Call Dont let them fall Role Modeling Safe


- Slides: 43
Call! Don’t let them fall! Role Modeling Safe Infant Sleep in the hospital setting to reduce infant injury and mortality Speaker: Becky Gams, MS, APRN, Advanced Practice Nurse Leader, University of Minnesota Masonic Children’s Hospital and AWHONN member
Objectives: 1) Describe current infant safe sleep recommendations. 2) Identify practices in the hospital setting that role model infant safe sleep for families. 3) Identify clinical practices to reduce infant mortality and prevent hospital based injury due to newborn falls. Target Audience: • Obstetric and pediatric providers, nurses, administrators, risk managers, patient safety officers, other health care professional staff.
Literature Review • Why is this important? – Under reported and under recognized – Babies can be injured in the fall – Those involved have emotional consequences of guilt and emotional distress – Legal implications – Financial costs • How do safe sleep practices impact newborn falls/drops? – Safe sleep practices will help prevent newborn falls • What risk factors have been identified and what interventions have other hospitals taken?
Infant Mortality • 2008 -2010, Minnesota’s infant mortality rate overall (5. 0 infant deaths per 1, 000 live births) was lower than the nation’s rate (6. 4 infants deaths per 1, 000 births) • 2006 -2010, African Americans (9. 8 infant deaths per 1, 000 births) and American Indians 9. 4 infant deaths per 1, 000 births) had the highest infant mortality rates in the state. These rates are double the rate for Whites (4. 4 infant deaths per 1, 000 births) • Even when babies of African American and American Indian women are full term and normal weight, their risk of death before the age of one year, is two to three times that of Whites. (Source: MDH Infant Mortality Reduction Plan, 2015)
Infant Mortality in MN • Congenital anomalies are the leading cause of infants in MN overall, and the leading cause of death in Asians, Hispanics and Whites • Prematurity is the leading cause of infant deaths among African Americans • Sudden Unexpected Infant Death (SUID), which includes Sudden Infant Deaths Syndrome (SIDS) and sleep related deaths, are among the leading causes of infant deaths among American Indians (2006 -2010) • One of the priority goals of the MN Infant Mortality Reduction Plan includes reducing the rate of Sudden Unexpected Infant Deaths (SUIDS) and these types of infants deaths are considered preventable
Calls to Action – many organizations promote safe newborn sleep • Association for Women’s Health, Obstetrics and Neonatal Nursing, Nursing for Women’s Health 2012 – Article examined barriers, controversies and suggestions for organizations to implement safe sleep strategies • HRSA/Maternal and Child Health Bureau • Centers for Disease Control and Prevention (CDC), Division of Reproductive Health* • American Academy of Pediatrics • American College of Obstetricians and Gynecologists (ACOG)* • First Candle (www. firstcandle. org) • American Society of Investigative Pathology (ASIP) • National Institute Child Health Development (NICHD) • MDH Infant Mortality Report: Executive Summary • Minnesota Hospital Association (MHA)
Calls to Action… MHA Safe Sleep survey questions in the MN Perinatal Safety Roadmap • The facility promotes safe sleep practices by: a) modeling and teaching safe sleep practices per CDC/NIH SAFE to Sleep Campaign b) providing patient/family education on preventing newborn falls • Recent survey of 21 MN hospitals using the MN Perinatal Safety Roadmap (6 Critical Access and 15 PPH) showed that only 62% of the two questions were answered yes. The MHA Perinatal Safety Advisory Team finds this alarming!
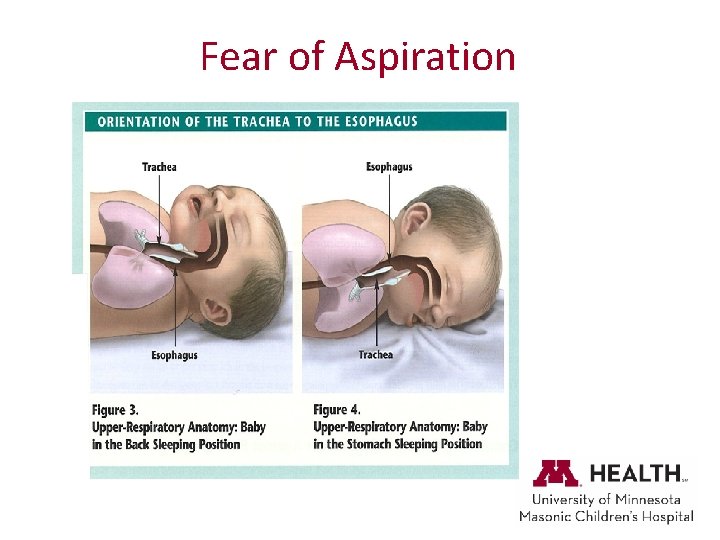
Role Modeling Safe Sleep: Nursing attitudes and knowledge • 13 of 16 studies in the review found that nurses and some mothers continue to use non-supine positioning. • 4 of the 16 studies discussed non-compliance with AAP recommendations • 11 of the 16 studies found nurses were providing incorrect information on safe sleep positioning to mothers • 5 of the 16 studies noted that nurses and mothers reported that fear of aspiration was the reasoning for not using supine positioning (Patton, 2015)
Role Modeling Safe Sleep Practices – Impacts on Parental Behavior • Reinforcing safe infant sleep practices via an intensive hospital based parent education initiative improved parent compliance with SIDS risk reduction recommendations. (Goodstein, March 2015)
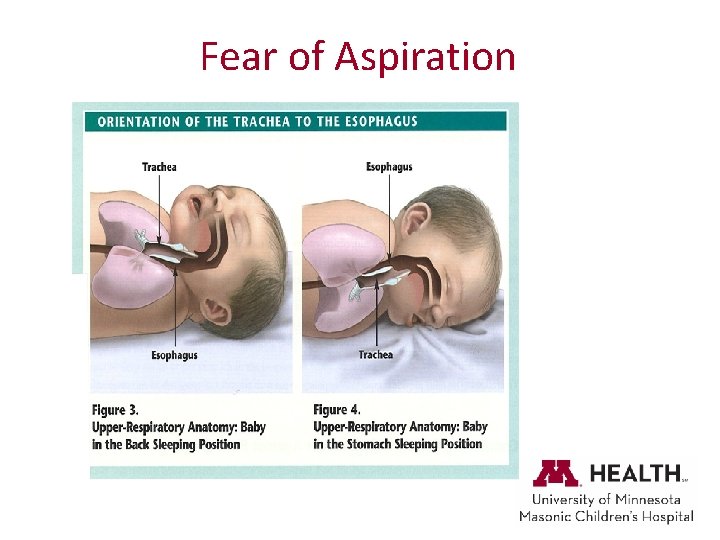
Fear of Aspiration
Speaking out on safe infant sleep recommendations • Overemphasis on no-bed sharing has created unintended consequences – mothers breastfeeding on fluffy sofas and falling asleep to avoid bed sharing • Other risks are greater: – – Prenatal and postnatal smoke exposure, sleeping with impaired adults, shared sleep on sofa and formula feeding • Tired parents need to feed their infants somewhere at night • This article recommends careful messaging regarding bed sharing as this could lead to more sofa sharing and cessation of breastfeeding (Bartick, 2014)
NICHD Safe to Sleep Campaign • AAP Policy Statement 2011 • Guess how long the NICHD has been promoting safe infant sleep? • 20 years as of 2014!
