Can we Talk A Personcentred Approach to Medication





















- Slides: 45

Can we Talk? A Person-centred Approach to Medication Management in an Acute Psychiatric Ward Project Team: Tom Andrews, Assistant Ward Manager; Deirdre Convery, Ward Sister and Pat Mullan, Staff Nurse Tobernaveen Centre, Holywell Hospital, Antrim Contact: tom. andrews@northerntrust. hscni. net November 2014 – June 2016 Report date: December 2016 Patients First Supporting nurse-led innovation in practice – A programme for clinically based nurse-led teams

Project Partners

Our Journey

Our Journey l l Twists and turns – not a straight line During the project, plans and timescales slipped, sometimes methods of adoption tried, then reviewed Motivation levels inevitably changed, up and down with time, pressure from both top and bottom Sometimes we had focus, then we had clarity, then sometimes it faded, then we refocused and eventually regained momentum

Tobernaveen Centre – December 2014 l l l Situated in Antrim, Northern Ireland under Northern Health and Social Care Trust 14 bedded acute inpatient unit for patients over 65 yrs of age with functional mental illness Input mainly from doctors, nurses, occupational therapists, physiotherapists, social work and advocacy
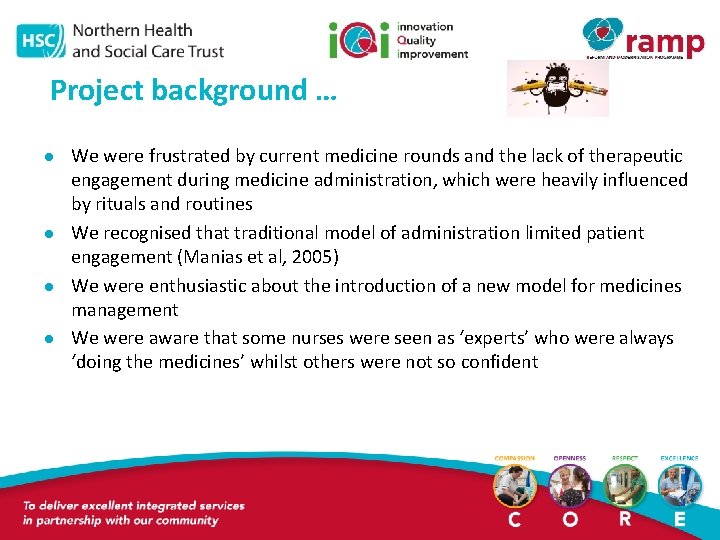
Project background … l l We were frustrated by current medicine rounds and the lack of therapeutic engagement during medicine administration, which were heavily influenced by rituals and routines We recognised that traditional model of administration limited patient engagement (Manias et al, 2005) We were enthusiastic about the introduction of a new model for medicines management We were aware that some nurses were seen as ‘experts’ who were always ‘doing the medicines’ whilst others were not so confident
l l l We agreed we needed to something to address this, but were not sure how During informal chats with nurses, the project team became aware that all felt they could do better Discussion developed on how to improve the current approach and how to be more person-centred There was also discussion about the importance of medicines management to a person’s recovery and to prevent relapse (Copeland, 2014), and a desire to reduce frequency of readmission for patients Could this time be better utilised as an opportunity for therapeutic engagement rather than a task? Also was there an opportunity to improve continuity of care?

We wanted to. . l l Enhance patient care Empower and encourage patients so that they felt they had more control over their own medicine management Use medicine management as a learning and recovery experience Create opportunities for person-centred interactions
We looked for guidance… l l Our ward sister had an informal chat about the change we would like to achieve with a local Practice Development Facilitator (PDF), who told us about the Patients First Programme We applied and were successful It was decided that Tom and the PDF would attend the workshops in London to represent the ward We thought… happy days… but then …
l l Just the week before our journey to London for the first workshop – the PDF was redeployed Staff were told to continue with the project Tom attended the first workshop alone with very little idea of what to do But returned and fed back to staff team what he had learnt

