Californias Health Care Workforce Are We Ready for

- Slides: 21
California’s Health Care Workforce: Are We Ready for the ACA? Overview: Physicians Catherine Dower Sacramento, March 14, 2012 http: //futurehealth. ucsf. edu
California’s Health Care Workforce: Readiness for the ACA Era Team: Tim Bates, MPP; Lisel Blash, MPA; Susan Chapman, BSN, MSN, Ph. D; Catherine Dower, JD; and Edward O’Neil, FAAN, MPA, Ph. D. Sponsor: Funded by The California Wellness Foundation Impetus: PPACA and Governor’s taskforce 2
Methodology • Literature review • Environmental scan • CA Department of Consumer Affairs Professional License Master. File • Key informant interviews 3
http: //futurehealth. ucsf. edu 4

5
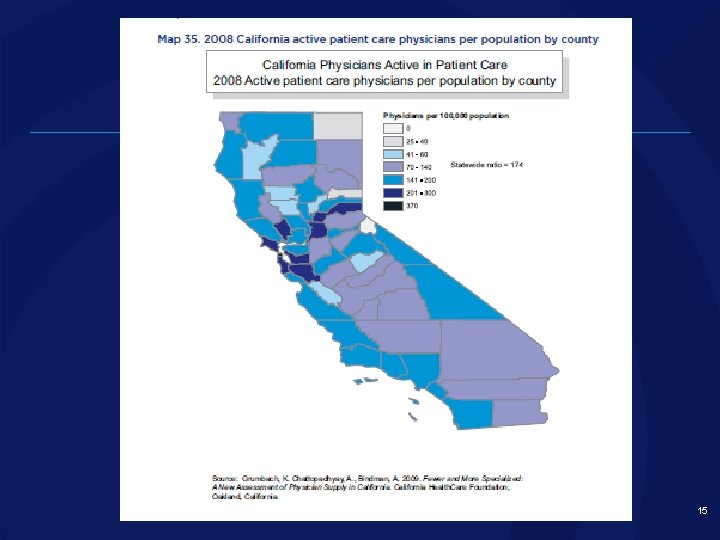
Key Findings • Health workforce major part of labor sector • Continued growth • Significant maldistribution • Growing population, more diverse population, aging population, changing disease burden • ACA implementation will strain primary care providers first 6
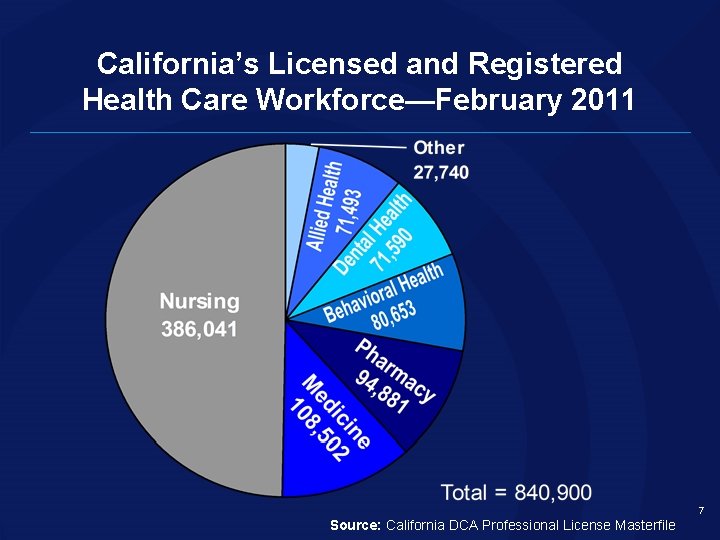
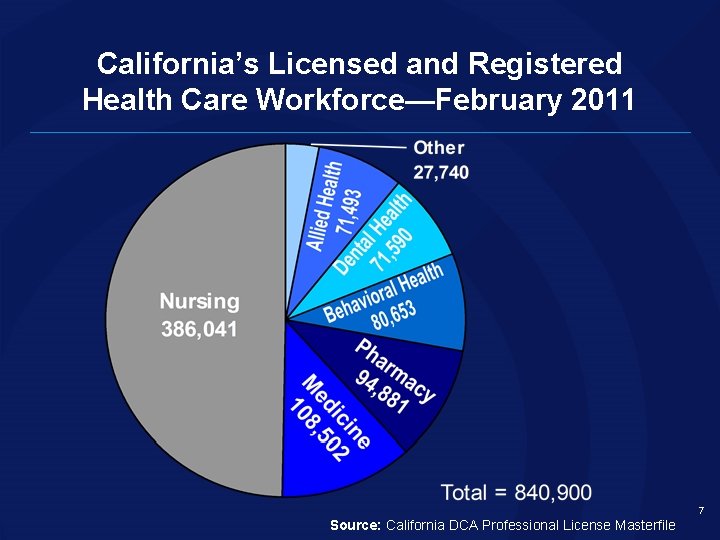
