Cancer Overdiagnosis A Clash of Science and Intuition

![NY Times June 8, 1924 “Dr. Bloodgood of Johns Hopkins declares elimination [of cancer] NY Times June 8, 1924 “Dr. Bloodgood of Johns Hopkins declares elimination [of cancer]](https://slidetodoc.com/presentation_image_h/86ae3ec4d19adc132333c216dc53595a/image-9.jpg)








- Slides: 33
Cancer Overdiagnosis: A Clash of Science and Intuition Barry Kramer, MD, MPH Director, NCI Division of Cancer Prevention
Disclosure Information • I have no financial relationships to disclose. • Opinions are mine, not official positions of the U. S. federal government or National Institutes of Health.
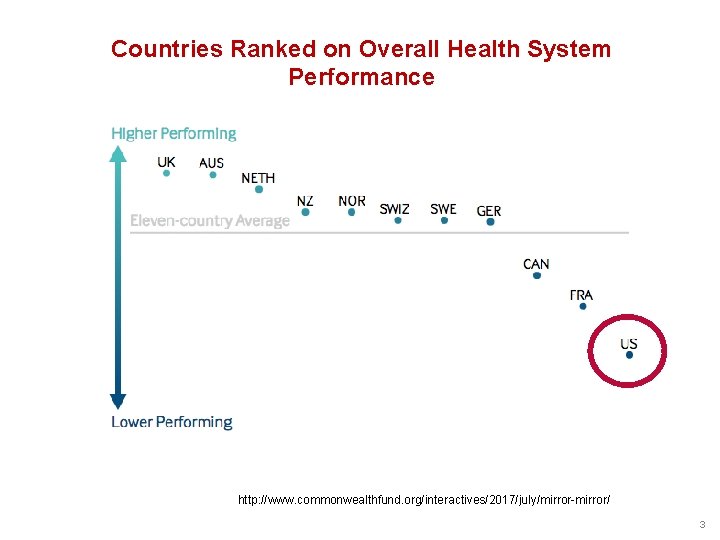
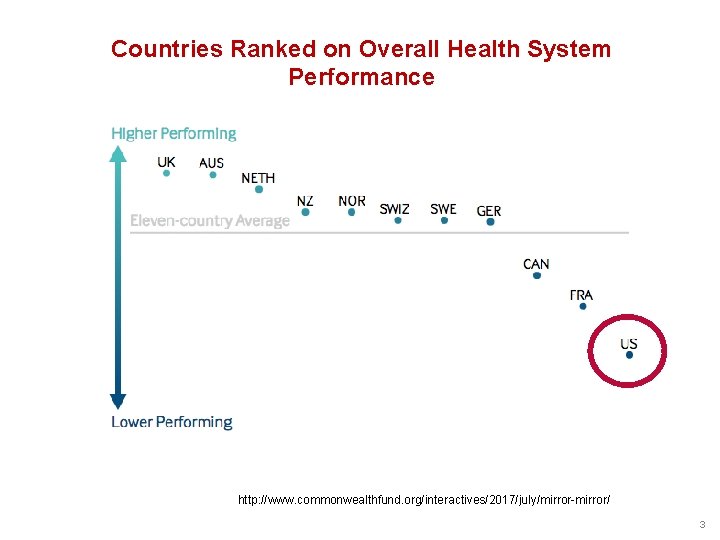
Countries Ranked on Overall Health System Performance http: //www. commonwealthfund. org/interactives/2017/july/mirror-mirror/ 3

Americans Spend More, Die Younger Organization for Economic Cooperation and Development (OECD) Countries Source: Laurie Meisler, Bloomberg. com https: //www. bloomberg. com/graphics/2017 -health-care-spending/
Requirements for Overdiagnosis • Existence of a silent disease reservoir • Activities leading to its detection (particularly screening) From G. Welch and W. Black, JNCI 2010 5
Iceberg: Symbol of Overdiagnosis 6
Core Issues in Screening § It is difficult to make healthy people better off than they already are. • It is sometimes easy to make healthy people worse off. § Strong evidence of benefit is important when putting large numbers of healthy people in harm’s way.