Take home learning from the first workshops … l l l The first two workshops facilitated by Fo. NS helped us to further develop the project We realised the importance of values and beliefs clarification in developing a common vision for our project We were now equipped with tools and techniques to explore values and beliefs and other exercises
l l l The discussion and interaction with other teams from across the UK was helpful The development of an action plan to achieve activities by the next workshop day helped focus team The support from Jo Odell (Practice Development Facilitator from Fo. NS) and the practice development work book supplied by Fo. NS enabled us to do these exercises effectively

Values and beliefs l l We carried out a values and beliefs clarification exercise with staff /team members (mainly nurses) to explore our values about the care we provide in relation to medication administration We endeavoured to gain insight into our patients’ perspectives and explored what patients really wanted to achieve in our unit during their stay and within their recovery

The values that came out of the exercises were: l We wish to have a caring, compassionate environment with openness and transparency, respecting patients’ wishes l We aspire to be an area of excellence for both staff and patients l Patients should be at the centre of all decision making
Patients’ perspectives l l l At the start we undertook an information gathering session and asked patients about their experiences This was gathered using informal chat and staff patient meetings This is what they said: § Patients wanted to know who is looking after them as early as possible (named nurse)
§ § Patients had preferences regarding what they were taking medicines with (with meals, glass of water etc. ) and they wanted to take medicines when they wanted to rather than when the nurse wanted to give them (choice and control) Patients didn’t like their names being called out in front of others Patients wanted to know more about their medicines Patients would like more privacy
Staff perspectives. . l We gathered staff perspectives during team meetings, daily briefings and through informal chats: § Staff would like to use medication administration time as a health promotion and recovery tool § Staff like the opportunity to discuss and asses a person’s mental state as soon as possible § Staff believe privacy and confidentiality should be upheld during medication administration § Staff feel their own morale would be lifted by doing the above, as well as having a sense of achievement

Models used. . 1. Kurt Lewin’s Change Model (1947) 2. Mc. Cormack and Mc. Cance’s Person Centred Framework (2016)
1. Lewin’s model of change l Unfreeze - Can be identified as the plan to implement change, discovering the motivation to change: – The unfreeze stage was straightforward to instigate as there was an awareness that current management of medications could be improved and we wanted to change current model § This was discussed by staff during our informal chats, briefings and staff meetings. Most of the staff were very open to change at this stage

l Change - This is the process of effective communication to bring about the desired change and to empower people: – The process of change started once we clarified values and beliefs, both ours and patients – We then developed a shared agenda to deliver patient centred processes for each patient. This helped us to engage authentically with patient needs in relation to medication management l Refreeze - This happens when the process is stabilised and embedded as best practice: – We then explored how to “refreeze” these values to ensure that we maintain our focus on person-centred goals
2. Mc. Cormack and Mc. Cance’s Personcentred Framework(2016) l This model has four components: ▪Skilled, competent, committed staff with clear values and beliefs of who they are and what they want to achieve ▪An effective environment with good staff relationships, organisational structures that are supportive and potential for innovation and positive risk taking ▪Person-centred processes, which focus on delivering care through a range of activities that can be negotiated keeping in mind of each person’s uniqueness and values. Excellent communication skills and therapeutic rapport are vital ▪Expected outcomes including satisfaction of care, involvement in care, feeling of wellbeing and creating a therapeutic environment
Component 1: Developing prerequisites l We initially focused on the pre-requisites of the framework by clarifying our values and beliefs and exploring the motivation of the team to have full commitment with the process of change. The values clarification exercises aided this process
Component 2: Ensuring care environment l l Gaining confidence from stakeholders through meeting them individually. We also ensured ongoing discussion by speaking with staff about the proposed change during regular meetings and staff briefings, ensuring a caring environment Discussions with patients in the process helped in developing shared decision making systems in an environment which encourages power sharing and engagement
Component 3: Patient centred processes l l We then combined patients’ beliefs and values with our values so that we could work with patients in a more harmonious environment and engage more authentically with patients This all helped staff in working toward the provision of holistic care using shared decision making
Component 4: Person-centred outcomes l l The whole process came into realisation as the patient centred moments became opportunities to engage authentically As a result of the whole process there has been a changing culture. Staff are moving from doing things as rituals or routines to opportunities for therapeutic engagement Patients reported that they now felt empowered and informed about the management of their own medications Some reported that they were able to identify trigger factors in relation to relapse of their illness and therefore could seek help from professionals at an earlier stage

