CAPD guide line n n n VS CAPD














- Slides: 49
CAPD guide line n n n VS 施孟甫 醫師 CAPD麗華 CR 蔡智生 醫師
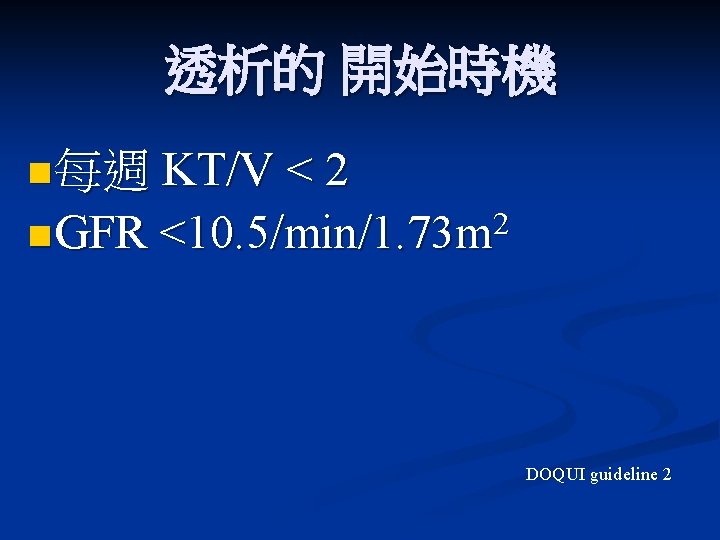
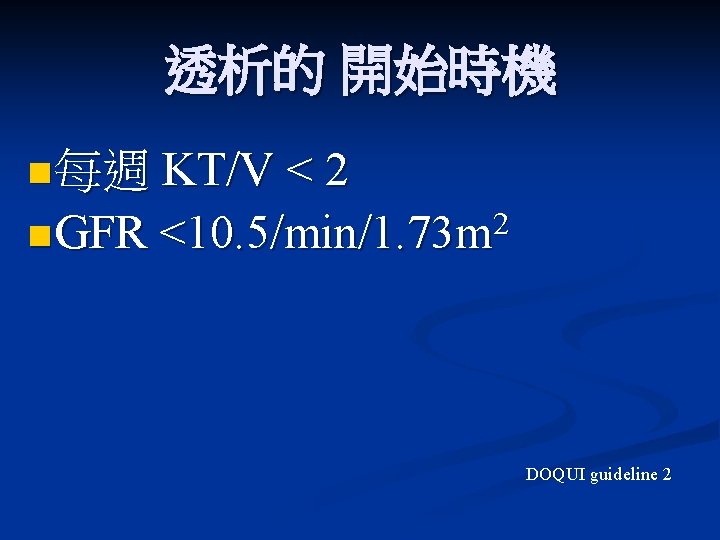
透析的 開始時機 n 每週 KT/V < 2 n GFR 2 <10. 5/min/1. 73 m DOQUI guideline 2
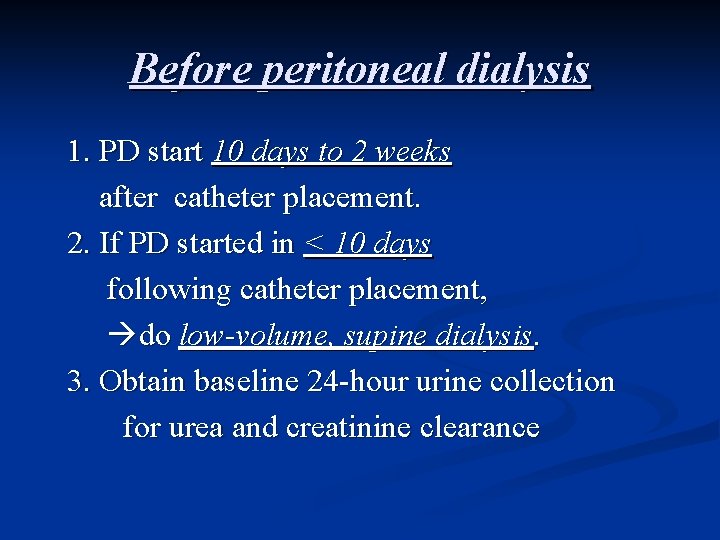
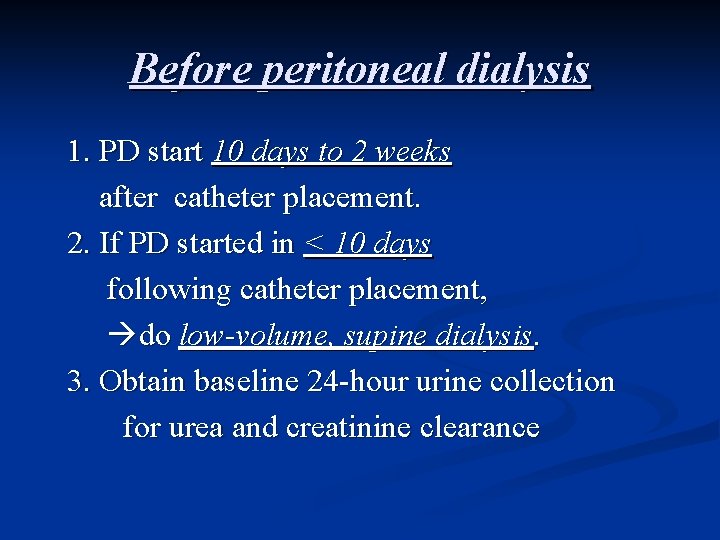
Before peritoneal dialysis 1. PD start 10 days to 2 weeks after catheter placement. 2. If PD started in < 10 days following catheter placement, do low-volume, supine dialysis. 3. Obtain baseline 24 -hour urine collection for urea and creatinine clearance
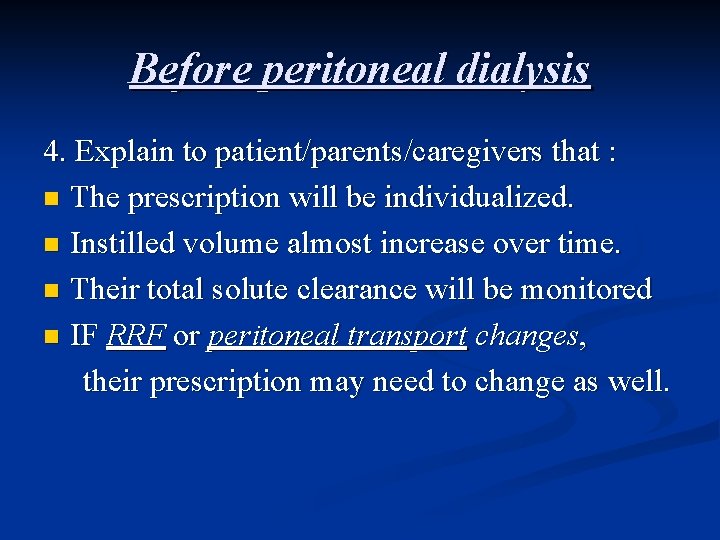
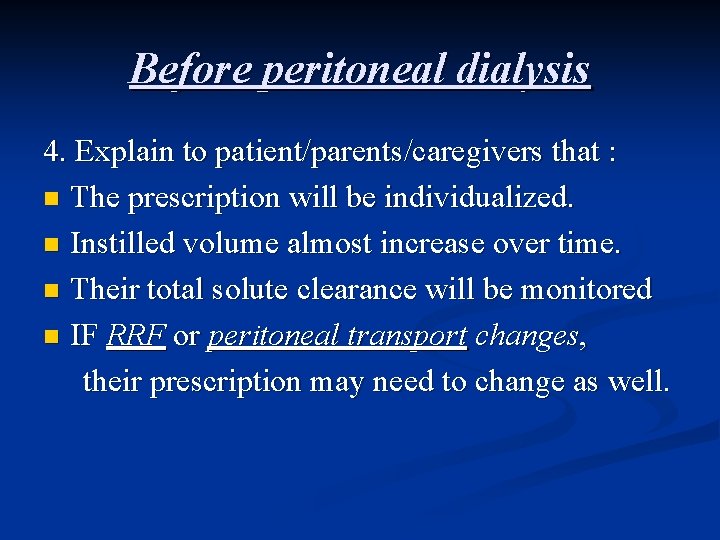
Before peritoneal dialysis 4. Explain to patient/parents/caregivers that : n The prescription will be individualized. n Instilled volume almost increase over time. n Their total solute clearance will be monitored n IF RRF or peritoneal transport changes, their prescription may need to change as well.