Ethics of Screening … there is an ethical difference between everyday medical practice and screening. If a patient asks a medical practitioner for help, the doctor does the best he can. He is not responsible for defects in medical knowledge. If, however, the practitioner initiates screening procedures he is in a very different situation. He should, in our view, have conclusive evidence that screening can alter the natural history of disease in a significant proportion of those screened. A. Cochrane and W. Holland, BMJ
![NY Times June 8 1924 Dr Bloodgood of Johns Hopkins declares elimination of cancer NY Times June 8, 1924 “Dr. Bloodgood of Johns Hopkins declares elimination [of cancer]](https://slidetodoc.com/presentation_image_h/86ae3ec4d19adc132333c216dc53595a/image-9.jpg)
NY Times June 8, 1924 “Dr. Bloodgood of Johns Hopkins declares elimination [of cancer] almost sure in early stage. ” “Deaths from cancer would be practically eliminated. . If persons afflicted sought medical aid immediately upon the discovery of a foreign growth in any part of the body. ”




Early Detection Articles Trend Toward Benefits Rather than Harms Hofmann and Skolbekken, The BMJ, May 2017 13

Trends in Publication on Early Detection by Specialty Hofmann and Skolbekken, The BMJ, May 2017 14
Consequences of Screening: The Good 1. Reduced risk of death from the target cancer (compared to no screening) • 2. Nearly always need a randomized controlled trial to determine this Reassurance (assuming healthy people need reassurance)
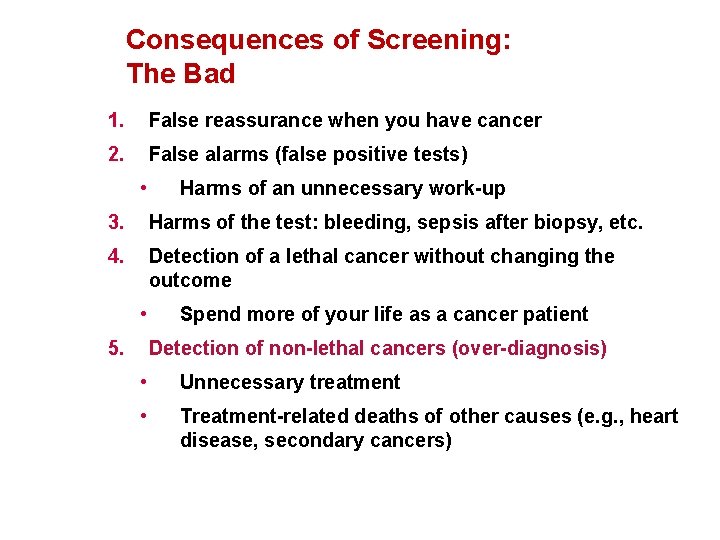
Consequences of Screening: The Bad 1. False reassurance when you have cancer 2. False alarms (false positive tests) • Harms of an unnecessary work-up 3. Harms of the test: bleeding, sepsis after biopsy, etc. 4. Detection of a lethal cancer without changing the outcome • 5. Spend more of your life as a cancer patient Detection of non-lethal cancers (over-diagnosis) • Unnecessary treatment • Treatment-related deaths of other causes (e. g. , heart disease, secondary cancers)
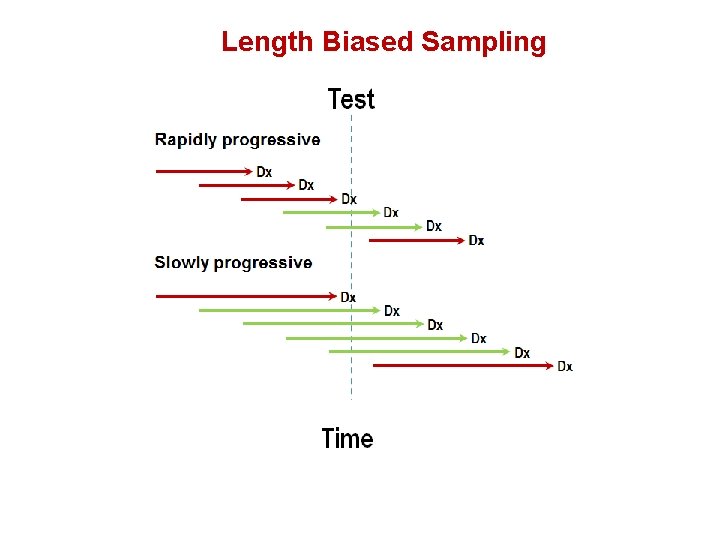
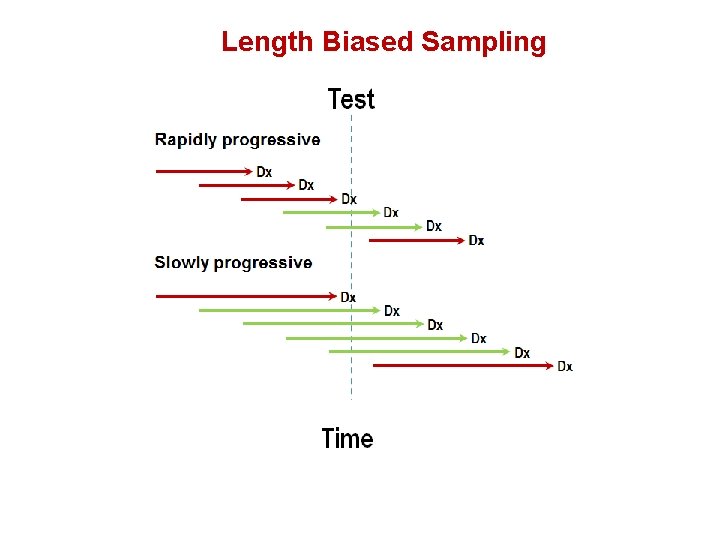
Length Biased Sampling

Overdiagnosis Screened and “cured” Death unrelated to cancer Cancer Never screened
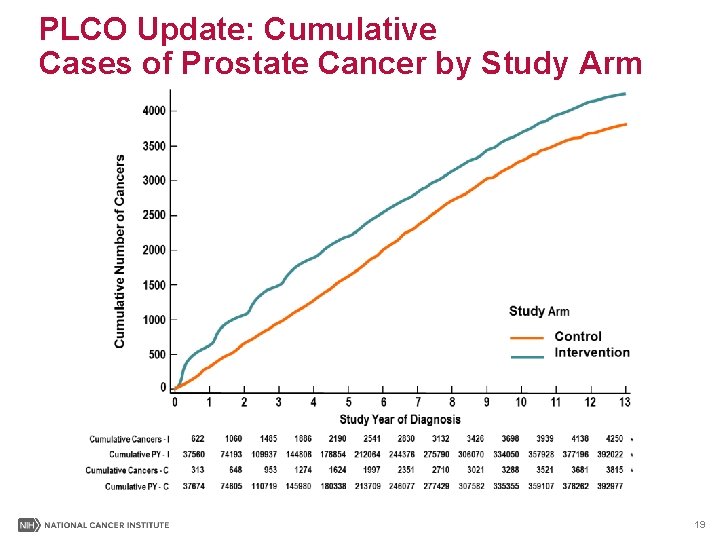
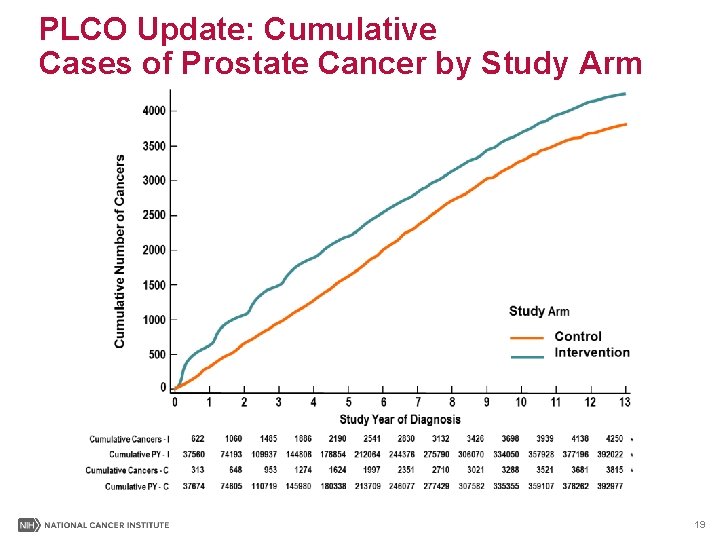
PLCO Update: Cumulative Cases of Prostate Cancer by Study Arm 19
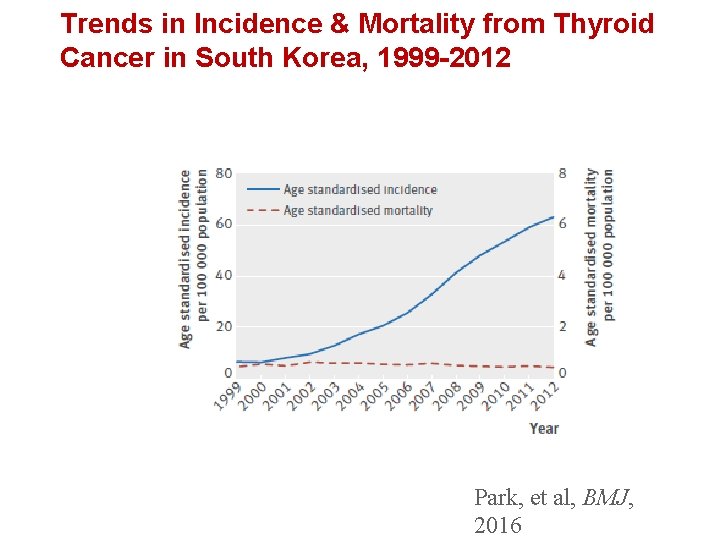