Example of Safe Sleep Practice: QI project in Georgia • Project aims: 1. Evaluation of current safe sleep promotion • No policy or guideline • Limited educational materials for parents • Compliance audits 2. Updating guidelines and parent education to include 2011 AAP recommendations • Policy written • Materials chosen with help of Parent Advisors • Results of evaluation shared with Administration (Abney-Roberts, S. E. 2015)
Aims of Georgia project continued: 3. Provide educational sessions to nursing and medical staff • Improve knowledge of AAP recommendations • Promote consistent role modeling of and education of safe sleep practices • Provided rationale for the AAP recommendations including physiology and concrete examples • Included new interns in Pediatrics, OB and Family Medicine 4. Evaluate Safe Sleep practice standards after the education sessions • Improvements in all categories of care providers (all statistically significant improvement in post test scores) 5. Improved documentation options for nursing Results: • Statistically significant improvement in pre vs post educational survey for all unit staff including providers • statistically significant improvement in crib audits
Now let’s look at newborn falls
Definition of newborn fall • A fall in which a newborn, infant, or child being held or carried by a healthcare professional, parent, family member, or visitor falls or slips from that person’s hands, arms, lap, etc. This can occur when a child is being transferred from one person to another. The fall is counted regardless of the surface on which the child lands (e. g. bed, chair, or floor) and regardless of whether or not the fall results in injury. Falls in which a child rolls off a bed, crib, chair, table, etc. count as falls but are not classified as drops. (The American Nurses Association’s National Database of Nursing Quality Indicators (© 2014 Press Ganey Associates, Inc. )
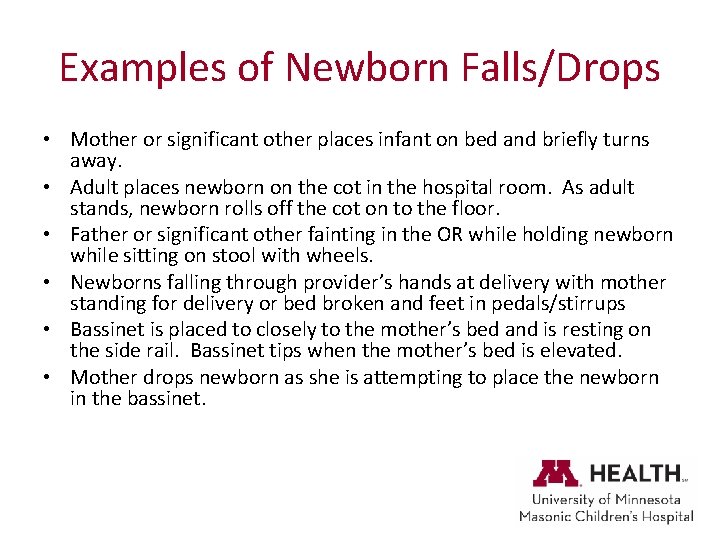
Examples of Newborn Falls/Drops • Mother or significant other places infant on bed and briefly turns away. • Adult places newborn on the cot in the hospital room. As adult stands, newborn rolls off the cot on to the floor. • Father or significant other fainting in the OR while holding newborn while sitting on stool with wheels. • Newborns falling through provider’s hands at delivery with mother standing for delivery or bed broken and feet in pedals/stirrups • Bassinet is placed to closely to the mother’s bed and is resting on the side rail. Bassinet tips when the mother’s bed is elevated. • Mother drops newborn as she is attempting to place the newborn in the bassinet.