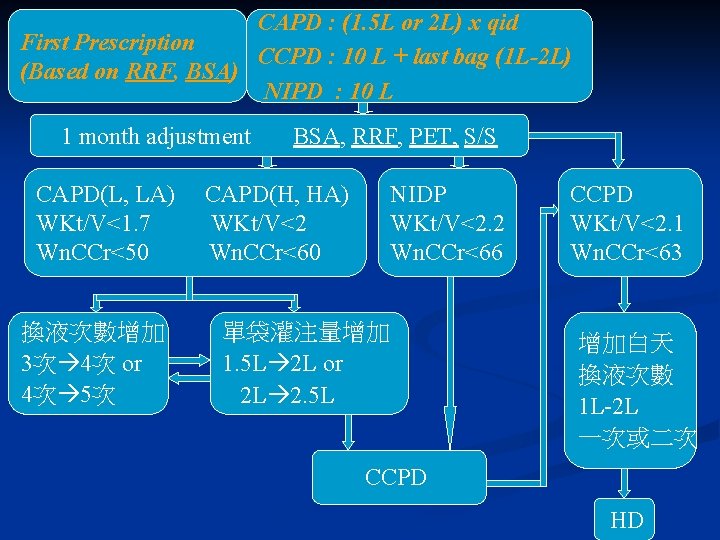
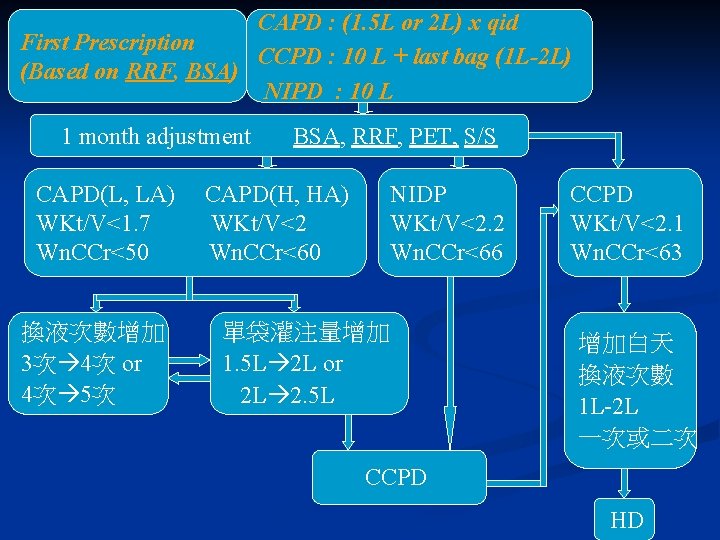
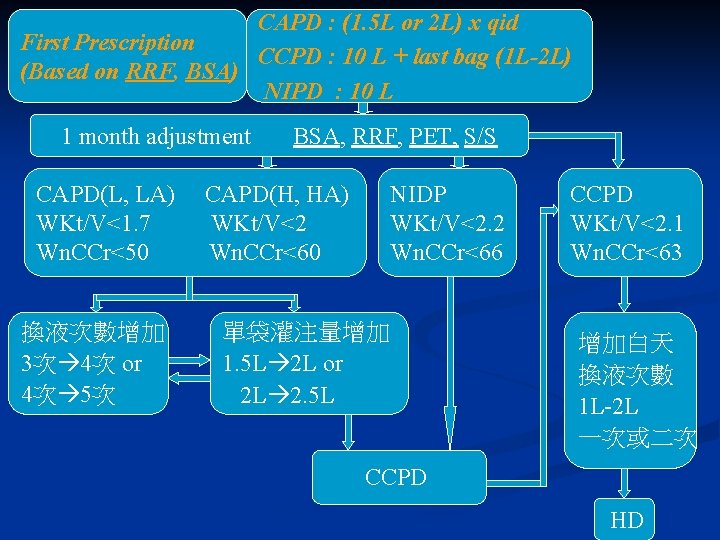
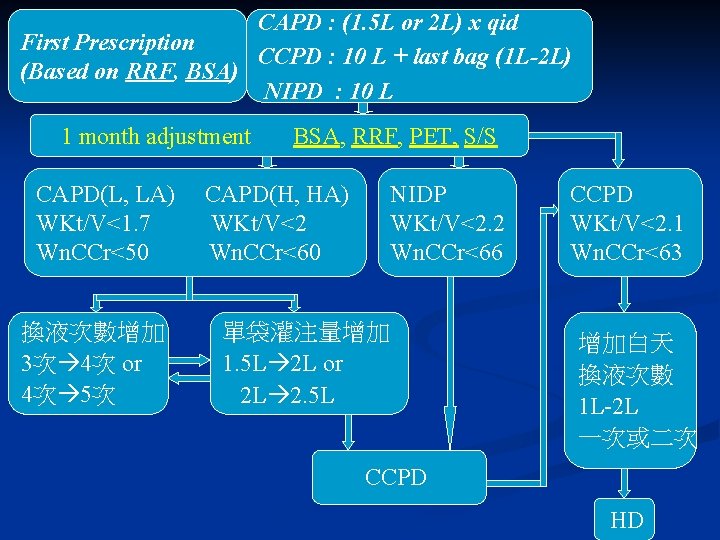
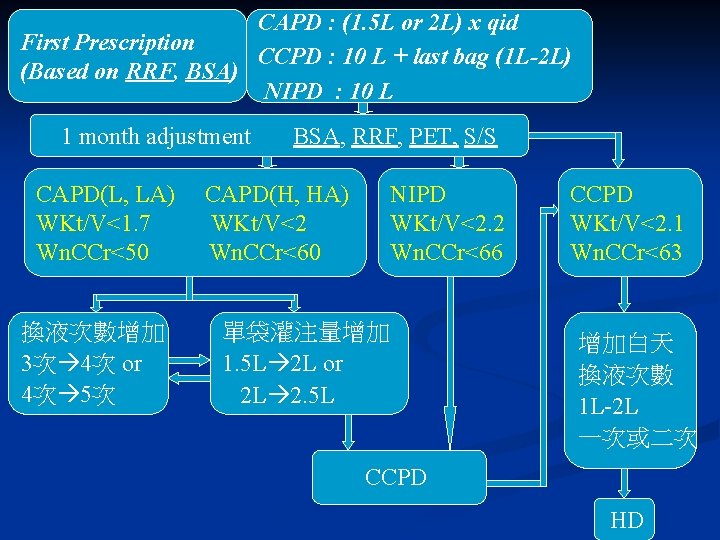
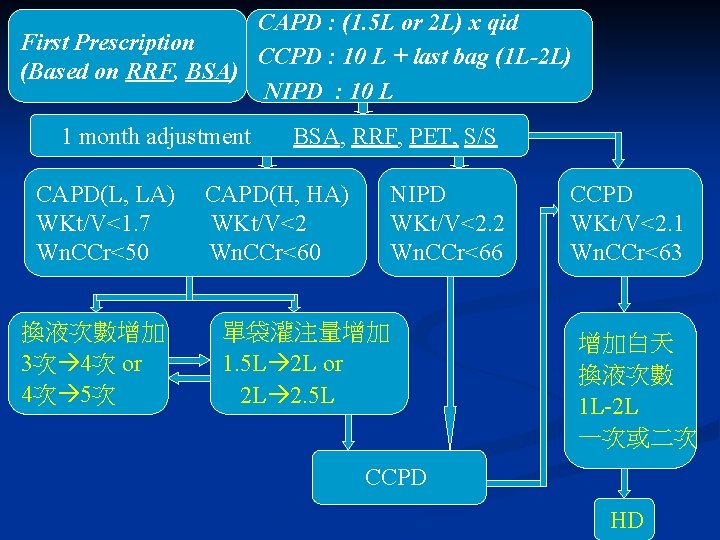
CAPD : (1. 5 L or 2 L) x qid First Prescription CCPD : 10 L + last bag (1 L-2 L) (Based on RRF, BSA) NIPD : 10 L 1 month adjustment CAPD(L, LA) WKt/V<1. 7 Wn. CCr<50 換液次數增加 3次 4次 or 4次 5次 BSA, RRF, PET, S/S CAPD(H, HA) WKt/V<2 Wn. CCr<60 NIDP WKt/V<2. 2 Wn. CCr<66 單袋灌注量增加 1. 5 L 2 L or 2 L 2. 5 L CCPD WKt/V<2. 1 Wn. CCr<63 增加白天 換液次數 1 L-2 L 一次或二次 CCPD HD
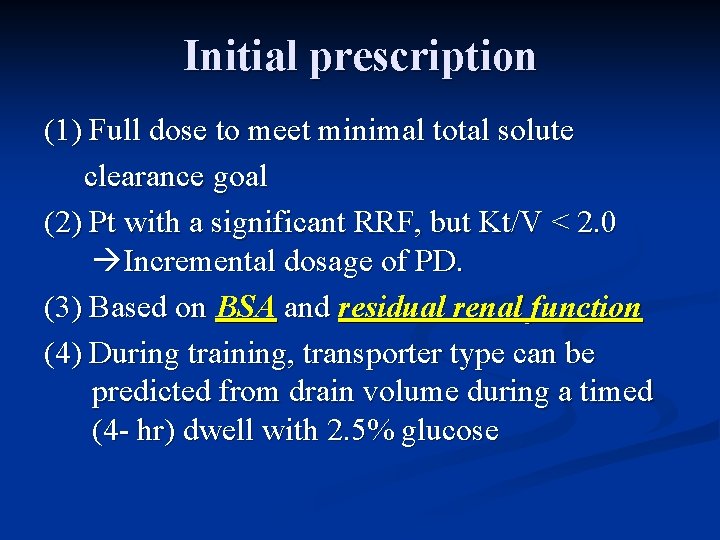
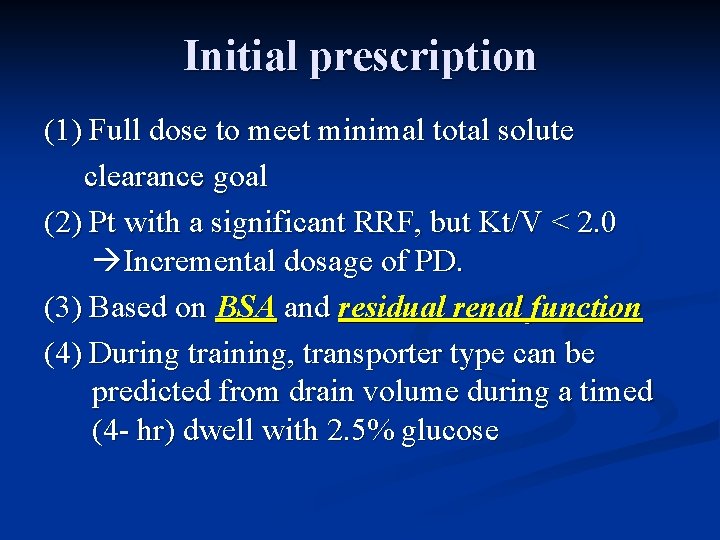
Initial prescription (1) Full dose to meet minimal total solute clearance goal (2) Pt with a significant RRF, but Kt/V < 2. 0 Incremental dosage of PD. (3) Based on BSA and residual renal function (4) During training, transporter type can be predicted from drain volume during a timed (4 - hr) dwell with 2. 5% glucose
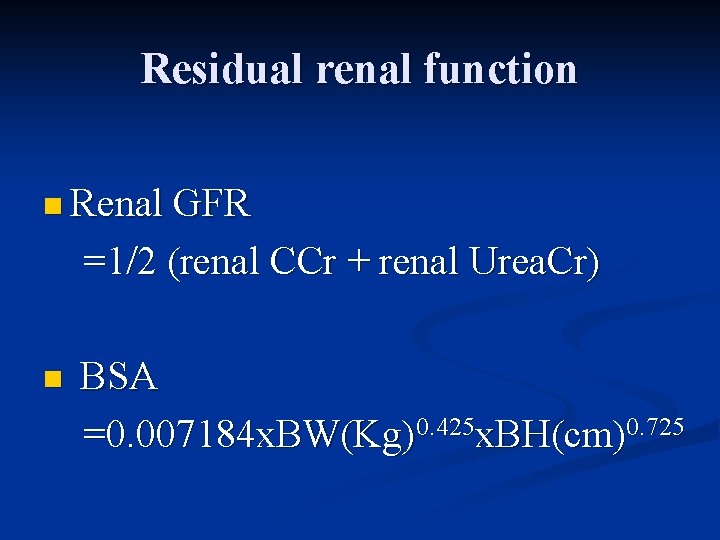
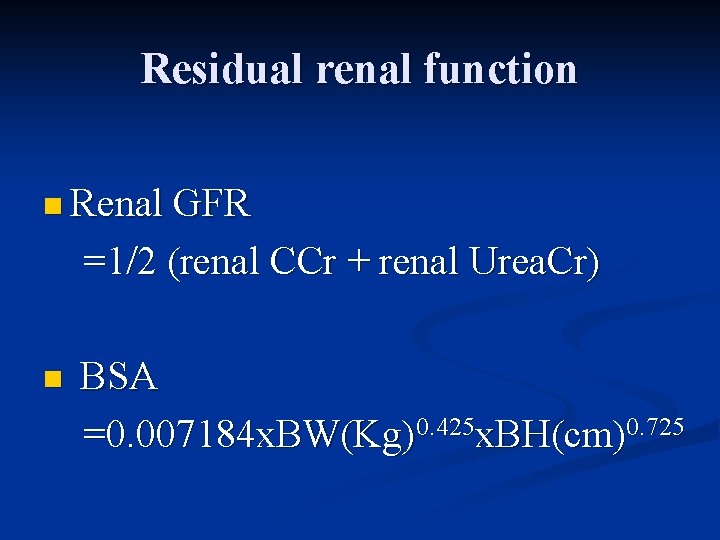
Residual renal function n Renal GFR =1/2 (renal CCr + renal Urea. Cr) n BSA =0. 007184 x. BW(Kg)0. 425 x. BH(cm)0. 725

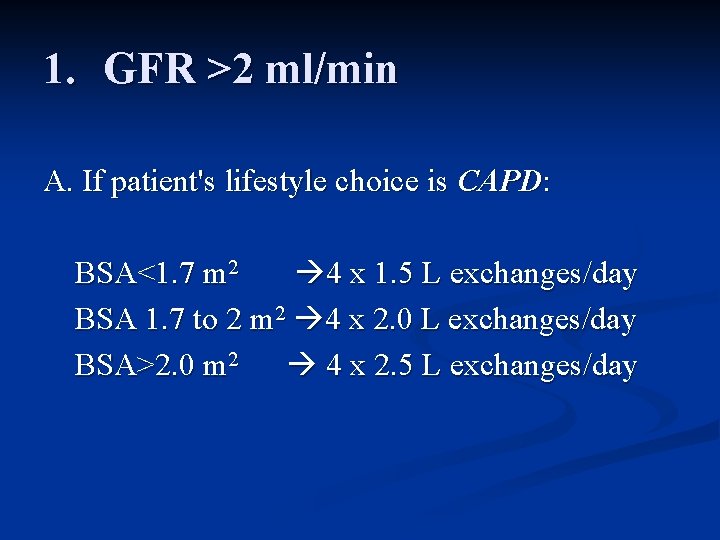
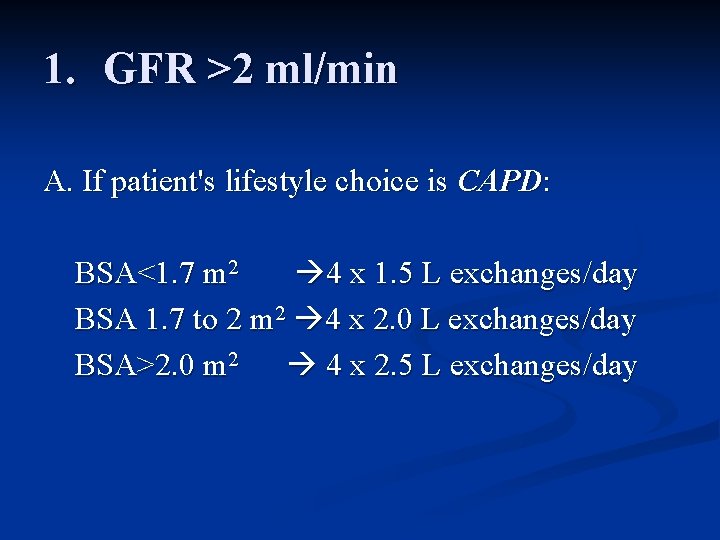