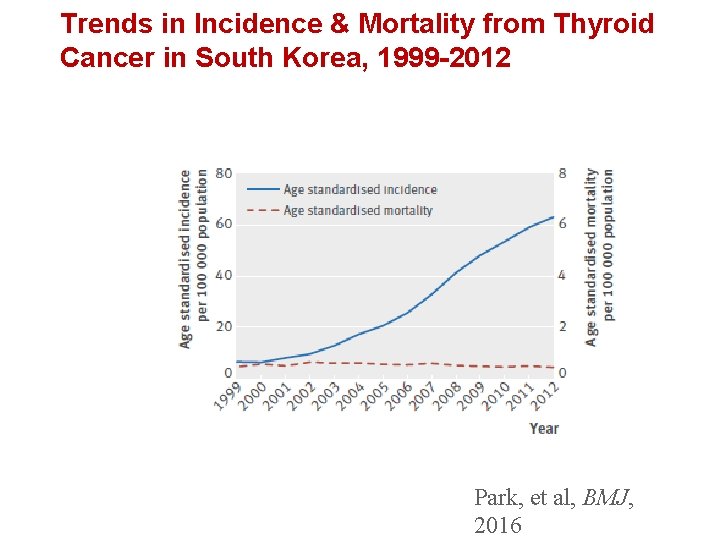
Trends in Incidence & Mortality from Thyroid Cancer in South Korea, 1999 -2012 Park, et al, BMJ, 2016
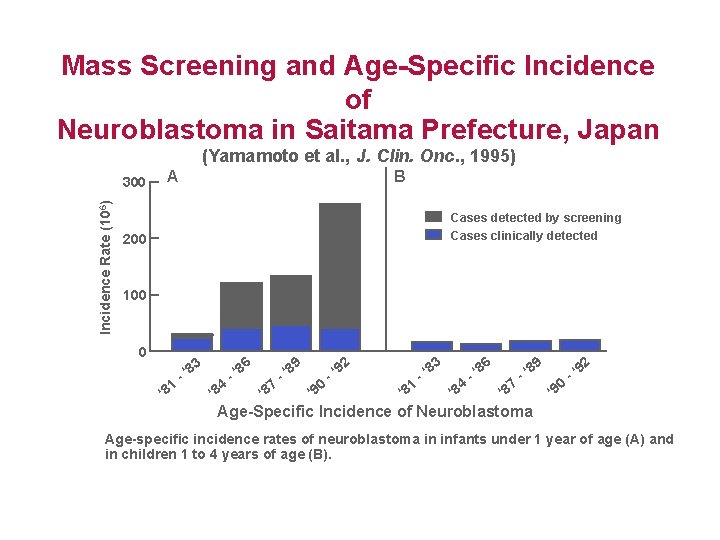
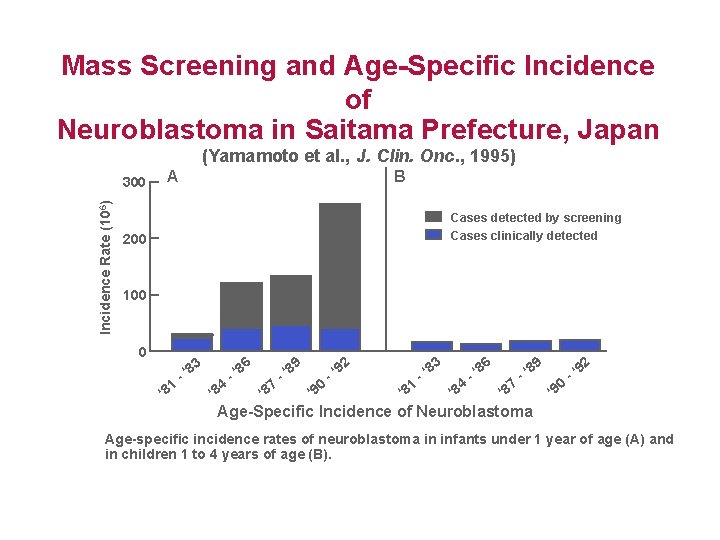
Mass Screening and Age-Specific Incidence of Neuroblastoma in Saitama Prefecture, Japan (Yamamoto et al. , J. Clin. Onc. , 1995) Incidence Rate (106) 300 A B Cases detected by screening Cases clinically detected 200 100 0 1 ‘ 8 4 ‘ 8 8 -‘ 7 ‘ 8 8 -‘ 0 ‘ 9 9 -‘ 1 ‘ 8 8 -‘ 4 ‘ 8 8 -‘ 2 9 6 3 8 -‘ 7 ‘ 8 8 -‘ 0 ‘ 9 9 -‘ Age-Specific Incidence of Neuroblastoma Age-specific incidence rates of neuroblastoma in infants under 1 year of age (A) and in children 1 to 4 years of age (B).
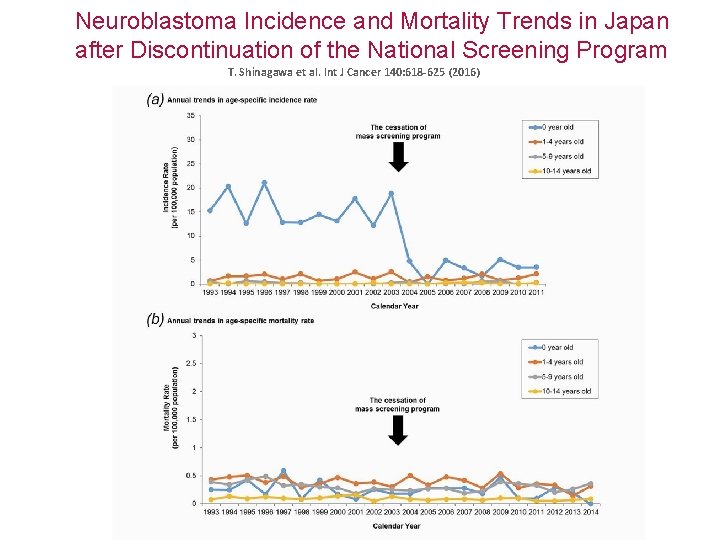
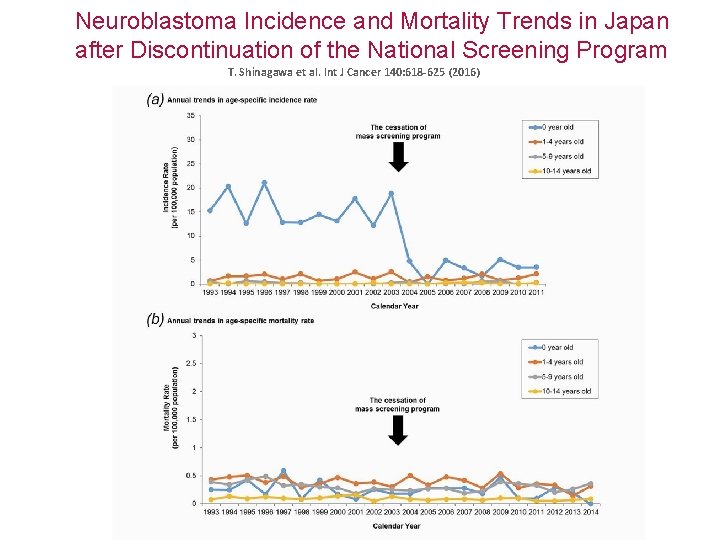
Neuroblastoma Incidence and Mortality Trends in Japan after Discontinuation of the National Screening Program T. Shinagawa et al. Int J Cancer 140: 618 -625 (2016)
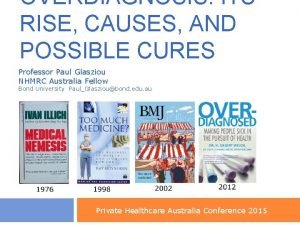
Risk Factors and the Transformation of Medicine “Ancient medical history”: diagnosis & management of established disease • Testicular cancer, lymphomas, childhood malignancies Screening for early, asymptomatic disease • Cervical cancer, colorectal