Camden Child and Adolescent Mental Health Service CAMHS

- Slides: 29
Camden Child and Adolescent Mental Health Service (CAMHS) 17 th December 2014 Dr Liz Searle Consultant Child and Adolescent Psychiatrist and Gill Markless Clinical Social Worker / Team Manager South Camden Community CAMHS Ampthill Square, 219 Eversholt Street, London NW 1 1 DR Tel: 0208 938 2700
What we will cover Structure of CAMHS in Camden Joint intake and referrals Our team and treatments offered CAMHS in primary care Key clinical scenarios: Depression Self-harm Any clinical scenarios you would like to discuss?
Camden CAMHS North Camden Community CAMHS – “Tier 2/3” South Camden Community CAMHS – “Tier 2/3” Under 5’s Service Brandon Centre Royal Free Hospital CAMHS (Eating Disorders, ADHD) MOSAIC CAMHS (Disability) Camden MALT (Child Protection and Looked After Children) EIS (1 st Onset Psychosis) IEYS (Children’s Centres) YOT (Offending) Special Schools and Pupil Referral Units Refugee Team (Tavi) Fostering and Adoption and Kinship Care Team (Tavi) Daytime duty cover at Tavistock Out of hours 24/7 on call psychiatry rota to A&E Access to inpatient Adolescent Units – Acute and Medium Stay