1. GFR >2 ml/min A. If patient's lifestyle choice is CAPD: BSA<1. 7 m 2 4 x 1. 5 L exchanges/day BSA 1. 7 to 2 m 2 4 x 2. 0 L exchanges/day BSA>2. 0 m 2 4 x 2. 5 L exchanges/day
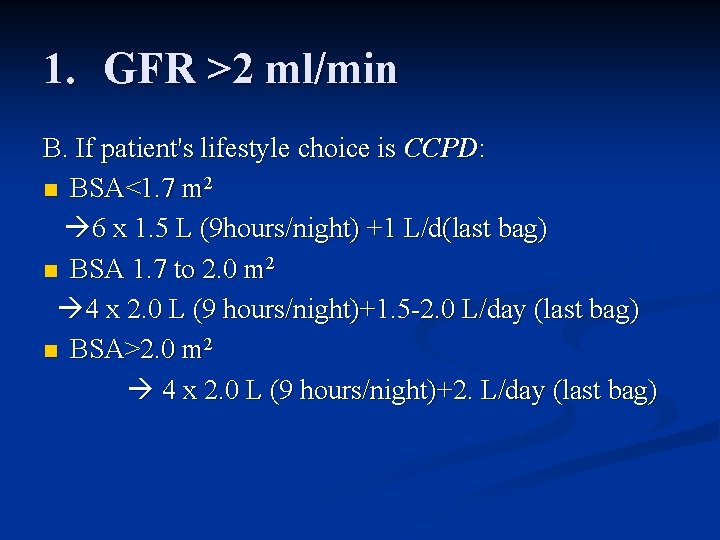
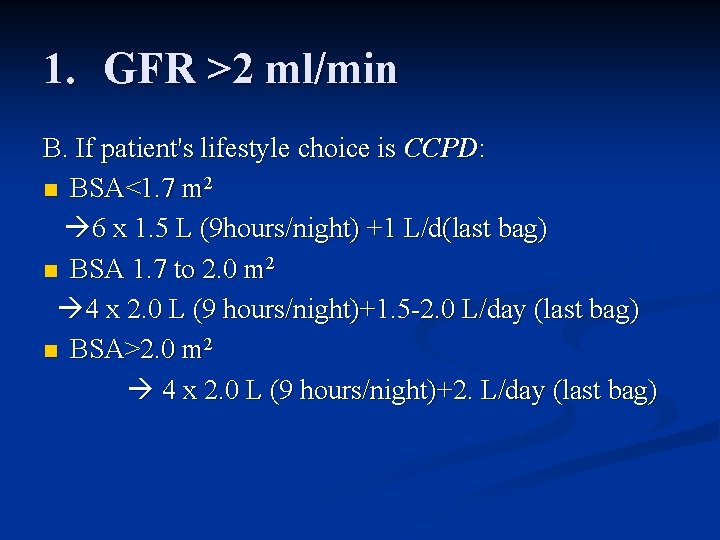
1. GFR >2 ml/min B. If patient's lifestyle choice is CCPD: n BSA<1. 7 m 2 6 x 1. 5 L (9 hours/night) +1 L/d(last bag) n BSA 1. 7 to 2. 0 m 2 4 x 2. 0 L (9 hours/night)+1. 5 -2. 0 L/day (last bag) n BSA>2. 0 m 2 4 x 2. 0 L (9 hours/night)+2. L/day (last bag)
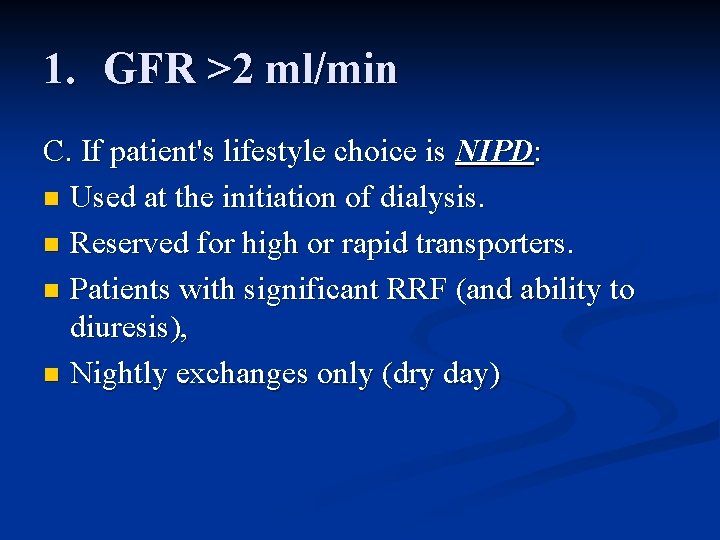
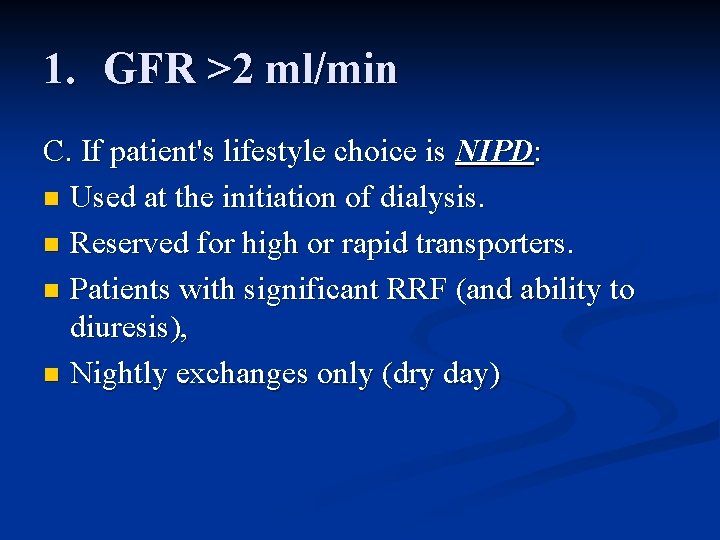
1. GFR >2 ml/min C. If patient's lifestyle choice is NIPD: n Used at the initiation of dialysis. n Reserved for high or rapid transporters. n Patients with significant RRF (and ability to diuresis), n Nightly exchanges only (dry day)
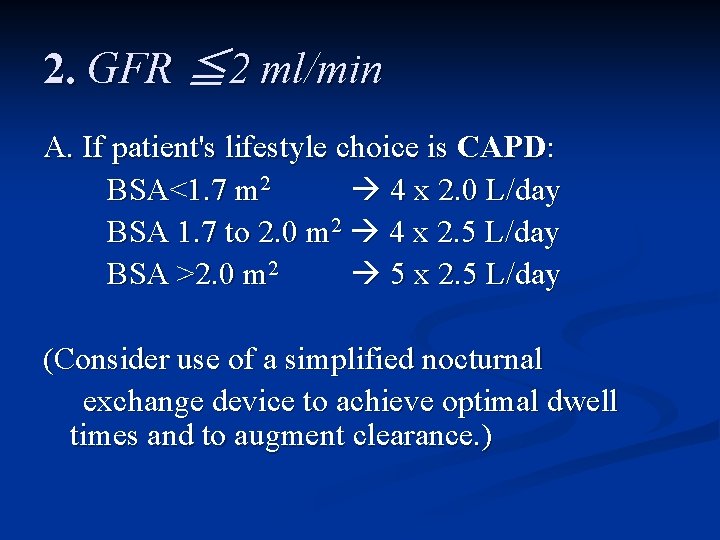
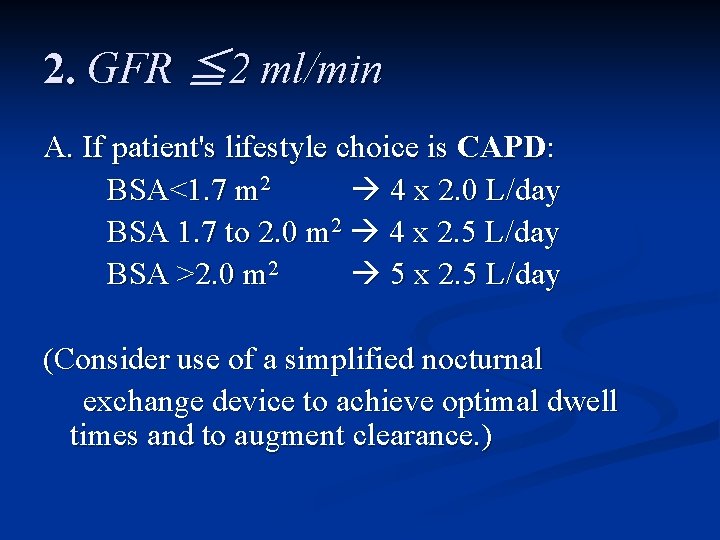
2. GFR ≦ 2 ml/min A. If patient's lifestyle choice is CAPD: BSA<1. 7 m 2 4 x 2. 0 L/day BSA 1. 7 to 2. 0 m 2 4 x 2. 5 L/day BSA >2. 0 m 2 5 x 2. 5 L/day (Consider use of a simplified nocturnal exchange device to achieve optimal dwell times and to augment clearance. )
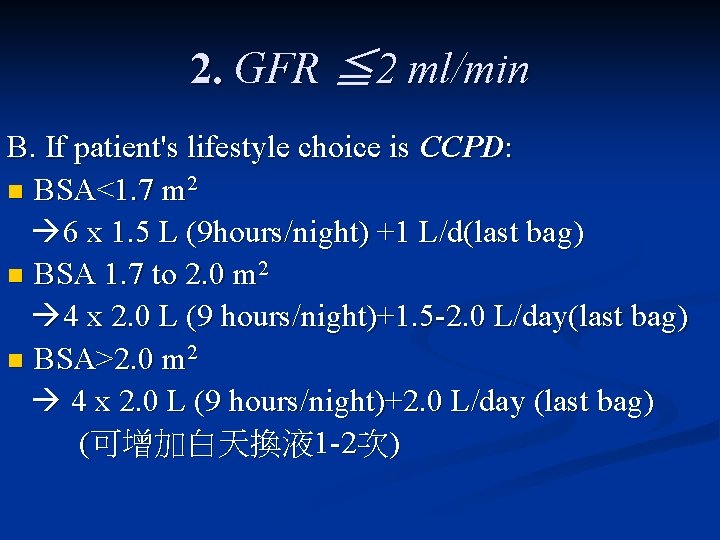
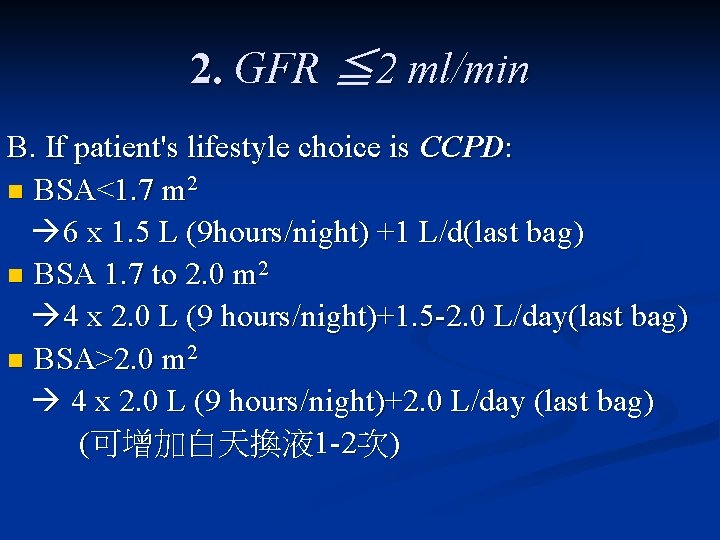