Newborn Fall Rate • Few published statistics • Under researched and under reported • In-hospital fall rates 600 -1, 400 newborn falls occur annually (1. 6 to 4. 14/10, 000 live births. • Causes of documented falls: majority occur when mother fell asleep while holding in bed or recliner, others occur during birth or transportation • Increasing rates as more hospitals across the country implement rooming-in, skin to skin and Baby Friendly best practices • Becoming recognized as a safety issue (CDC 2012)

• • • Risk Factors identified in the literature Relationship between medication administration & newborn falls- mothers received sedating medication within 6 hours of fall Fatigue – mother, father/S. O. and other family members, previously reminded about safe sleep, nodding off, early am hours Breastfeeding and skin-to-skin Patient safety instructions given following delivery when mother and others are fatigued Mother alone, no support person with her though another study frequently found another adult in the room Fathers or S. O. in the Operating Room – Fatigue, lack of nutrition or hydration predispose to fainting or dropping baby – New environment and donning mask, gown, head/shoe covers increase warmth – OR stool instability (remove stools with wheels) Parent fell asleep while holding baby, usually in early morning hours Cesarean delivery Adult carrying the newborn fell, tripped, or had a seizure & dropped baby (small number dropped by nurse) Mother/partner awake & newborn fell from mother’s bed Families were reluctant to report the fall – Rarely discussed by nurses & providers – Night shift
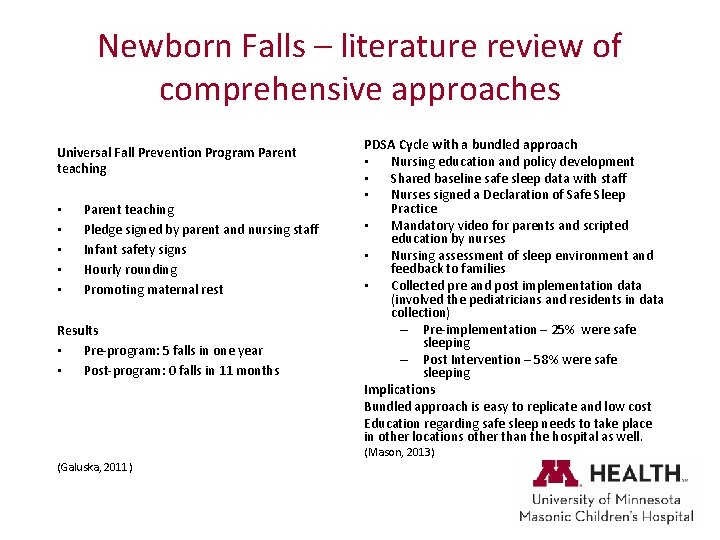
Newborn Falls – literature review of comprehensive approaches Universal Fall Prevention Program Parent teaching • • • Parent teaching Pledge signed by parent and nursing staff Infant safety signs Hourly rounding Promoting maternal rest Results • Pre-program: 5 falls in one year • Post-program: 0 falls in 11 months (Galuska, 2011) PDSA Cycle with a bundled approach • Nursing education and policy development • Shared baseline safe sleep data with staff • Nurses signed a Declaration of Safe Sleep Practice • Mandatory video for parents and scripted education by nurses • Nursing assessment of sleep environment and feedback to families • Collected pre and post implementation data (involved the pediatricians and residents in data collection) – Pre-implementation – 25% were safe sleeping – Post Intervention – 58% were safe sleeping Implications Bundled approach is easy to replicate and low cost Education regarding safe sleep needs to take place in other locations other than the hospital as well. (Mason, 2013)
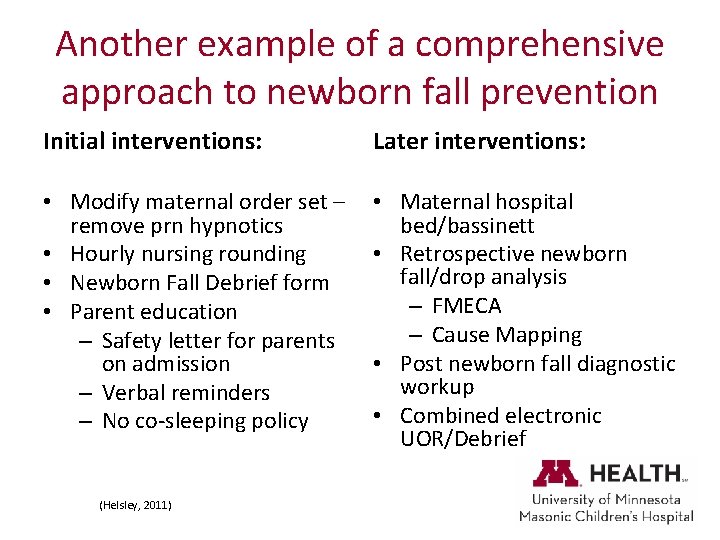
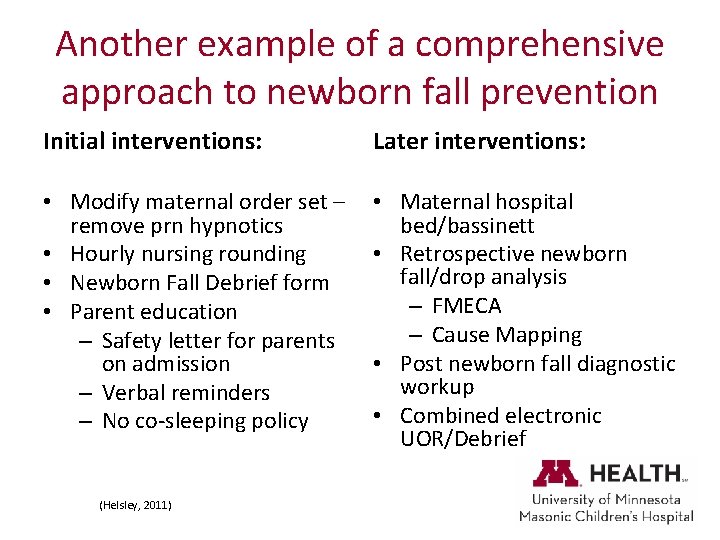
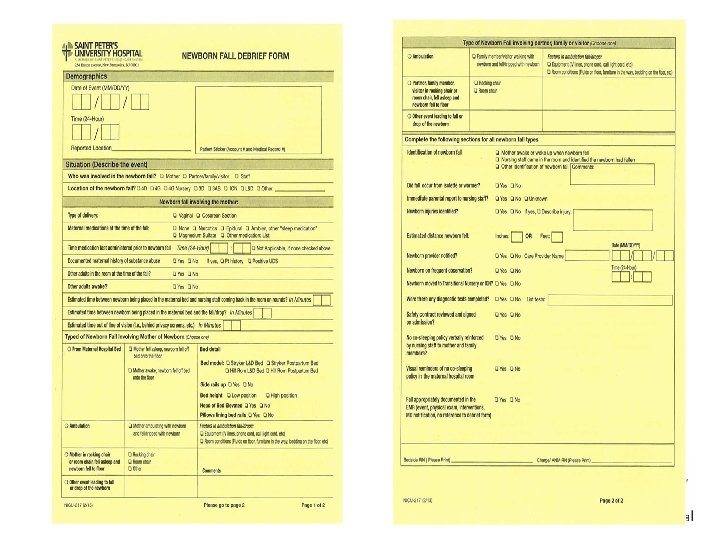