cancer, lung cancer Screening for risk factors of disease • Family history, genetics, obesity Screening for risk factors (“disease risk predisposition”) • Genetic markers for nicotine addiction, obesity, microbiomics, diabetes… • Mammogram calcium to predict cardiac atherosclerosis

Transformation of Philosophy in the Era of “Omics” § The old days: “You are healthy until proven otherwise. ” § The modern era: “You are sick until proven otherwise. ” Adapted from E. Diamondis & M. Li, Clin Chem Lab Med 2016; 54(3): 389 -396
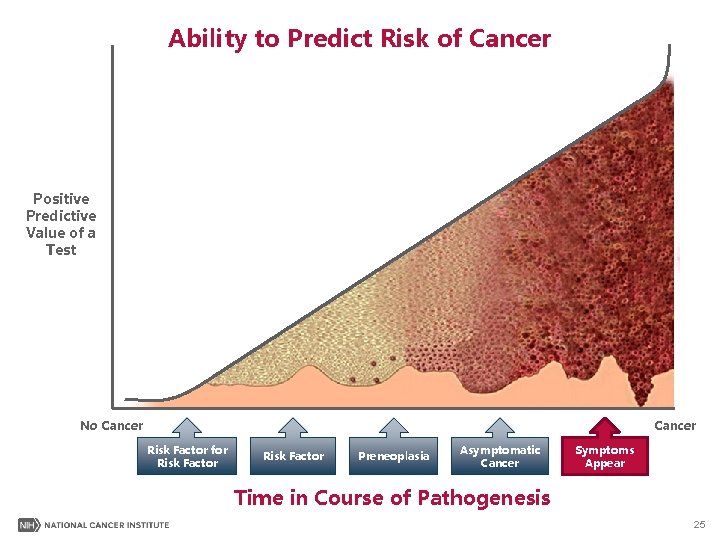
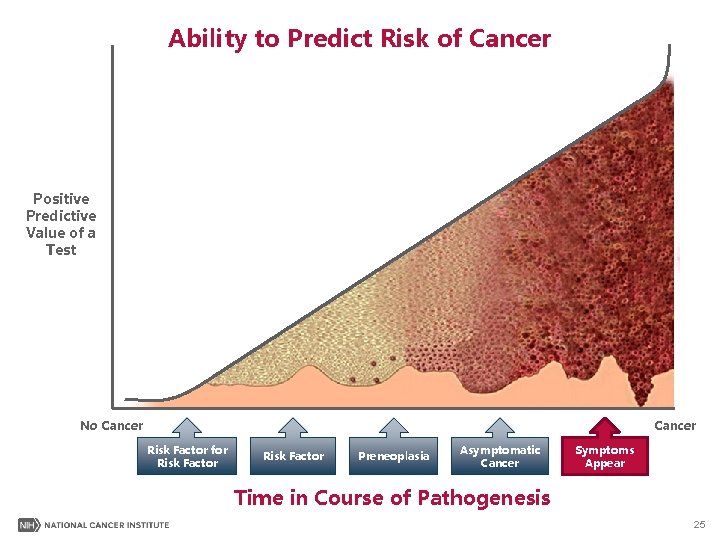
Ability to Predict Risk of Cancer Positive Predictive Value of a Test No Cancer Risk Factor for Risk Factor Preneoplasia Asymptomatic Cancer Symptoms Appear Time in Course of Pathogenesis 25
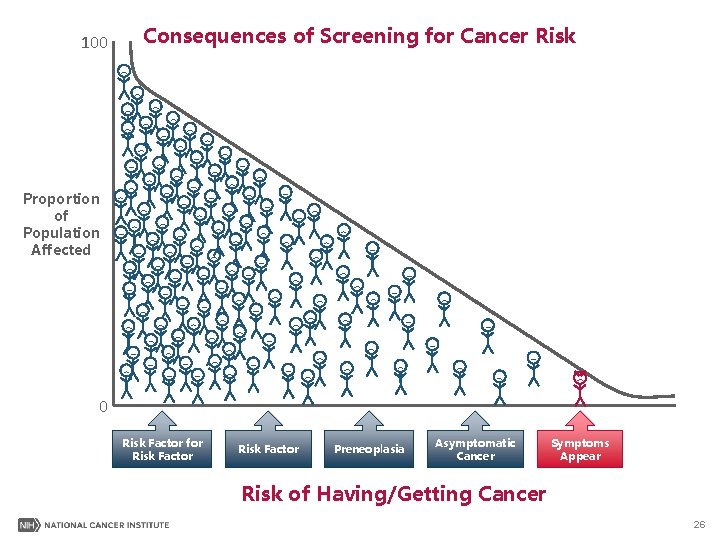
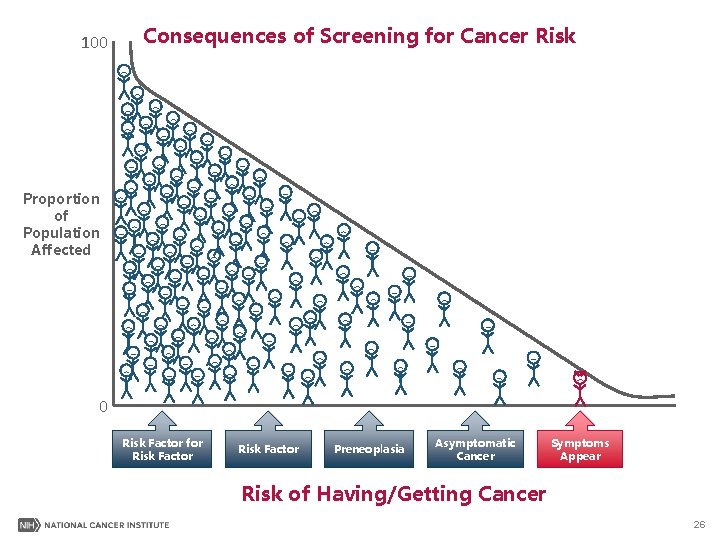
100 Consequences of Screening for Cancer Risk Proportion of Population Affected 0 Risk Factor for Risk Factor Preneoplasia Asymptomatic Cancer Symptoms Appear Risk of Having/Getting Cancer 26
“ The increased vigilance against pre-diseases might also change the way we perceive life itself, slowly transforming life into what can be characterized as pre-death. ” Bjorn Hofmann and John-Arne Skolbekken Surge in Publications on Early Detection, BMJ, 2017