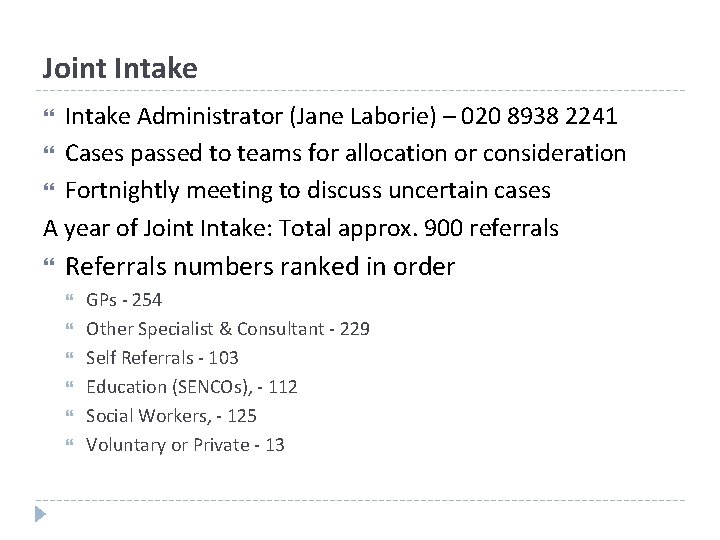
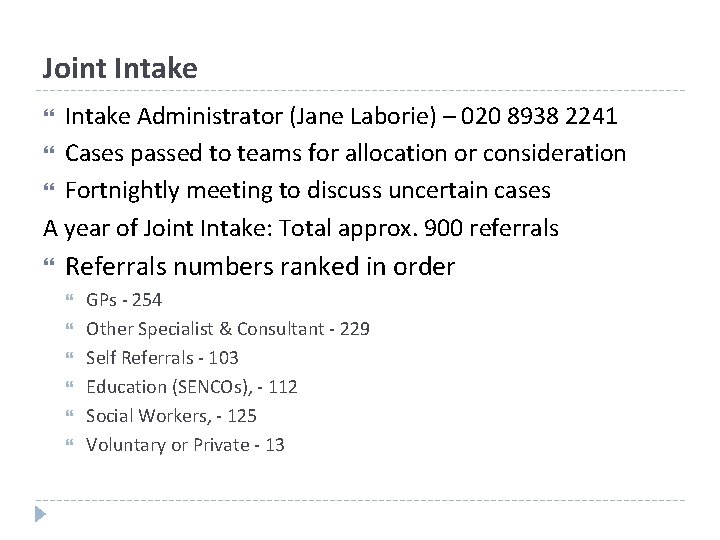
Joint Intake Administrator (Jane Laborie) – 020 8938 2241 Cases passed to teams for allocation or consideration Fortnightly meeting to discuss uncertain cases A year of Joint Intake: Total approx. 900 referrals Referrals numbers ranked in order GPs - 254 Other Specialist & Consultant - 229 Self Referrals - 103 Education (SENCOs), - 112 Social Workers, - 125 Voluntary or Private - 13
What happens Choice of initial appt offered to family within 11 weeks max. 75% discharged after less than 10 appts 20% 11 – 30 appts 5% more. Outreach for cases that need to be seen
The Multi Disciplinary Team Child and Adolescent Psychiatry Clinical / Educational Psychology Child and Adolescent Psychotherapy Family Therapy Community Mental Health Nursing Social Work Occupational Therapy
Interventions “Generic” Family Therapy (Systems) Individual Psychodynamic Psychotherapy CBT EMDR Parenting Groups Psychopharmacology