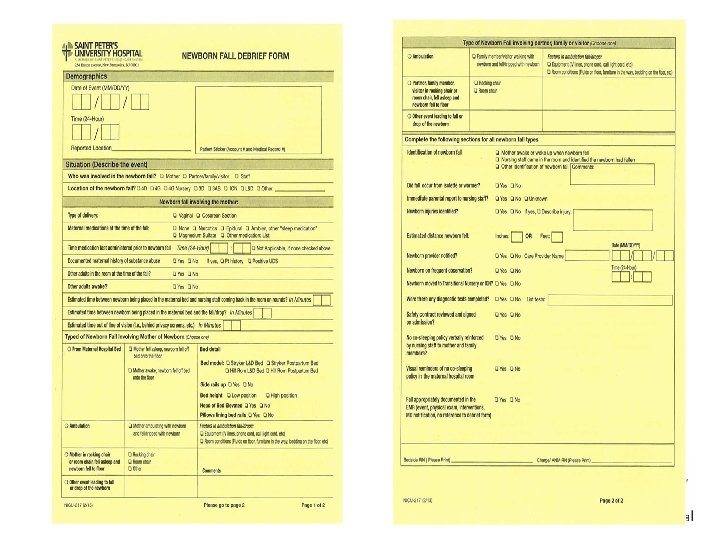
Another example of a comprehensive approach to newborn fall prevention Initial interventions: Later interventions: • Modify maternal order set – remove prn hypnotics • Hourly nursing rounding • Newborn Fall Debrief form • Parent education – Safety letter for parents on admission – Verbal reminders – No co-sleeping policy • Maternal hospital bed/bassinett • Retrospective newborn fall/drop analysis – FMECA – Cause Mapping • Post newborn fall diagnostic workup • Combined electronic UOR/Debrief (Helsley, 2011)
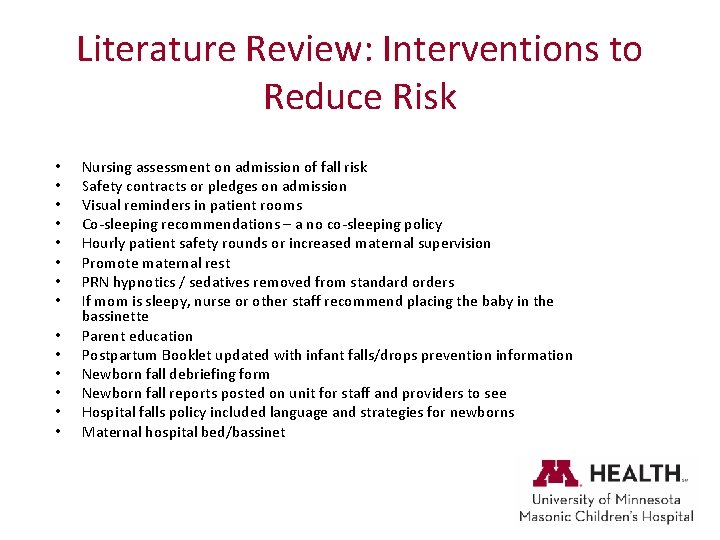
Literature Review: Interventions to Reduce Risk • • • • Nursing assessment on admission of fall risk Safety contracts or pledges on admission Visual reminders in patient rooms Co-sleeping recommendations – a no co-sleeping policy Hourly patient safety rounds or increased maternal supervision Promote maternal rest PRN hypnotics / sedatives removed from standard orders If mom is sleepy, nurse or other staff recommend placing the baby in the bassinette Parent education Postpartum Booklet updated with infant falls/drops prevention information Newborn fall debriefing form Newborn fall reports posted on unit for staff and providers to see Hospital falls policy included language and strategies for newborns Maternal hospital bed/bassinet
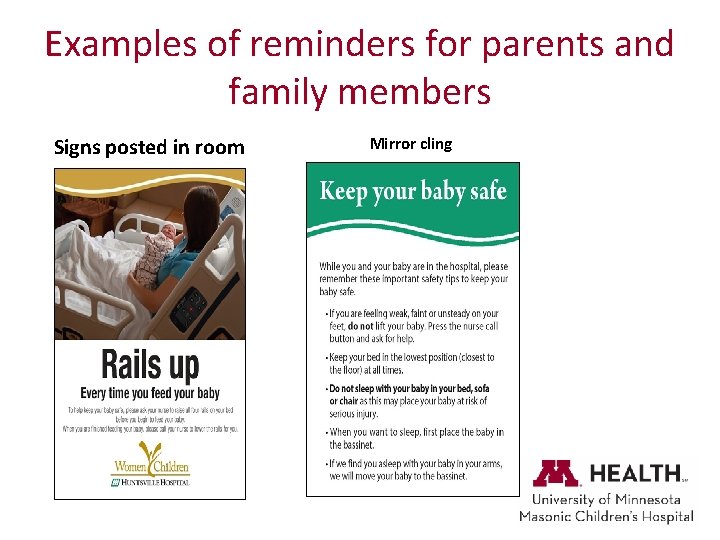
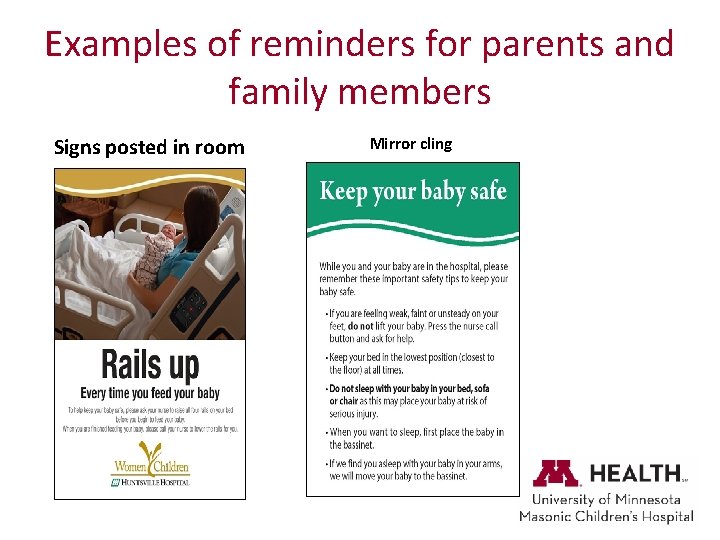
Examples of reminders for parents and family members Signs posted in room Mirror cling
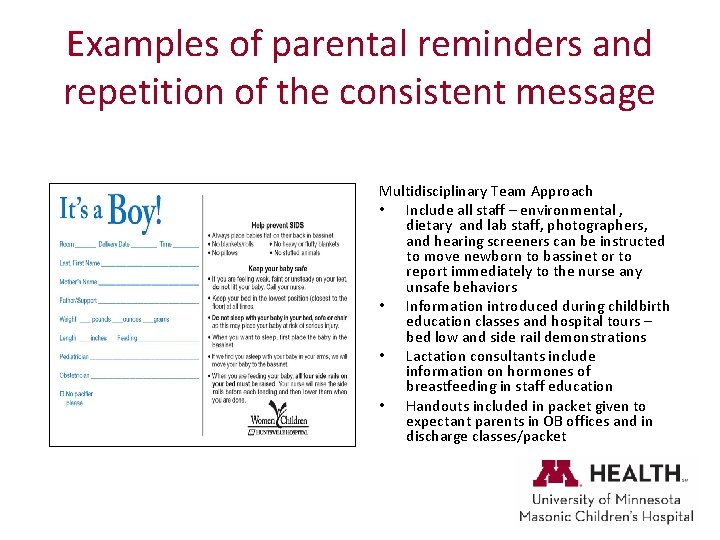
Examples of parental reminders and repetition of the consistent message Multidisciplinary Team Approach • Include all staff – environmental , dietary and lab staff, photographers, and hearing screeners can be instructed to move newborn to bassinet or to report immediately to the nurse any unsafe behaviors • Information introduced during childbirth education classes and hospital tours – bed low and side rail demonstrations • Lactation consultants include information on hormones of breastfeeding in staff education • Handouts included in packet given to expectant parents in OB offices and in discharge classes/packet
Raising Awareness and Reporting • Transparency in adverse event reporting • Clear patient falls policy that includes newborn falls • Consider creating a Newborn fall/drop clinical work up algorithm that clearly outlines assessment for nursing and providers • Consider a newborn fall/drop debrief form • National Database of Nursing Quality Indicators (NDNQI) – Spring 2013 added reporting of newborn fall/drops with and without injury
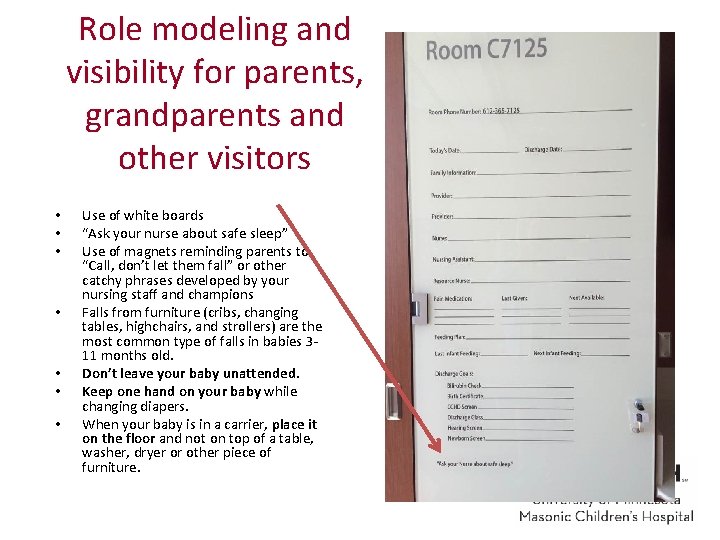
