Cancer colon 1 The peak incidence for colorectal

- Slides: 20
Cancer colon 1
• The peak incidence for colorectal carcinoma is between ages 60 and 79. Fewer than 20% of cases occur before age 50. • When colorectal carcinoma is found in a young person, pre-existing ulcerative colitis or one of the polyposis syndromes must be suspected. • Male-to-female ratio is 1. 2: 1. • Colorectal carcinoma has a worldwide distribution, with the highest death rates in the United States. 2
* Risk factors for cancer colon: 1. Genetic predisposition. 2. Dietary factors. 3. Precancerous lesions: – Colonic adenoma. – Hereditary familial polyposis coli. – Ulcerative colitis. 3
• The dietary factors receiving the most attention as predisposing to a higher incidence of cancer colon are: A diet with high calories and low fibers is risky…. • Mechanism: 1. Reduced fiber content leads to decreased stool bulk, increased fecal transit time in the bowel, and an altered bacterial flora of the intestine. Potentially toxic oxidative byproducts of carbohydrate degradation by bacteria are therefore present in higher concentrations in the stools and are held in contact with the colonic mucosa for longer periods of time. 4
2. High content of refined carbohydrates which contain less of vitamins A, C, and E, which act as oxygen-radical scavengers. 3. Excess intake of red meat: High cholesterol intake in red meat enhances the synthesis of bile acids by the liver, which in turn may be converted into potential carcinogens by intestinal bacteria. 5
* Morphology: - The distribution of the cancers in the colorectum is as follows: • Rectosigmoid colon 55%. • Cecum/ascending colon 22% • Transverse colon 11%. • Descending colon 6%. • Other sites 6%. 6
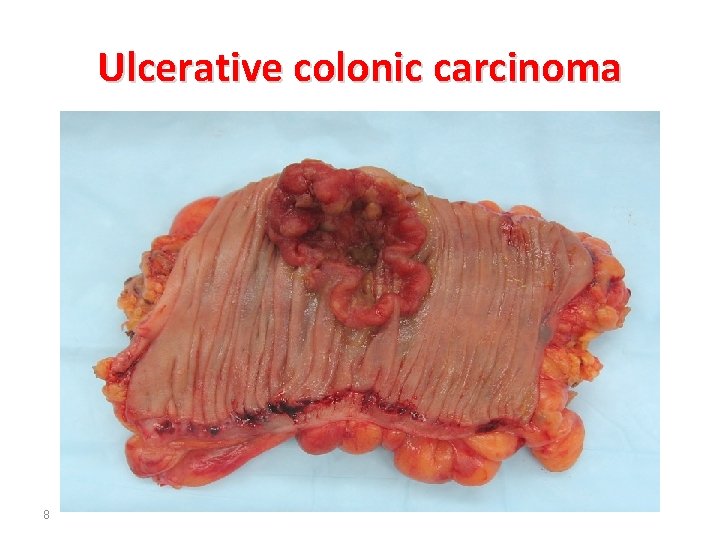
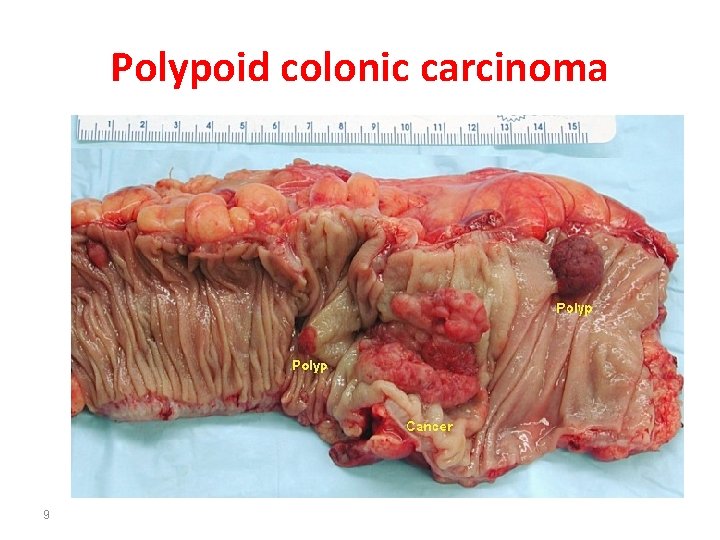
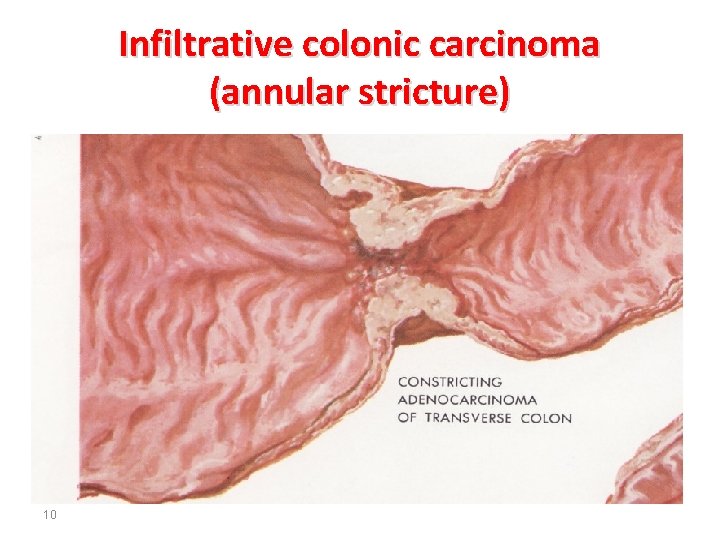