CAMHS in Primary Care CAMHS clinicians – Consultation Liaison Model: Training, Consultation, Joint Appointments, Direct work with less complex cases. Referral on of more complex cases. Pros and Cons of CAMHS in Primary Care: +ve: Easy Access See cases not otherwise seen Available resource for consultation -ve: Cases may not get to see MDT Lack of Space Too busy for consultation – you’re the experts
Depression in children & adolescents Important & underrecognised, treatable Prevalence of depression 6% in adolescents; 0. 5 -2% in pre-adolescents Girls>boys in adolescence Probably boys> preadolescence
Depression 2 Typical depressive symptoms eg. appetite, concentration, energy & motivation, anhedonia. . . Can present atypically in C&A eg. disturbed/increased sleep & appetite, irritability, school refusal, self-harm, somatic symptoms (headaches, stomach aches)
Depression – Treatment NICE guideline: Psychological treatment 1 st-line for mild-moderate Anti-depressant treatment should be started by ‘specialist’ Good research evidence for SSRIs and CBT eg. TADS study Combination most effective Fluoxetine 1 st choice in under-18 s Risk of increased suicidal ideation Start low & monitor closely for suicidality Continue for 6/12 -1 year after improvement
Self-Harm What is it? Includes: Cutting eg. cuts to arms, legs, abdomen Self-poisoning – ‘overdose’ Can include taking excessive amounts of drugs or alcohol Burning Pulling hair, picking skin Self-strangulation, hanging, suffocation Other harmful behaviours………. . Non-accidental – Terms: ‘Deliberate self-harm’ (DSH); ‘parasuicide’; ‘attempted suicide’ ‘Non-accidental self-injury’/’Non-suicidal self-injury’ now preferred by some authors
Who? • • • Many episodes never come to professional attention (only 12% do) Relatively uncommon in childhood Peak in adolescence 7 -14% of adolescents will self harm at some time Under 12, commoner in boys Girls > boys in adolescence 5: 1
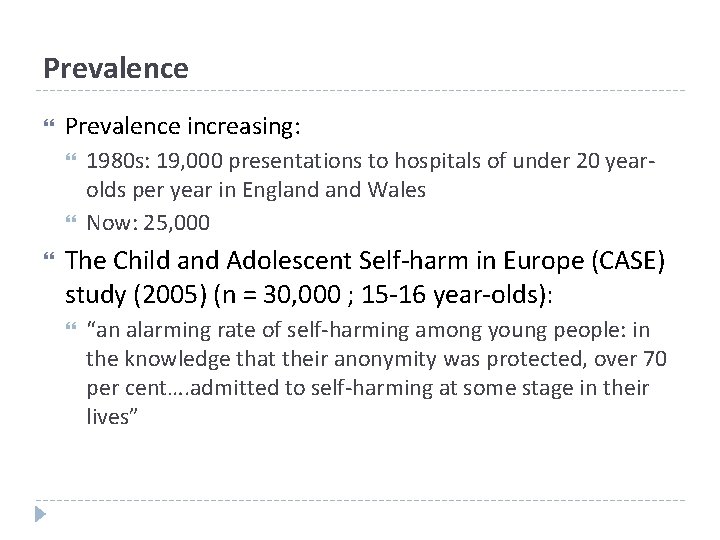
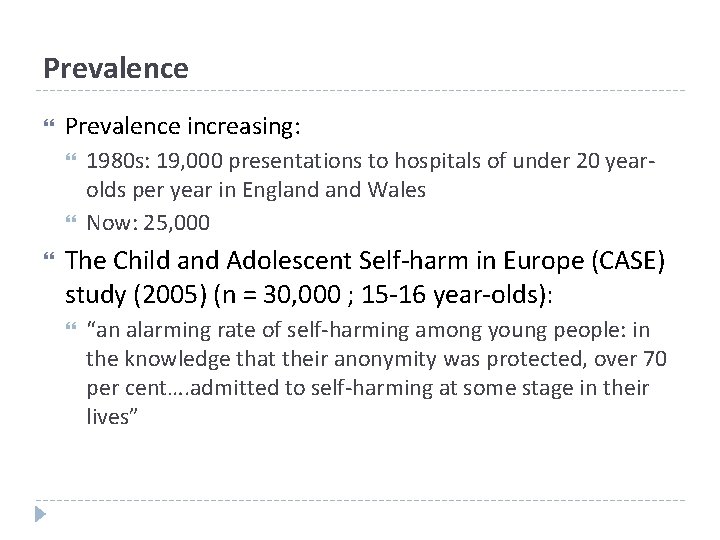
Prevalence increasing: 1980 s: 19, 000 presentations to hospitals of under 20 yearolds per year in England Wales Now: 25, 000 The Child and Adolescent Self-harm in Europe (CASE) study (2005) (n = 30, 000 ; 15 -16 year-olds): “an alarming rate of self-harming among young people: in the knowledge that their anonymity was protected, over 70 per cent…. admitted to self-harming at some stage in their lives”