Role modeling and visibility for parents, grandparents and other visitors • • Use of white boards “Ask your nurse about safe sleep” Use of magnets reminding parents to “Call, don’t let them fall” or other catchy phrases developed by your nursing staff and champions Falls from furniture (cribs, changing tables, highchairs, and strollers) are the most common type of falls in babies 311 months old. Don’t leave your baby unattended. Keep one hand on your baby while changing diapers. When your baby is in a carrier, place it on the floor and not on top of a table, washer, dryer or other piece of furniture.

Suggested Interventions: Raising lower rail during infant feeding might prevent infant falls
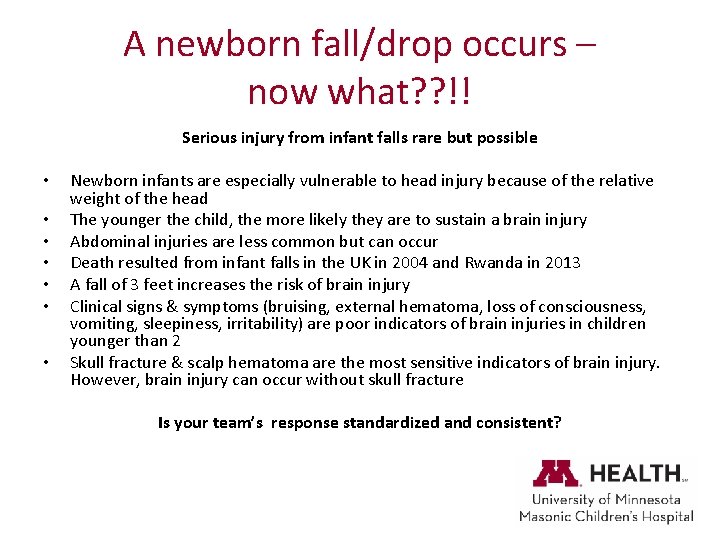
A newborn fall/drop occurs – now what? ? !! Serious injury from infant falls rare but possible • • Newborn infants are especially vulnerable to head injury because of the relative weight of the head The younger the child, the more likely they are to sustain a brain injury Abdominal injuries are less common but can occur Death resulted from infant falls in the UK in 2004 and Rwanda in 2013 A fall of 3 feet increases the risk of brain injury Clinical signs & symptoms (bruising, external hematoma, loss of consciousness, vomiting, sleepiness, irritability) are poor indicators of brain injuries in children younger than 2 Skull fracture & scalp hematoma are the most sensitive indicators of brain injury. However, brain injury can occur without skull fracture Is your team’s response standardized and consistent?
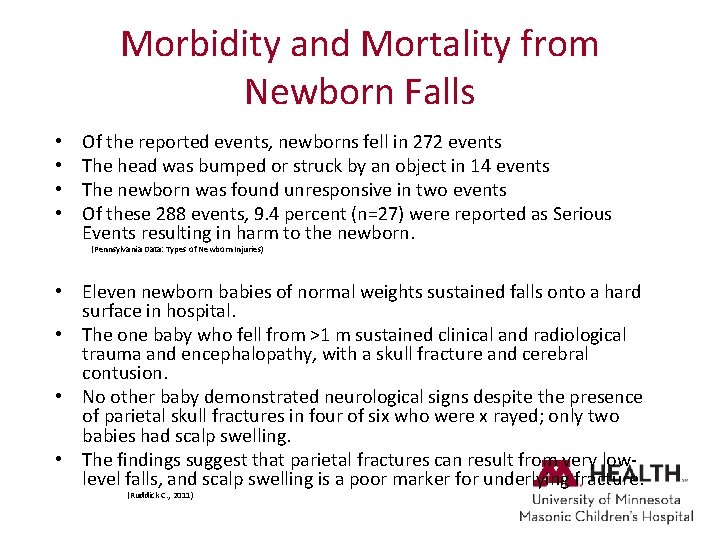
Morbidity and Mortality from Newborn Falls • • Of the reported events, newborns fell in 272 events The head was bumped or struck by an object in 14 events The newborn was found unresponsive in two events Of these 288 events, 9. 4 percent (n=27) were reported as Serious Events resulting in harm to the newborn. (Pennsylvania Data: Types of Newborn Injuries) • Eleven newborn babies of normal weights sustained falls onto a hard surface in hospital. • The one baby who fell from >1 m sustained clinical and radiological trauma and encephalopathy, with a skull fracture and cerebral contusion. • No other baby demonstrated neurological signs despite the presence of parietal skull fractures in four of six who were x rayed; only two babies had scalp swelling. • The findings suggest that parietal fractures can result from very lowlevel falls, and scalp swelling is a poor marker for underlying fracture. (Ruddick C. , 2011)
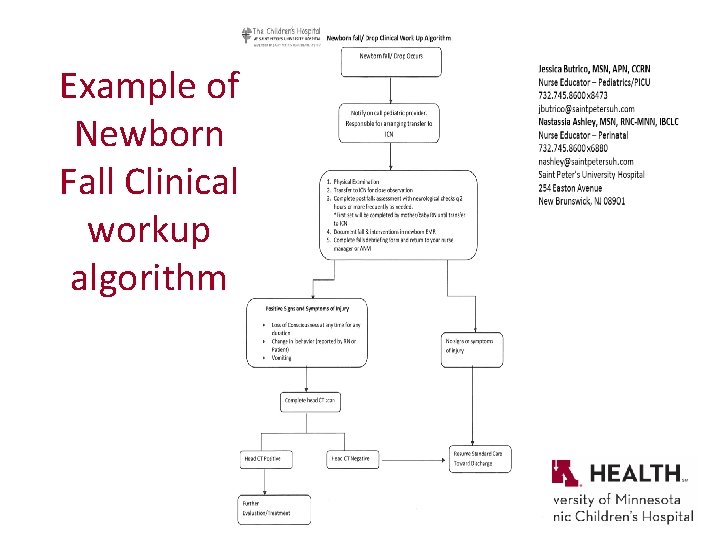
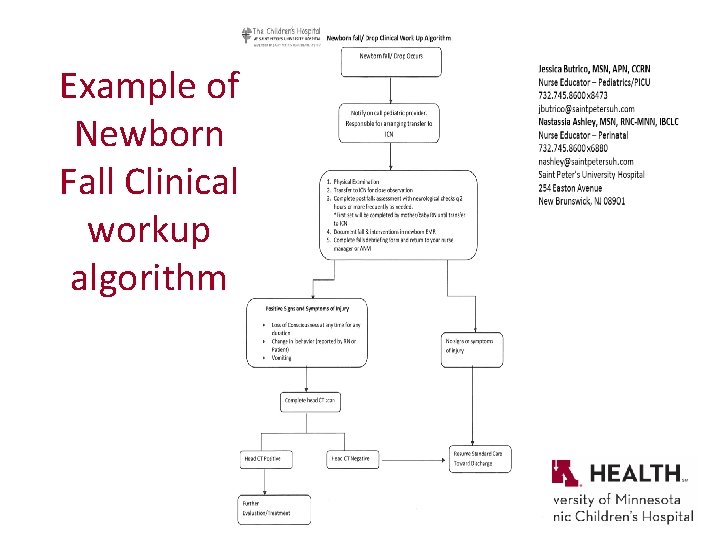
Example of Newborn Fall Clinical workup algorithm