California’s Licensed and Registered Health Care Workforce—February 2011 7 Source: California DCA Professional License Masterfile
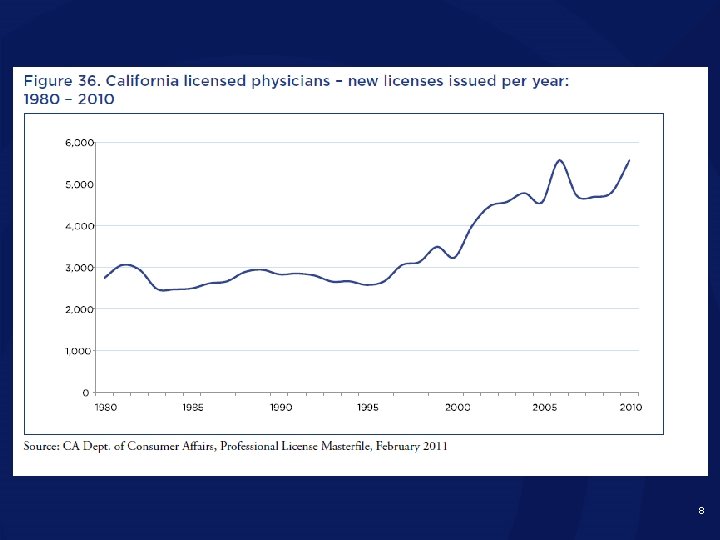
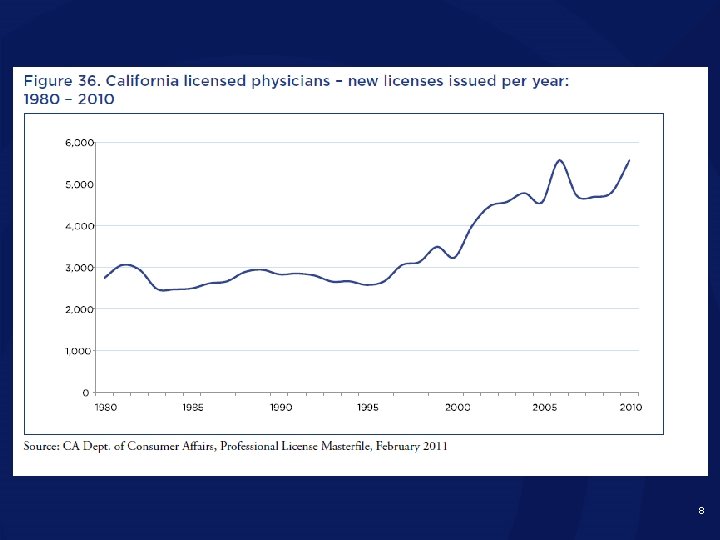
8
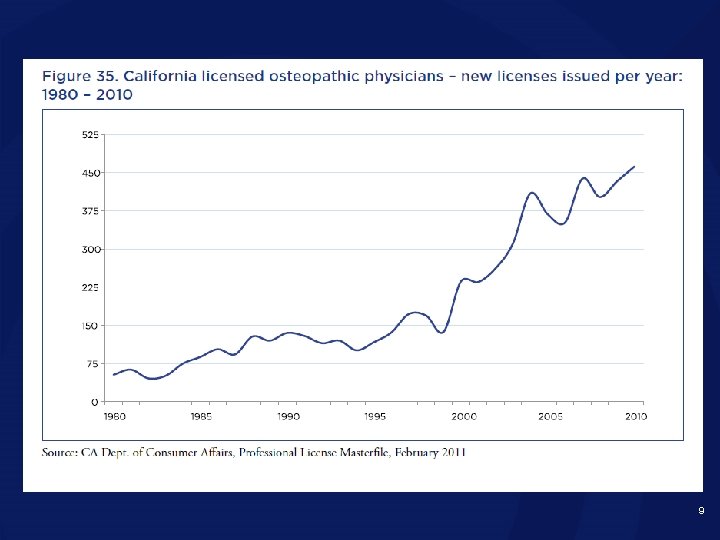
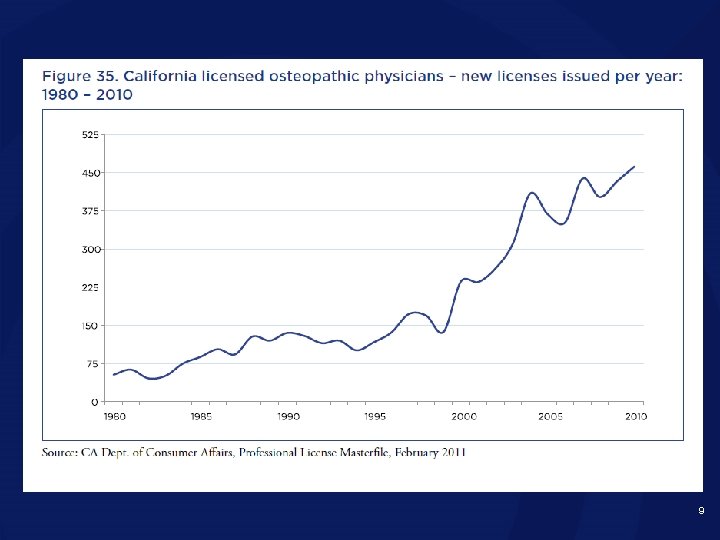
9
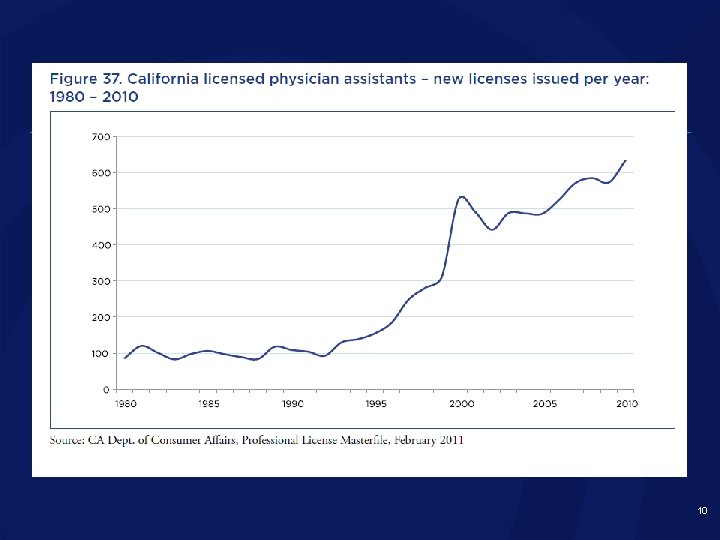
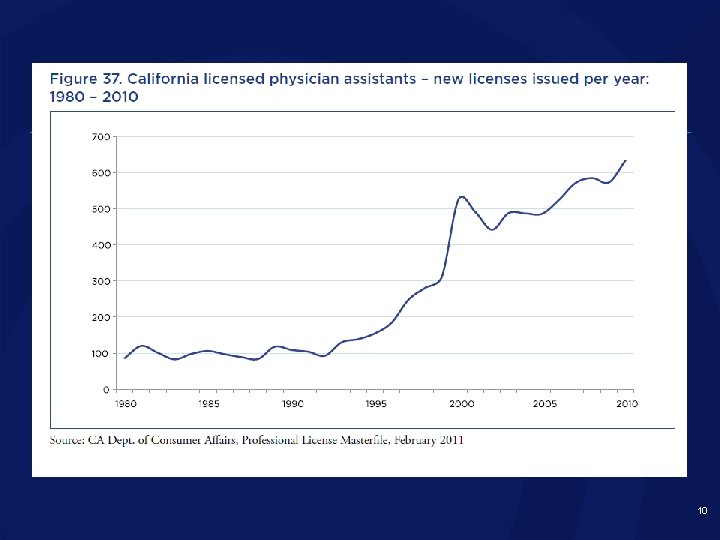
10
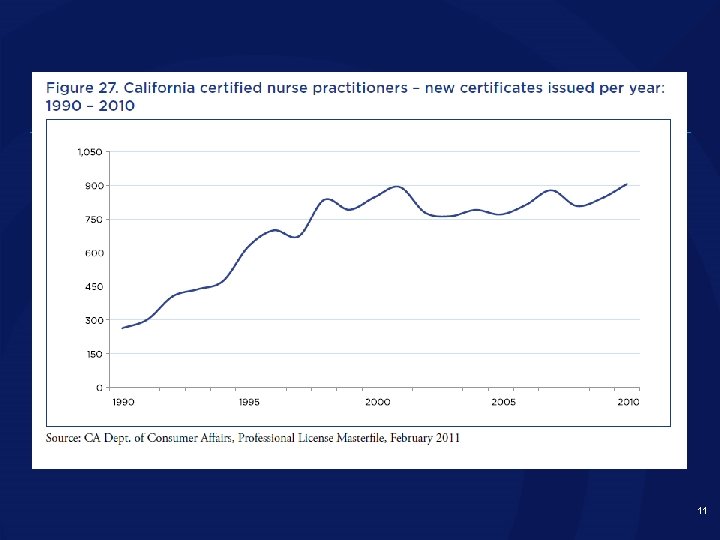
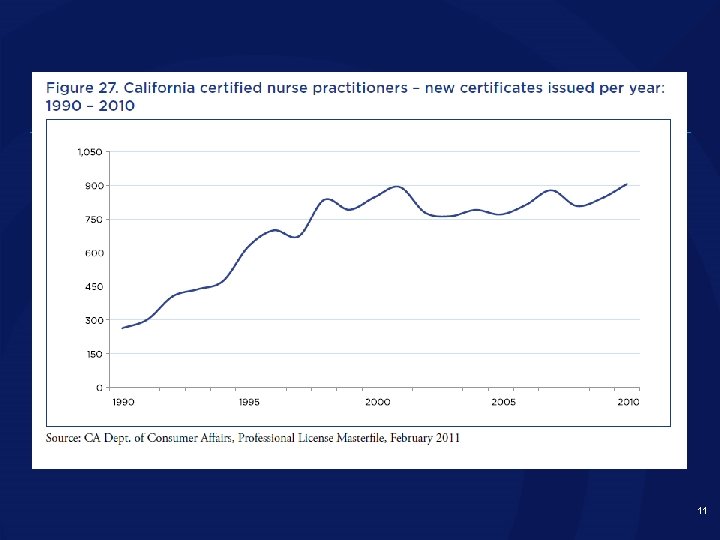
11
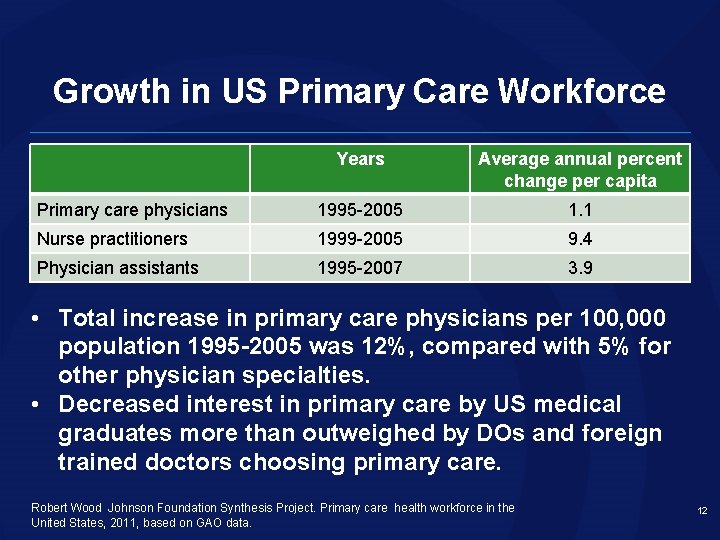
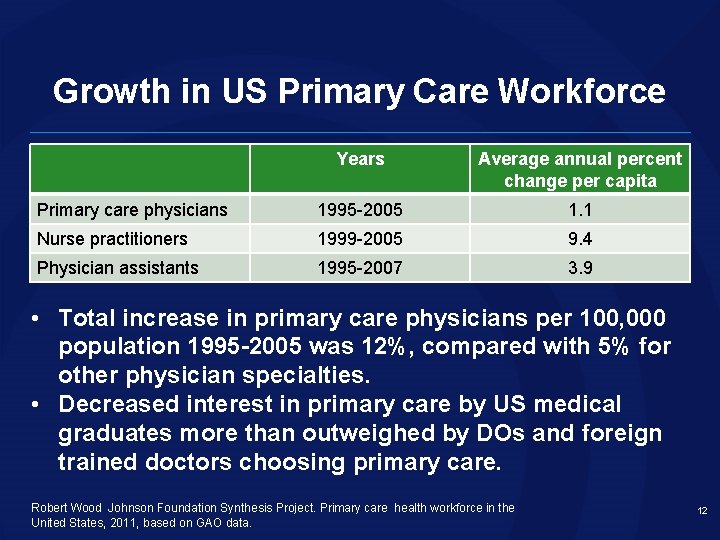
