Cancer Survivorship Prostate Cancer Risks and Treatments Photo




















- Slides: 114
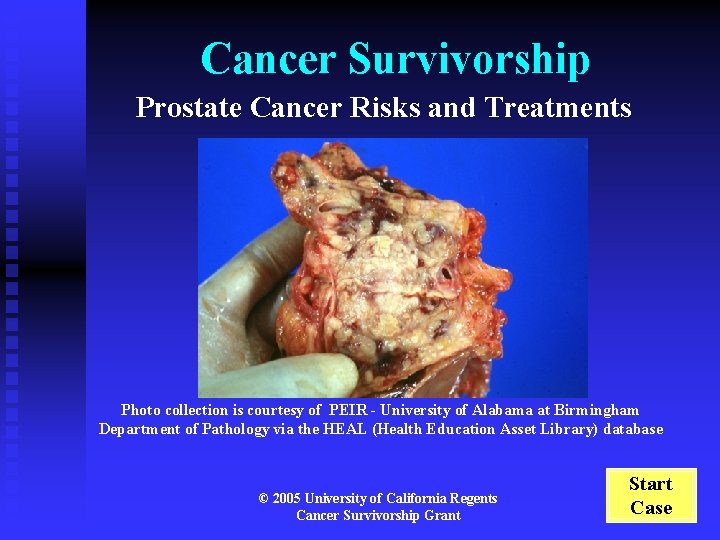
Cancer Survivorship Prostate Cancer Risks and Treatments Photo collection is courtesy of PEIR - University of Alabama at Birmingham Department of Pathology via the HEAL (Health Education Asset Library) database © 2005 University of California Regents Cancer Survivorship Grant Start Case

Goal of this Module This is an interactive and self-directed learning module intended to build a foundation of knowledge around the epidemiology and late effects of cancer survival. This is one of several educational modules you will complete during your core clinical clerkships. Themes emphasized in this, and other modules, are: u Epidemiology of survival u Late effects u Psychosocial concerns u Secondary prevention u Strategies for behavior change Meet your patient
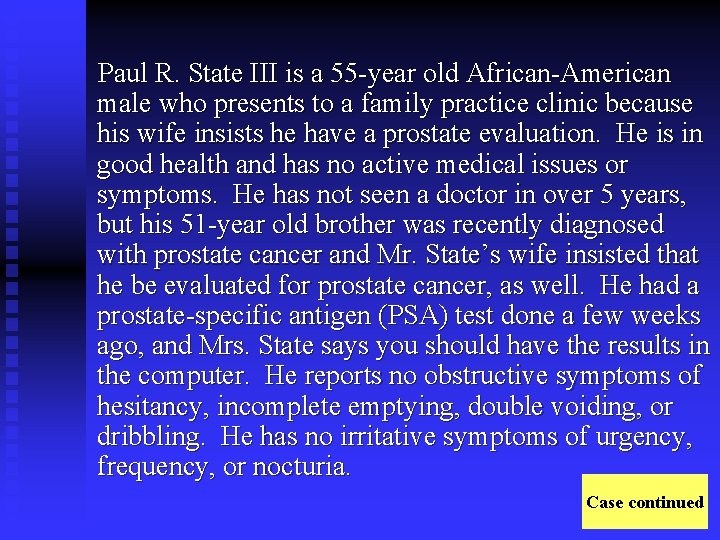
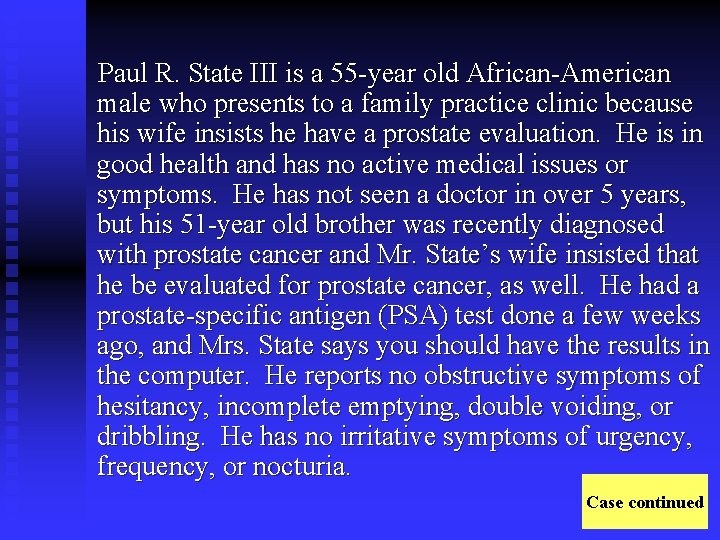
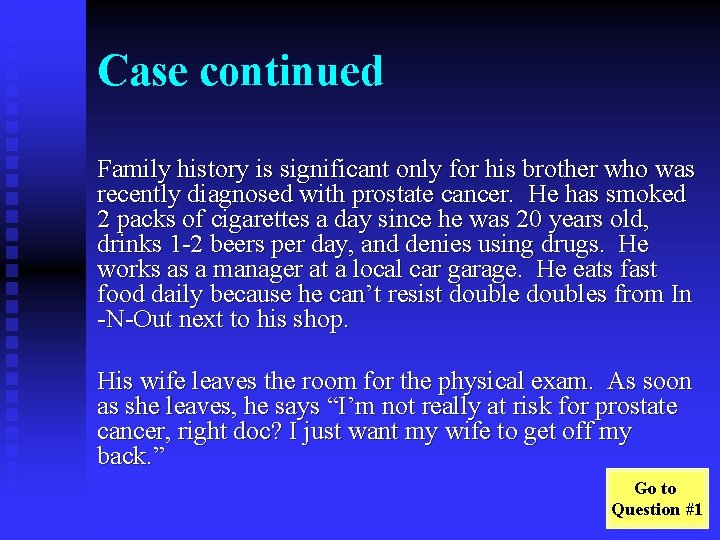
Paul R. State III is a 55 -year old African-American male who presents to a family practice clinic because his wife insists he have a prostate evaluation. He is in good health and has no active medical issues or symptoms. He has not seen a doctor in over 5 years, but his 51 -year old brother was recently diagnosed with prostate cancer and Mr. State’s wife insisted that he be evaluated for prostate cancer, as well. He had a prostate-specific antigen (PSA) test done a few weeks ago, and Mrs. State says you should have the results in the computer. He reports no obstructive symptoms of hesitancy, incomplete emptying, double voiding, or dribbling. He has no irritative symptoms of urgency, frequency, or nocturia. Case continued
Case continued Family history is significant only for his brother who was recently diagnosed with prostate cancer. He has smoked 2 packs of cigarettes a day since he was 20 years old, drinks 1 -2 beers per day, and denies using drugs. He works as a manager at a local car garage. He eats fast food daily because he can’t resist doubles from In -N-Out next to his shop. His wife leaves the room for the physical exam. As soon as she leaves, he says “I’m not really at risk for prostate cancer, right doc? I just want my wife to get off my back. ” Go to Question #1
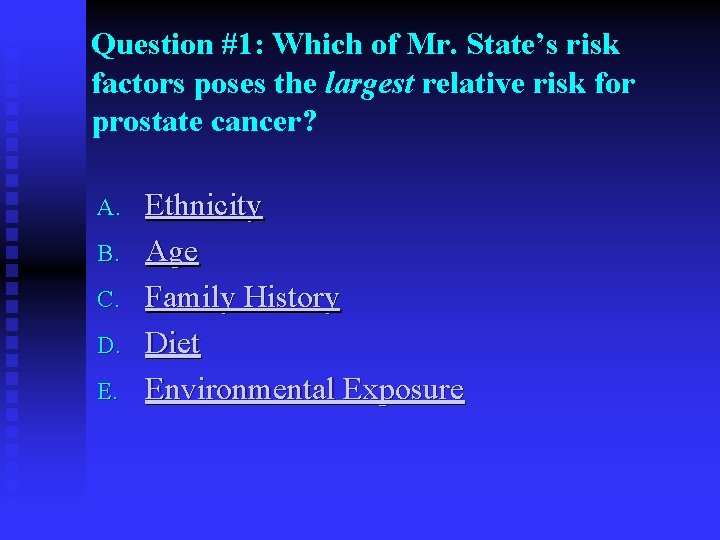
Question #1: Which of Mr. State’s risk factors poses the largest relative risk for prostate cancer? A. B. C. D. E. Ethnicity Age Family History Diet Environmental Exposure
Question #1: Incorrect Answer A. Ethnicity: African-Americans are at higher risk for prostate cancer than matched Caucasians. On average, they present with more advanced disease at initial diagnosis. The potential increased mortality for African-Americans compared to Caucasians is controversial. Prostate cancer screening should begin at 40 years of age for African-Americans. Ethnicity does not pose the largest relative risk in this patient. Ethnicity article (Kang, BJU 2004) Return to Question #1
Question #1: Correct Answer B. Age: The incidence of prostate cancer increases with age. Clinically significant prostate cancer develops in 0. 01% of men<40 years old, 1% of men 40 -59 years old, and 13% of men over the age of 60. Age article (Thompson, NEJM 2004) Continue case
Question #1: Incorrect Answer C. Family History: The age at which the disease was diagnosed in a first-degree family member is vital to determining the relative risk for Mr. State. The relative risk for prostate cancer is 47 x if the age of onset was 50 years old, 3 -5 x if the age of onset was 60 years old, and 2 -4 x if the age of onset was 70 years old. Prostate cancer screening should begin at 40 years of age for patients with a family history of prostate cancer. Family history article (Thompson, NEJM 2004) Return to Question #1
Question #1: Incorrect Answer D. Diet: Although high fat intake doubles Mr. States risk of prostate cancer, diet does not pose the largest relative risk. Diet article (Mazhar: BJU 2004) Return to Question #1
Question #1: Incorrect Answer E. Environmental exposure: His risk of prostate cancer increases with exposure to alkaline batteries, welding chemicals, and, possibly, tobacco (all contain cadmium, which is carcinogenic in the prostate. ) However, these exposures do not pose the largest relative risk. Environmental exposure article (Deutsch: Lancet Oncol 2004) Return to Question #1