• Tumors in the proximal colon tend to grow as polypoid, exophytic masses. Obstruction is uncommon. • While carcinomas in the distal colon tend to be ulcerative forming malignant ulcer or tend to be infiltrative forming annular, encircling lesions that produce malignant constrictions of the bowel. 7
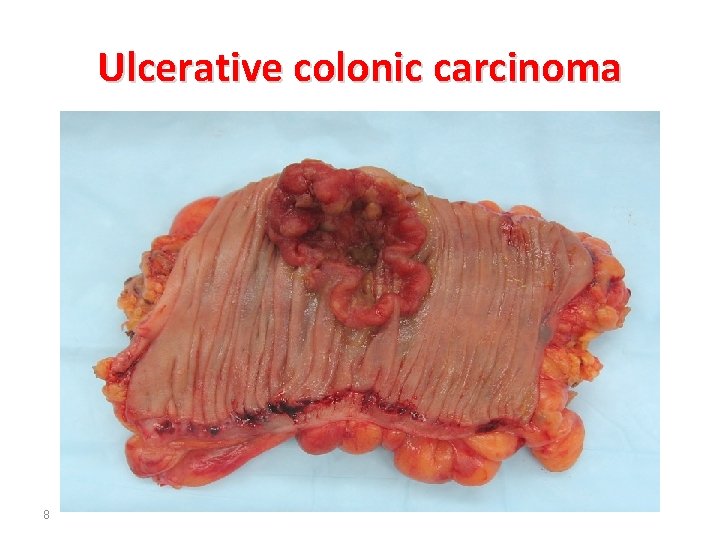
Ulcerative colonic carcinoma 8
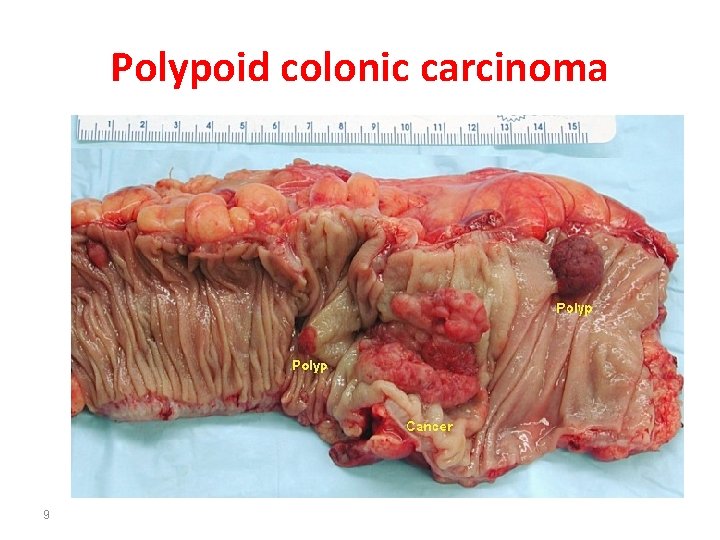
Polypoid colonic carcinoma 9
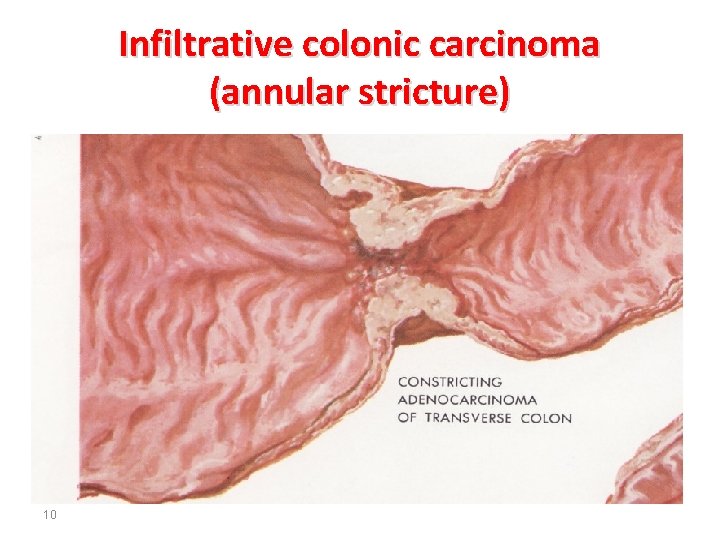
Infiltrative colonic carcinoma (annular stricture) 10
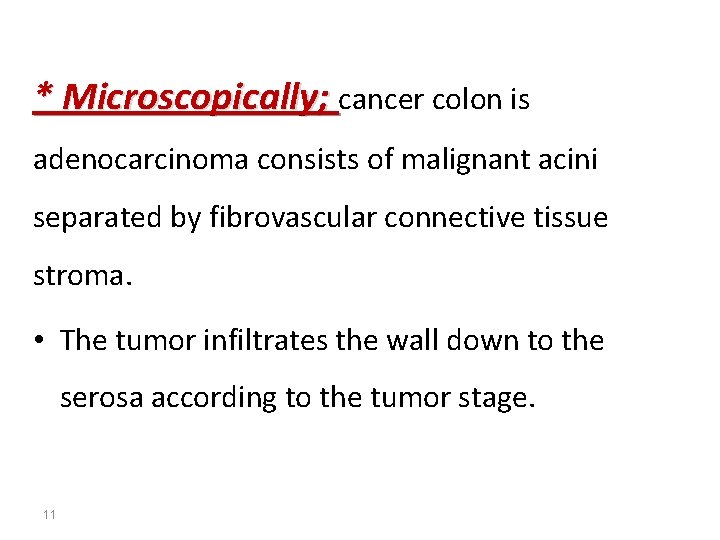
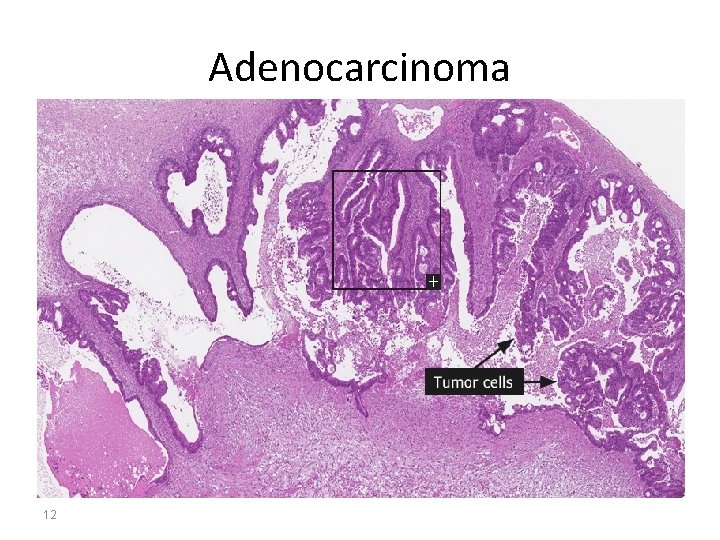
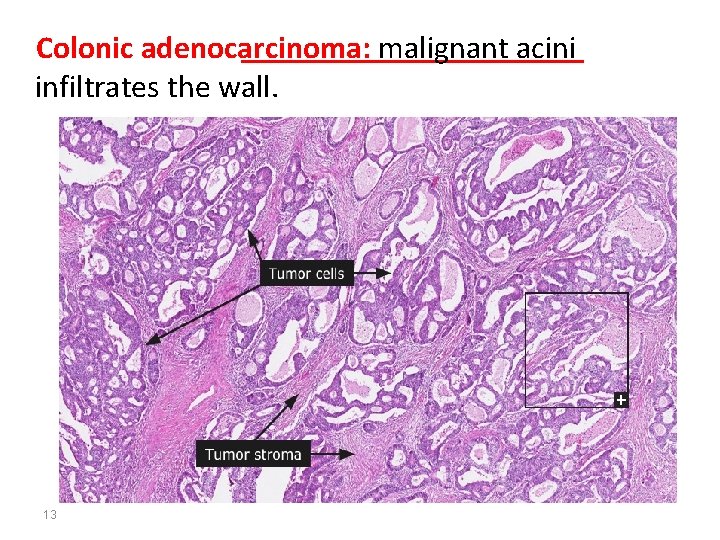
