Campylobacter Morphology charecteristic features Small thin 0 2
Campylobacter
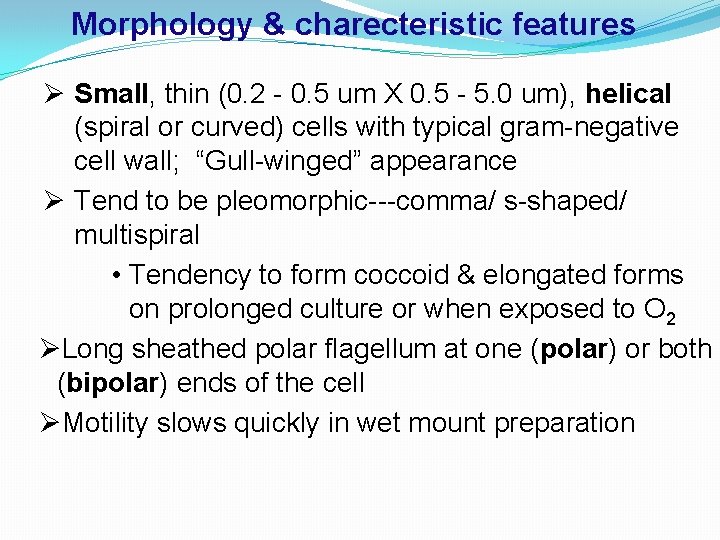
Morphology & charecteristic features Ø Small, thin (0. 2 - 0. 5 um X 0. 5 - 5. 0 um), helical (spiral or curved) cells with typical gram-negative cell wall; “Gull-winged” appearance Ø Tend to be pleomorphic---comma/ s-shaped/ multispiral • Tendency to form coccoid & elongated forms on prolonged culture or when exposed to O 2 ØLong sheathed polar flagellum at one (polar) or both (bipolar) ends of the cell ØMotility slows quickly in wet mount preparation
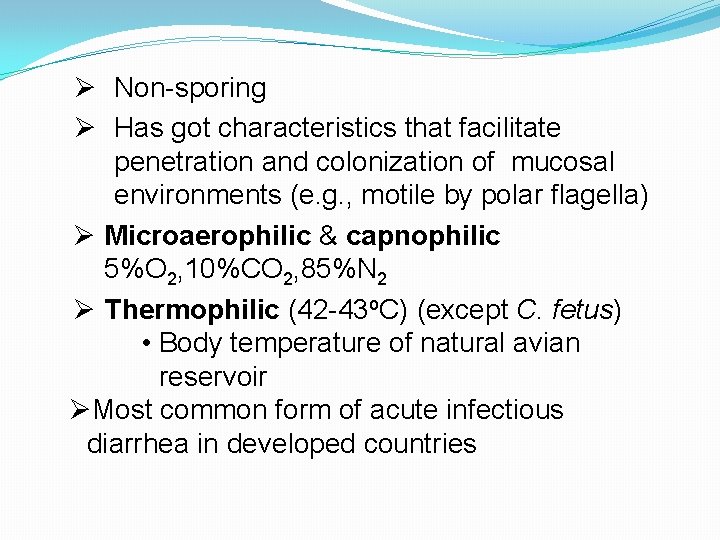
Ø Non-sporing Ø Has got characteristics that facilitate penetration and colonization of mucosal environments (e. g. , motile by polar flagella) Ø Microaerophilic & capnophilic 5%O 2, 10%CO 2, 85%N 2 Ø Thermophilic (42 -43 o. C) (except C. fetus) • Body temperature of natural avian reservoir ØMost common form of acute infectious diarrhea in developed countries
Campylobacter of medical importance: Causing diarrheal disease- C. jejani, C. coli, C. lari Causing extraintestinal infections- C. fetus Causing abcess- C. sputorum, C. conciscus