What Can We Do about Cancer Overdiagnosis? 1. Education about its existence § Public and Media (the honest brokers of information) § Health professionals 2. Change the terminology § Language corrupts thought (and action) § “The slovenliness of our language makes it easier to have foolish thoughts. ” (George Orwell) 28
A Note of Caution Regarding Terminology “Words represent things, but the words are not the things. We know that, but we can forget. ” James Gleick, Time Travel, 2016
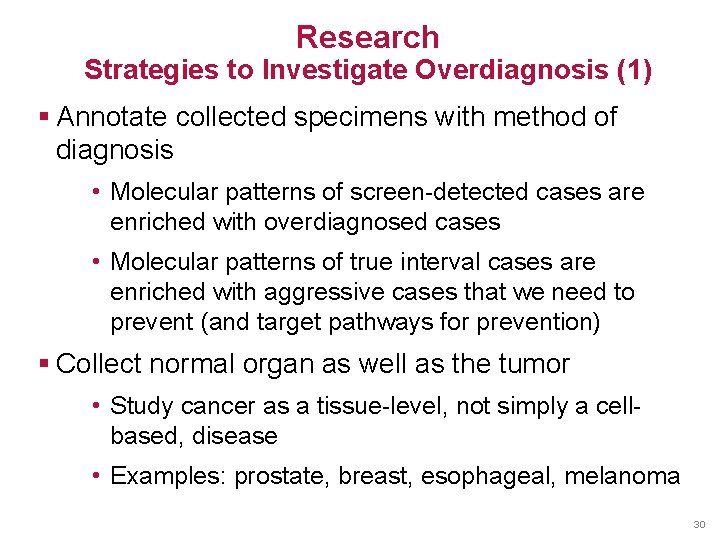
Research Strategies to Investigate Overdiagnosis (1) § Annotate collected specimens with method of diagnosis • Molecular patterns of screen-detected cases are enriched with overdiagnosed cases • Molecular patterns of true interval cases are enriched with aggressive cases that we need to prevent (and target pathways for prevention) § Collect normal organ as well as the tumor • Study cancer as a tissue-level, not simply a cellbased, disease • Examples: prostate, breast, esophageal, melanoma 30