Growth in US Primary Care Workforce Years Average annual percent change per capita Primary care physicians 1995 -2005 1. 1 Nurse practitioners 1999 -2005 9. 4 Physician assistants 1995 -2007 3. 9 • Total increase in primary care physicians per 100, 000 population 1995 -2005 was 12%, compared with 5% for other physician specialties. • Decreased interest in primary care by US medical graduates more than outweighed by DOs and foreign trained doctors choosing primary care. Robert Wood Johnson Foundation Synthesis Project. Primary care health workforce in the United States, 2011, based on GAO data. 12
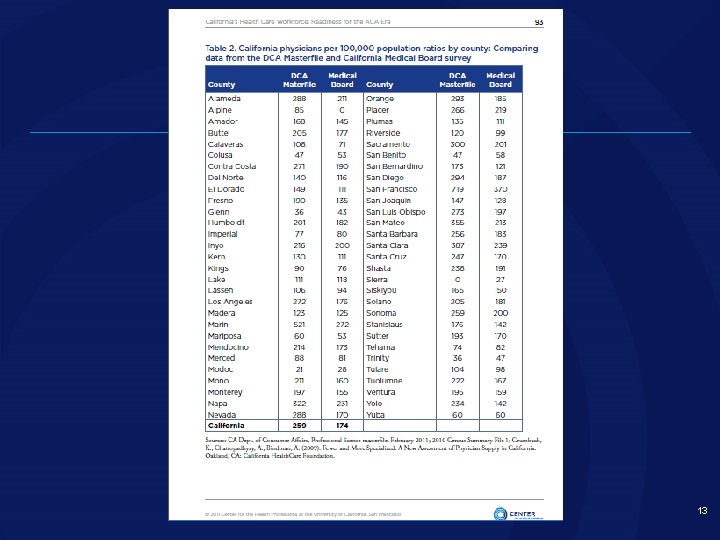
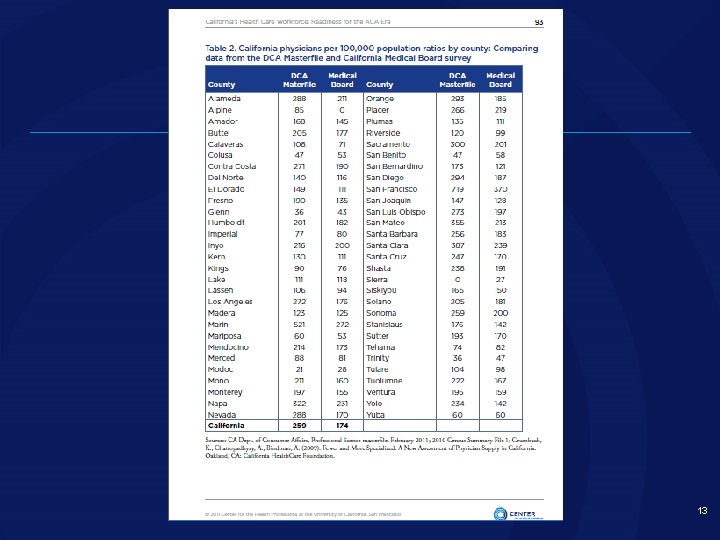
13
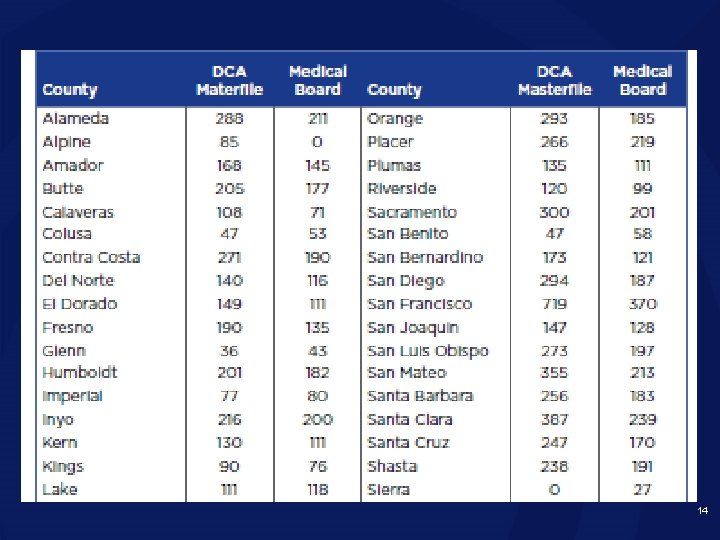
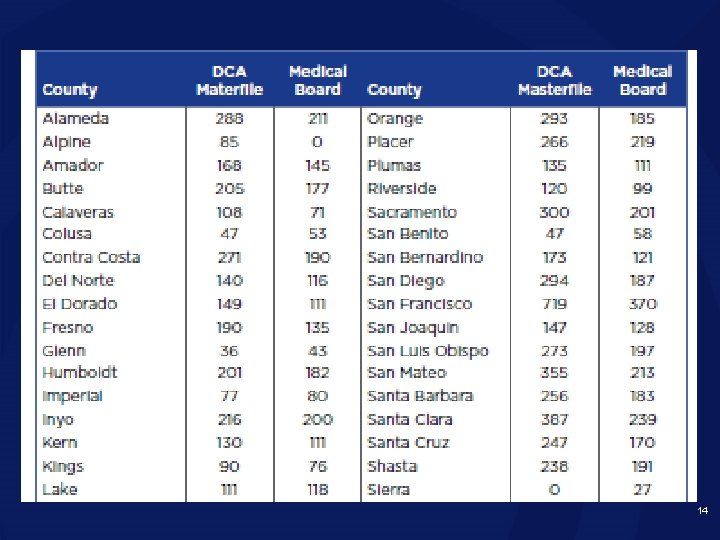
14
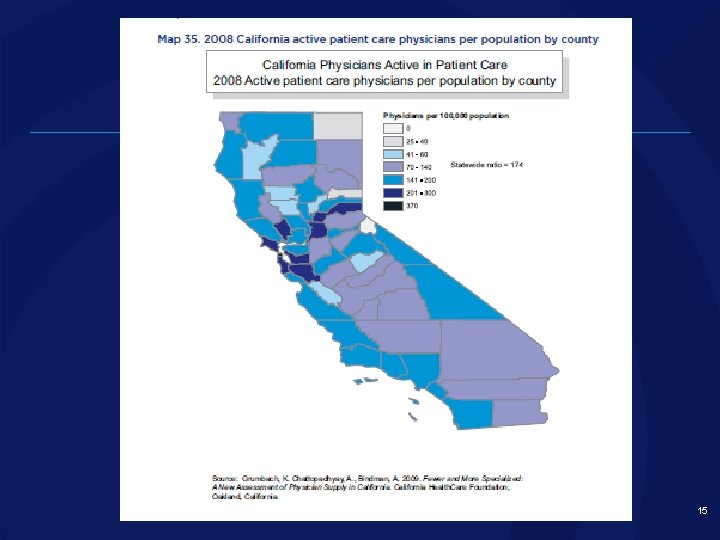
15
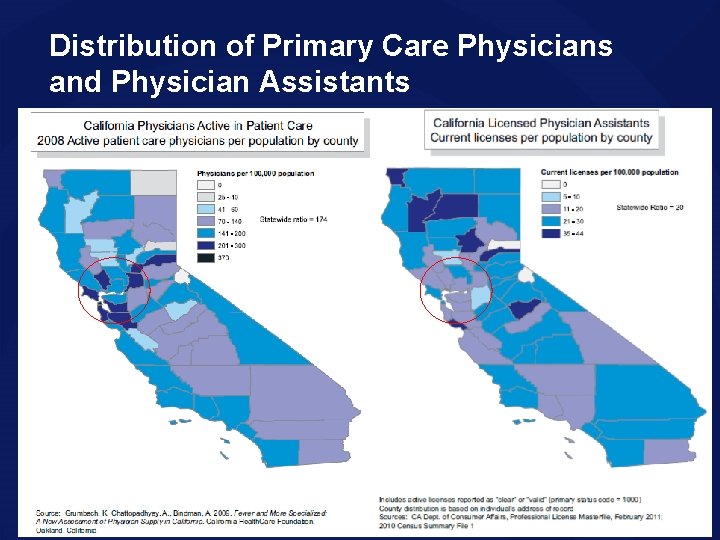
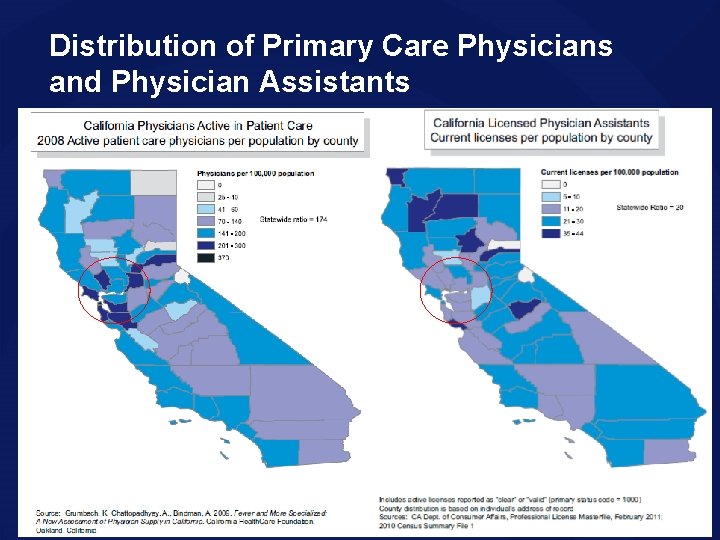
Distribution of Primary Care Physicians and Physician Assistants 16
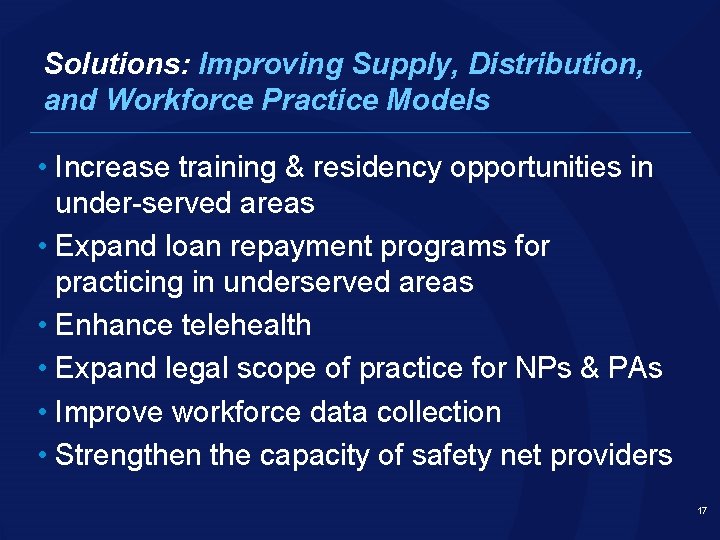
Solutions: Improving Supply, Distribution, and Workforce Practice Models • Increase training & residency opportunities in under-served areas • Expand loan repayment