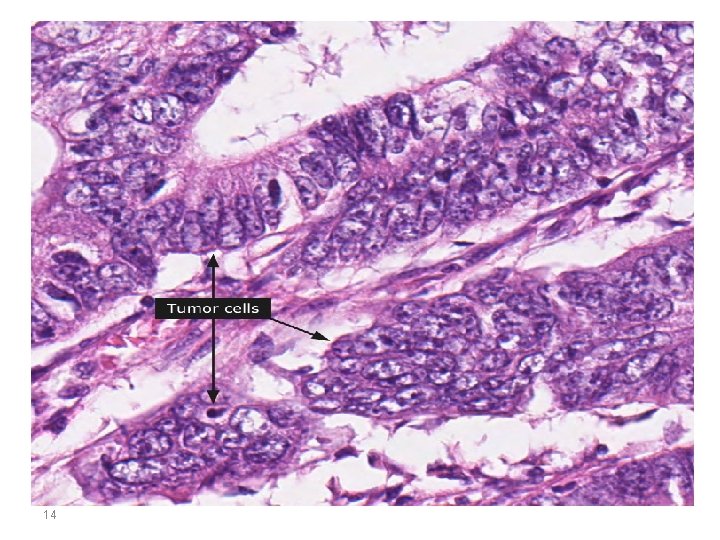
* Microscopically; cancer colon is adenocarcinoma consists of malignant acini separated by fibrovascular connective tissue stroma. • The tumor infiltrates the wall down to the serosa according to the tumor stage. 11
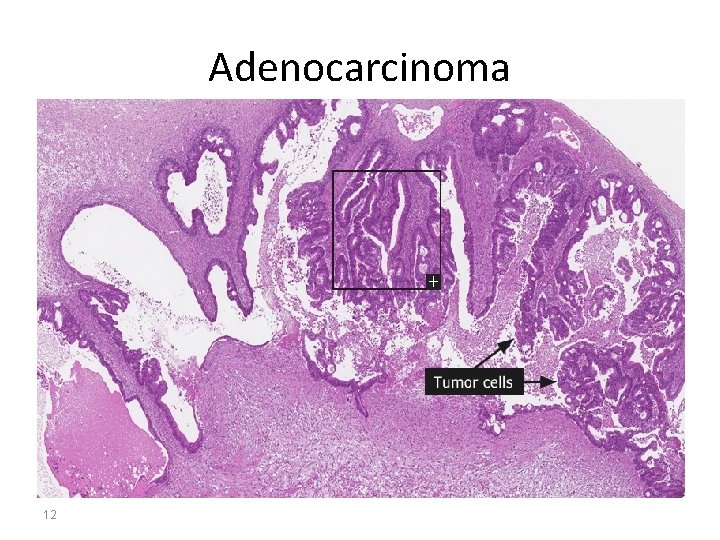
Adenocarcinoma 12
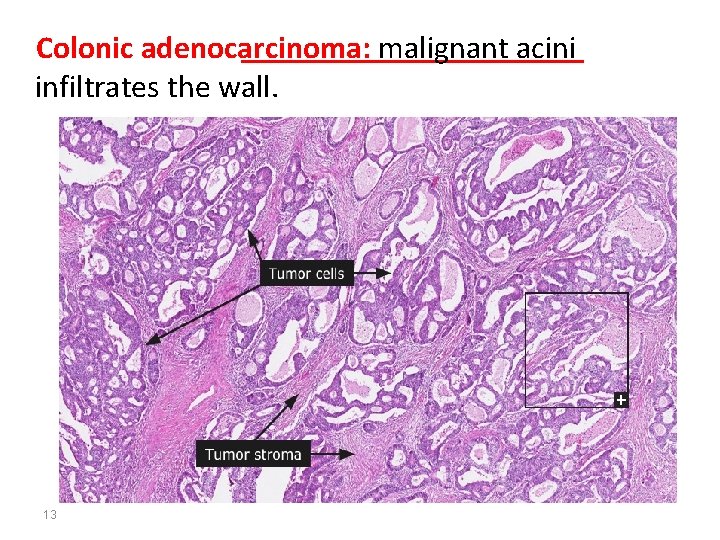
Colonic adenocarcinoma: malignant acini infiltrates the wall. 13
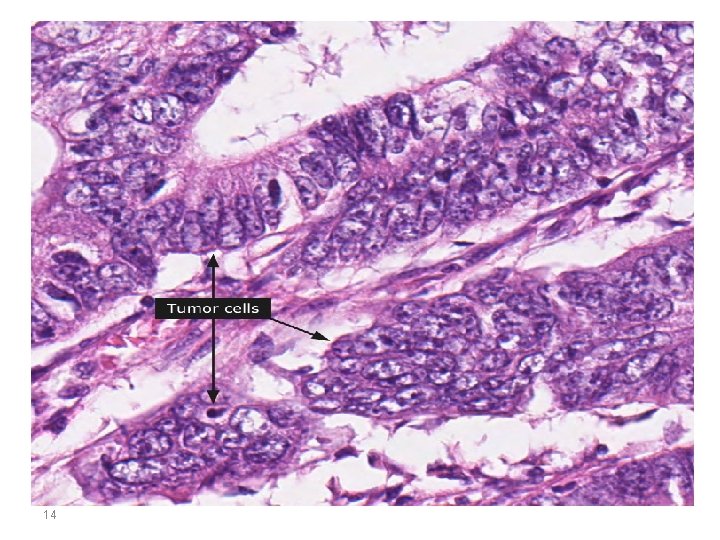
14
* Clinical Features: • Colorectal cancers remain asymptomatic for years. • Ceacal and right colonic cancers cause fatigue, weakness, and iron-deficiency anemia. These bulky lesions bleed