Case Continued On physical exam, Mr. State is obese and in no apparent distress. HEENT, cardiovascular, pulmonary, and abdominal exams are within normal limits. Continue case
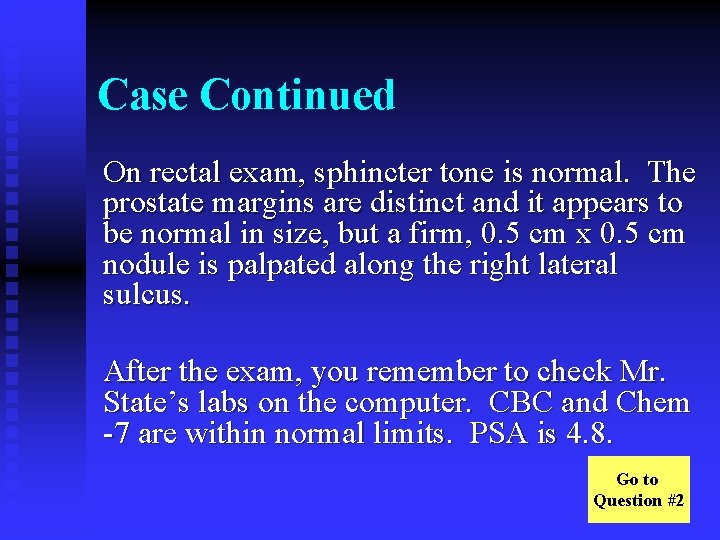
Case Continued On rectal exam, sphincter tone is normal. The prostate margins are distinct and it appears to be normal in size, but a firm, 0. 5 cm x 0. 5 cm nodule is palpated along the right lateral sulcus. After the exam, you remember to check Mr. State’s labs on the computer. CBC and Chem -7 are within normal limits. PSA is 4. 8. Go to Question #2
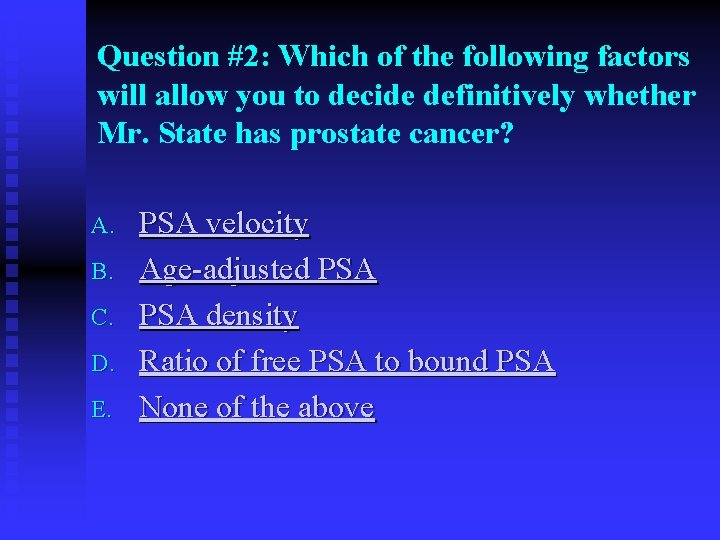
Question #2: Which of the following factors will allow you to decide definitively whether Mr. State has prostate cancer? A. B. C. D. E. PSA velocity Age-adjusted PSA density Ratio of free PSA to bound PSA None of the above
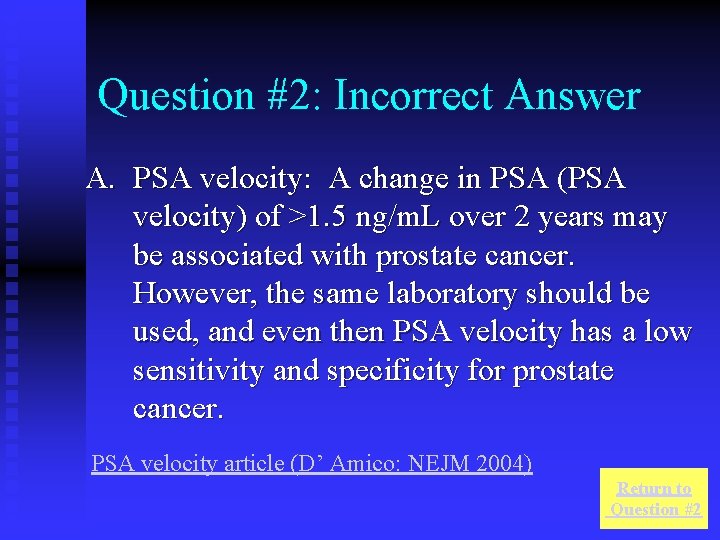
Question #2: Incorrect Answer A. PSA velocity: A change in PSA (PSA velocity) of >1. 5 ng/m. L over 2 years may be associated with prostate cancer. However, the same laboratory should be used, and even then PSA velocity has a low sensitivity and specificity for prostate cancer. PSA velocity article (D’ Amico: NEJM 2004) Return to Question #2
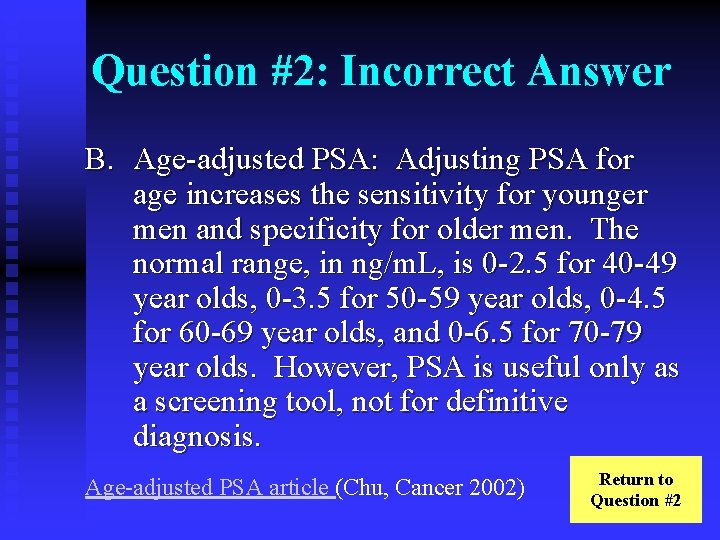
Question #2: Incorrect Answer B. Age-adjusted PSA: Adjusting PSA for age increases the sensitivity for younger men and specificity for older men. The normal range, in ng/m. L, is 0 -2. 5 for 40 -49 year olds, 0 -3. 5 for 50 -59 year olds, 0 -4. 5 for 60 -69 year olds, and 0 -6. 5 for 70 -79 year olds. However, PSA is useful only as a screening tool, not for definitive diagnosis. Age-adjusted PSA article (Chu, Cancer 2002) Return to Question #2
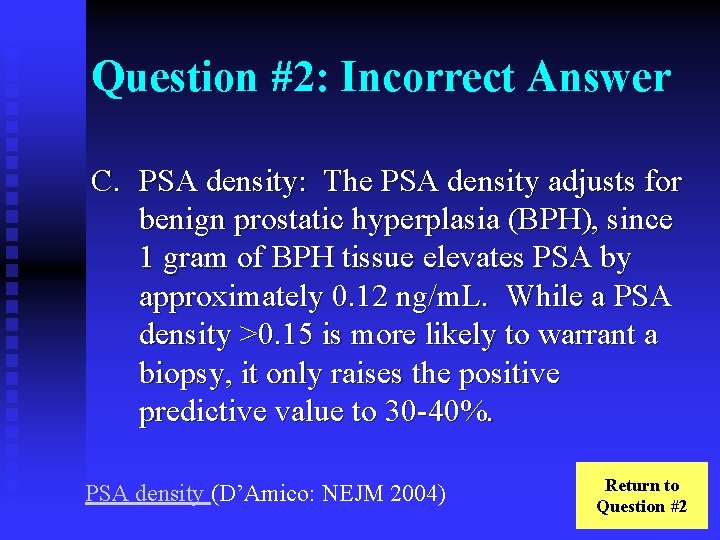
Question #2: Incorrect Answer C. PSA density: The PSA density adjusts for benign prostatic hyperplasia (BPH), since 1 gram of BPH tissue elevates PSA by approximately 0. 12 ng/m. L. While a PSA density >0. 15 is more likely to warrant a biopsy, it only raises the positive predictive value to 30 -40%. PSA density (D’Amico: NEJM 2004) Return to Question #2
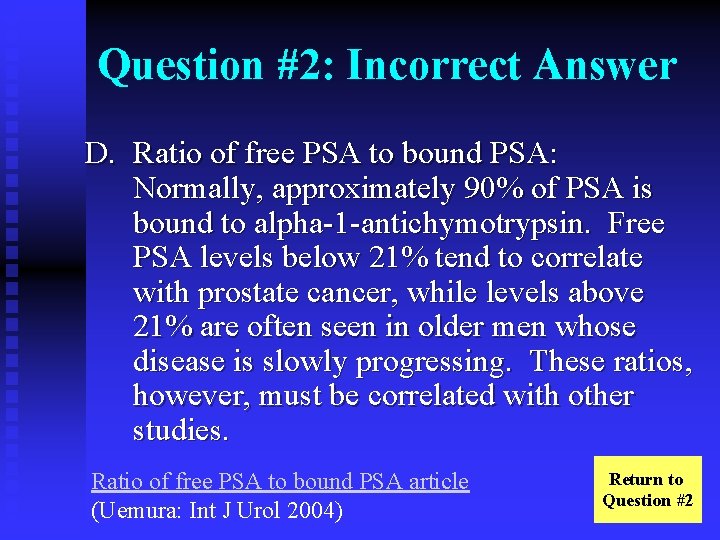
Question #2: Incorrect Answer D. Ratio of free PSA to bound PSA: Normally, approximately 90% of PSA is bound to alpha-1 -antichymotrypsin. Free PSA levels below 21% tend to correlate with prostate cancer, while levels above 21% are often seen in older men whose disease is slowly progressing. These ratios, however, must be correlated with other studies. Ratio of free PSA to bound PSA article (Uemura: Int J Urol 2004) Return to Question #2
Question #2: Correct Answer E. None of the above: PSA>4 ng/m. L has a positive predictive value of 20 -30% for carcinoma of the prostate. While each of the above adjustments is useful in improving the sensitivity and specificity of the test to some extent, PSA should still be used to guide a further work-up and should be considered in the context of the patient’s other personal risk factors, history, physical exam, and other findings. PSA may be elevated secondary to BPH, urethral instrumentation, infection, prostatic infarction, or prostatic massage. The only way to definitively diagnose prostate cancer is with biopsy. Continue case
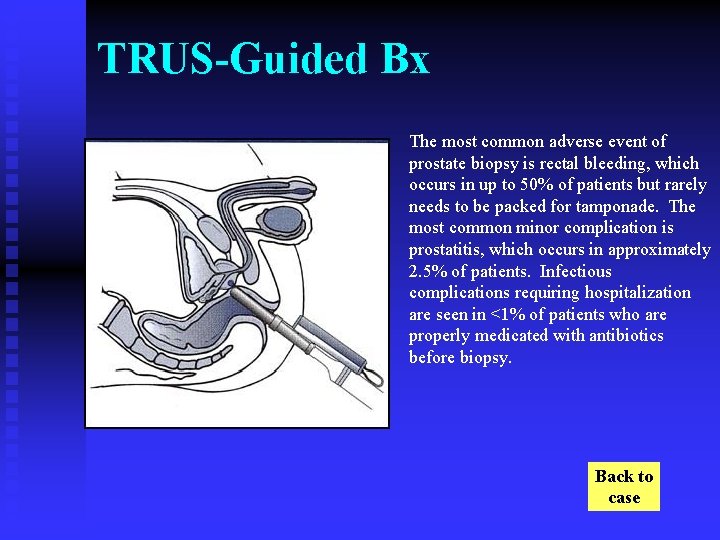
Case Continued You tell Mr. State that you would like to perform a trans-rectal ultrasound (TRUS)-guided biopsy. He argues that it is an uncomfortable procedure and says he doesn’t see the point, but Mrs. State chides him that “the doctor knows best”. He agrees to the procedure. Before performing the TRUS, you try to predict where a potential cancer might be found. Go to Question #3
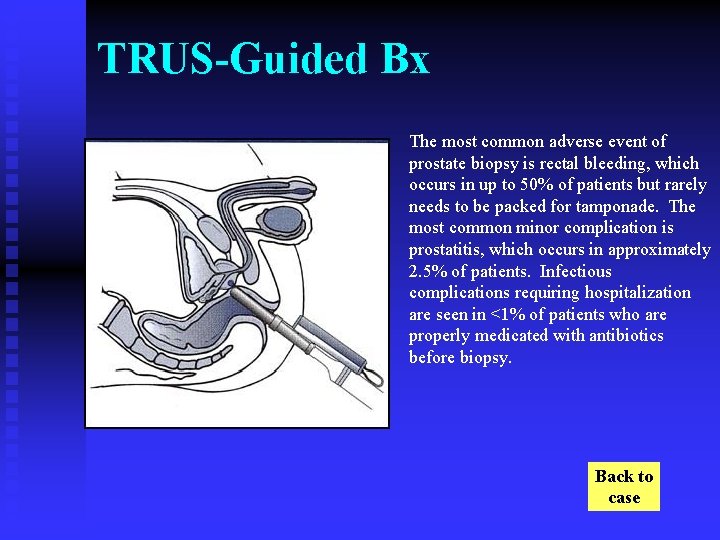
TRUS-Guided Bx The most common adverse event of prostate biopsy is rectal bleeding, which occurs in up to 50% of patients but rarely needs to be packed for tamponade. The most common minor complication is prostatitis, which occurs in approximately 2. 5% of patients. Infectious complications requiring hospitalization are seen in <1% of patients who are properly medicated with antibiotics before biopsy. Back to case
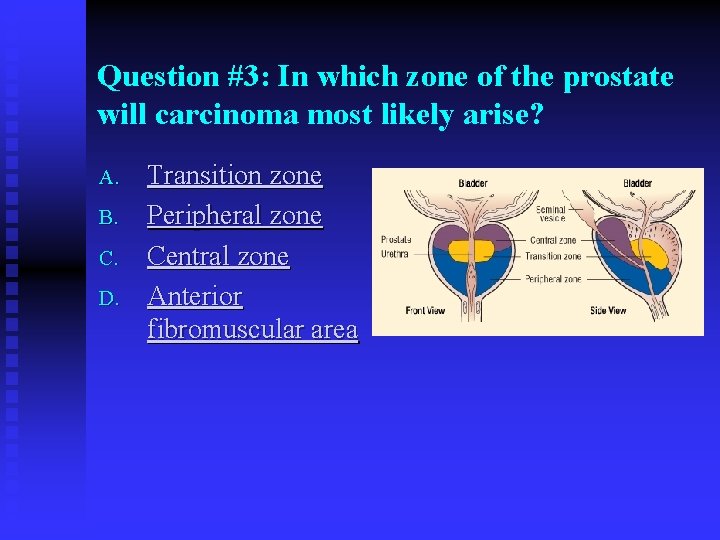
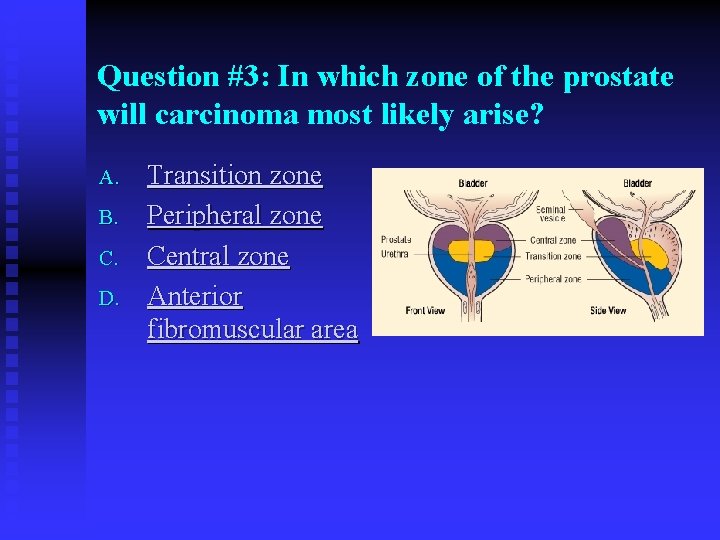
Question #3: In which zone of the prostate will carcinoma most likely arise? A. B. C. D. Transition zone Peripheral zone Central zone Anterior fibromuscular area
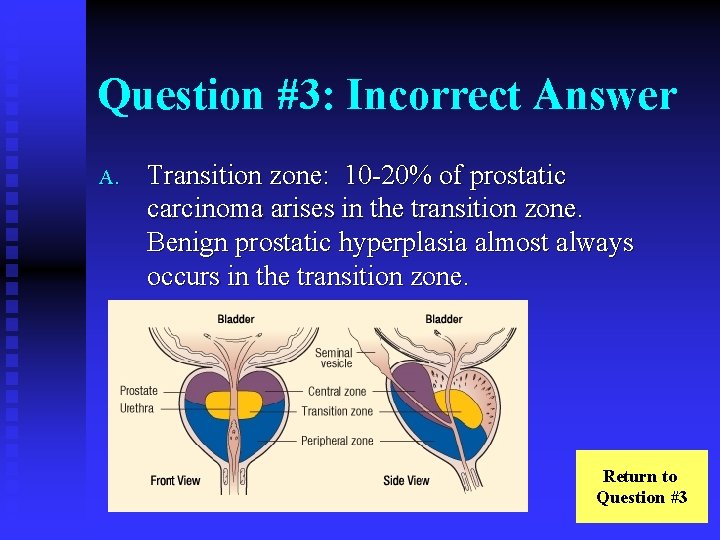
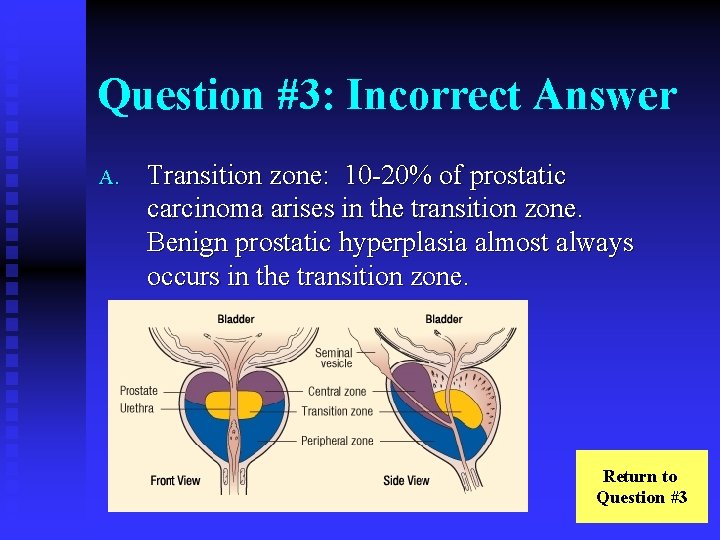
Question #3: Incorrect Answer A. Transition zone: 10 -20% of prostatic carcinoma arises in the transition zone. Benign prostatic hyperplasia almost always occurs in the transition zone. Return to Question #3