programs for practicing in underserved areas • Enhance telehealth • Expand legal scope of practice for NPs & PAs • Improve workforce data collection • Strengthen the capacity of safety net providers 17
Solutions: Improving the Education Pipeline • Encourage medical students to practice in primary care • Refocus some education resources on NP & PA training and innovative education models • Enhance retention in CC health careers programs • Invest in primary and secondary (K-12) education programs 18
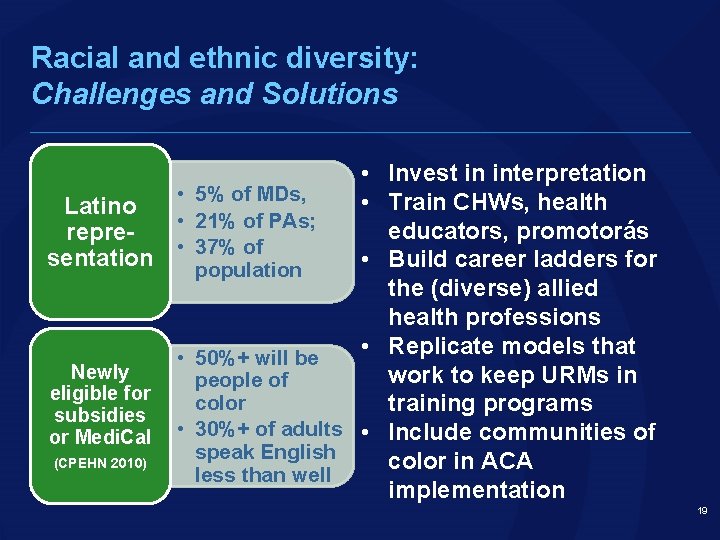