Suggested Clinical Nursing Strategies • Educate yourself about the topic • Bed-sharing can be a risk – mother falling asleep or trying to put the baby back in the bassinette while she is in bed • Room sharing, not bed sharing • Develop or utilize a newborn risk assessment tool – Huntsville Hospital for Women & Children developed risk stratification assessment tool: low, medium and high risk. Interventions are based on the level of risk and could include moving the newborn to the nursery away from the mother’s bedside • Document newborn falls at your institution • Hourly rounding to assess maternal sleepiness • Recognize the risk of newborn falls during mother-baby care situations
Suggestions continued • Implement a safe sleep policy (no bed sharing) and include all staff – providers, nurses, support personnel, hospital administrators • Educate all staff about the policy using a variety of communication methods • Assess the patient’s learning style, preferences and knowledge deficits about infant falls • Educate mothers, support persons, and other home care givers about the risk of newborn falls and utilize teach back methodology • Utilize patient teaching materials that can be taken home and used for reference • Use translation services for interpretation of verbal instructions and translation of written instructions (Matteson, 2013)
NICU and preterm baby recommendations • • The AAP stresses that NICUs should endorse and model SUID risk reduction recommendations well before discharge. Large urban NICU team instituted: – – – • Results: – – • Algorithm to determine when SSP (safe sleep practices) should begin “back to sleep” crib card Education for staff and parents Audit tool Post discharge phone calls to audit parent reports of SSP at home Post discharge phone calls to remind parents of the importance of SSP at home Supine positioning compliance increased 39% to 83% (P<. 0010) Firm sleeping surface increased 5% to 96% (P<. 001) Removal of soft objects from bed increased 45% to 75% (P=. 001) Parental compliance reported on post discharge phone call improved 23% to 82% (P<. 001) Conclusion: multiple interventions are need to improve compliance with SSP in the NICU and home environments. (Gelfer, 2013)
University of MN Masonic Children’s Hospital strategies for newborn safe sleep and newborn fall prevention • House-wide policies – Promoting safe sleep for newborns – Safe sleep for pediatrics patients – Newborns Sharing Their Parent's Beds– specifies that if mother or other adult is found sleeping with the newborn, the newborn will be moved to the bassinette – Rooming of well newborn with hospitalized parent – specifies a that the newborn will have their own sleep space
Every unit needs a champion: Meet Toyless Tom, aka, Tom George, M. D. , Director of the NICU at University of MN Masonic Children’s Hospital.