Question #3: Correct Answer B. Peripheral zone: 65 -70% of prostatic carcinoma arises in the peripheral zone. The peripheral zone can be palpated on digital rectal exam (DRE), making DRE a useful screening tool for prostate cancer. Continue case
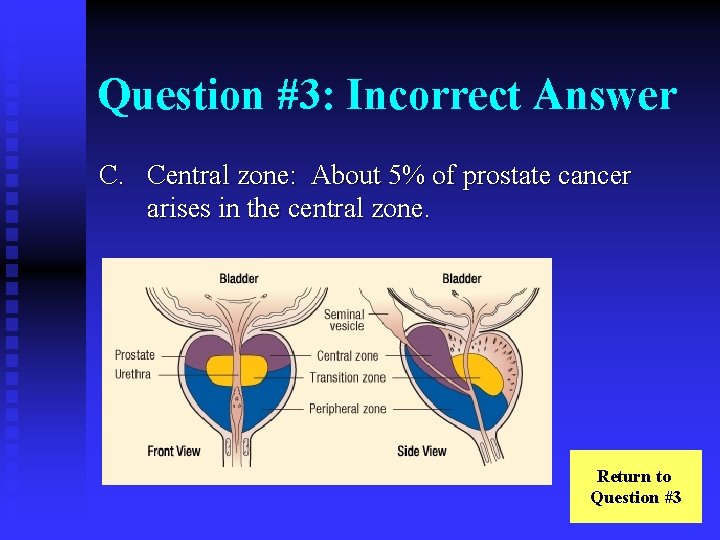
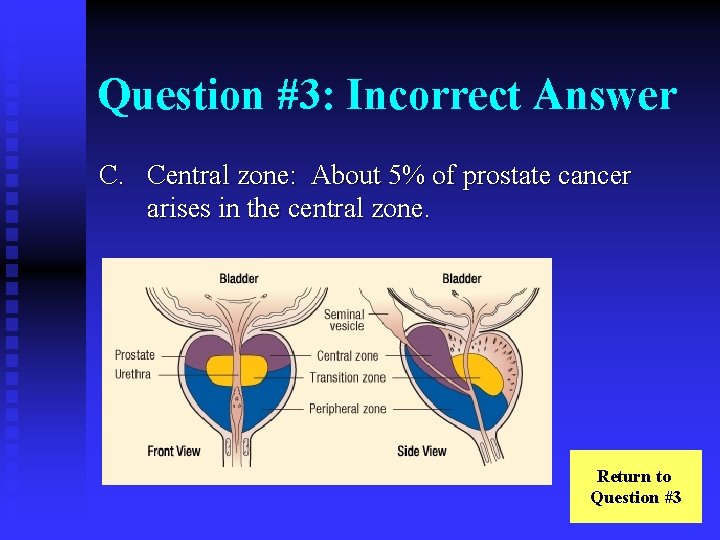
Question #3: Incorrect Answer C. Central zone: About 5% of prostate cancer arises in the central zone. Return to Question #3

Question #3: Incorrect Answer D. Anterior fibromuscular area: Prostatic cancer rarely arises in the anterior fibromuscular area. Return to Question #3
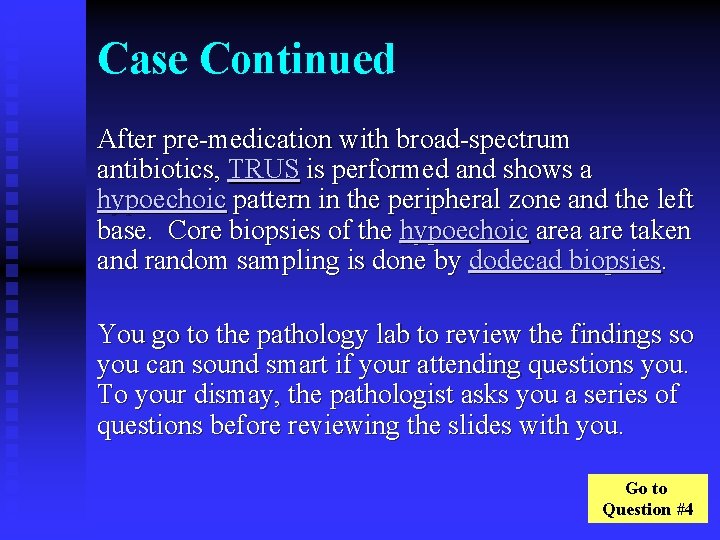
Case Continued After pre-medication with broad-spectrum antibiotics, TRUS is performed and shows a hypoechoic pattern in the peripheral zone and the left base. Core biopsies of the hypoechoic area are taken and random sampling is done by dodecad biopsies. You go to the pathology lab to review the findings so you can sound smart if your attending questions you. To your dismay, the pathologist asks you a series of questions before reviewing the slides with you. Go to Question #4
Question #4: If Mr. State has cancer of the prostate, which is the most likely histology? A. B. C. D. Small cell carcinoma Sarcoma Adenocarcinoma Transitional cell carcinoma

Question #4: Incorrect Answer A. Small cell carcinoma: Small cell carcinomas account for less than 1% of prostate cancer. Return to Question #4
Question #4: Incorrect Answer B. Sarcoma: Sarcomas account for less than 1% of prostate cancer. Return to Question #4
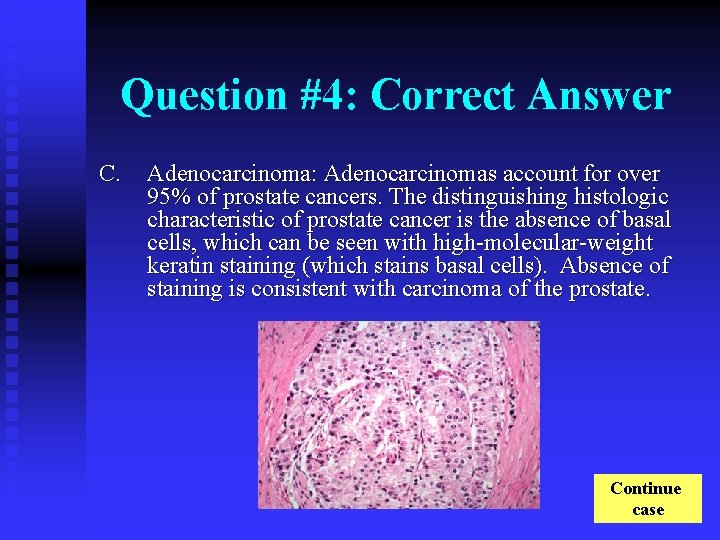
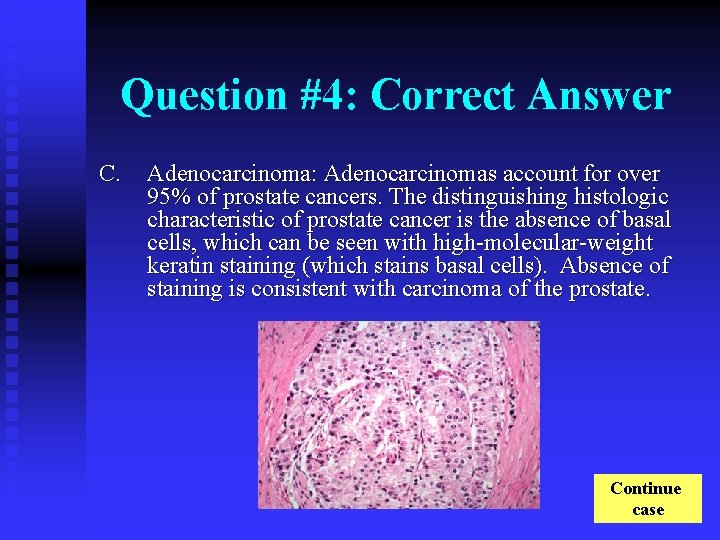
Question #4: Correct Answer C. Adenocarcinoma: Adenocarcinomas account for over 95% of prostate cancers. The distinguishing histologic characteristic of prostate cancer is the absence of basal cells, which can be seen with high-molecular-weight keratin staining (which stains basal cells). Absence of staining is consistent with carcinoma of the prostate. Continue case
Question #4: Incorrect Answer D. Transitional cell carcinoma: Transitional cell carcinomas account for approximately 4% of prostate cancer. They do account for over 90% of bladder cancer. Return to Question #4

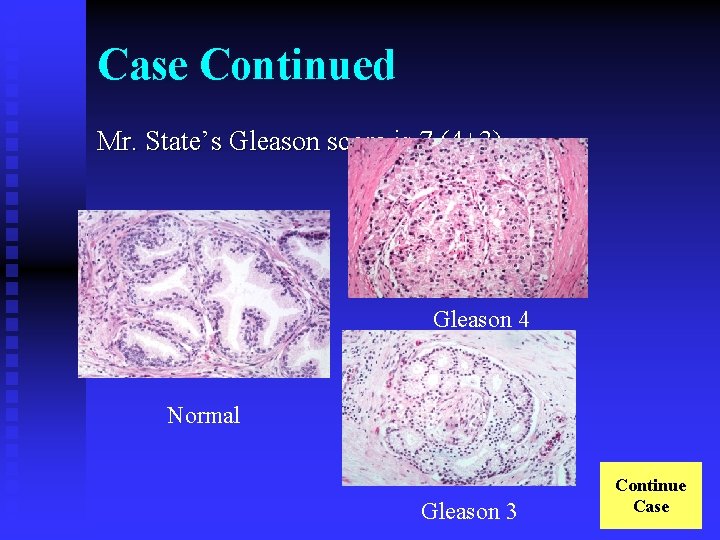
Case Continued Upon viewing the slides with the pathologist, you note a basophilic cytoplasm with enlarged, hyperchromatic nuclei with enlarged nucleoli. You ask the pathologist if she has stained the cells with high-molecular-weight keratin and, impressed by your knowledge, she says she has and points out the absence of staining where the basal cell layer is normally found. The pathologist asks how prostatic cancer is graded. After you correctly identify the Gleason grading system, she asks about the significance of different Gleason scores. Go to Question #5
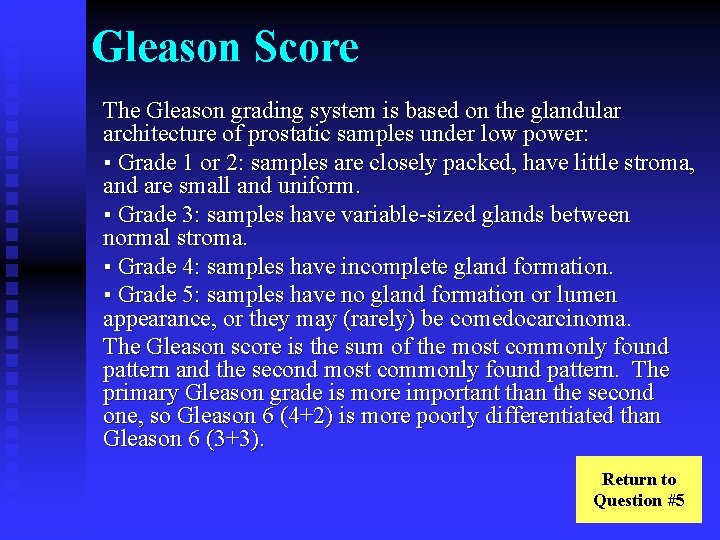
Gleason Score The Gleason grading system is based on the glandular architecture of prostatic samples under low power: ▪ Grade 1 or 2: samples are closely packed, have little stroma, and are small and uniform. ▪ Grade 3: samples have variable-sized glands between normal stroma. ▪ Grade 4: samples have incomplete gland formation. ▪ Grade 5: samples have no gland formation or lumen appearance, or they may (rarely) be comedocarcinoma. The Gleason score is the sum of the most commonly found pattern and the second most commonly found pattern. The primary Gleason grade is more important than the second one, so Gleason 6 (4+2) is more poorly differentiated than Gleason 6 (3+3). Return to Question #5

Question #5: What Gleason score would suggest that Mr. State’s cancer is poorly differentiated? A. B. C. D. Gleason 2 (1+1) Gleason 4 (2+2) Gleason 6 (3+3) Gleason 10 (5+5)