readily and may be discovered at an early stage. • Left-sided cancers cause occult bleeding, changes in bowel habit, or crampy left lower quadrant discomfort. 15
• All colorectal tumors spread by direct extension into adjacent structures and by metastasis through the lymphatics and blood vessels. • In order of preference, the favored sites of metastatic spread are the regional lymph nodes, liver, lungs, and bones. 16
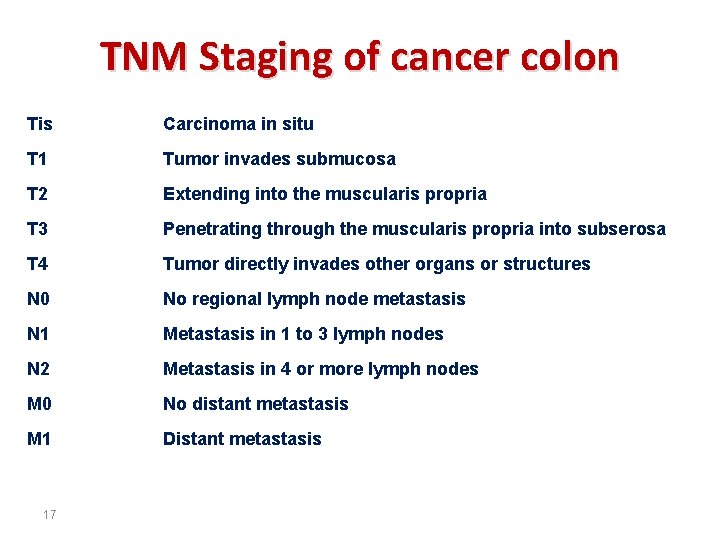
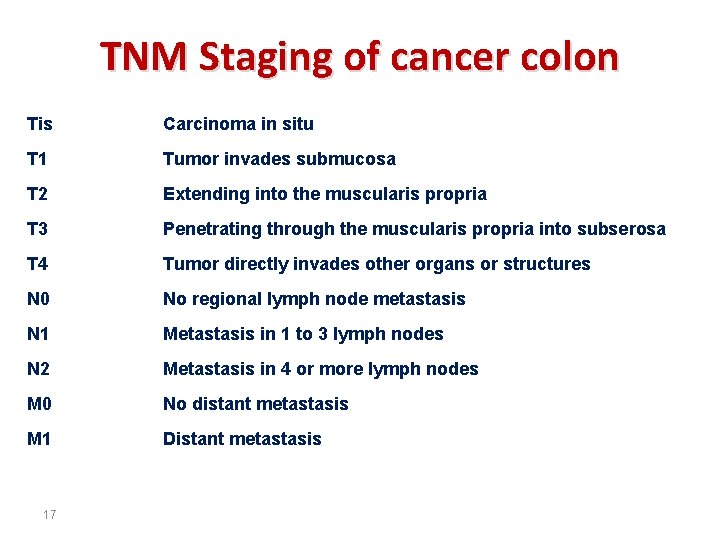
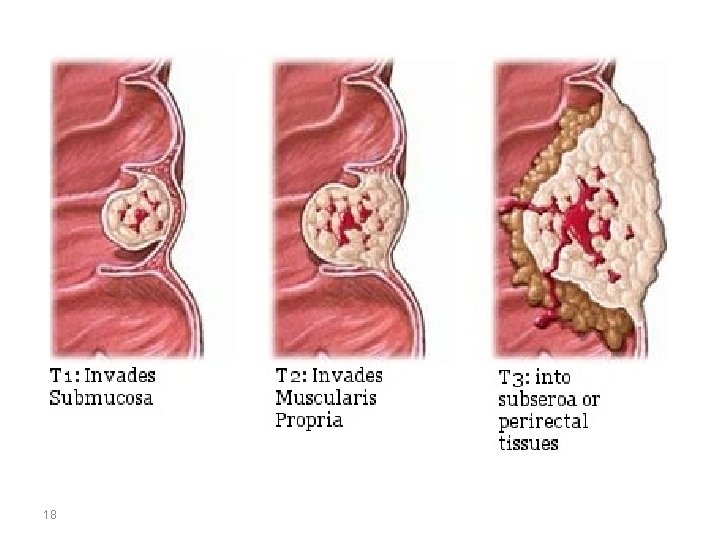