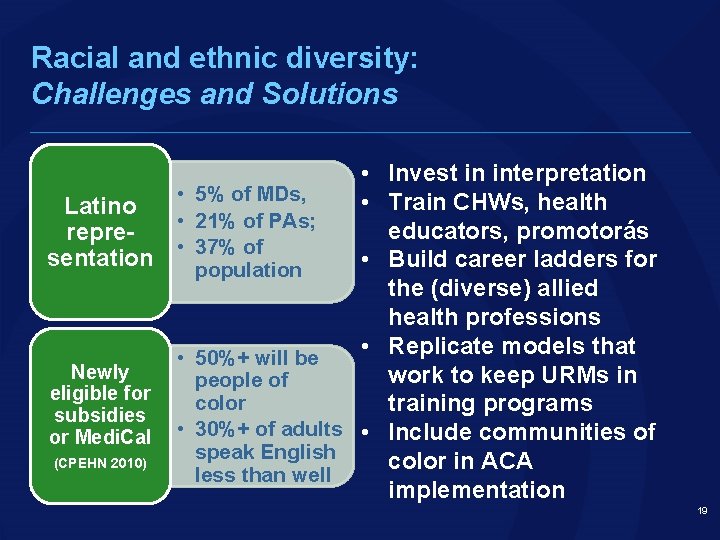
Racial and ethnic diversity: Challenges and Solutions • Latino • representation • Newly eligible for subsidies or Medi. Cal (CPEHN 2010) • • • Invest in interpretation 5% of MDs, • Train CHWs, health 21% of PAs; educators, promotorás 37% of • Build career ladders for population the (diverse) allied health professions • Replicate models that 50%+ will be work to keep URMs in people of color training programs 30%+ of adults • Include communities of speak English color in ACA less than well implementation 19
California’s Health Care Workforce: Moving Forward Challenge • Growing pressure on safety net providers • Geographic maldistribution of workforce • Diversity challenges Promise • Continued job growth despite the recession • HIT leveraged to facilitate new models of care • Alternative training programs can scale up fast • New finance and delivery models may decrease costs --improve access and quality of care 20
California’s Health Care Workforce: Readiness for the ACA Era Contact: Catherine Dower cdower@thecenter. ucsf. edu 415 -476 -1894 http: //www. futurehealth. ucsf. edu 21