Question #5: Incorrect Answer A. Gleason 2 (1+1): Gleason 2 (1+1) is considered very well-differentiated. Normal Gleason 1 Return to Question #5
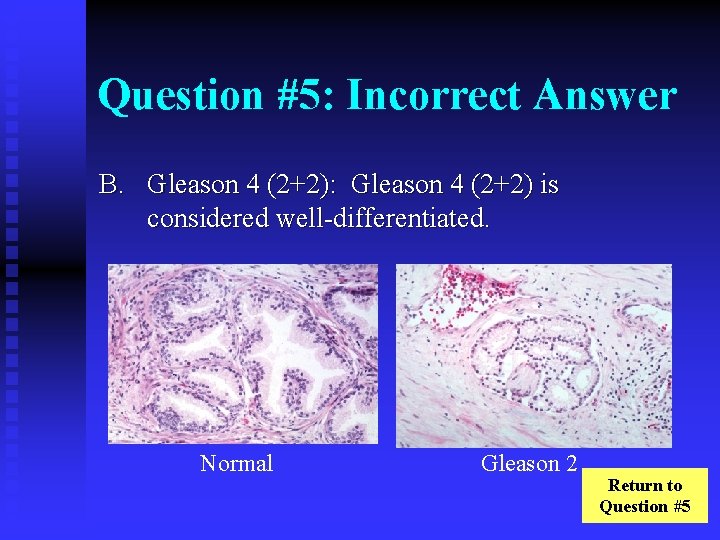
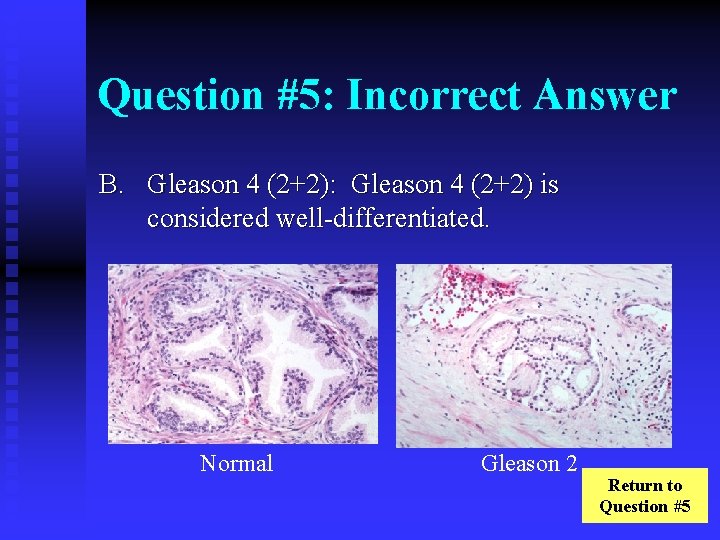
Question #5: Incorrect Answer B. Gleason 4 (2+2): Gleason 4 (2+2) is considered well-differentiated. Normal Gleason 2 Return to Question #5

Question #5: Incorrect Answer C. Gleason 6 (3+3): Gleason 5 -6 is considered moderately differentiated. The primary Gleason grade is more important than the second one, so Gleason 6 (4+2) is more poorly differentiated than Gleason 6 (3+3). Normal Gleason 3 Return to Question #5
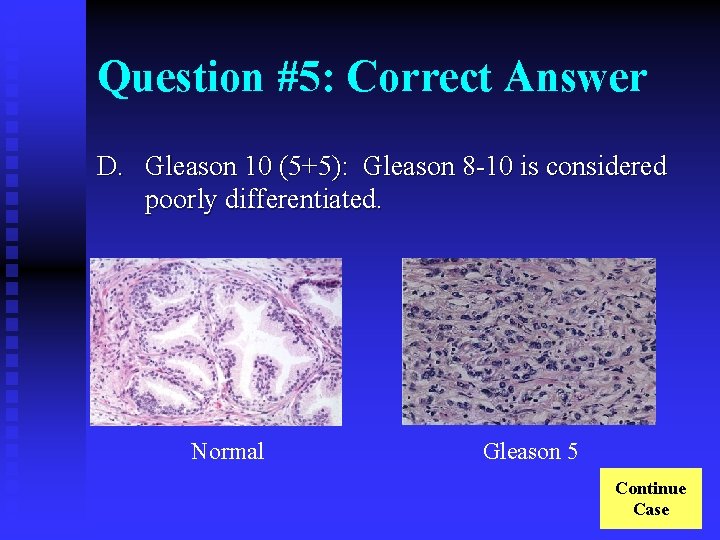
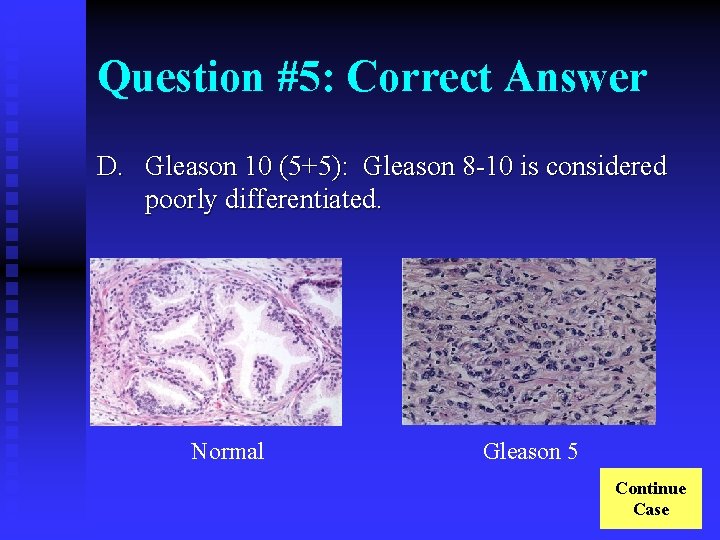
Question #5: Correct Answer D. Gleason 10 (5+5): Gleason 8 -10 is considered poorly differentiated. Normal Gleason 5 Continue Case
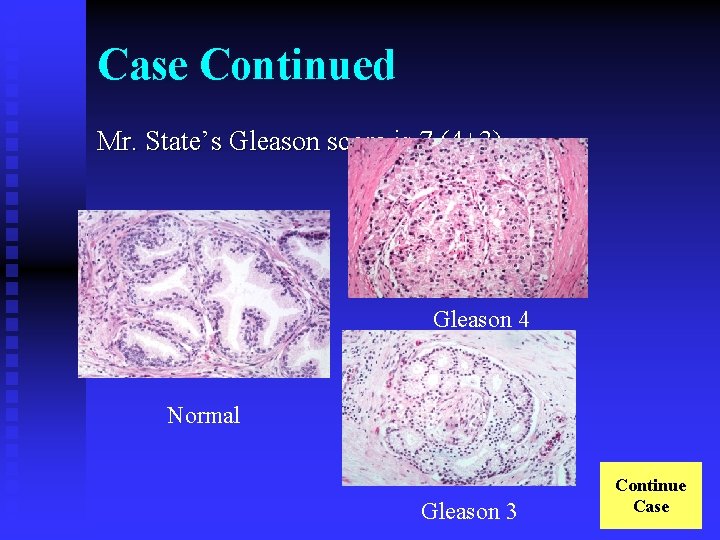
Case Continued Mr. State’s Gleason score is 7 (4+3). Gleason 4 Normal Gleason 3 Continue Case
Case Continued Mr. State now inquires about the clinical stage of his prostate cancer. Go to Question #6
Question #6: Evidence supports the usefulness of which of the following possible staging modalities for localized prostate cancer? A. B. C. D. E. Pelvic CT PSA Digital Rectal Exam (DRE) Trans-rectal ultrasound Radionuclide bone scan
Question #6: Incorrect Answer A. Pelvic CT: Pelvic CT is rarely used to assess whether pelvic lymph nodes are enlarged, a finding that would suggest possible nodal metastasis. Because lymph node metastasis is exceedingly rare with Gleason score ≤ 7 and PSA < 10, pelvic CT is not routinely done with these values unless clinically indicated. Return to Question #6
Question #6: Incorrect Answer B. PSA: Serum PSA correlates very roughly with tumor extent. Return to Question #6
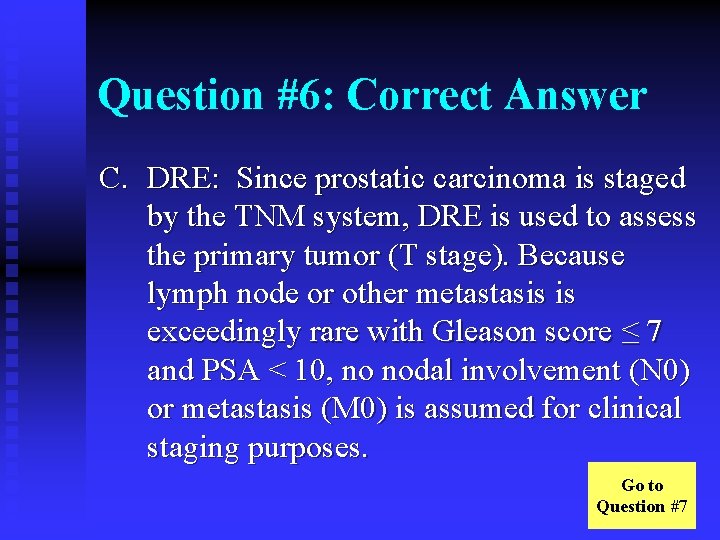
Question #6: Correct Answer C. DRE: Since prostatic carcinoma is staged by the TNM system, DRE is used to assess the primary tumor (T stage). Because lymph node or other metastasis is exceedingly rare with Gleason score ≤ 7 and PSA < 10, no nodal involvement (N 0) or metastasis (M 0) is assumed for clinical staging purposes. Go to Question #7
Question #6: Incorrect Answer D. Trans-rectal ultrasound (TRUS): TRUS is typically used to direct biopsy, not for staging. Return to Question #6