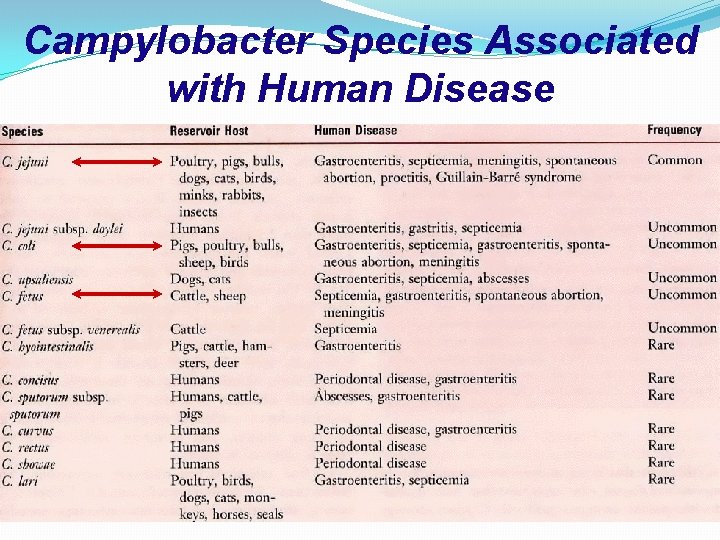
Campylobacter Species Associated with Human Disease
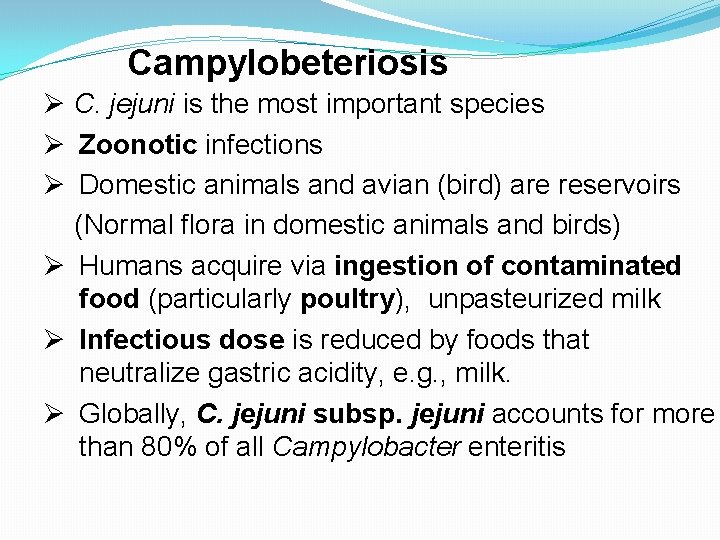
Campylobeteriosis Ø C. jejuni is the most important species Ø Zoonotic infections Ø Domestic animals and avian (bird) are reservoirs (Normal flora in domestic animals and birds) Ø Humans acquire via ingestion of contaminated food (particularly poultry), unpasteurized milk Ø Infectious dose is reduced by foods that neutralize gastric acidity, e. g. , milk. Ø Globally, C. jejuni subsp. jejuni accounts for more than 80% of all Campylobacter enteritis
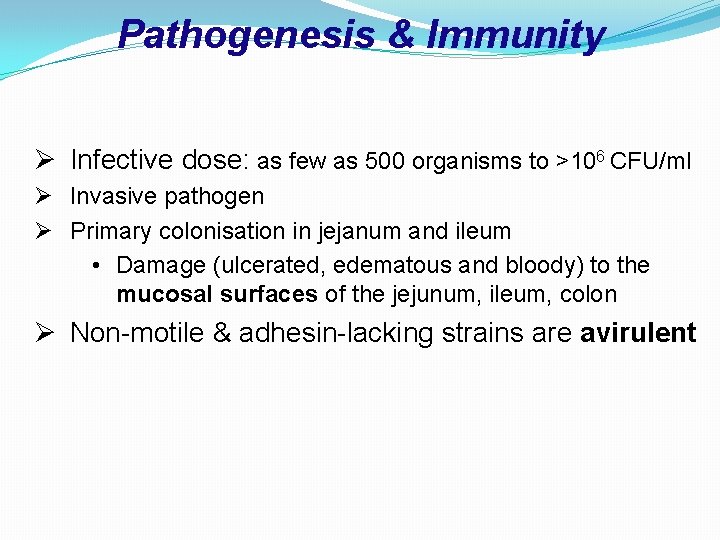
Pathogenesis & Immunity Ø Infective dose: as few as 500 organisms to >106 CFU/ml Ø Invasive pathogen Ø Primary colonisation in jejanum and ileum • Damage (ulcerated, edematous and bloody) to the mucosal surfaces of the jejunum, ileum, colon Ø Non-motile & adhesin-lacking strains are avirulent
Major virulence factors �Motility �Invasion �Enterotoxins
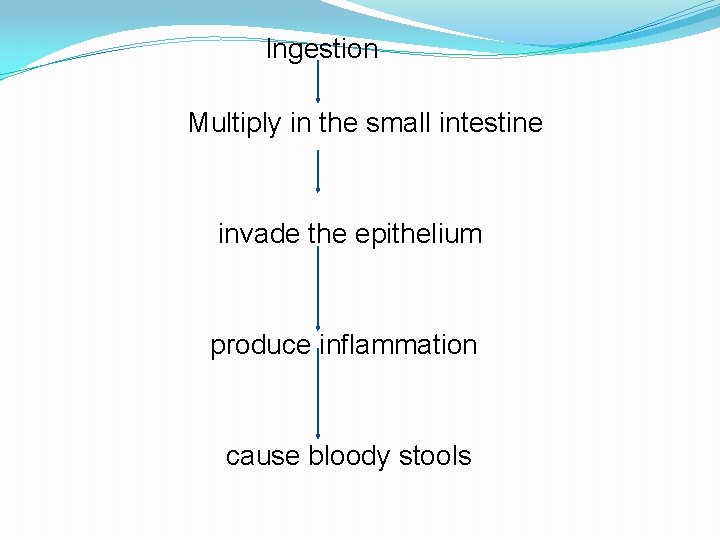