Risk Factors Lack of supportive family relationships History of abuse or neglect Family psychiatric disorder Alcohol use in parent/s Substance misuse espec. alcohol School/work problems eg. bullying Some have psychiatric condition Depression Eating disorders Personality difficulties Sexuality
Why? Self-harm is always a sign of something being wrong Usually not a suicide attempt • • • But can lead to accidental death + associated with suicide risk Strongest predictor of completed suicide “People often link self-harm to suicide but for me it was something very different; it was my alternative to suicide; my way of coping even though sometimes I would wish my world would end. ” Relieve tension/anger/distress Feelings of guilt or shame Numbness secondary to trauma or abuse • feel more connected and alive To show desperation to others Change others’ behaviour or revenge
Triggers Often impulsive Often a clear precipitant A minor stressor may be ‘the last straw’ in someone who has had multiple prior adversities Arguments Drugs or alcohol impulsivity friends, family, partner Access to means eg. razors, medication
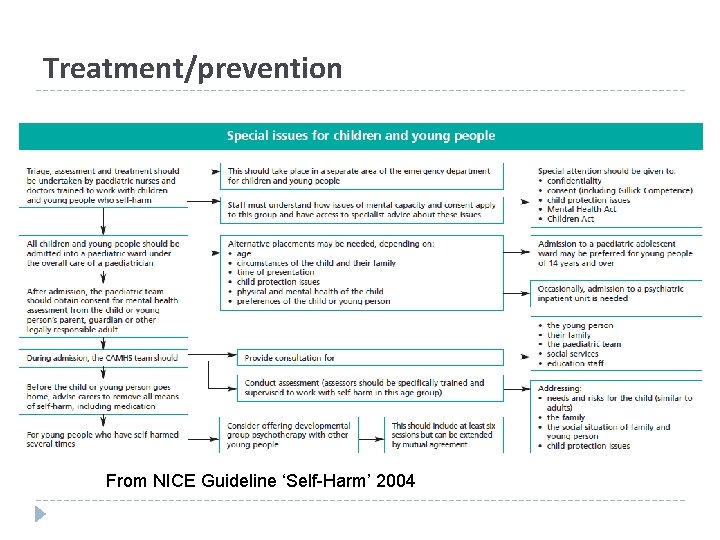
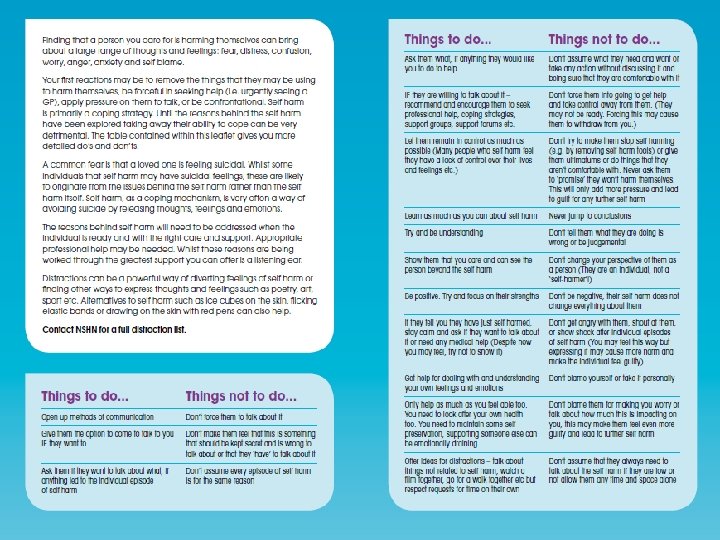
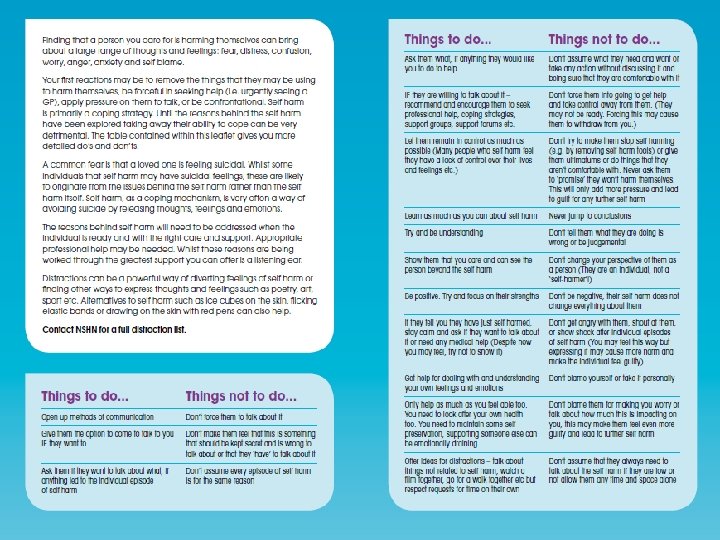
Assessment All should be assessed by ‘specialist’ Need medical assessment if OD Admit overnight under paediatrics if present to hospital (NICE guideline 2004) Ideally assess with family + alone NICE guidance 2011 on longerterm management : Include assessment of family, social situation, and child protection issues
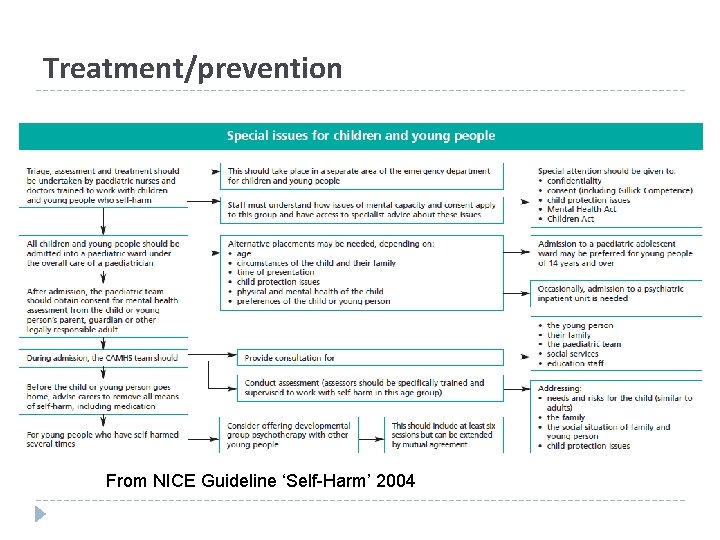
Treatment/prevention From NICE Guideline ‘Self-Harm’ 2004
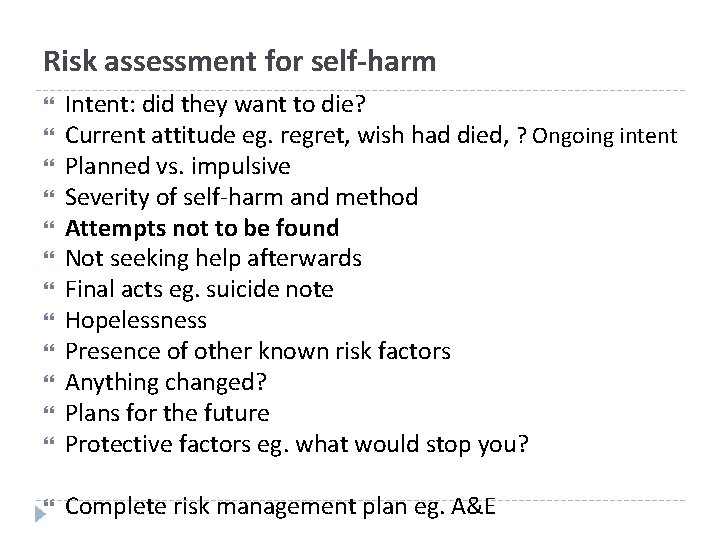
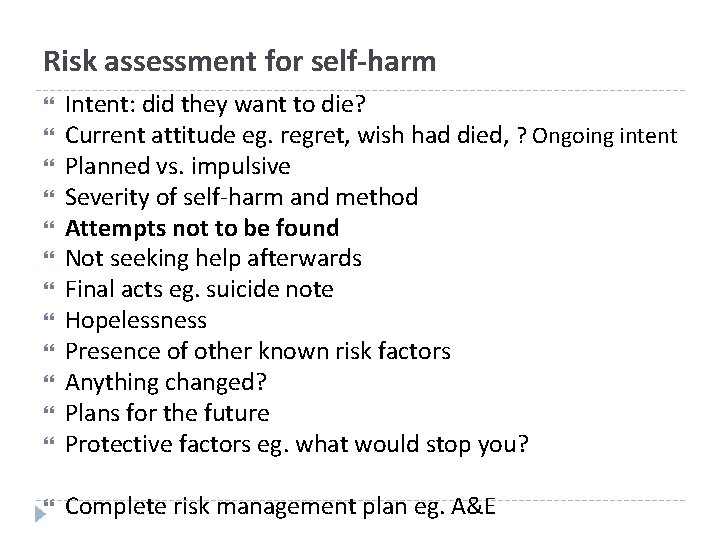
Risk assessment for self-harm Intent: did they want to die? Current attitude eg. regret, wish had died, ? Ongoing intent Planned vs. impulsive Severity of self-harm and method Attempts not to be found Not seeking help afterwards Final acts eg. suicide note Hopelessness Presence of other known risk factors Anything changed? Plans for the future Protective factors eg. what would stop you? Complete risk management plan eg. A&E
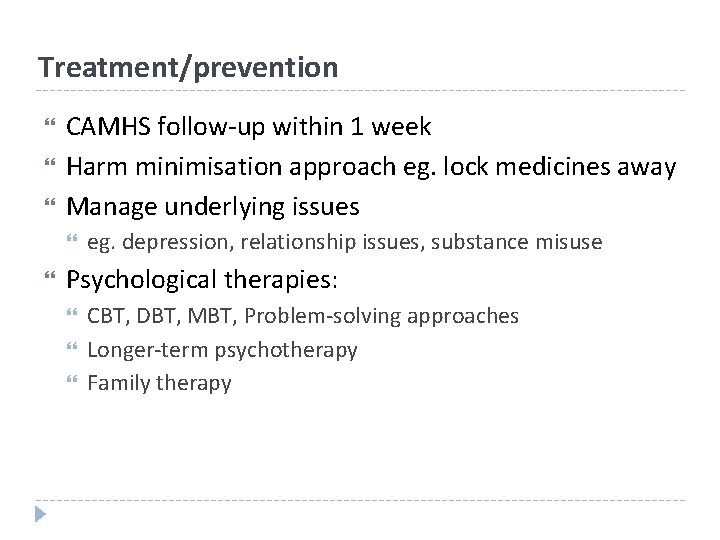
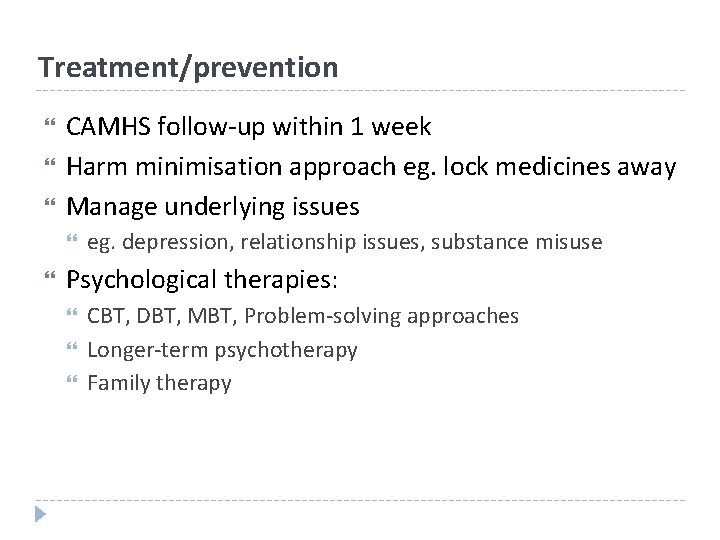