2. GFR ≦ 2 ml/min B. If patient's lifestyle choice is CCPD: n BSA<1. 7 m 2 6 x 1. 5 L (9 hours/night) +1 L/d(last bag) n BSA 1. 7 to 2. 0 m 2 4 x 2. 0 L (9 hours/night)+1. 5 -2. 0 L/day(last bag) n BSA>2. 0 m 2 4 x 2. 0 L (9 hours/night)+2. 0 L/day (last bag) (可增加白天換液 1 -2次)
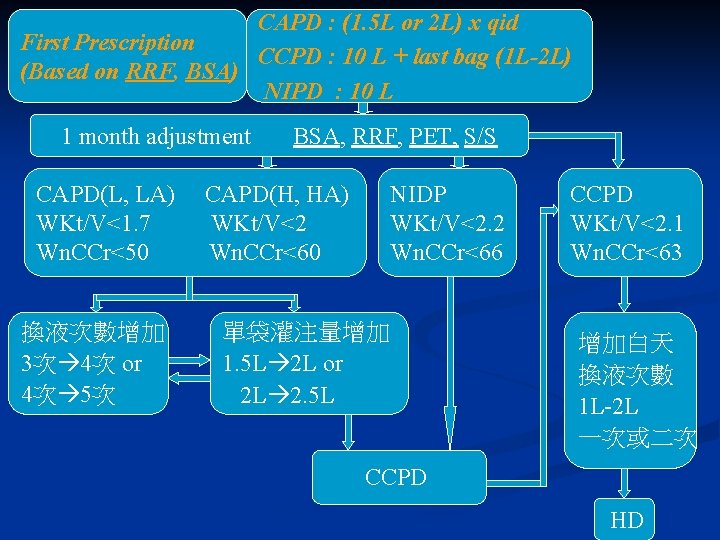
CAPD : (1. 5 L or 2 L) x qid First Prescription CCPD : 10 L + last bag (1 L-2 L) (Based on RRF, BSA) NIPD : 10 L 1 month adjustment CAPD(L, LA) WKt/V<1. 7 Wn. CCr<50 換液次數增加 3次 4次 or 4次 5次 BSA, RRF, PET, S/S CAPD(H, HA) WKt/V<2 Wn. CCr<60 NIDP WKt/V<2. 2 Wn. CCr<66 單袋灌注量增加 1. 5 L 2 L or 2 L 2. 5 L CCPD WKt/V<2. 1 Wn. CCr<63 增加白天 換液次數 1 L-2 L 一次或二次 CCPD HD
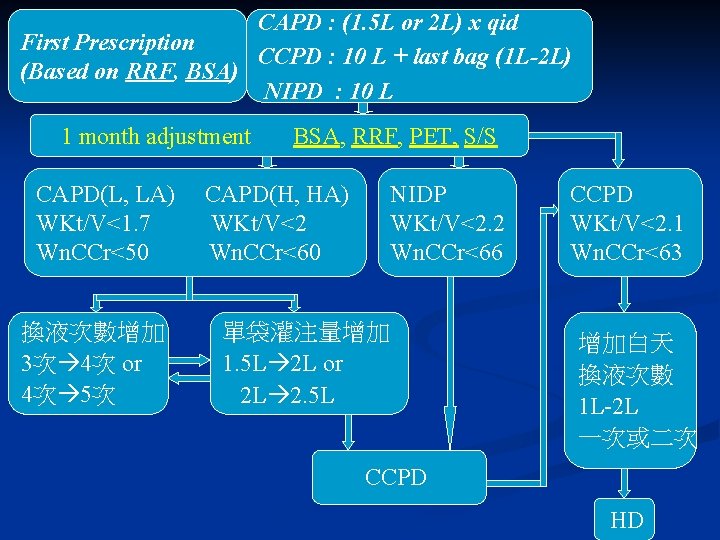
CAPD : (1. 5 L or 2 L) x qid First Prescription CCPD : 10 L + last bag (1 L-2 L) (Based on RRF, BSA) NIPD : 10 L 1 month adjustment CAPD(L, LA) WKt/V<1. 7 Wn. CCr<50 換液次數增加 3次 4次 or 4次 5次 BSA, RRF, PET, S/S CAPD(H, HA) WKt/V<2 Wn. CCr<60 NIDP WKt/V<2. 2 Wn. CCr<66 單袋灌注量增加 1. 5 L 2 L or 2 L 2. 5 L CCPD WKt/V<2. 1 Wn. CCr<63 增加白天 換液次數 1 L-2 L 一次或二次 CCPD HD
Adequate dialysis 1. Adequate solute removal ability 2. Adequate ultrafiltration
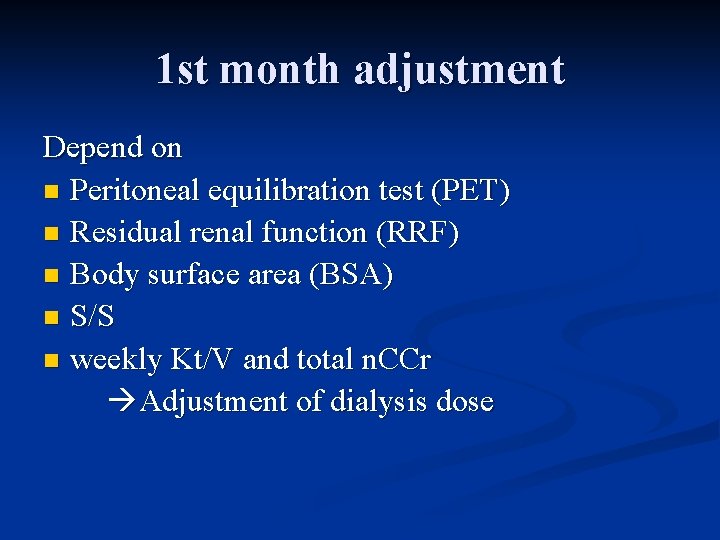
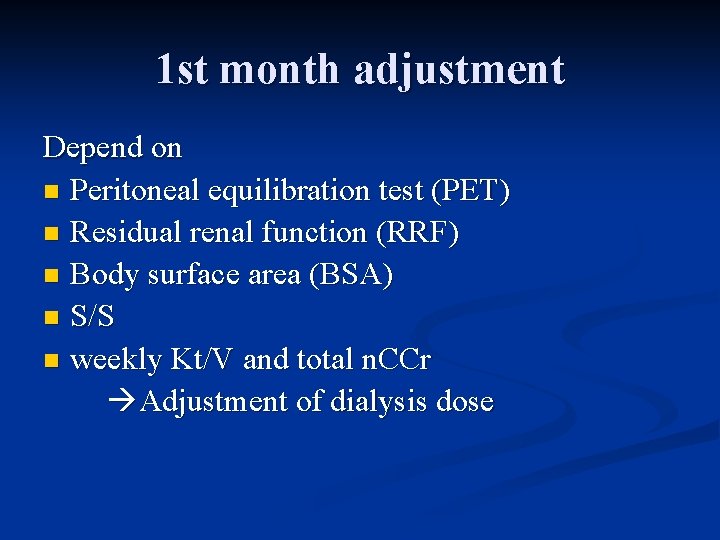