Question #6: Incorrect Answer E. Radionuclide bone scan: Bony metastases are rare with a PSA < 20 ng/m. L. Although radionuclide bone scanning is very sensitive to detect bony metastasis, it is not routinely done with a PSA < 10 if the Gleason score is ≤ 7. Return to Question #6
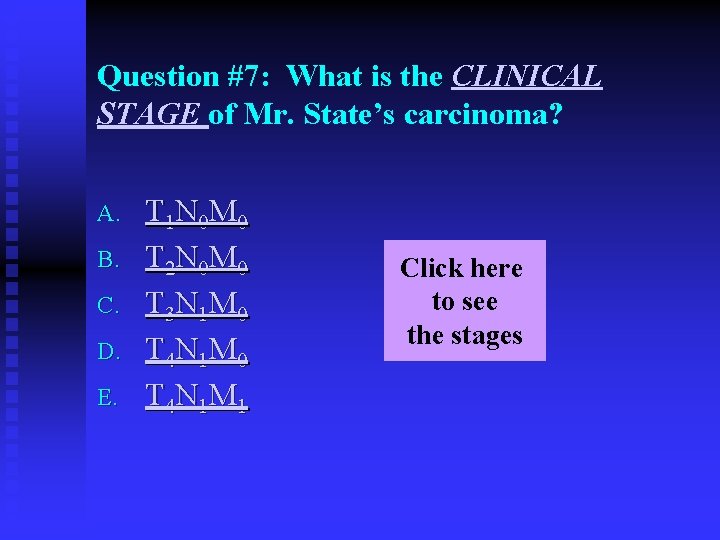
Question #7: What is the CLINICAL STAGE of Mr. State’s carcinoma? A. B. C. D. E. T 1 N 0 M 0 T 2 N 0 M 0 T 3 N 1 M 0 T 4 N 1 M 1 Click here to see the stages
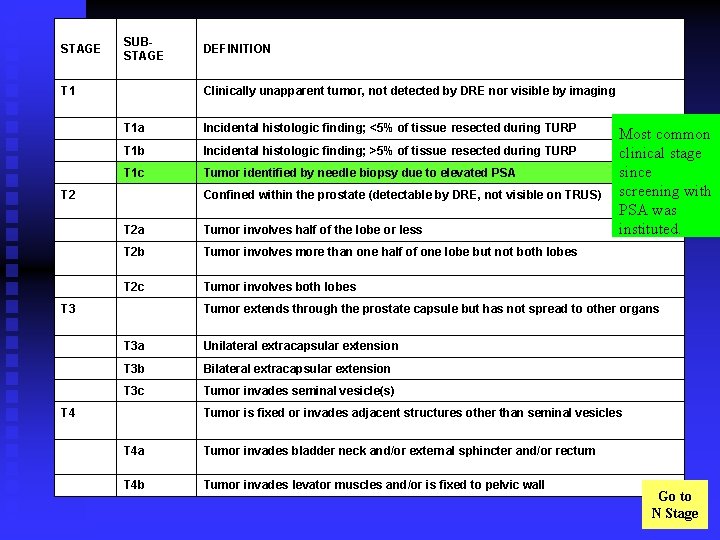
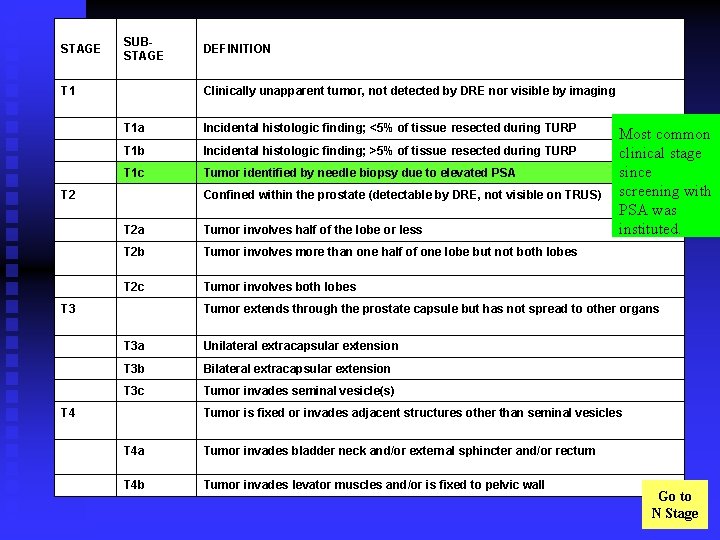
STAGE SUBSTAGE DEFINITION T 1 Clinically unapparent tumor, not detected by DRE nor visible by imaging T 1 a Incidental histologic finding; <5% of tissue resected during TURP T 1 b Incidental histologic finding; >5% of tissue resected during TURP T 1 c Tumor identified by needle biopsy due to elevated PSA T 2 Confined within the prostate (detectable by DRE, not visible on TRUS) T 2 a Tumor involves half of the lobe or less T 2 b Tumor involves more than one half of one lobe but not both lobes T 2 c Tumor involves both lobes T 3 Tumor extends through the prostate capsule but has not spread to other organs T 3 a Unilateral extracapsular extension T 3 b Bilateral extracapsular extension T 3 c Tumor invades seminal vesicle(s) T 4 Tumor is fixed or invades adjacent structures other than seminal vesicles T 4 a Tumor invades bladder neck and/or external sphincter and/or rectum T 4 b Tumor invades levator muscles and/or is fixed to pelvic wall Most common clinical stage since screening with PSA was instituted. Go to N Stage
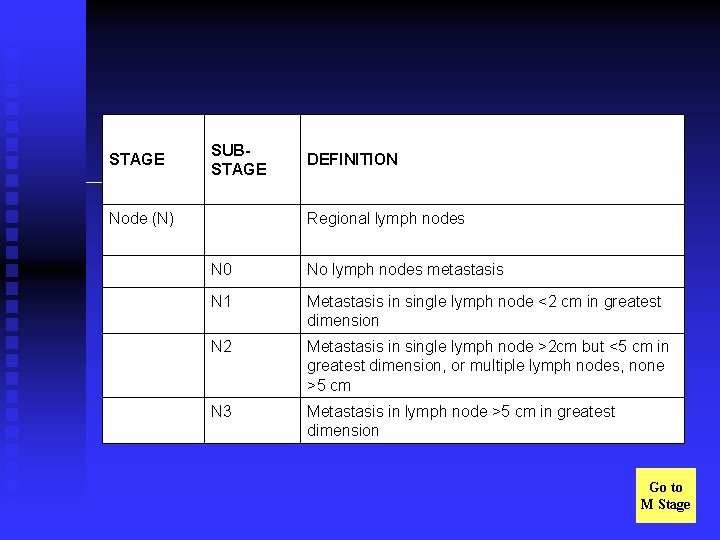
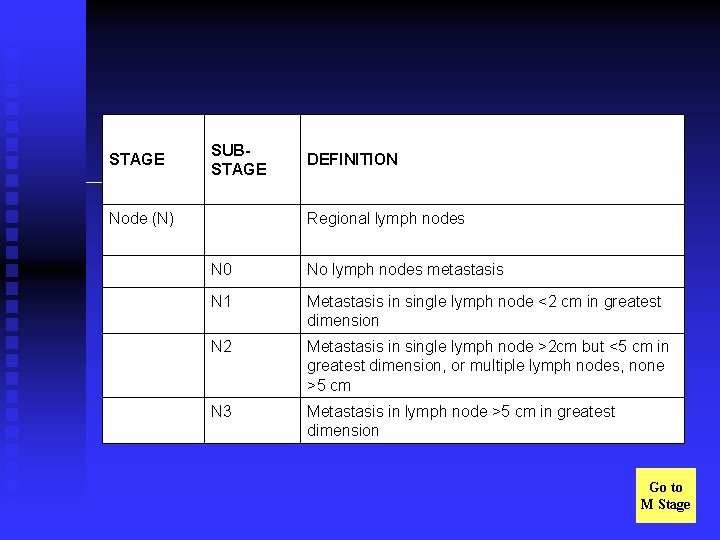
STAGE SUBSTAGE DEFINITION Node (N) Regional lymph nodes N 0 No lymph nodes metastasis N 1 Metastasis in single lymph node <2 cm in greatest dimension N 2 Metastasis in single lymph node >2 cm but <5 cm in greatest dimension, or multiple lymph nodes, none >5 cm N 3 Metastasis in lymph node >5 cm in greatest dimension Go to M Stage
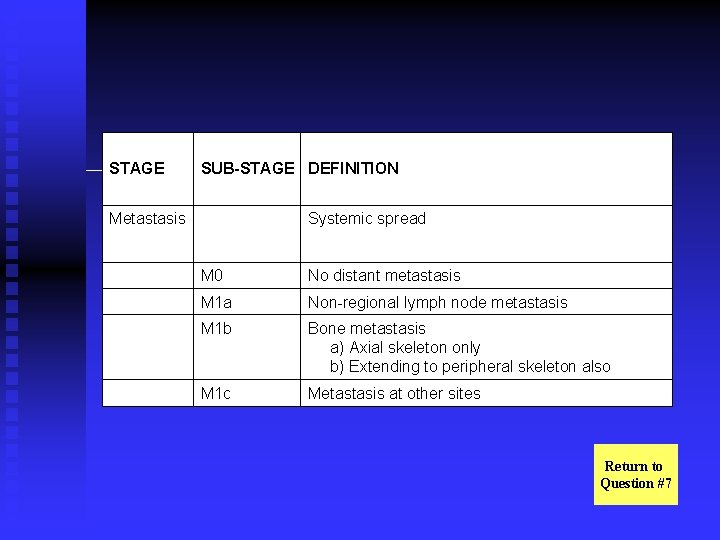
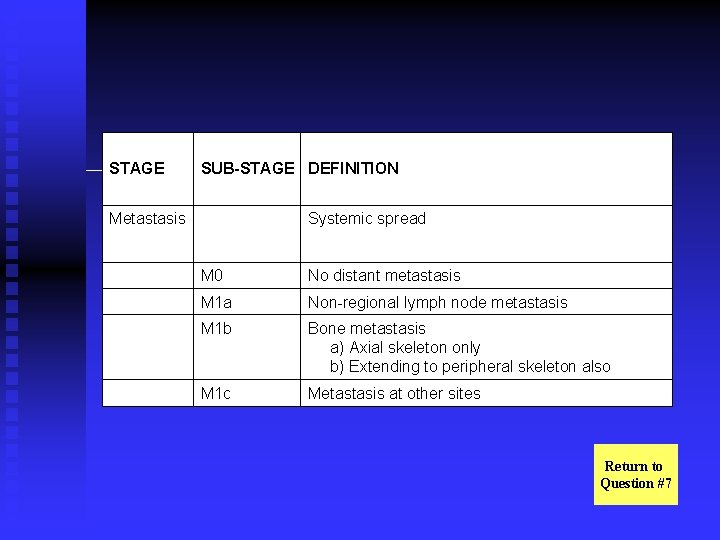
STAGE SUB-STAGE DEFINITION Metastasis Systemic spread M 0 No distant metastasis M 1 a Non-regional lymph node metastasis M 1 b Bone metastasis a) Axial skeleton only b) Extending to peripheral skeleton also M 1 c Metastasis at other sites Return to Question #7
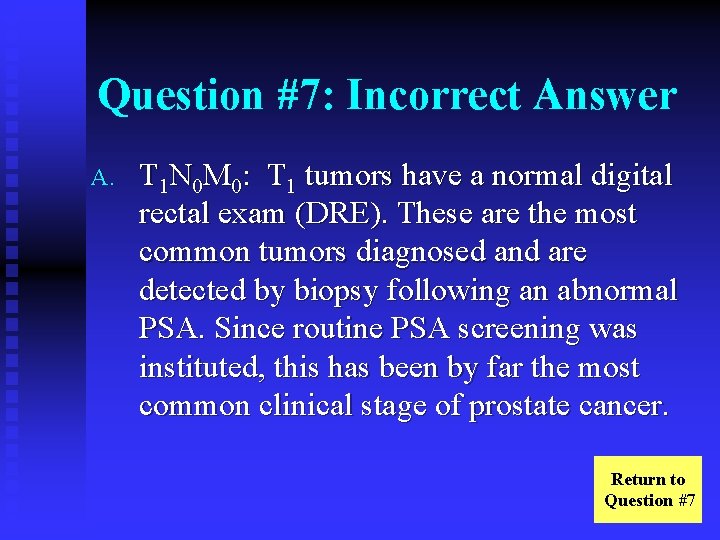
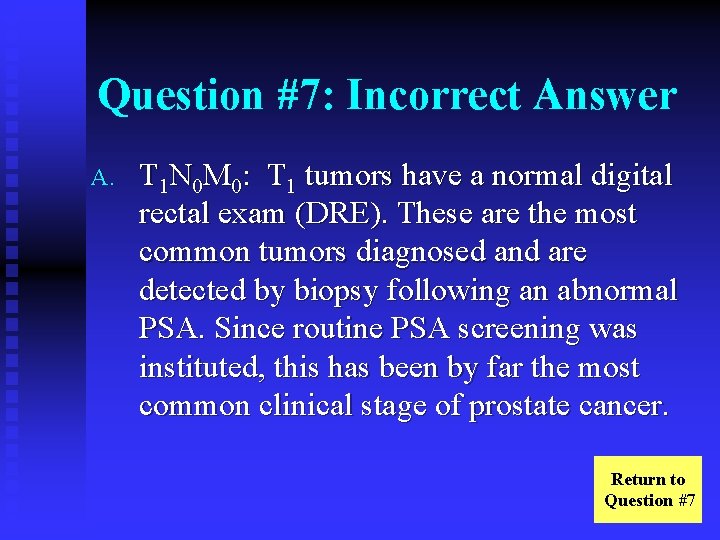
Question #7: Incorrect Answer A. T 1 N 0 M 0: T 1 tumors have a normal digital rectal exam (DRE). These are the most common tumors diagnosed and are detected by biopsy following an abnormal PSA. Since routine PSA screening was instituted, this has been by far the most common clinical stage of prostate cancer. Return to Question #7
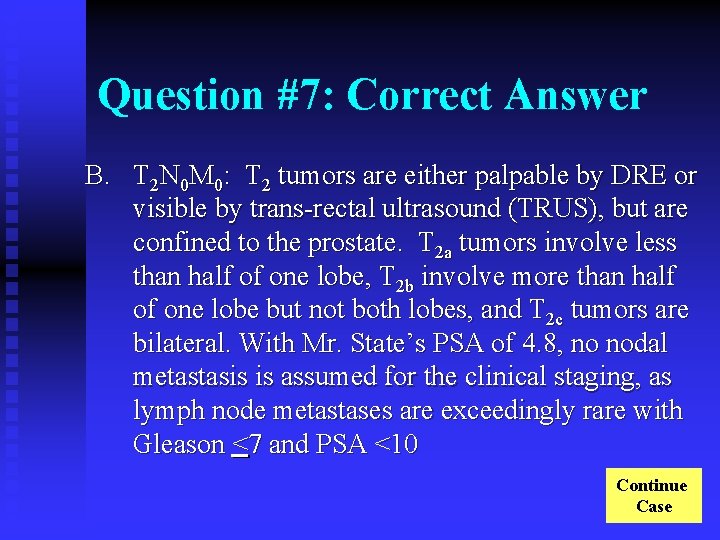
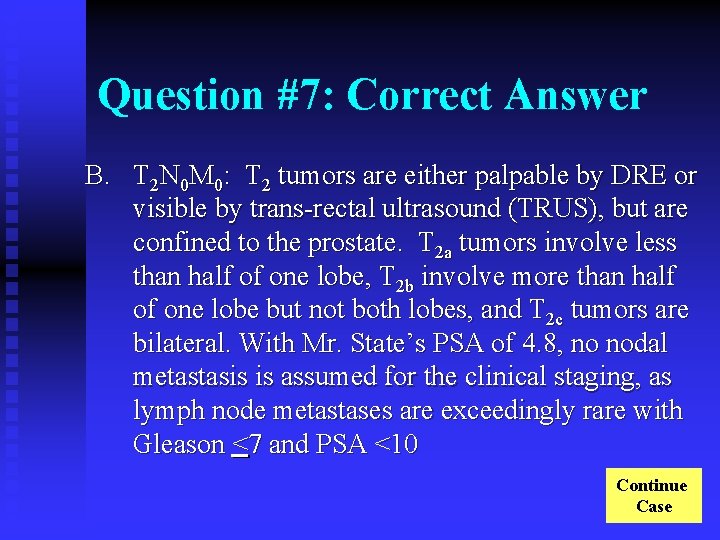
Question #7: Correct Answer B. T 2 N 0 M 0: T 2 tumors are either palpable by DRE or visible by trans-rectal ultrasound (TRUS), but are confined to the prostate. T 2 a tumors involve less than half of one lobe, T 2 b involve more than half of one lobe but not both lobes, and T 2 c tumors are bilateral. With Mr. State’s PSA of 4. 8, no nodal metastasis is assumed for the clinical staging, as lymph node metastases are exceedingly rare with Gleason <7 and PSA <10 Continue Case
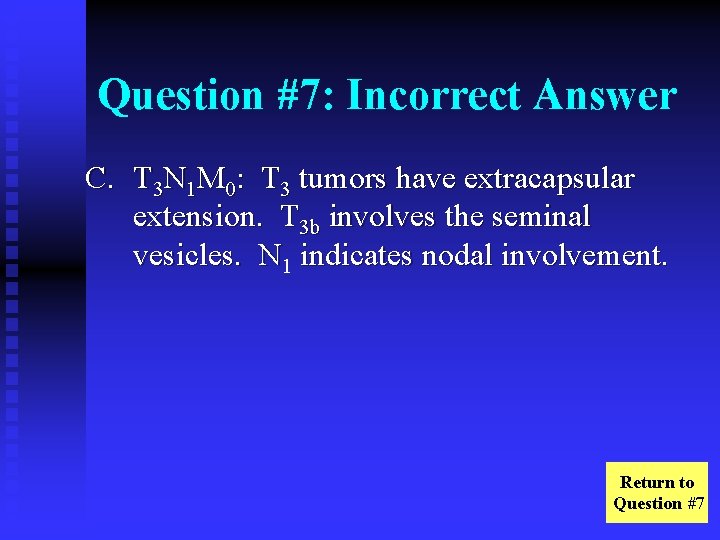
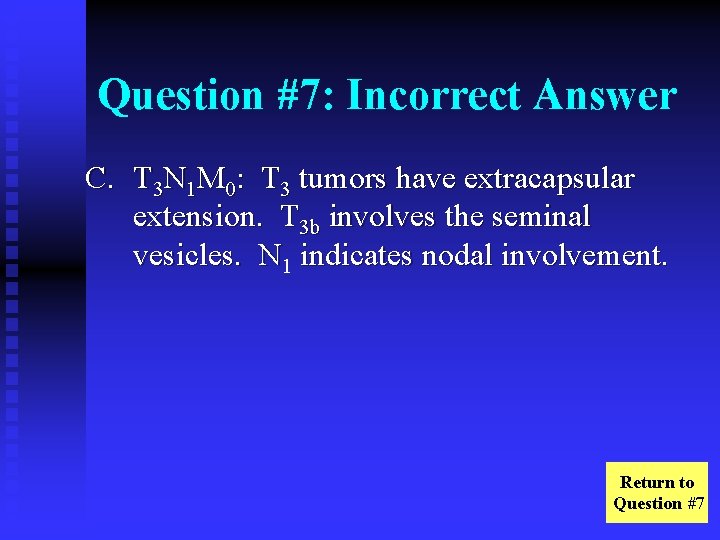
Question #7: Incorrect Answer C. T 3 N 1 M 0: T 3 tumors have extracapsular extension. T 3 b involves the seminal vesicles. N 1 indicates nodal involvement. Return to Question #7
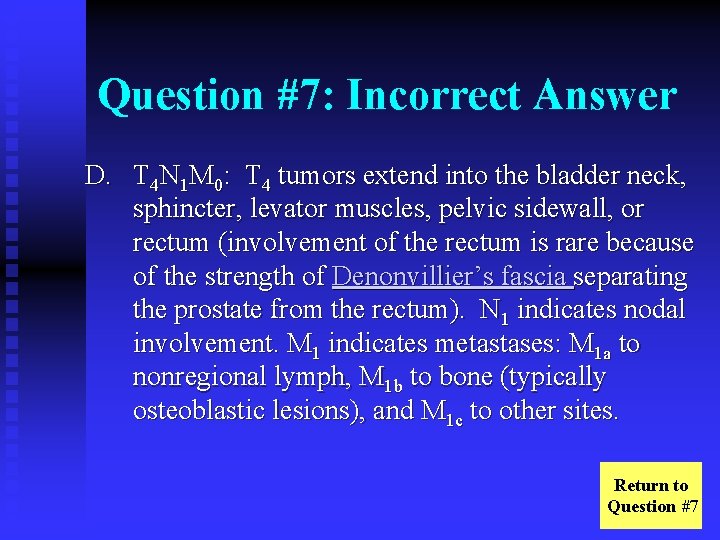
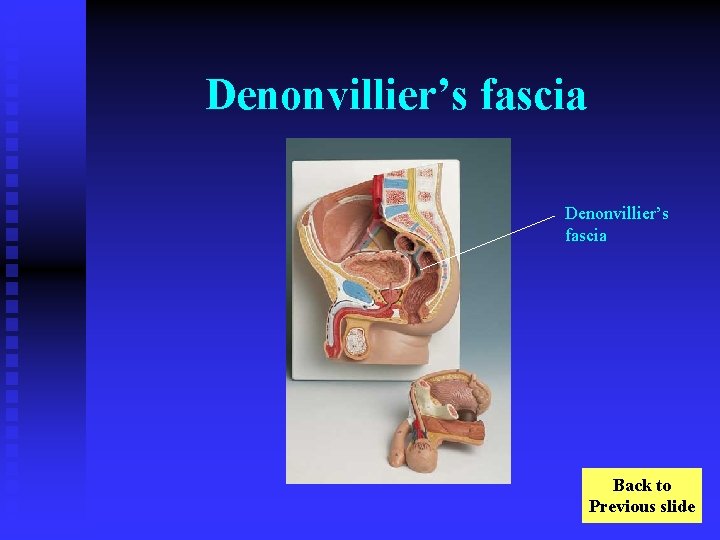
Question #7: Incorrect Answer D. T 4 N 1 M 0: T 4 tumors extend into the bladder neck, sphincter, levator muscles, pelvic sidewall, or rectum (involvement of the rectum is rare because of the strength of Denonvillier’s fascia separating the prostate from the rectum). N 1 indicates nodal involvement. M 1 indicates metastases: M 1 a to nonregional lymph, M 1 b to bone (typically osteoblastic lesions), and M 1 c to other sites. Return to Question #7
Question #7: Incorrect Answer E. T 4 N 1 M 1: T 4 tumors extend into the bladder neck, sphincter, rectum, levator muscles, or pelvic sidewall. N 1 indicates nodal involvement. Return to Question #7
Case Continued Mr. State inquires about his different treatment options. You explain that the major categorical options include watchful waiting, radiation therapy, and radical prostatectomy. You recommend the National Cancer Institute (NCI) website discussion on treatment options. http: //www. nci. nih. gov/cancertopics/understanding-prostate-cancertreatment/page 5 Continue Case
Case Continued At this time, he has normal erections sufficient for penetration and no urinary incontinence. Despite his high-fat diet, his lipid panel is within normal limits and he has no other cardiovascular risk factors other than smoking and obesity (BMI 32). On review of systems, he appears to be in good health. Continue Case