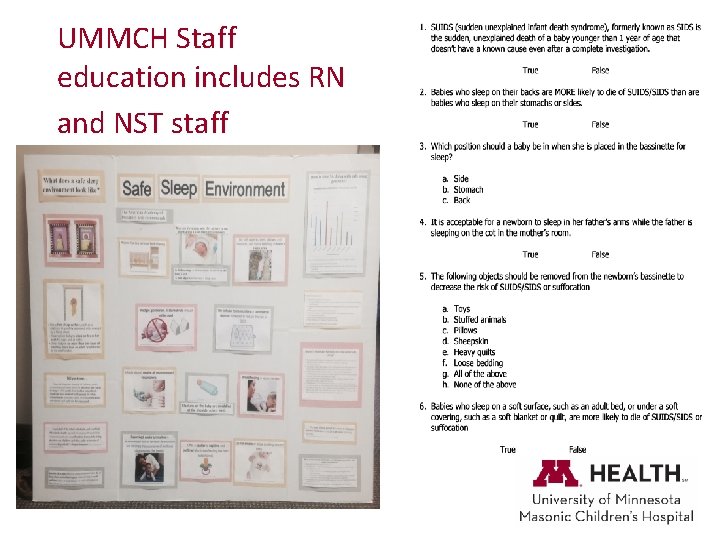
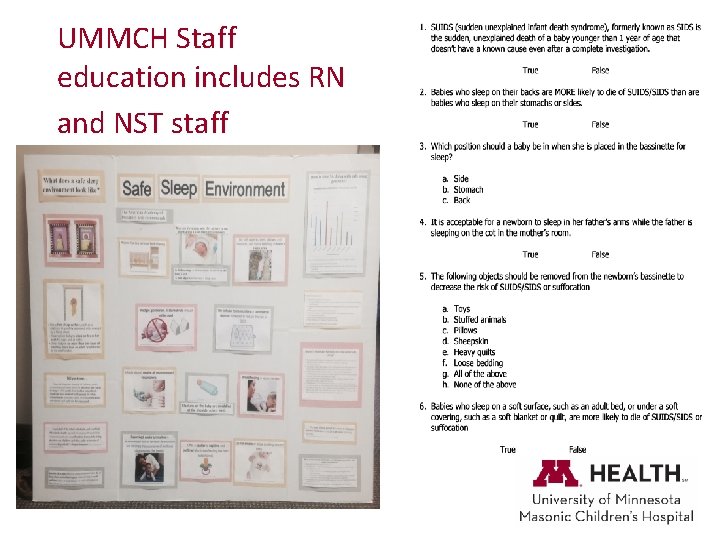
UMMCH Staff education includes RN and NST staff
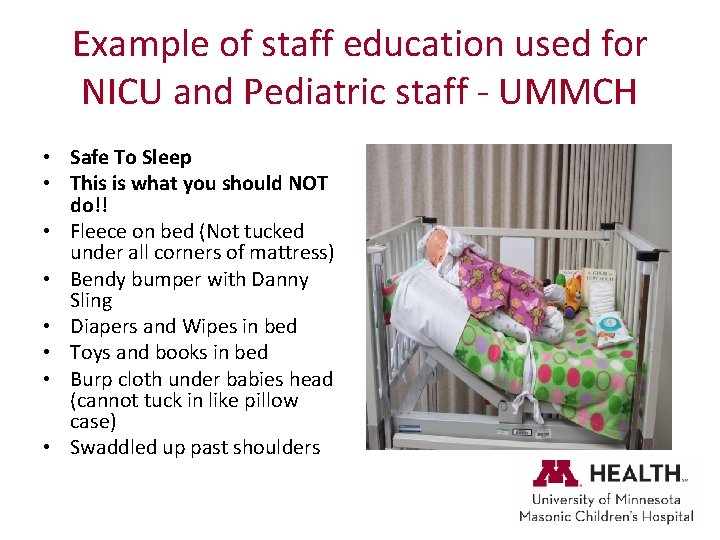
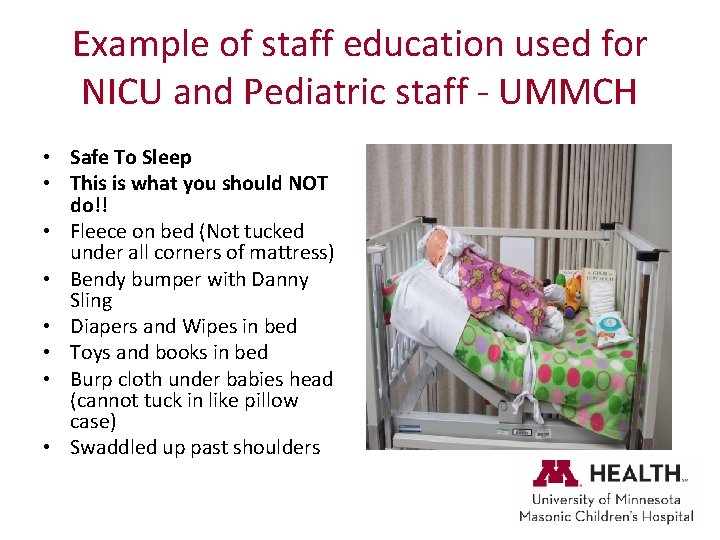
Example of staff education used for NICU and Pediatric staff - UMMCH • Safe To Sleep • This is what you should NOT do!! • Fleece on bed (Not tucked under all corners of mattress) • Bendy bumper with Danny Sling • Diapers and Wipes in bed • Toys and books in bed • Burp cloth under babies head (cannot tuck in like pillow case) • Swaddled up past shoulders
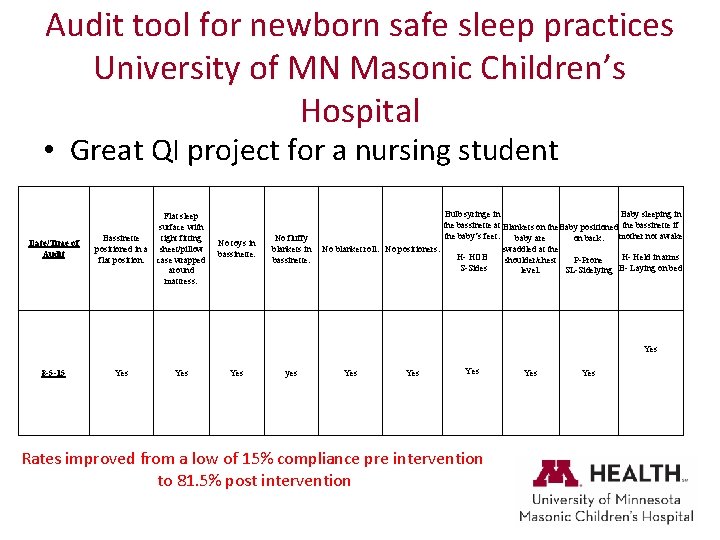
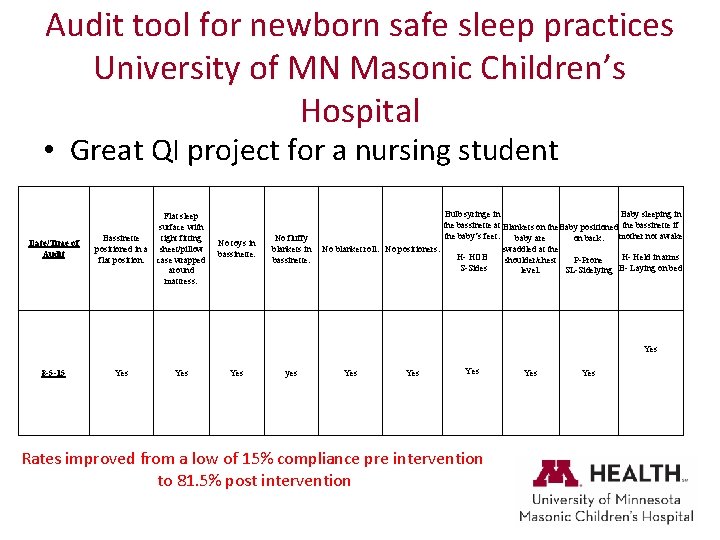
Audit tool for newborn safe sleep practices University of MN Masonic Children’s Hospital • Great QI project for a nursing student Date/Time of Audit Flat sleep surface with Bassinette tight fitting positioned in a sheet/pillow flat position. case wrapped around mattress. No toys in bassinette. No fluffy blankets in bassinette. Bulb syringe in Baby sleeping in the bassinette at Blankets on the Baby positioned the bassinette if the baby’s feet. mother not awake baby are on back. No blanket roll. No positioners. swaddled at the H- HOB H- Held in arms shoulder/chest P-Prone S-Sides level. SL-Sidelying B- Laying on bed Yes 8 -5 -15 Yes Yes yes Yes Yes Rates improved from a low of 15% compliance pre intervention to 81. 5% post intervention Yes
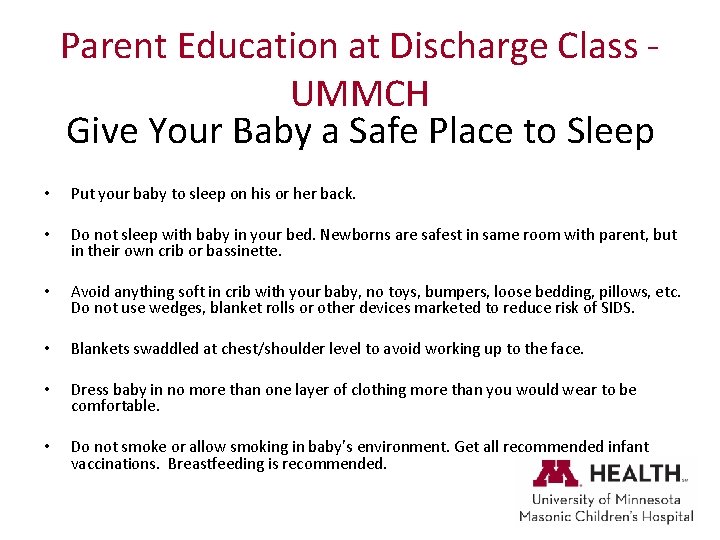
Parent Education at Discharge Class - UMMCH Give Your Baby a Safe Place to Sleep • Put your baby to sleep on his or her back. • Do not sleep with baby in your bed. Newborns are safest in same room with parent, but in their own crib or bassinette. • Avoid anything soft in crib with your baby, no toys, bumpers, loose bedding, pillows, etc. Do not use wedges, blanket rolls or other devices marketed to reduce risk of SIDS. • Blankets swaddled at chest/shoulder level to avoid working up to the face. • Dress baby in no more than one layer of clothing more than you would wear to be comfortable. • Do not smoke or allow smoking in baby’s environment. Get all recommended infant vaccinations. Breastfeeding is recommended.
Parent Education - UMMCH • Orientation to the room and the Newborn Family Care Center includes safe sleep and fall prevention • Role modeling by all nursing staff – – – removal of toys and fluffy blankets, baby back to sleep every baby every time bulb syringe at the newborn’s feet, no pacifier Swaddled with blanket at level of shoulders Halo is used for wrapping and given to family at discharge • Discharge class for parents evening prior to discharge – English, Spanish and Somali – Slides cover safe sleep practices and fall prevention • Parent education is documented in electronic medical record
