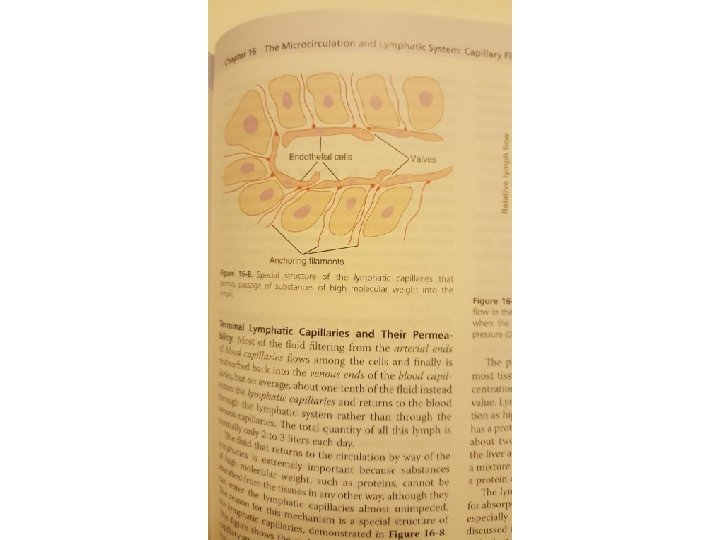
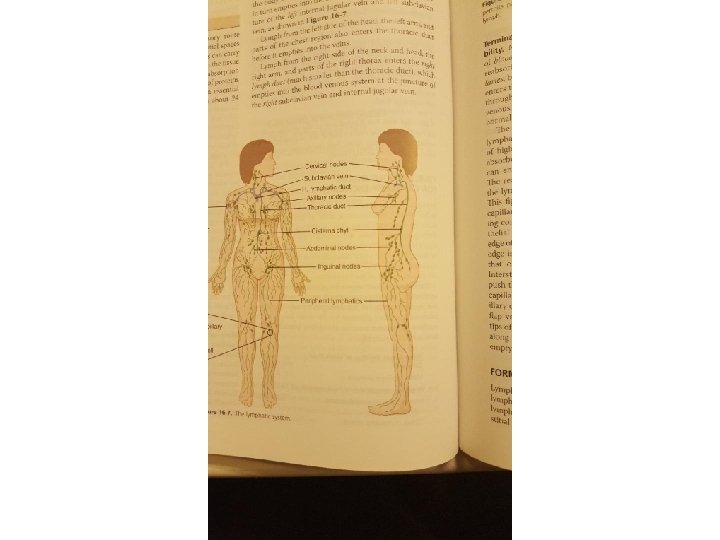
LYMPHATIC CIRCULATION 1 -LYMPHATIC STRUCTURE 2 -FACTORS DETERMINE LYMPHATIC FLOW A. LYMPHATIC PUMP B. INTERSTIAL FLUID PRESSURE
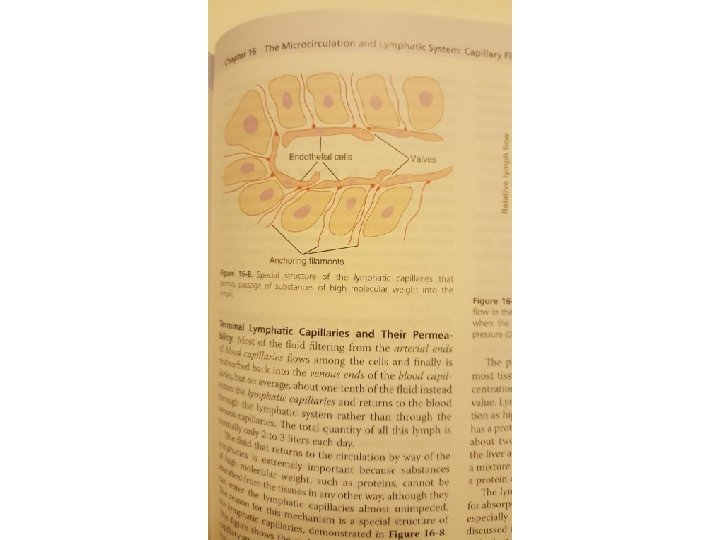
LYMPHATIC FUNCTION CONTROLL INTERSTIALFLUID 1. PROTEIN CONCENTRATION 2. VOLUME 3. PRESSURE
Lymph flow 1. Interstial fluid pressure A. Elevate capillary pressure B. Increase interstitial fluid colloid osmotic pressure C. Decrease plasma colloid osmotic pressure D. Increase permeability of capillaries
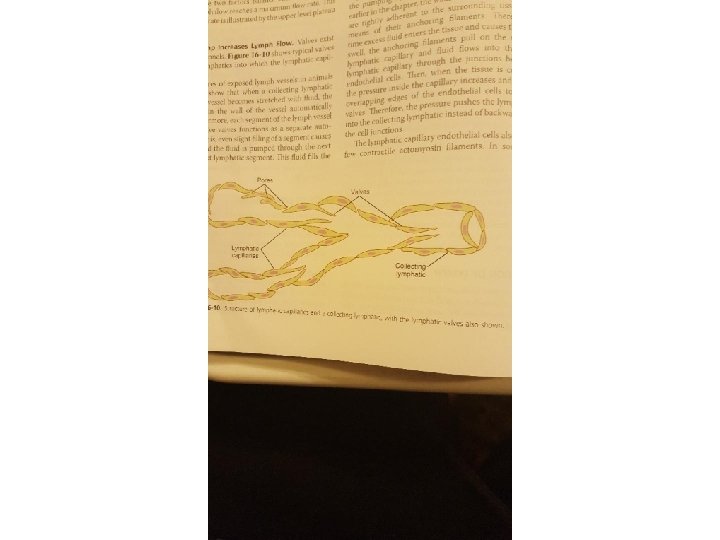
2. Lymph pump and valves 3. External compression A. Surrounding skeletal muscles B. Movements of parts of the body C. Pulsation of arteries D. Compression of the tissues by objects outside the body
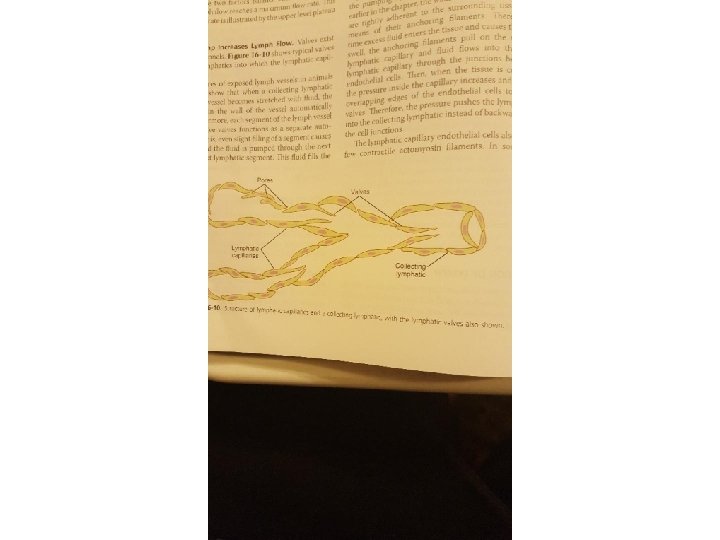
Lymphatic capillary pump. 4