1 st month adjustment Depend on n Peritoneal equilibration test (PET) n Residual renal function (RRF) n Body surface area (BSA) n S/S n weekly Kt/V and total n. CCr Adjustment of dialysis dose


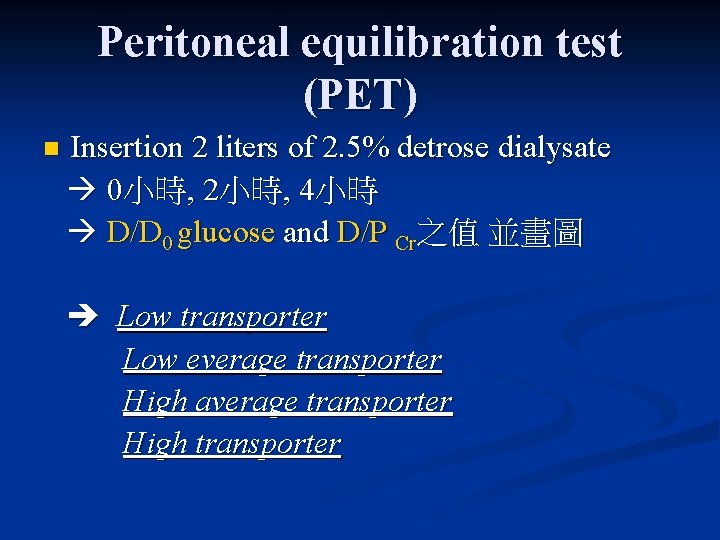
Peritoneal equilibration test (PET) n Insertion 2 liters of 2. 5% detrose dialysate 0小時, 2小時, 4小時 D/D 0 glucose and D/P Cr之值 並畫圖 Low transporter Low everage transporter High average transporter High transporter



Adequate solute removal ability
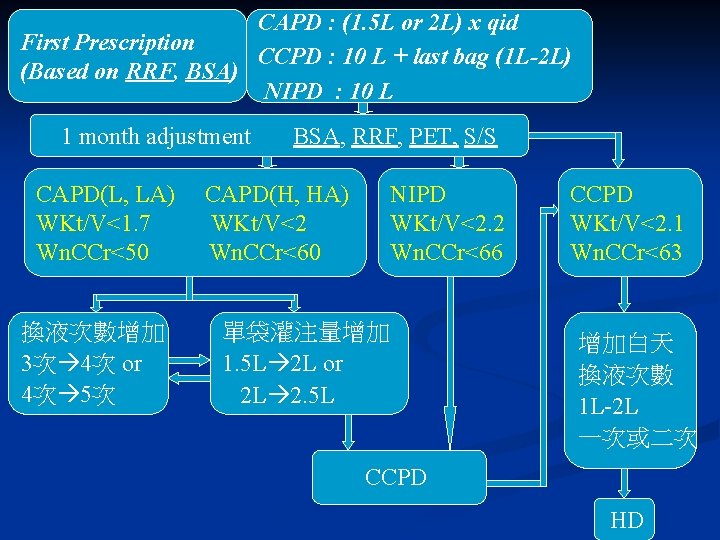
CAPD : (1. 5 L or 2 L) x qid First Prescription CCPD : 10 L + last bag (1 L-2 L) (Based on RRF, BSA) NIPD : 10 L 1 month adjustment CAPD(L, LA) WKt/V<1. 7 Wn. CCr<50 換液次數增加 3次 4次 or 4次 5次 BSA, RRF, PET, S/S CAPD(H, HA) WKt/V<2 Wn. CCr<60 NIPD WKt/V<2. 2 Wn. CCr<66 單袋灌注量增加 1. 5 L 2 L or 2 L 2. 5 L CCPD WKt/V<2. 1 Wn. CCr<63 增加白天 換液次數 1 L-2 L 一次或二次 CCPD HD

適量的腹膜透析 Weekly Kt/V =7 x (peritoneal Kt/V + renal Kt/V) Weekly n. CCr =7 x (Peritoneal CCr + renal. GFR)/(BSA/1. 73) =7 x [Peritoneal CCr + 1/2( renal CCr+renal ure. Cr)]/(BSA/1. 73)
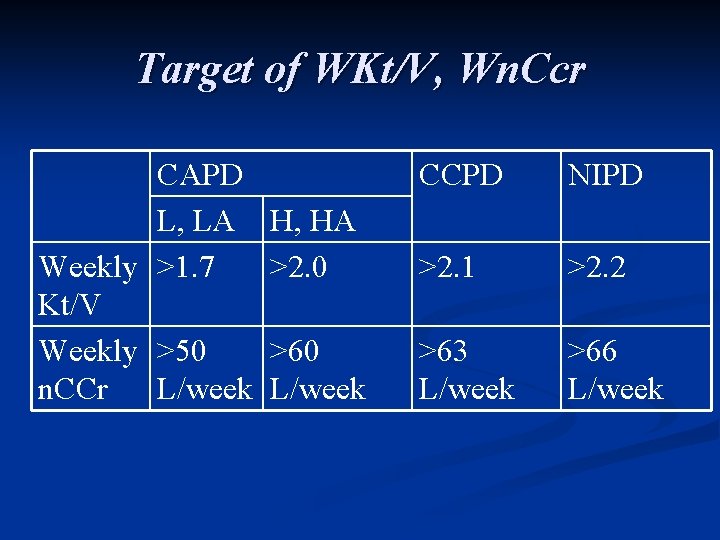
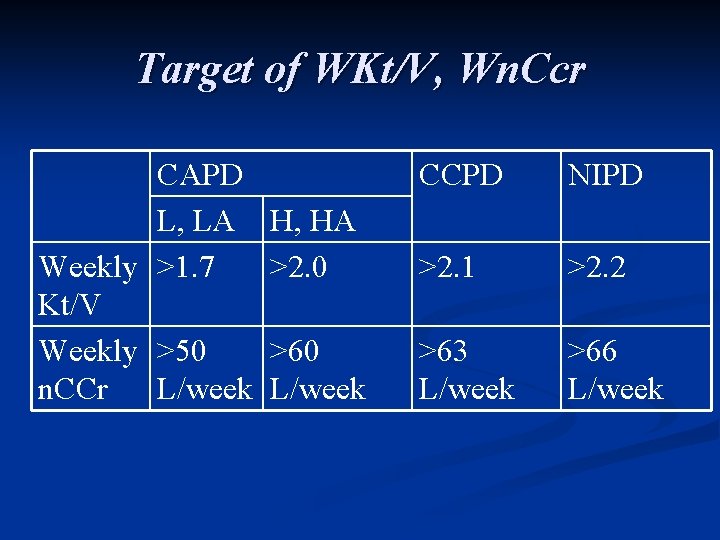
Target of WKt/V, Wn. Ccr CAPD L, LA H, HA Weekly >1. 7 >2. 0 Kt/V Weekly >50 >60 n. CCr L/week CCPD NIPD >2. 1 >2. 2 >63 L/week >66 L/week