TNM Staging of cancer colon Tis Carcinoma in situ T 1 Tumor invades submucosa T 2 Extending into the muscularis propria T 3 Penetrating through the muscularis propria into subserosa T 4 Tumor directly invades other organs or structures N 0 No regional lymph node metastasis N 1 Metastasis in 1 to 3 lymph nodes N 2 Metastasis in 4 or more lymph nodes M 0 No distant metastasis M 1 Distant metastasis 17
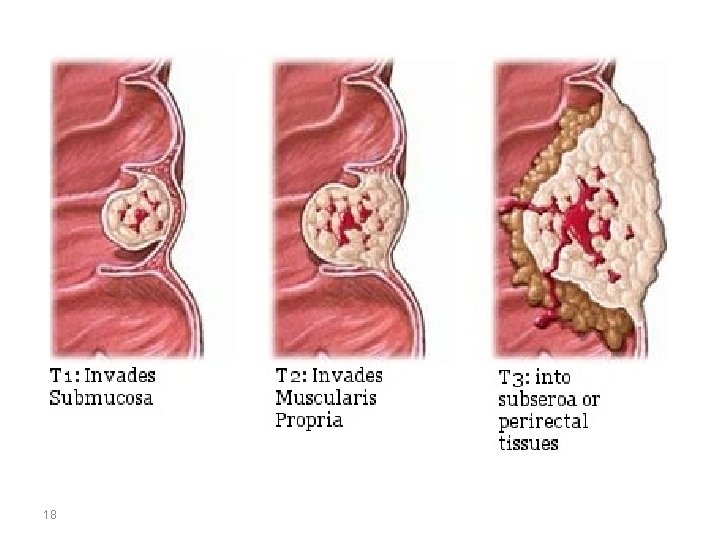
18
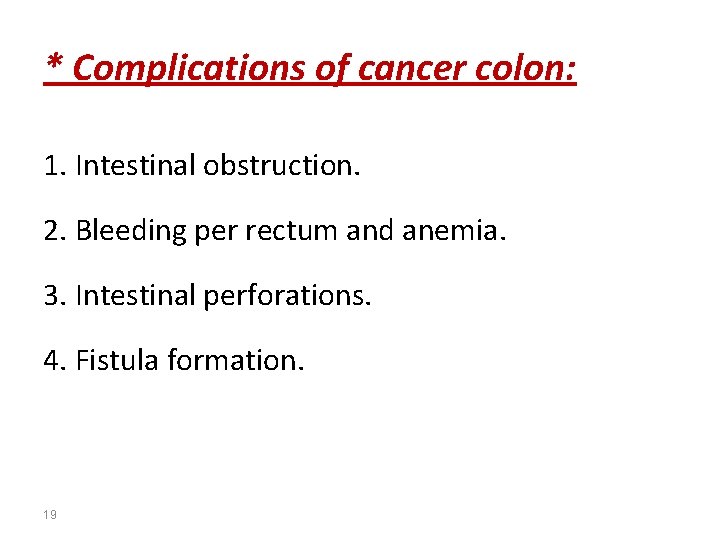
* Complications of cancer colon: 1. Intestinal obstruction. 2. Bleeding per rectum and anemia. 3. Intestinal perforations. 4. Fistula formation. 19

THANKS References: Robbins and Cotran’s: Pathologic Basis of Disease. Seventh edition. 20