Case Continued Mr. State is not enthusiastic about surgery or radiation and says “Doc, if I just wait and don’t do anything else, won’t I die of something else before the prostate cancer gets me? ” Go to Question #8
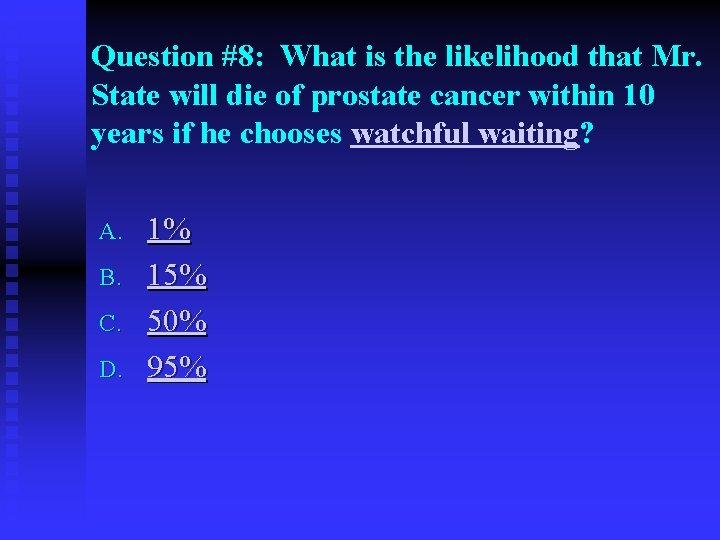
Question #8: What is the likelihood that Mr. State will die of prostate cancer within 10 years if he chooses watchful waiting? A. B. C. D. 1% 15% 50% 95%
Question #8: Incorrect Answer A. 1%: Very few prostate cancers are indolent enough to have a 10 year diseasespecific mortality of ≤ 1% Return to Question #8
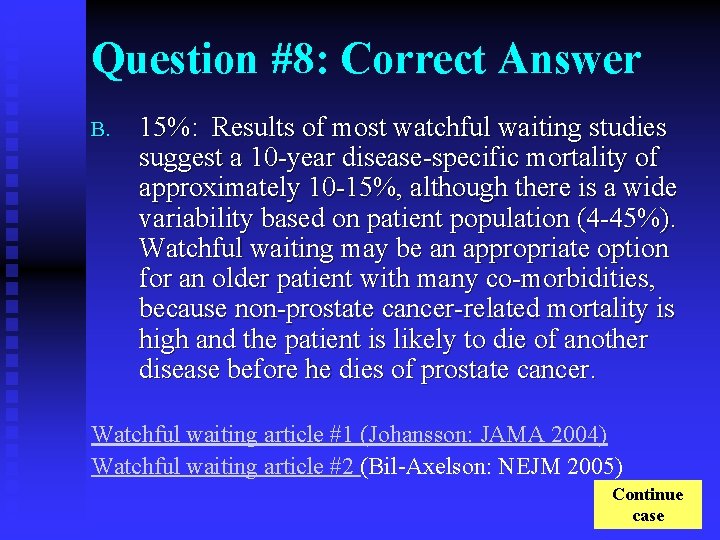
Question #8: Correct Answer B. 15%: Results of most watchful waiting studies suggest a 10 -year disease-specific mortality of approximately 10 -15%, although there is a wide variability based on patient population (4 -45%). Watchful waiting may be an appropriate option for an older patient with many co-morbidities, because non-prostate cancer-related mortality is high and the patient is likely to die of another disease before he dies of prostate cancer. Watchful waiting article #1 (Johansson: JAMA 2004) Watchful waiting article #2 (Bil-Axelson: NEJM 2005) Continue case
Question #8: Incorrect Answer C. 50%: While some prostate cancers are aggressive enough to result in diseasespecific death within 10 years, most are less aggressive. Return to Question #8
Question #8: Incorrect Answer D. 95%: Very few prostate cancers are aggressive enough to have a 10 year disease-specific mortality of ≥ 95% Return to Question #8
Case Continued After hearing your discussion of the watchful waiting option, Mr. State wants to know more about radiation therapy. A family friend who had prostate cancer 10 years ago and was treated with external beam therapy had terrible side-effects and discontinued treatment before completing the entire course. His cancer recurred within 5 years and he passed away. Mr. State is concerned about the side-effects of radiation therapy. Radiation therapy article (Nilsson, Acta Oncol, 2004) Go to Question #9
Question #9: Which of the following are potential complications of radiation treatment? A. B. C. D. E. Frequency Fatigue Impotence Bowel bother All of the above

Question #9: Incorrect Answer A. Frequency: Most patients experience urinary frequency and dysuria. Over 90% of these cases, however, resolve within one year. Back to Question #9

Question #9: Incorrect Answer B. Fatigue: The degree of fatigue is variable, but significant in up to 75% of patients during radiation treatment. Within 2 -3 months of treatment completion, most patients return to baseline energy levels. Back to Question #9
Question #9: Incorrect Answer C. Impotence: Impotence has been reported in up to 35 -40% of patients. Back to Question #9
Question #9: Incorrect Answer D. Bowel bother: Mild, self-limited rectal bleeding is present in approximately 10% of patients. Back to Question #9

Question #9: Correct Answer E. All of the above. Frequency, fatigue, impotence, and bowel bother are all potential side-effects of radiation therapy. Continue Case