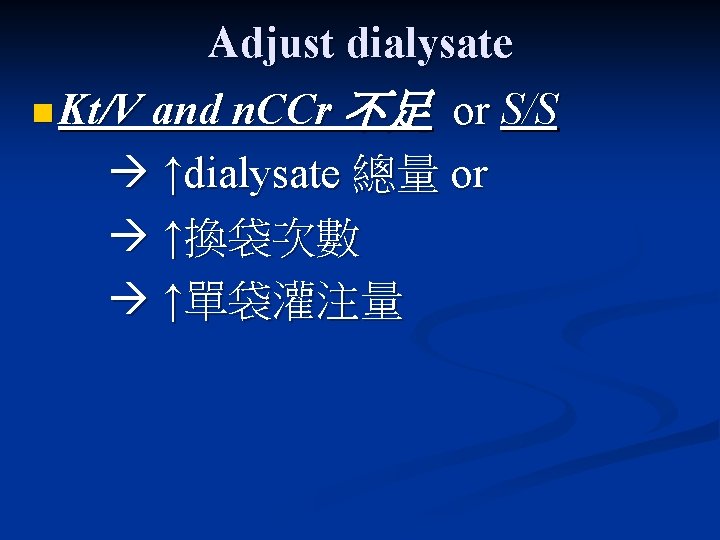
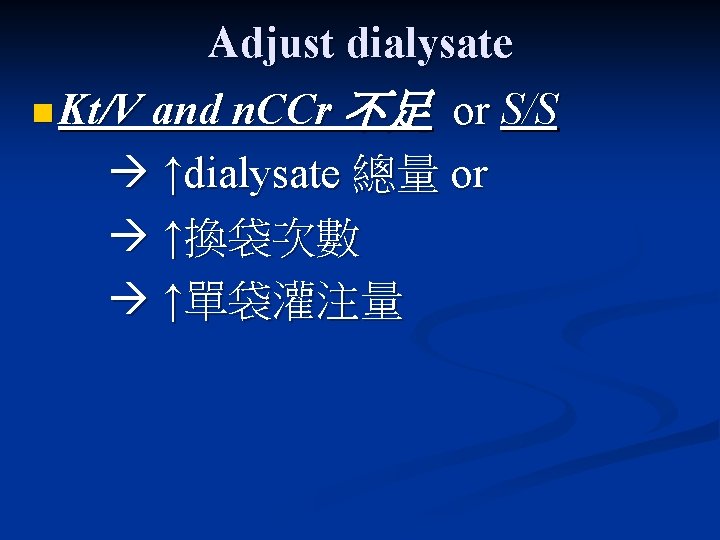
Adjust dialysate n Kt/V and n. CCr 不足 or S/S ↑dialysate 總量 or ↑換袋次數 ↑單袋灌注量
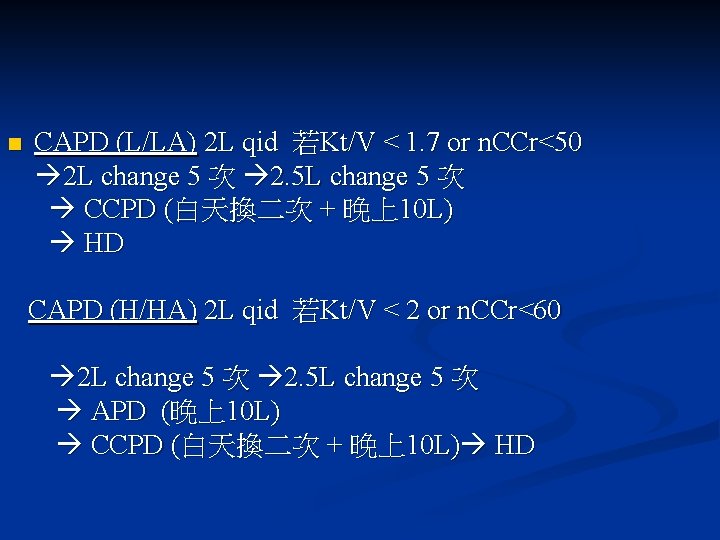
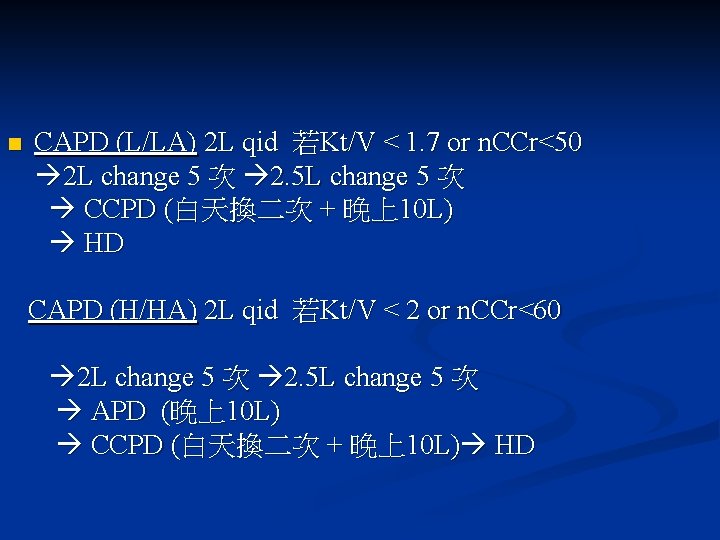
n CAPD (L/LA) 2 L qid 若Kt/V < 1. 7 or n. CCr<50 2 L change 5 次 2. 5 L change 5 次 CCPD (白天換二次 + 晚上10 L) HD CAPD (H/HA) 2 L qid 若Kt/V < 2 or n. CCr<60 2 L change 5 次 2. 5 L change 5 次 APD (晚上10 L) CCPD (白天換二次 + 晚上10 L) HD
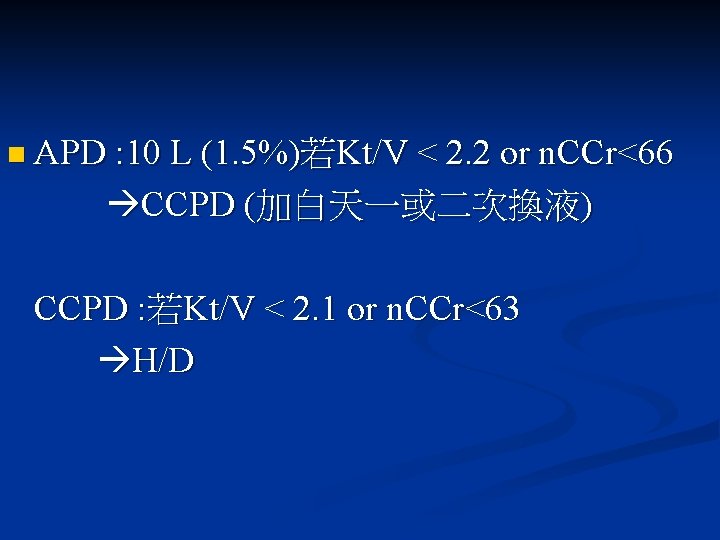
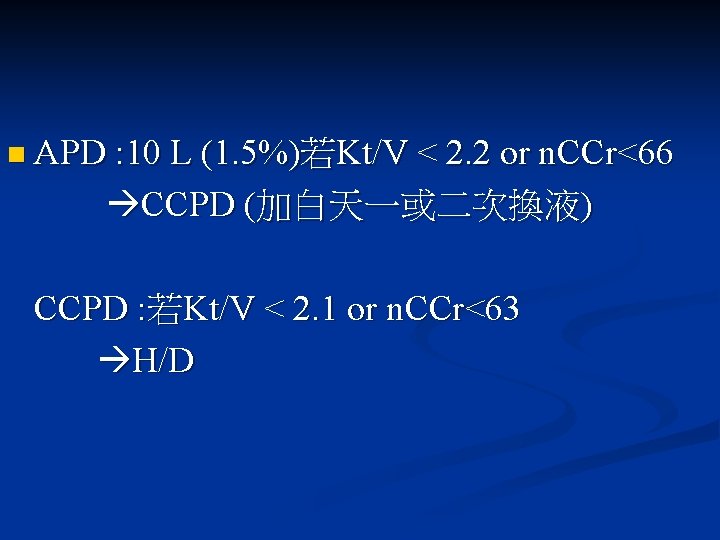
n APD : 10 L (1. 5%)若Kt/V < 2. 2 or n. CCr<66 CCPD (加白天一或二次換液) CCPD : 若Kt/V < 2. 1 or n. CCr<63 H/D
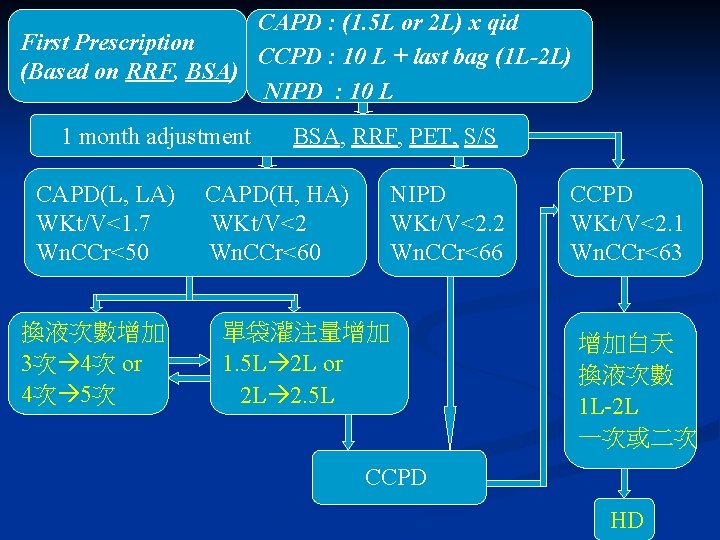
CAPD : (1. 5 L or 2 L) x qid First Prescription CCPD : 10 L + last bag (1 L-2 L) (Based on RRF, BSA) NIPD : 10 L 1 month adjustment CAPD(L, LA) WKt/V<1. 7 Wn. CCr<50 換液次數增加 3次 4次 or 4次 5次 BSA, RRF, PET, S/S CAPD(H, HA) WKt/V<2 Wn. CCr<60 NIPD WKt/V<2. 2 Wn. CCr<66 單袋灌注量增加 1. 5 L 2 L or 2 L 2. 5 L CCPD WKt/V<2. 1 Wn. CCr<63 增加白天 換液次數 1 L-2 L 一次或二次 CCPD HD

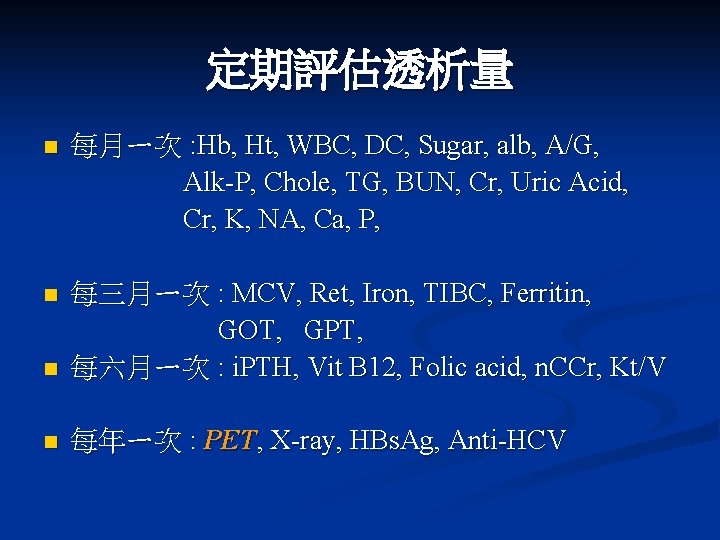
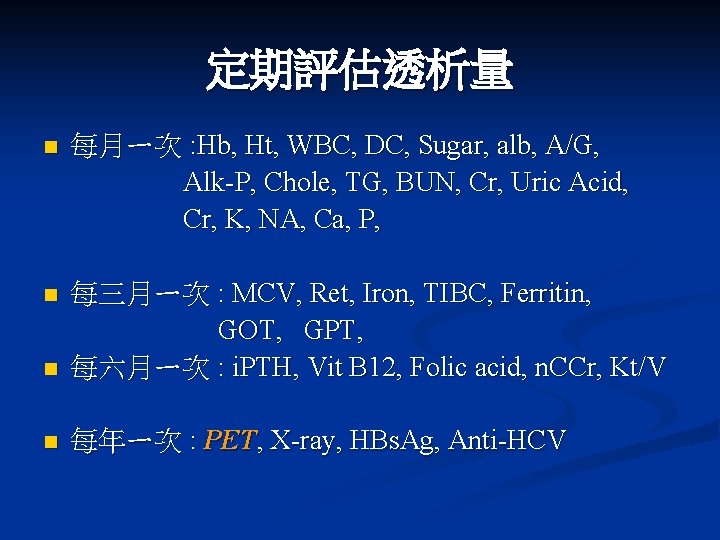
定期評估透析量 n 每月ㄧ次 : Hb, Ht, WBC, DC, Sugar, alb, A/G, Alk-P, Chole, TG, BUN, Cr, Uric Acid, Cr, K, NA, Ca, P, n n 每三月ㄧ次 : MCV, Ret, Iron, TIBC, Ferritin, GOT, GPT, 每六月ㄧ次 : i. PTH, Vit B 12, Folic acid, n. CCr, Kt/V n 每年ㄧ次 : PET, X-ray, HBs. Ag, Anti-HCV