Ingestion Multiply in the small intestine invade the epithelium produce inflammation cause bloody stools
Clinical symptoms �Incubation period: 1 -7 days �Symptom start with fever, abdominal pain and watery diarrhea �Generally self limited
Other clinical conditions �Arthritis, Reiter’s Syndrome �Hemolytic Uremic Syndrome �Septicemia �Leading to infection of nearly any organ, including appendix, abdominal cavity, heart, nervous system, etc. �Guillain-Barre Syndrome (GBS) Ø Low incidence potential sequelae Ø Reactive, self-limited, autoimmune disease
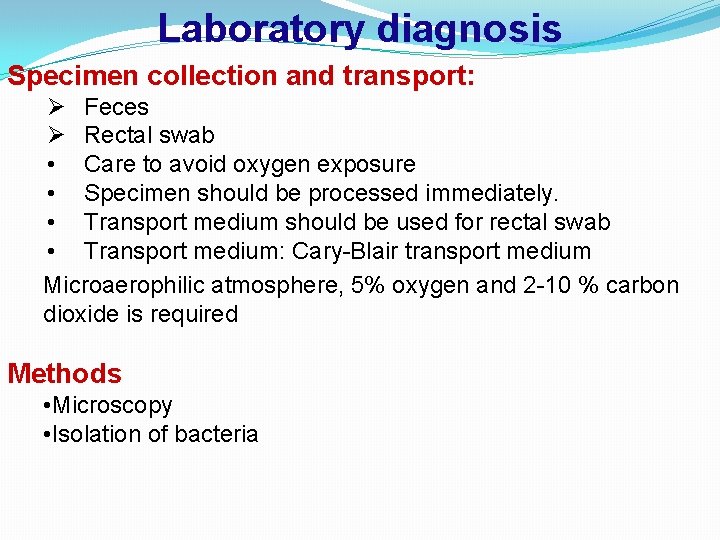
Laboratory diagnosis Specimen collection and transport: Ø Feces Ø Rectal swab • Care to avoid oxygen exposure • Specimen should be processed immediately. • Transport medium should be used for rectal swab • Transport medium: Cary-Blair transport medium Microaerophilic atmosphere, 5% oxygen and 2 -10 % carbon dioxide is required Methods • Microscopy • Isolation of bacteria
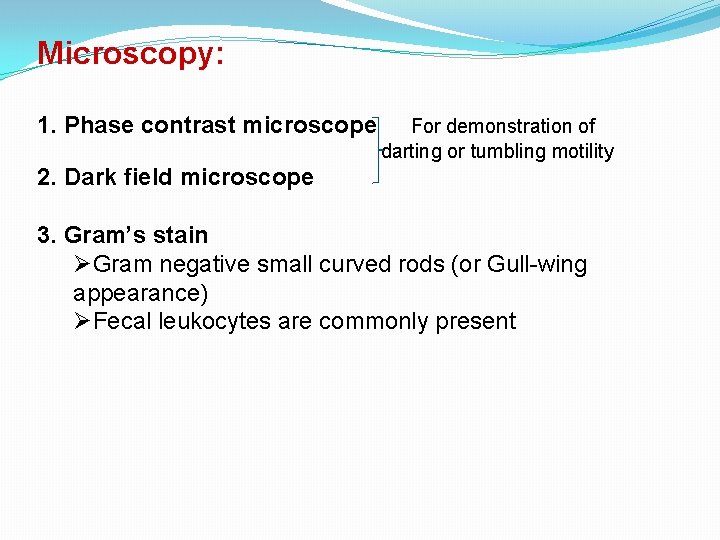