Stake holders. . l l l The next step in our journey was to identify essential stake holders We identified them as the medical team, nursing team, advocacy service and senior management team We tried to arrange meetings with all of them together on several occasions but realised it’s not as easy as we thought We spoke to each one of the disciplines separately and all were happy to support our project Discussions about the project and our journey became an integral part of staff supervision and appraisals

Patient engagement l l Patient engagement was an integral part of this project We used these opportunities to promote health and wellbeing and to educate patients about the importance of medication adherence in preventing relapse

l We used verbal feedback from staff patient meetings, health promotion meetings with patients and informal chats, and feedback through questionnaires to evaluate the effectiveness of our approach:
Steps forward/steps back l l l Staff who had rarely undertaken medication administration began to build their confidence Incidents happened in the ward which knocked their confidence Facilitation and support from Fo. NS remained essential and helped us think forward There were significant challenges experienced during this project including sickness, maternity leave, resistance to change and day-to-day operational issues This resulted in our focus shifting away from the project at times during the 18 month period
Project meetings/workshops l l We attended five workshops in London, the last one in June 2016 was a celebration event. Each one helped us to regain focus Fo. NS supported and encouraged us when we got stuck - by visiting us, speaking to staff, using creative methods like Evoke cards, values clarification, claims, concerns and issues exercises etc. We used every opportunity offered to reflect on the progress of the project, this included informal talks, clinical supervision, staff meetings, appraisal meetings and daily briefings Those who were sceptical started to engage more with our new approach to medication management
Hindsight: 20/20 vision. . l l l We missed some opportunities to formally evaluate and measure the project outcomes The lack of a full written record throughout has ultimately proved challenging in terms of writing up this final report Contemporaneous notes would have helped complete the timeline more fully
Our Journey so far. . l l l Each nurse now administers the medication for their own patients Nurses use this time as an opportunity to interact therapeutically and asses the patient’s mental state Patients are able to interact with their named nurse many more times during the day We no longer have ‘medication nurses’ who do the medications all the time. Now each nurse administers medications to their own patients approximately 4 -5 times per day This has resulted in an increase in confidence and skills in the safe administration of medication
One of our colleagues wrote. . ‘‘Since the project commenced, my confidence has been enhanced and a true sense of achievement felt when involved in the administration of medications to my group of patients, making me feel valued as a primary nurse’’

What our patients say. . l l Some patients report that they can now recognise triggers that would be indicative of a deterioration in their mental health and are able to report these to their named nurse sooner thus preventing relapse of their illness Patients report that they are more confident with their medication regime as they feel more empowered by their named nurse and they feel they have more choice
Other good news. . l l The Regulation and Quality Improvement Authority(RQIA) highlighted that our project was in line with good practice The ward has developed a pamphlet for patients which includes a rationale for the importance of responsible ownership of medications during their leave period and upon discharge from the ward The use of on demand/emergency ‘PRN’ benzodiazepines decreased as patients had more opportunities to avail themselves of therapeutic input with their named nurse Our senior management team have recognised our achievement and agreed to provide funding for one member of staff to do a post-graduate course in practice development

We developed a poster about the project and presented this at the celebration event at the King’s Fund in London in June 2016
Challenges and opportunities ahead. . l l l Since October 2015, the Tobernaveen Centre has become a 20 bedded unit (increased from 14) 10 beds for over 65 yrs and 10 beds for under 65 yrs patients We now have 2 consultants and their teams – thus increasing the size of the multi-disciplinary team We now have access to a psychologist one day per week We plan to use this time to develop staff knowledge, understanding and skills in ‘talking therapies’ Our intention is to then deliver low intensity therapies such as mindfulness in a more structured way
l We are in the process of recruiting support workers who are patients to help us with the recovery and wellbeing of patients
What we learned as a team. . l l l Recording outcomes as the project progressed is essential to aid drafting of a final report Identifying values, beliefs and goals helped to maintain a focus and achieve the project’s aims Fo. NS’ support for the project was very important The involvement of a local facilitator may have been helpful in identifying milestones/deadlines etc. We heard about the PD forum within the trust, but were not confident or bold enough to be part of it at that time - we could have used it for support
l l l We could have been more creative and bolder in our use of resources, for example using Evoke cards more often, using Survey Monkey to collect data, contacting our governance department to gather data etc. Service improvement/practice development opportunities are brilliant. It works!!. This is not someone's idea, it’s ours! This journey has shown us numerous methods to capture data something we will keep in mind for our future person-centred projects