Treatment/prevention CAMHS follow-up within 1 week Harm minimisation approach eg. lock medicines away Manage underlying issues eg. depression, relationship issues, substance misuse Psychological therapies: CBT, DBT, MBT, Problem-solving approaches Longer-term psychotherapy Family therapy
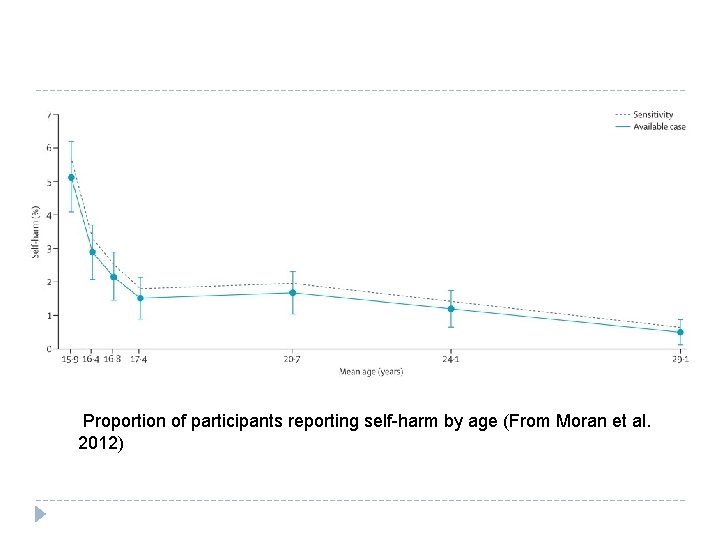
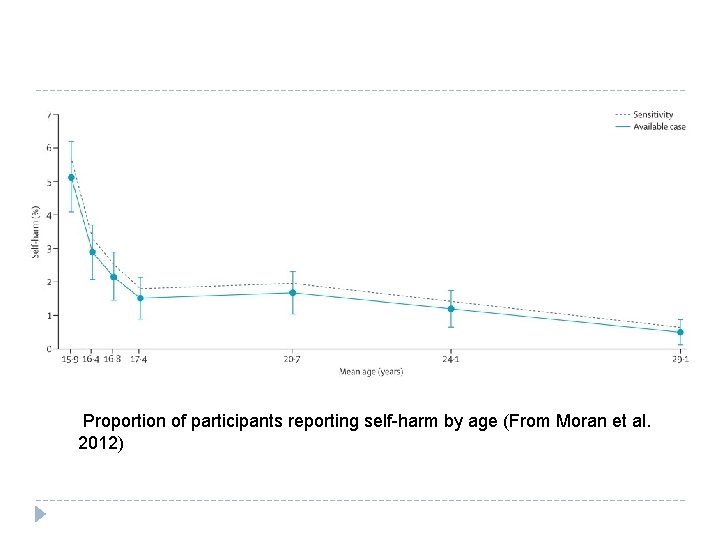
Proportion of participants reporting self-harm by age (From Moran et al. 2012)
Useful websites NSPCC/Childline http: //www. childline. org. uk/Explore/Damaging. Yourself /Pages/Self. Harm. aspx • National Self harm Network http: //www. nshn. co. uk/index. html • Youth 2 Youth http: //www. youth 2 youth. co. uk/index. htm • The Site http: //www. thesite. org/healthandwellbeing/mentalhe alth/selfharm •

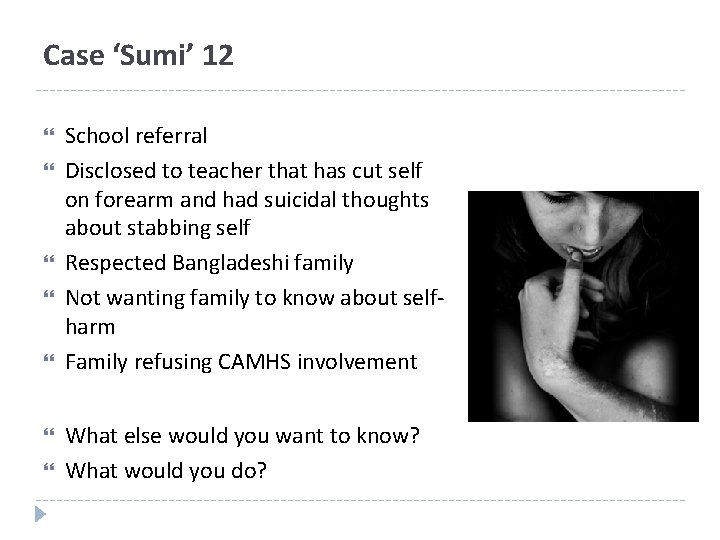
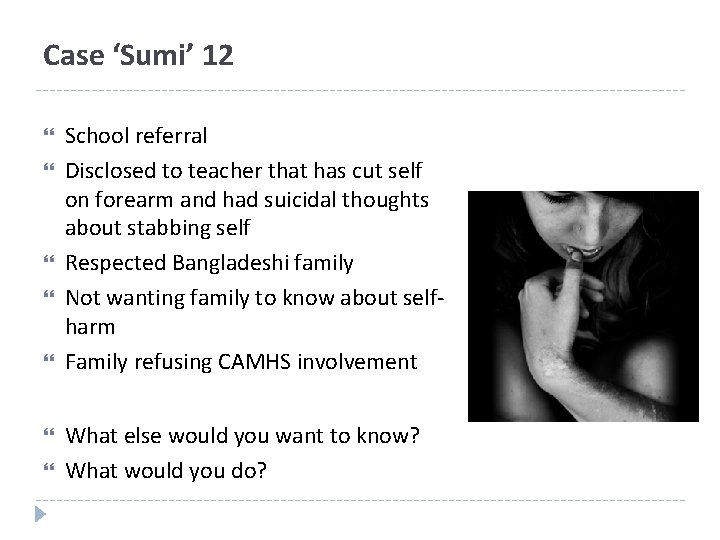
Case ‘Sumi’ 12 School referral Disclosed to teacher that has cut self on forearm and had suicidal thoughts about stabbing self Respected Bangladeshi family Not wanting family to know about selfharm Family refusing CAMHS involvement What else would you want to know? What would you do?