Case Continued Mr. State now inquires about survival rates after radiation therapy. Go to Question # 10
Question #10: What are overall and disease-specific 10 -year survival after radiation therapy? A. B. C. 80% and 90%, respectively 60% and 70%, respectively 40% and 50%, respectively
Question #10: Correct Answer A. 80% & 90%: Overall 10 -year survival after radiation therapy is approximately 80%. Disease-specific survival is approximately 90%. These results indicate that approximately 20% of patients with prostate cancer treated with radiation therapy die within 10 years, with half (10%) dying of prostate cancer. Continue Case
Question #10: Incorrect Answer B. 60% & 70%: Both overall and diseasespecific 10 -year survival are significantly better than 60% and 70%, respectively. Return to Question #10
Question #10: Incorrect Answer C. 40% & 50%: Both overall and diseasespecific 10 -year survival are significantly better than 40% and 50%, respectively. . Return to Question #10
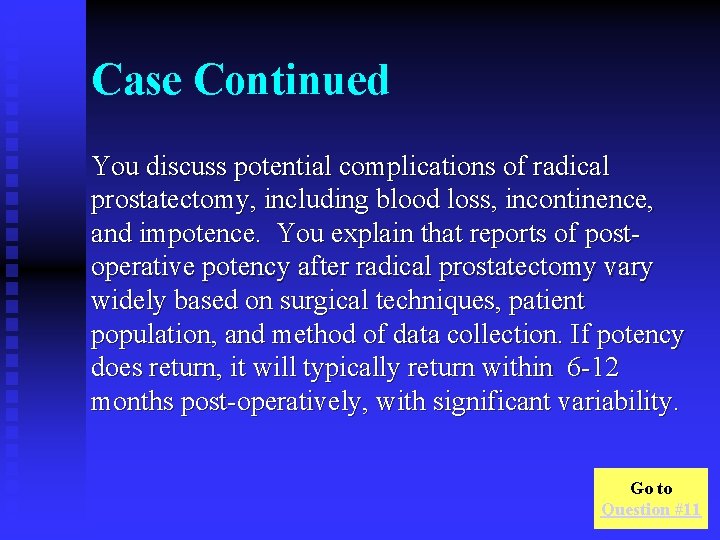
Case Continued Mr. State now wants to know more about radical prostatectomy. You explain that the procedure entails a 2 -3 hour operation that generally requires a 2 -3 day hospital stay. He will be able to donate autologous units of blood to minimize the likelihood of transfusion reaction if transfusion becomes necessary. He will have a catheter to drain his bladder for the first 7 -10 days after surgery. Continue Case
Case Continued You discuss potential complications of radical prostatectomy, including blood loss, incontinence, and impotence. You explain that reports of postoperative potency after radical prostatectomy vary widely based on surgical techniques, patient population, and method of data collection. If potency does return, it will typically return within 6 -12 months post-operatively, with significant variability. Go to Question #11
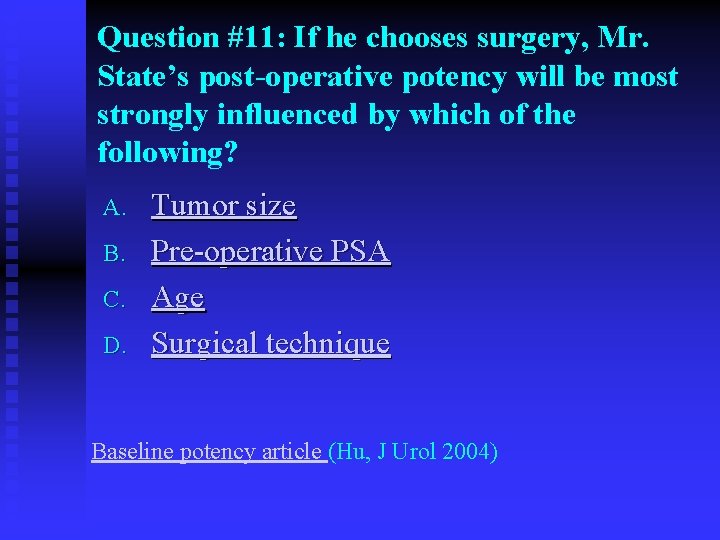
Question #11: If he chooses surgery, Mr. State’s post-operative potency will be most strongly influenced by which of the following? A. B. C. D. Tumor size Pre-operative PSA Age Surgical technique Baseline potency article (Hu, J Urol 2004)
Question #11: Incorrect Answer A. Tumor size: Tumor size correlates very roughly with post-operative potency. Extremely large tumors, however, are associated with a higher likelihood of capsular penetration, often precluding nerve-sparing operative techniques. Return to Question #11
Question #11: Incorrect Answer B. Pre-operative PSA: Pre-operative PSA correlates very roughly with post-operative potency. PSA>10, however, is associated with a higher likelihood of capsular penetration, often precluding nerve-sparing operative techniques. Return to Question #11
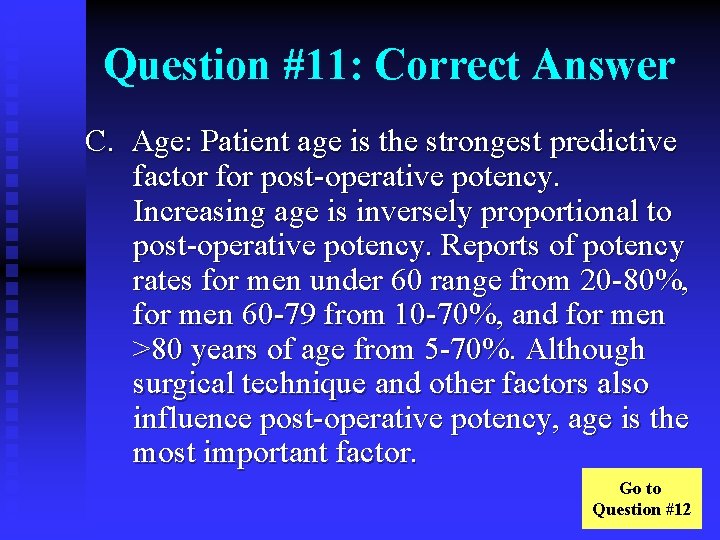
Question #11: Correct Answer C. Age: Patient age is the strongest predictive factor for post-operative potency. Increasing age is inversely proportional to post-operative potency. Reports of potency rates for men under 60 range from 20 -80%, for men 60 -79 from 10 -70%, and for men >80 years of age from 5 -70%. Although surgical technique and other factors also influence post-operative potency, age is the most important factor. Go to Question #12
Question #11: Incorrect Answer D. Surgical technique: Reports of potency rates for men under 60 after bilateral nervesparing operations range from 40 -80%, but drop to 20 -60% after unilateral nervesparing operations. The respective rates are 25 -75% and 10 -50% in men over the age of 60. Surgical technique is not the strongest predictor of post-operative potency. Return to Question #11
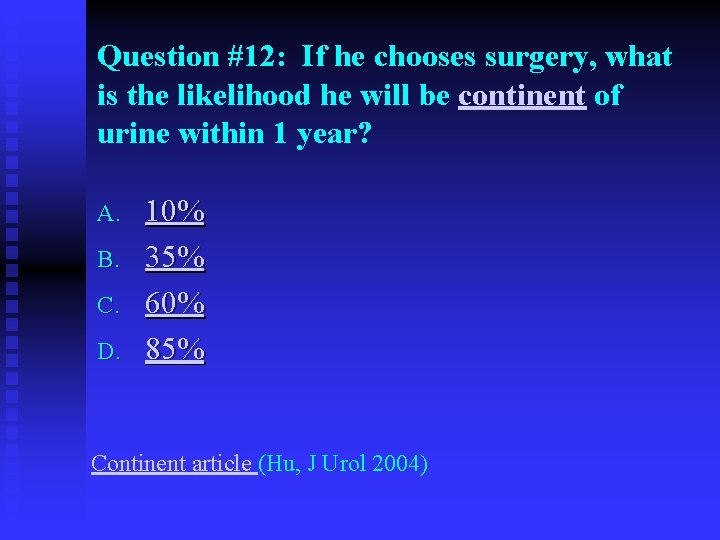
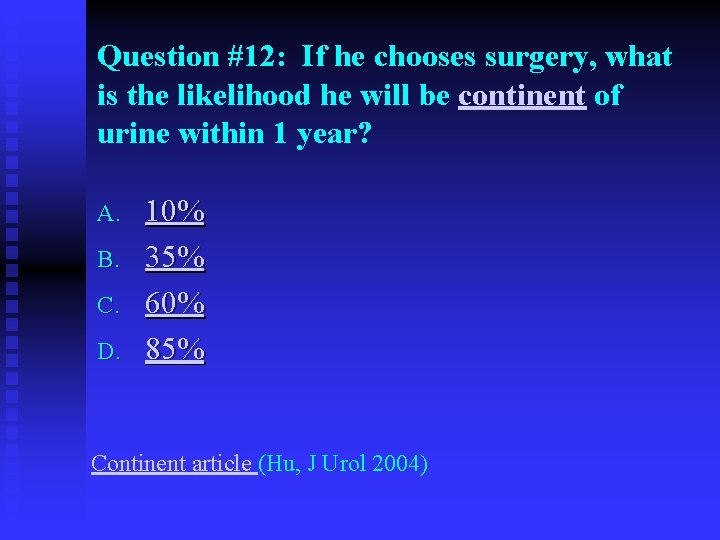
Question #12: If he chooses surgery, what is the likelihood he will be continent of urine within 1 year? A. B. C. D. 10% 35% 60% 85% Continent article (Hu, J Urol 2004)

Question #12: Incorrect Answer A. 10%: Most patients are continent of urine within 1 year. Return to Question #12
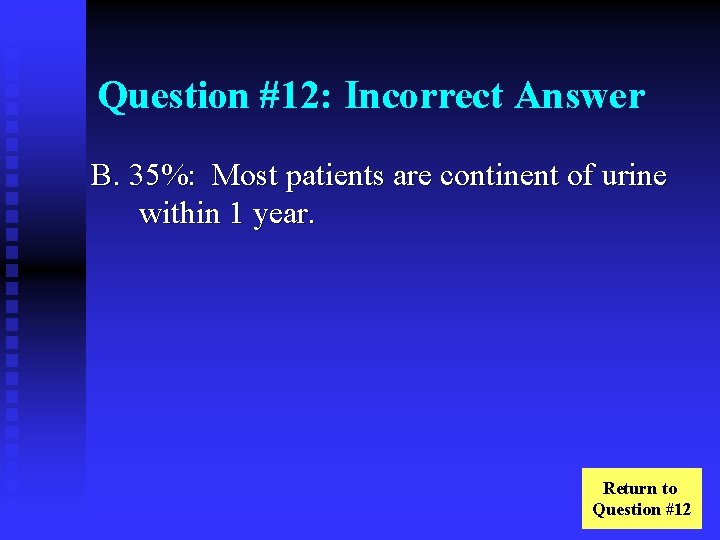
Question #12: Incorrect Answer B. 35%: Most patients are continent of urine within 1 year. Return to Question #12
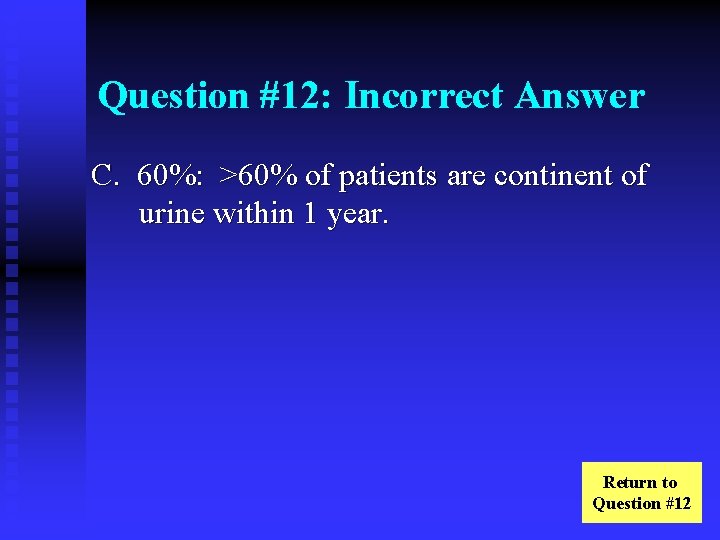
Question #12: Incorrect Answer C. 60%: >60% of patients are continent of urine within 1 year. Return to Question #12
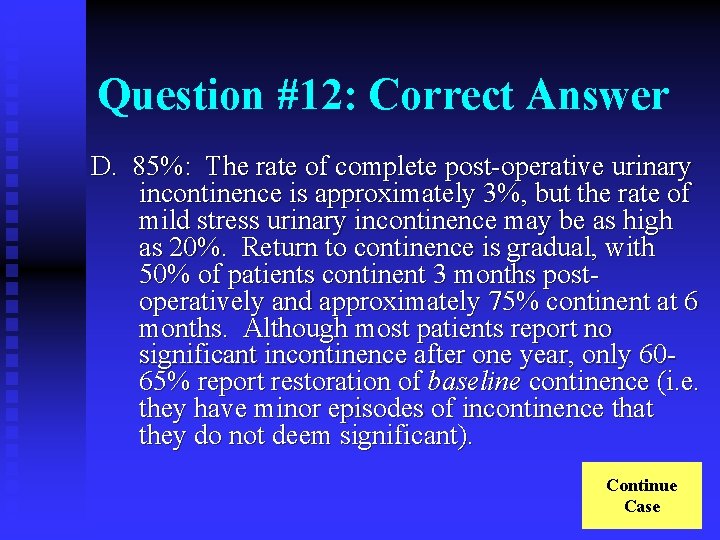
Question #12: Correct Answer D. 85%: The rate of complete post-operative urinary incontinence is approximately 3%, but the rate of mild stress urinary incontinence may be as high as 20%. Return to continence is gradual, with 50% of patients continent 3 months postoperatively and approximately 75% continent at 6 months. Although most patients report no significant incontinence after one year, only 6065% report restoration of baseline continence (i. e. they have minor episodes of incontinence that they do not deem significant). Continue Case
Case Continued Based on Mr. States clinical exam, PSA and biopsy results you use a Partin table to determine there is a 67% likelihood his prostate cancer is confined to the prostate. Continue Case
Case Continued Mr. State chooses to undergo radical prostatectomy. His final surgical pathology is Gleason (4+3=7) confined to the prostate. Go to Question #13
Question #13: In this patient, what is the likelihood of disease-free 10 year survival? A. B. C. D. 40% 60% 80% 95% Disease-free 10 year survival article (Roehl, J Urol 2004)
Question #13: Incorrect Answer A. 40%: Patients with extensive extracapsular extension have 70% 5 -year disease-free survival rates and 40% 10 -year survival rates. Return to Question #13
Question #13: Incorrect Answer B. 60%: Because he does not have extracapsular extension, the probability of disease-free 10 year survival is better than 60%. Return to Question #13

Question #13: Correct Answer C. 80%: Patients with organ-confined prostate cancer have approximately 80% 10 -year disease-free survival rates. Continue Case
Question #13: Incorrect Answer D. 95%: Even if he had extracapsular extension there would be a >5% possibility of disease-specific 10 year mortality. Return to Question #13
Case Continued Mr. State does well after surgery. His catheter is removed 10 days post-operatively and his wounds are well-healed. You schedule a follow-up appointment for 3 months. Continue Case
Case Continued Mr. State comes for a 3 month follow-up. He has occasional loss of urine when he plays tennis, but is otherwise fully continent. He has begun having satisfactory erections again. You discuss cancer surveillance. Go to Question #14

Question #14: What is the best way to test for recurrence of Mr. State’s prostate cancer? A. B. C. D. Bone scan PSA Chest X-ray Physical exam
Question #14: Incorrect Answer A. Bone scan: Unnecessary due to the low likelihood of bone metastasis. Return to Question #14
Question #14: Correct Answer B. PSA: PSA levels should be undetectable following radical prostatectomy. This test is typically ordered at the 3 month followup visit. Rising PSA levels suggest biochemical disease recurrence. Continue case