References • • • • • AAP Policy Statement. SIDS and Other Sleep-Related Infant Deaths: Expansion of Recommendations for a Safe Infant Sleeping Environment. Task Force on Sudden Infant Death Syndrome. www. pediatrics. org/cgi/doi/10. 1542/peds. 2011 -2284 Abney-Roberts, S. E. , Infant Safe Sleep Practice Update: A Successful Quality Improvement Project. Presentation AWHONN Conference, , Long Beach, CA. June 2015 Ainsworth, R. M. Mog, C. , and Summerlin-Long, S. , Comprehensive Newborn Falls Strategy: The First Two Years. Huntsville Hospital for Women & Children. October 24, 2014, downloaded 8 -15 Bartick, M. , and Smith, L. J. , Speaking Out of Safe Sleep: Evidence Based Sleep Recommendations. Breastfeeding Medicine. 9(9): 417 -22, Nov. 2014. Galuska, L. Nursing for Women’s Health, 15(1); 59 -61, Feb-Mar 2011 Gelfer, P. , Cameron, R. , Masters, K. , and Kennedy, K. , Integrating “Back to Sleep” Recommendations in the Neonatal ICU Practice. Pediatrics. 131(4), April 2013. Goodstein, M. H. , Bell T. , and Krugman, S. D, Improving Infant Sleep Safety Through a Comprehensive Hospital-Based Program. Clinical Pediatrics. 54(3), 212 -21. March 2015. Helsley, L. , Mc. Donald, J. V. & Stewart, V. T. Addressing In-Hospital “Falls” of Newborn Infants. The Joint Commission Journal on Quality & Patient Safety July 2010; 327 -333. Hitchcock, S. , Endorsing Safe Infant Sleep: A Call to Action. Nursing for Women’s Health, 16. 5. Oct/Nov. 2012 ; 386 -396 Manson, B. , Ahlers-Schmidt, C. , and Schunn, C. , Improving Safe Sleep Environments for Well Newborns in the Hospital Setting. Clinical Pediatrics. 2013. 52, 10, p. 969 -975. Downloaded cpj. sagepub. com June 24, 2015. Matteson, T. , Henderson-Williams, A. , Nelson, J. , Preventing In Hospital Newborn Falls: A Literature Review. MCN, 38; 6, Nov/Dec 2013, 359366. Mc. Donald, J. , Helsley, L. , Newborn Falls/Drops in the Hospital Setting. Providence Women’s Health, downloaded Mead Johnson Virtual Club, Feb 9, 2011 Monson, S. A. , Henry, E. , Lambert, D. , Schmutz, N. , and Christensen, R. , In-Hospital Falls of Newborn Infants: Data from a Multihospital Health Care System. Pediatrics 2008; 122; e 277 -e 280. Patton, C. , Stiltner, D. , Wright, K. B. , and Kautz, D. D. , Advances in Neonatal Care. 15(1): 8 -22, Feb. 2015. Ruddick C. , Platt MW. , and Lazaro C. , Head Trauma Outcomes of Verifiable Falls in Newborn Babies. Arch Dis Child Fetal Neonatal Ed. 2010. 95(2), F 144 -5. (ISSN: 1468 -2052) Segal, D. , Hospital Newborn Falls and Drops, National Perinatal Information Center webinar, January 27, 2015. Stokowski, L. , Why Are Nurses Reluctant to Put Infants “Back to Sleep? ” Medscape. Jun 19, 2015.
Thank You. • Contact information: • Becky Gams bgams 1@fairview. org