Microscopy: 1. Phase contrast microscope For demonstration of darting or tumbling motility 2. Dark field microscope 3. Gram’s stain ØGram negative small curved rods (or Gull-wing appearance) ØFecal leukocytes are commonly present
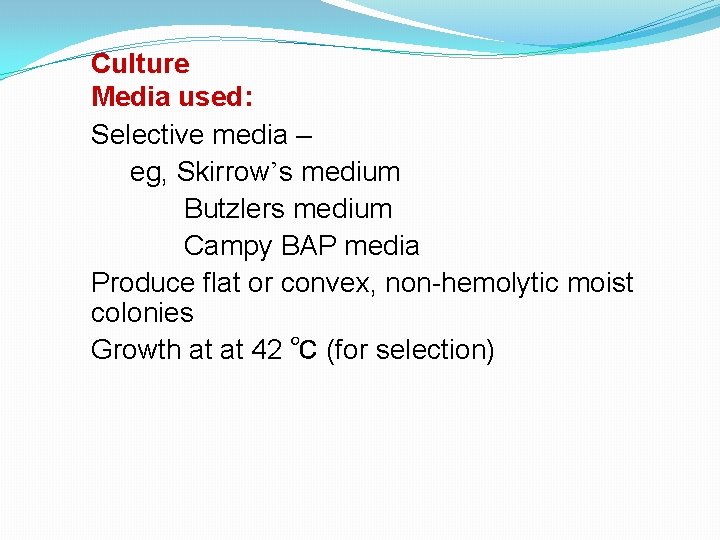
Culture Media used: Selective media – eg, Skirrow’s medium Butzlers medium Campy BAP media Produce flat or convex, non-hemolytic moist colonies Growth at at 42 ℃ (for selection)
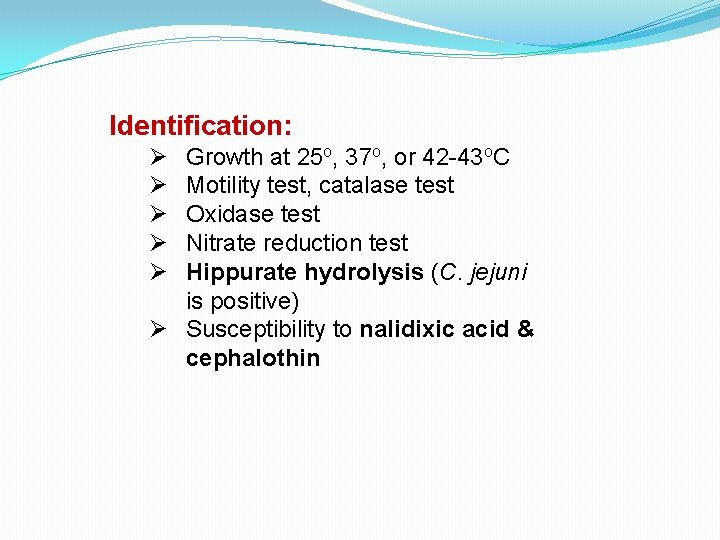
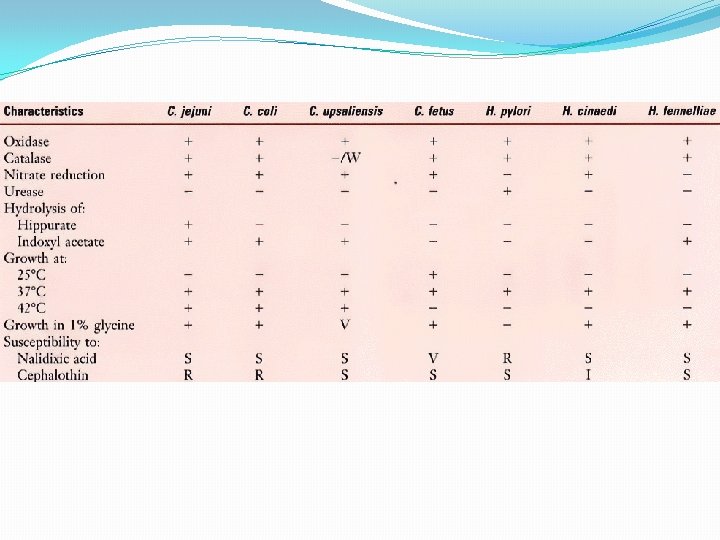
Identification: Ø Ø Ø Growth at 25 o, 37 o, or 42 -43 o. C Motility test, catalase test Oxidase test Nitrate reduction test Hippurate hydrolysis (C. jejuni is positive) Ø Susceptibility to nalidixic acid & cephalothin
Treatment, Prevention & Control Ø Gastroenteritis: • Self-limiting; Replace fluids and electrolytes • Antibiotic treatment can shorten the excretion period; Erythromycin is drug of choice for severe or complicated enteritis & bacteremia; • Fluroquinolones are highly active (e. g. , ciprofloxacin was becoming drug of choice) but fluoroquinolone resistance has developed
- Slides: 17