Question #14: Incorrect Answer C. Chest X-ray: Unnecessary due to the low likelihood of bone metastasis. Return to Question #14
Question #14: Incorrect Answer D. Physical exam: Should be performed, but will only identify gross disease, which is highly unlikely in this patient. Return to Question #14
Case Continued Mr. State’s PSA is undetectable. He returns 9 months later (1 year post-operatively) to recheck his PSA, which is <0. 1. He has returned to full continence and is having satisfactory erections. He passes away 10 years later of unrelated cardiovascular disease. End case
Thank you. You have successfully completed this cancer survivorship case. Please provide feedback by completing an online Evaluation This case was developed by Steve Lerman, MD and Jonathan Bergman, MD, Department of Urology This module was designed by Tatum Langford Korin and Sarah Afrand, Instructional Design & Technology Unit To leave case hit ‘Esc’ (Escape) on your keyboard -found in the upper left corner Photo collection is courtesy of PEIR - University of Alabama at Birmingham Department of Pathology via the HEAL (Health Education Asset Library) database Cancer Survivorship Grant Project # © 2005, University of California Regents Start of case
Glossary Dodecad Biopsy: During prostate biopsy, 12 or more samples are taken to increase the likelihood of detecting cancer if it is present. Return to case
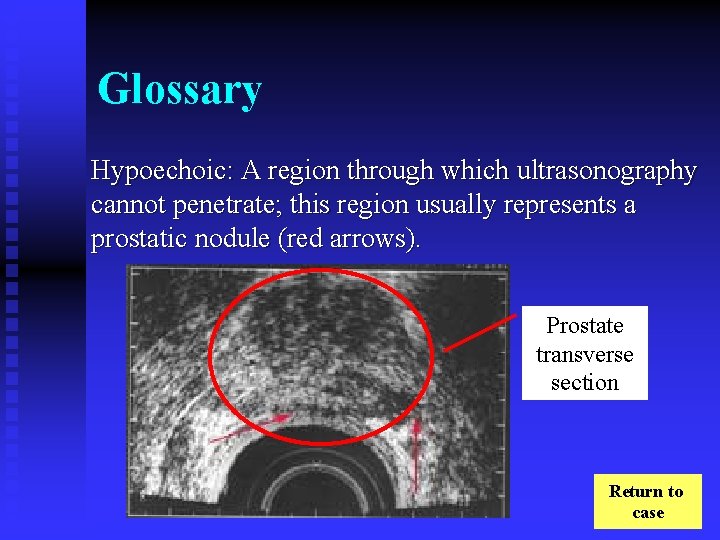
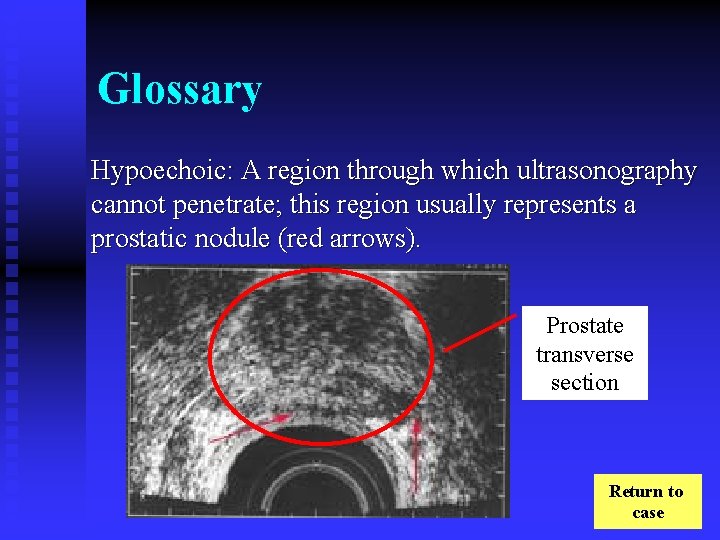
Glossary Hypoechoic: A region through which ultrasonography cannot penetrate; this region usually represents a prostatic nodule (red arrows). Prostate transverse section Return to case
Glossary Autologous: One’s own blood. By donating blood to themselves pre-operatively, patients can decrease the risk of transfusion reaction if they require an intraoperative or postoperative blood transfusion. Donation is done a few months prior to the procedure so the patient’s red blood cell count can re-stabilize. Return to case
Partin Tables 1) 2) 3) 4) Partin coefficient tables estimate prognosis by determining four probabilities: The probability that the patient has completely organ -confined disease The probability that the patient has “established capsular penetration” The probability that the patient has extension of his prostate cancer into his seminal vesicles The probability that the patient has prostate cancer which has spread into his lymph nodes Partin Table (word document) Return to case

Gleason Score The Gleason grading system is based on the glandular architecture of prostatic cells under low power. Grade 1 or 2 cells are closely packed, have little stroma, and are small and uniform. Grade 3 cells have variable-sized glands between normal stroma. Grade 4 cells have incomplete gland formation. Grade 5 cells have no gland formation or lumen appearance, or they may (rarely) be comedocarcinoma. The Gleason score is the sum of the most commonly found cell and the second most commonly found cell. The primary Gleason grade is more important than the second one, so Gleason 6 (4+2) is more poorly differentiated than Gleason 6 (3+3). Return to Case
Clinical versus Pathological Staging Clinical staging of prostate cancer involves estimation of disease extent based on physical examination, laboratory studies, and imaging studies. Pathological staging involves analysis of the removed specimen, as well. The pathologic stage of prostate cancer is as advanced as the clinical stage in 30% of cases, more advanced in 70% of cases, and rarely less advanced. Return to Case
Clinical versus Pathological Staging Clinical staging of prostate cancer involves estimation of disease extent based on physical examination, laboratory studies, and imaging studies. Pathological staging involves analysis of the removed specimen, as well. The pathologic stage of prostate cancer is as advanced as the clinical stage in 30% of cases, more advanced in 70% of cases, and rarely less advanced. Return to Question #7
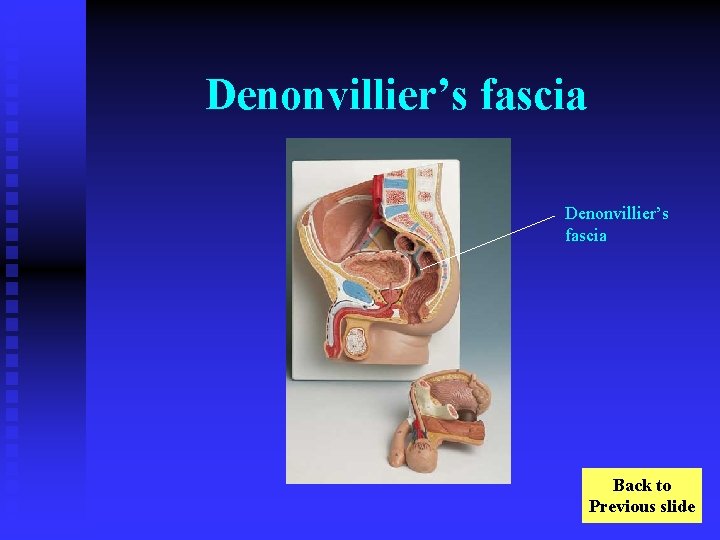
Denonvillier’s fascia Back to Previous slide
Disease-Free Survival Disease-free survival is the length of time a patient lives with no evidence of the disease in question. If a prostate cancer patient were alive 10 years after radical prostatectomy, but with a rising PSA, the patient would be categorized as a cancer survivor, but not a disease-free survivor. Return to Question #13
Obesity is currently defined by body mass index (BMI). A BMI of 25 -29 kg/m 2 is overweight, 30 -39 kg/m 2 is obese, and >40 kg/m 2 is morbidly obese. Return to Text
Disease-Free Survival Disease-free survival is the length of time a patient lives with no evidence of the disease in question. If a prostate cancer patient were alive 10 years after radical prostatectomy, but with a rising PSA, the patient would be categorized as a cancer survivor, but not a disease-free survivor. Return to Question #10
 Prostate cancer staging
Prostate cancer staging Mdv3100 prostate cancer
Mdv3100 prostate cancer Prostate cancer survival rates
Prostate cancer survival rates Laprp
Laprp Prostate cancer tnm classification
Prostate cancer tnm classification Hormonothérapie cancer prostate
Hormonothérapie cancer prostate Type 1 and 2 survivorship curve
Type 1 and 2 survivorship curve K selected species survivorship curve
K selected species survivorship curve K selected species survivorship curve
K selected species survivorship curve Type 1 survivorship examples
Type 1 survivorship examples Types of life table
Types of life table Bubble survivorship lab answer key
Bubble survivorship lab answer key Survivorship bubble lab
Survivorship bubble lab Lynx and hare relationship
Lynx and hare relationship Survivorship bias
Survivorship bias Survivorship vancouver
Survivorship vancouver Population growth curve
Population growth curve Dementia treatments and interventions near patterson
Dementia treatments and interventions near patterson Challenges and opportunities of media and information
Challenges and opportunities of media and information Function of the ductus deferens
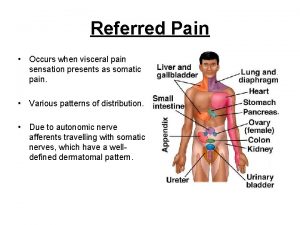
Function of the ductus deferens Prostate referred pain
Prostate referred pain Normal weight of prostate
Normal weight of prostate Prostate
Prostate Thyroid chapman point
Thyroid chapman point Prostatakreft symptomer
Prostatakreft symptomer Prostate adenocarcinoma perineural invasion
Prostate adenocarcinoma perineural invasion Anatomie zonale de mac neal
Anatomie zonale de mac neal Prostate pathology
Prostate pathology Prostate histology
Prostate histology Tuip prostate
Tuip prostate Base of prostate gland
Base of prostate gland Base of prostate gland
Base of prostate gland Prostate pathology
Prostate pathology Pirads radiopedia
Pirads radiopedia What does a prostate look like
What does a prostate look like Prostate
Prostate Male reproductive system
Male reproductive system Prostate anatomy
Prostate anatomy Adenocarcinome prostate
Adenocarcinome prostate Inguinocele
Inguinocele Protocole irm prostate
Protocole irm prostate Celine duperron
Celine duperron Treatments for acute renal failure
Treatments for acute renal failure Facial electrical treatments level 3
Facial electrical treatments level 3 Multi-element design
Multi-element design Hiv treatments
Hiv treatments Diabetes treatments
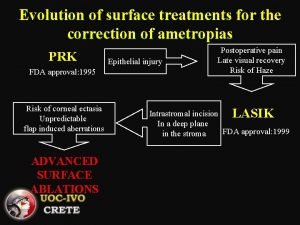
Diabetes treatments Advanced surface treatments
Advanced surface treatments Insomnia treatments
Insomnia treatments Actions to address risks and opportunities
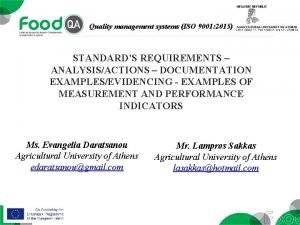
Actions to address risks and opportunities Costs and risks of database approach
Costs and risks of database approach Chapter 1 lesson 3 health risks and your behavior
Chapter 1 lesson 3 health risks and your behavior Cloud computing benefits and risks
Cloud computing benefits and risks Chapter 1 lesson 3 health risks and your behavior
Chapter 1 lesson 3 health risks and your behavior Chapter 1 lesson 3 health risks and your behavior
Chapter 1 lesson 3 health risks and your behavior Technology and operational risk
Technology and operational risk Physical hazards
Physical hazards Risks and mitigation slide
Risks and mitigation slide Understanding hazards and risks
Understanding hazards and risks Project finance risks and mitigants
Project finance risks and mitigants It infrastructure domains
It infrastructure domains What factors affect region/community location decisions?
What factors affect region/community location decisions? The biggest risk is not taking any risk
The biggest risk is not taking any risk Scr limited
Scr limited David chaffey
David chaffey Risks of e procurement
Risks of e procurement Instant messaging security risks
Instant messaging security risks Civil engineering insurance policies
Civil engineering insurance policies 21.hromosomas trisomijas risks
21.hromosomas trisomijas risks Enterprise risk management for credit unions
Enterprise risk management for credit unions Bulimia nervosa diagnostic criteria
Bulimia nervosa diagnostic criteria Sourcing process cips
Sourcing process cips Inherent risks examples
Inherent risks examples Chapter 22 lesson 1
Chapter 22 lesson 1 A thick, sticky, dark fluid produced when tobacco burns.
A thick, sticky, dark fluid produced when tobacco burns. Principles of credit risk management
Principles of credit risk management Ar = ir x cr x dr
Ar = ir x cr x dr Owasp top 10 privacy risks
Owasp top 10 privacy risks Cash management risks
Cash management risks Human resource risk examples
Human resource risk examples Balfour beatty 6 fatal risks
Balfour beatty 6 fatal risks Material selection risks
Material selection risks Managing risks in school curriculum activities
Managing risks in school curriculum activities Natural risks in business
Natural risks in business Data center consolidation strategy
Data center consolidation strategy What is the nature of risk
What is the nature of risk Institutional risks
Institutional risks Lullaby trust spot the risks
Lullaby trust spot the risks Risks digest
Risks digest Programmatic risk
Programmatic risk Risks of doing business in emerging markets
Risks of doing business in emerging markets Health risks
Health risks Market risk meaning
Market risk meaning Possible risks
Possible risks Digital transformation risks in banking
Digital transformation risks in banking Lifewave matrix 2
Lifewave matrix 2 Special contingency risks
Special contingency risks Managing risks in schools
Managing risks in schools Chapter 25 introduction to risk management
Chapter 25 introduction to risk management Chapter 20 lesson 2 choosing to live tobacco free
Chapter 20 lesson 2 choosing to live tobacco free Special contingency risks
Special contingency risks Chapter 24 the immune and lymphatic systems and cancer
Chapter 24 the immune and lymphatic systems and cancer The lymphatic capillaries are
The lymphatic capillaries are Socialization through the life course
Socialization through the life course Look at the film stills and discuss the questions
Look at the film stills and discuss the questions Look at the photos and answer the questions
Look at the photos and answer the questions In pairs look at the photo and answer the questions
In pairs look at the photo and answer the questions Photography comes from the greek words photo and graph
Photography comes from the greek words photo and graph In pairs look at the photos and answer the questions
In pairs look at the photos and answer the questions Where does the word photography come from
Where does the word photography come from National breast and cervical cancer early detection program
National breast and cervical cancer early detection program National breast and cervical cancer early detection program
National breast and cervical cancer early detection program Breast cancer anatomy and early warning signs
Breast cancer anatomy and early warning signs Risk factors of head and neck cancer
Risk factors of head and neck cancer Shaukat khanum memorial cancer hospital and research centre
Shaukat khanum memorial cancer hospital and research centre