Adequate ultrafiltration


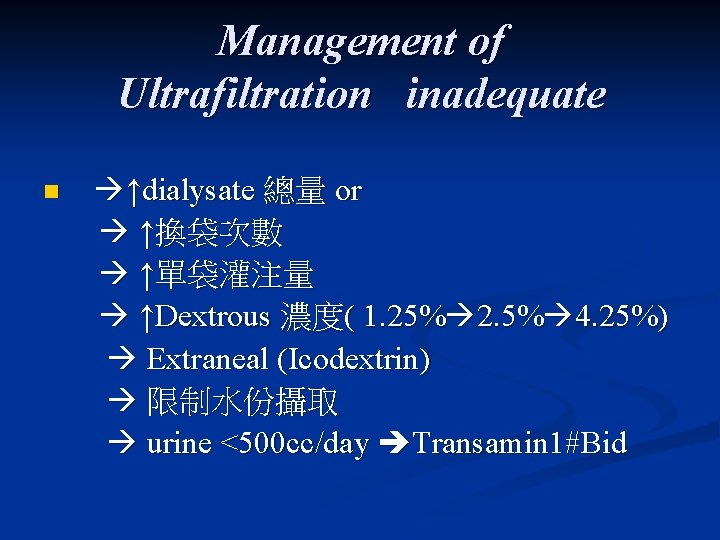
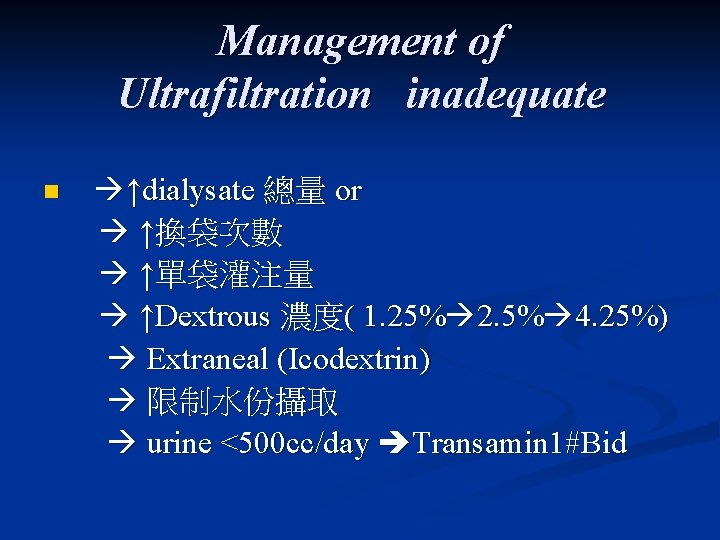
Management of Ultrafiltration inadequate n ↑dialysate 總量 or ↑換袋次數 ↑單袋灌注量 ↑Dextrous 濃度( 1. 25% 2. 5% 4. 25%) Extraneal (Icodextrin) 限制水份攝取 urine <500 cc/day Transamin 1#Bid
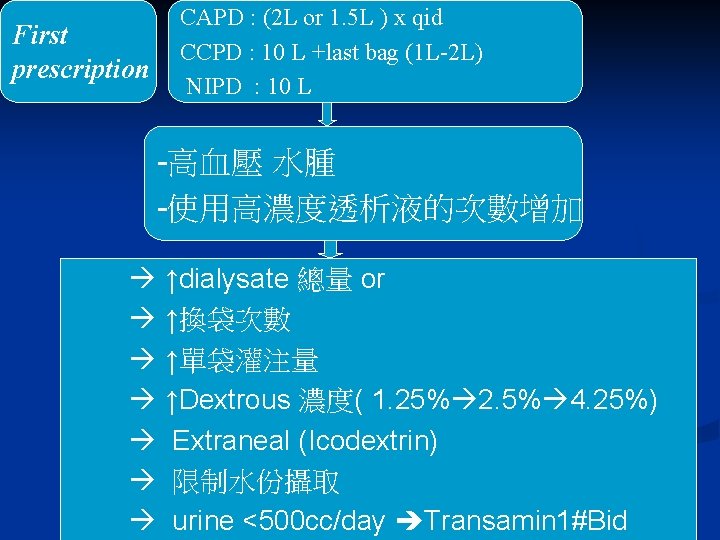
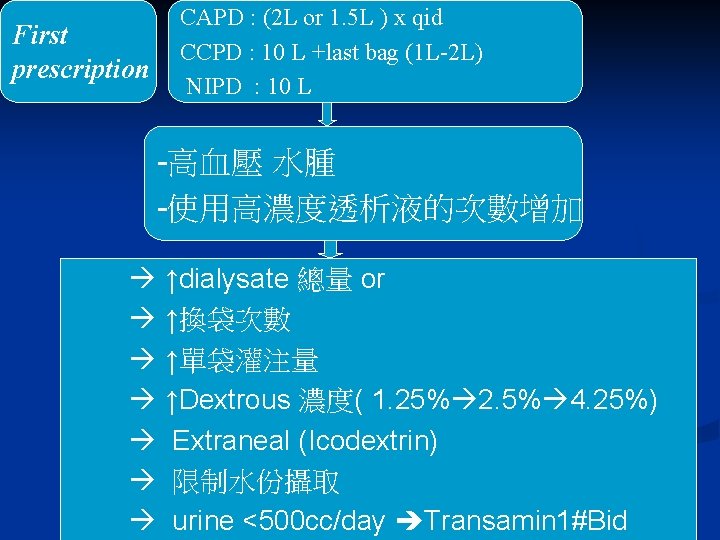
First prescription CAPD : (2 L or 1. 5 L ) x qid CCPD : 10 L +last bag (1 L-2 L) NIPD : 10 L -高血壓 水腫 -使用高濃度透析液的次數增加 ↑dialysate 總量 or ↑換袋次數 ↑單袋灌注量 ↑Dextrous 濃度( 1. 25% 2. 5% 4. 25%) Extraneal (Icodextrin) 限制水份攝取 urine <500 cc/day Transamin 1#Bid

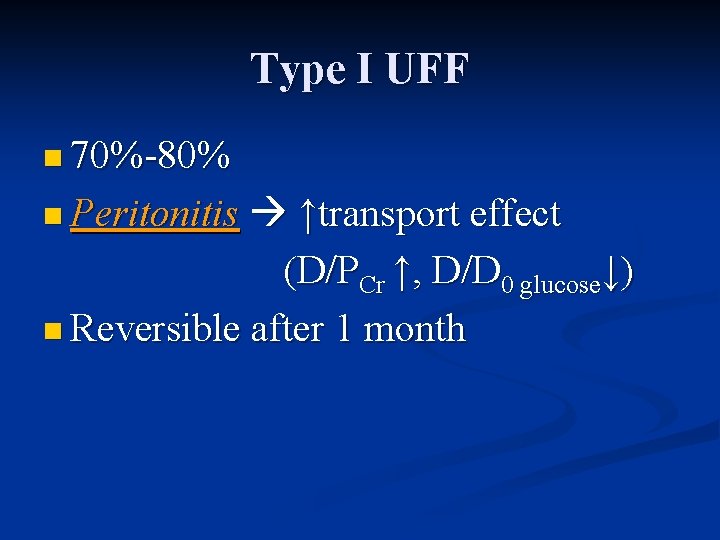
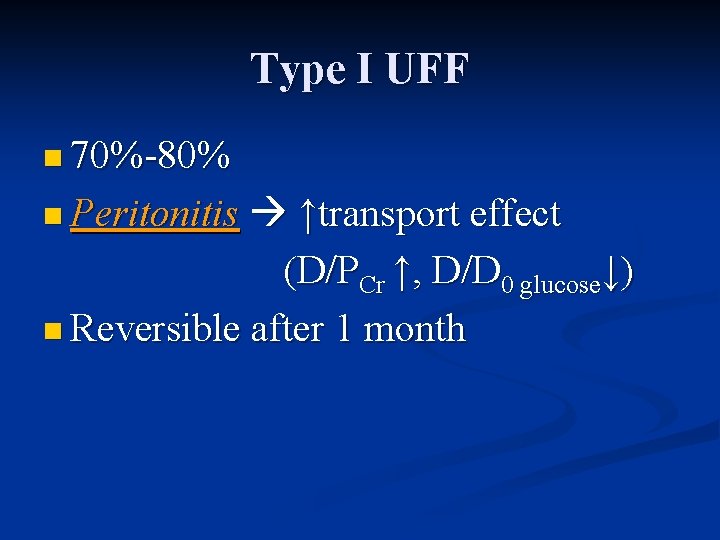
Type I UFF n 70%-80% ↑transport effect (D/PCr ↑, D/D 0 glucose↓) n Reversible after 1 month n Peritonitis
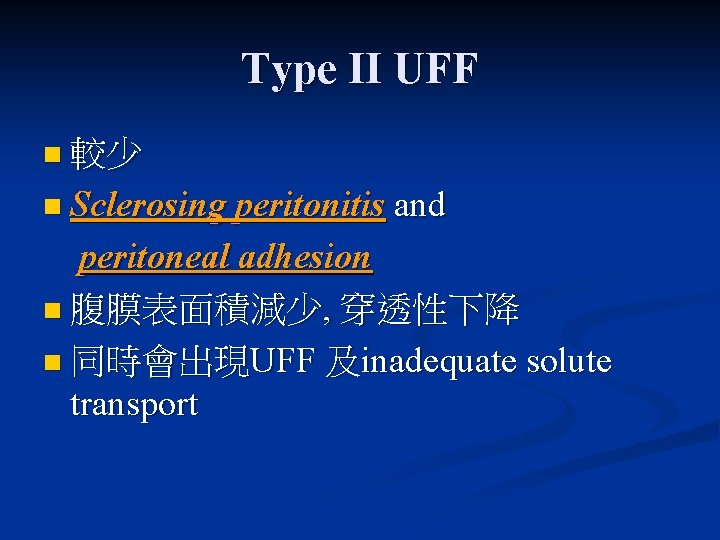
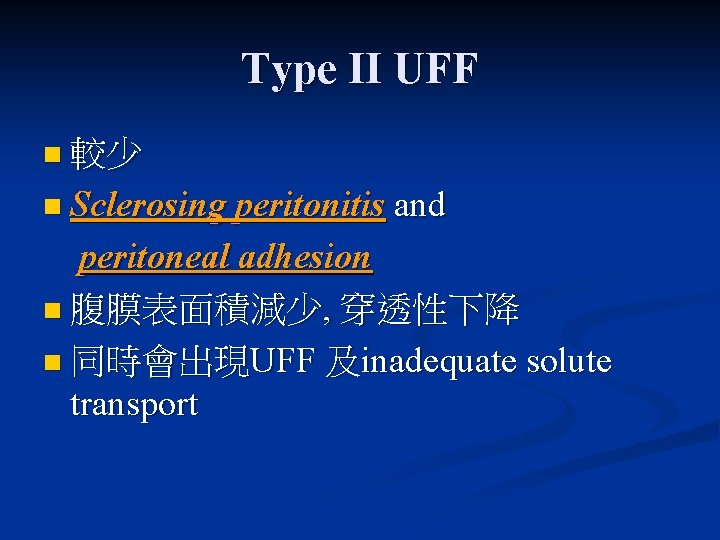
Type II UFF n 較少 n Sclerosing peritonitis and peritoneal adhesion n 腹膜表面積減少, 穿透性下降 n 同時會出現UFF 及inadequate solute transport
Type III UFF n High lymphatic absorption rate n Uncommon
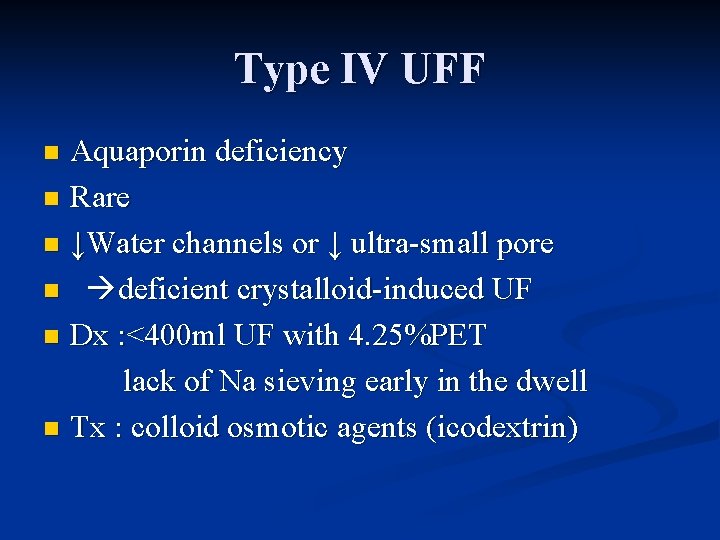
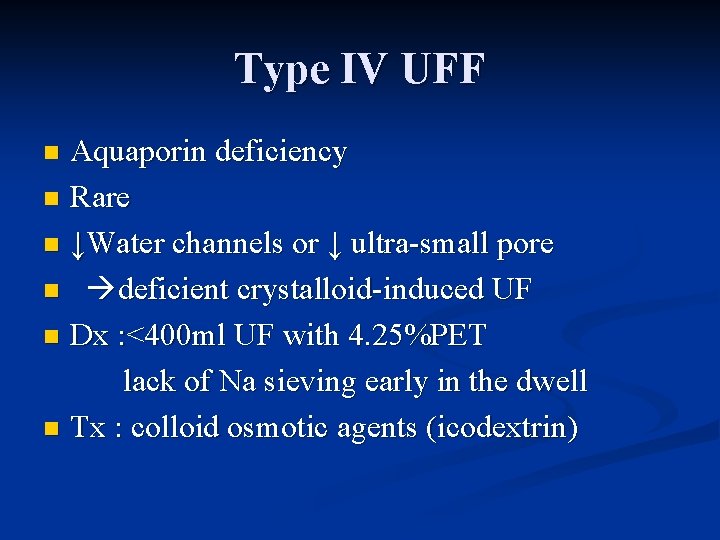