Acknowledgements. . l l l We thank the Foundation of Nursing Studies and Burdett Trust for Nursing for all the support and guidance given during our project We would also like thank Jo Odell and her team for facilitating workshops and visiting us at our work base to support us on several occasions The bursary was our lifeline for travel and other expenses

l l Other project teams from different parts of the United Kingdom were very supportive and informative throughout the 18 month period. We really enjoyed their company Our senior management team were very supportive, releasing staff and giving us protected time to undertake activities in relation to this project We would not have been able to achieve anything without the efforts and commitment of our multidisciplinary team at the Tobernaveen Centre Our patients were the core in this project. So many of them supported it and benefited greatly during their journey with us in Tobernaveen Centre

Wee final thought. . l We look forward to embracing further person-centred innovations to improve quality and care for patients and staff

A few photos from a patient engagement session

References l l l Copeland, M. E. (2014) WRAP for Life. Peach Press: Dummerston, Vermont. Heyes, S. (2005) Art of Recovery: A Pocket Guide to Recovery from Mental Distress. Mind: South Somerset. Lewin, K. (1947) The Kurt Lewin Change Model. Retrieved from: http: //www. change-management-coach. com/kurt_lewin. html Manias, E. , Aitken, R. and Dunning, T. (2005) How graduate nurses use protocols to manage patients’ medications. Journal of Clinical Nursing. 14 (8) pp 935 -944. Mc. Cormack, B. and Mc. Cance, T. (2016) Person-Centred Practice in Nursing and Health Care: Theory and Practice. Wiley Blackwell, Oxford.
 Talk read talk write template
Talk read talk write template Amateurs talk strategy professionals talk logistics
Amateurs talk strategy professionals talk logistics The words use are not
The words use are not Nurullah alınak
Nurullah alınak We can talk mental health training
We can talk mental health training We use can to talk about
We use can to talk about Nunca patino ni monto en bicicleta
Nunca patino ni monto en bicicleta Datagram network and virtual circuit network
Datagram network and virtual circuit network Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Waterfall strategy marketing
Waterfall strategy marketing Multiple conflict
Multiple conflict Bandura's reciprocal determinism
Bandura's reciprocal determinism Process of research definition
Process of research definition Traditional approach vs object oriented approach
Traditional approach vs object oriented approach Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Cpt code for medication management
Cpt code for medication management 10 rights of medication
10 rights of medication Lot number on medication
Lot number on medication Thrombolytic drugs mechanism of action
Thrombolytic drugs mechanism of action Ivpb medication
Ivpb medication Rca and capa of medication error
Rca and capa of medication error Difference between prescription and medication order
Difference between prescription and medication order Preanesthetic medication
Preanesthetic medication Defaulter vaccination schedule
Defaulter vaccination schedule Preanesthetic medication
Preanesthetic medication Im injection sites and volumes pediatrics
Im injection sites and volumes pediatrics Preanesthetic medication
Preanesthetic medication Fluid balance chart nsw health pdf
Fluid balance chart nsw health pdf Uhc medication prior authorization form
Uhc medication prior authorization form National standard medication chart
National standard medication chart Bactrim pediatric dosing
Bactrim pediatric dosing Iv medication formula
Iv medication formula Intravenous medication administration pretest
Intravenous medication administration pretest Concepts of medication administration pretest
Concepts of medication administration pretest 5 rights of medication
5 rights of medication Ati oral and topical medication administration posttest
Ati oral and topical medication administration posttest Medication reconciliation معني
Medication reconciliation معني Gtt/min formula
Gtt/min formula Uses of diethyl ether
Uses of diethyl ether Faa caci asthma
Faa caci asthma Rdns medication authority
Rdns medication authority What is a prn medication
What is a prn medication Drug dose calculation formula for adults
Drug dose calculation formula for adults Dmdd medication
Dmdd medication Medication management plan
Medication management plan Parenteral medication examples
Parenteral medication examples