Research Strategies to Investigate Overdiagnosis (2) § Use clinical opportunities to study natural history of indolent lesions • Prostate cancer: active surveillance • Barrett’s esophagus: serial endoscopy/biopsy § Better animal models of progression of very early lesions 31
www. cancer. gov/espanol
 Drip hiss the rain never stops
Drip hiss the rain never stops Chapter 29 the clash between traditionalism and modernism
Chapter 29 the clash between traditionalism and modernism Why did johnson and congress clash over reconstruction
Why did johnson and congress clash over reconstruction Conversation about favorite subject
Conversation about favorite subject Jung thinking feeling sensing intuiting
Jung thinking feeling sensing intuiting Rationalism vs romanticism
Rationalism vs romanticism American romanticism 1800 to 1860 worksheet answers
American romanticism 1800 to 1860 worksheet answers Romanticism qualities
Romanticism qualities Values feeling and intuition over reason
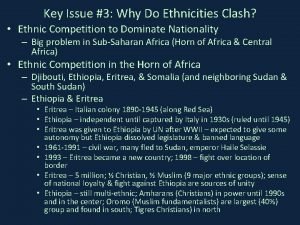
Values feeling and intuition over reason Why do ethnicities clash
Why do ethnicities clash A conflict is a struggle between two opposing forces
A conflict is a struggle between two opposing forces Clan manager
Clan manager Semantic clash
Semantic clash Central european monarchs clash
Central european monarchs clash Clash of lights 10
Clash of lights 10 Col to come together with great force to clash
Col to come together with great force to clash Lesson 3 a clash of values
Lesson 3 a clash of values Scopes trial political cartoon
Scopes trial political cartoon Chapter 21 section 3 central european monarchs clash
Chapter 21 section 3 central european monarchs clash X bogen clash of clans
X bogen clash of clans Chapter 5 a clash of cultures
Chapter 5 a clash of cultures Clash of civilizations huntington
Clash of civilizations huntington Clash of civilizations huntington
Clash of civilizations huntington Reconstruction lesson plans
Reconstruction lesson plans Lol 450 champions
Lol 450 champions Hku course disapprove
Hku course disapprove Chapter 13 section 1 cultures clash on the prairie
Chapter 13 section 1 cultures clash on the prairie Former allies clash
Former allies clash The struggle between two opposing forces
The struggle between two opposing forces Clash of armies
Clash of armies Central european monarchs clash
Central european monarchs clash Balanceamento clash
Balanceamento clash Gisle henden
Gisle henden J cole my intuitions
J cole my intuitions