Type IV UFF Aquaporin deficiency n Rare n ↓Water channels or ↓ ultra-small pore n deficient crystalloid-induced UF n Dx : <400 ml UF with 4. 25%PET lack of Na sieving early in the dwell n Tx : colloid osmotic agents (icodextrin) n

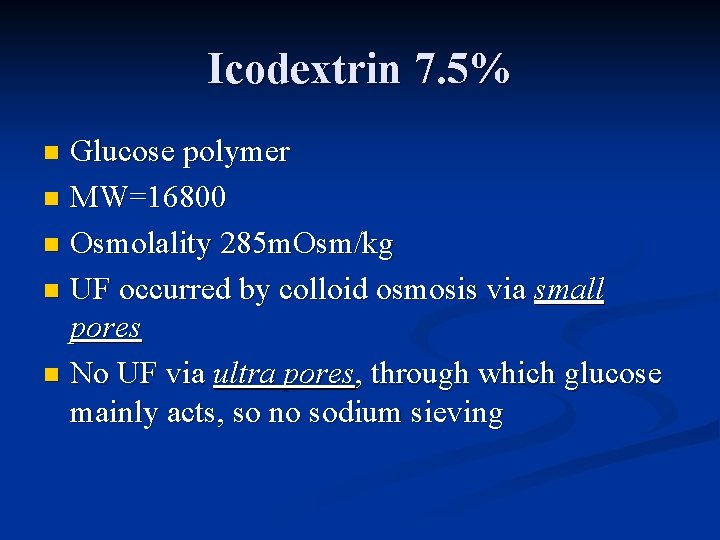
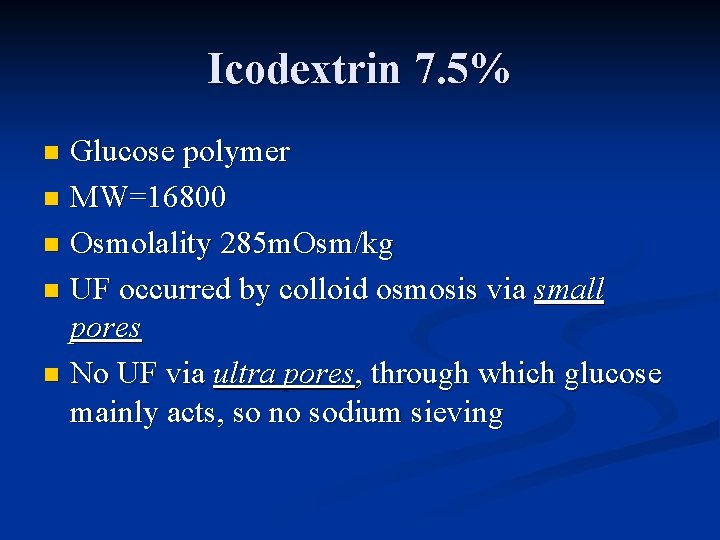
Icodextrin 7. 5% Glucose polymer n MW=16800 n Osmolality 285 m. Osm/kg n UF occurred by colloid osmosis via small pores n No UF via ultra pores, through which glucose mainly acts, so no sodium sieving n

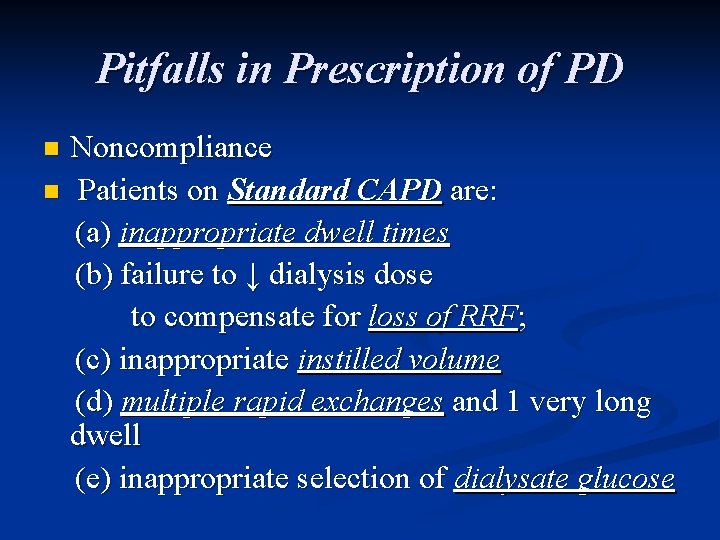
Pitfalls in Prescription of PD Noncompliance n Patients on Standard CAPD are: (a) inappropriate dwell times (b) failure to ↓ dialysis dose to compensate for loss of RRF; (c) inappropriate instilled volume (d) multiple rapid exchanges and 1 very long dwell (e) inappropriate selection of dialysate glucose n
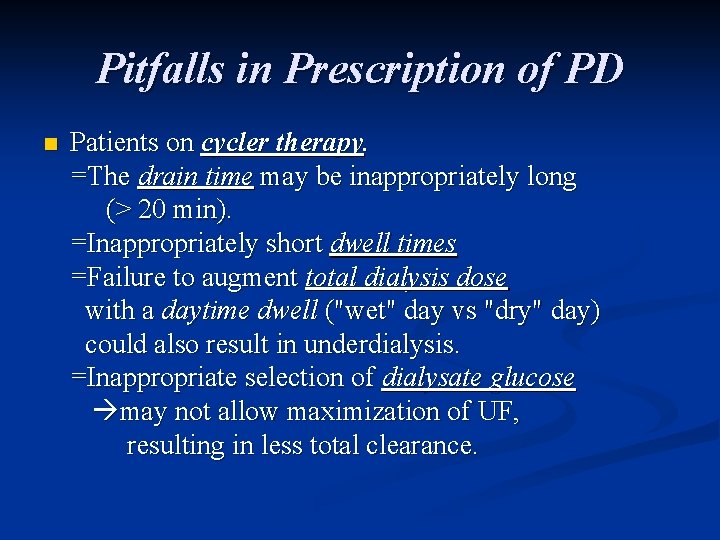
Pitfalls in Prescription of PD n Patients on cycler therapy. =The drain time may be inappropriately long (> 20 min). =Inappropriately short dwell times =Failure to augment total dialysis dose with a daytime dwell ("wet" day vs "dry" day) could also result in underdialysis. =Inappropriate selection of dialysate glucose may not allow maximization of UF, resulting in less total clearance.