Calderdale and Greater Huddersfield Integrated Health and Social






- Slides: 22
Calderdale and Greater Huddersfield Integrated Health and Social Care Strategic Review Update March 2014 Status : Issued Version: v 2 Date: 5 th March, 2014
Agenda • • • Background to the Strategic Review What our engagement to date has told us Our vision for our future system Commissioners’ responsibilities The providers’ Strategic Outline Case High level timetable and next steps
Background and Context • Seven partner organisations • 2 years - shared vision - innovate and transform services. • Transformation is needed to address the significant challenges facing the health and social care system now and in the years ahead. • • • Ageing population with increasing needs Increase of long-term health / social care needs High quality, sustainable healthcare Responding to the needs expressed by patients Limited and diminishing resources.

Background and Context • • Key overarching aims taken from the priorities in both JSNAs All partners share the vision to change the way health and social care is provided to enable: – Easy access to the right information and guidance for people to make informed choices for themselves and their families – People only have to tell their story once and are supported to make positive choices – As much care as possible is provided close to home to keep people safe, well and as healthy as possible for as long as possible – Every child has a healthy start with opportunities to achieve their full potential – High quality, safe and effective specialist care is available when needed – Different agencies make best use of shared resources

Engagement activity to date • • • More than 2, 500 people directly engaged 300 young people 44 people at planned care event 1, 700 people unplanned care survey 500 staff All national and local surveys, PALS, complaints, patient opinion and NHS choices information from the past 3 years collated. • Unplanned care engagement – 2, 500 views • Call to Action – 280 public views
What you told us you want • Timely and consistent access to services • Co-ordinated and integrated care • Services closer to home • Involve us in decisions about our care and in planning care • Better use of technology
Call to Action – 13 Themes • Education and information – all information should be available in easy to understand formats • Invest in community and primary care as well as local community and voluntary groups • National solutions and campaigns are needed for changes on a national scale • Self Care – or self help/self management • Improve access to health services. Opening times and appointment availability, particularly GP practices • Staff training including changing the culture of the NHS, communication and transparency. • Working together, all agencies, not just health, should work together to improve health and wellbeing
Call to Action – 13 Themes • Regular check-ups including annual check ups or possibly more frequent depending on the age / condition • Discharge planning and better hospitals including discharge plans with 24/7 support and hospital services in community settings. • Manage risk and safeguarding – keeping people safe when they were unwell. • More services in the community • Invest in technology – especially for monitoring and sharing information between services and patients. • Be accountable – clear measures, learn from mistakes, educate people on their rights and responsibilities and base contracting decisions on research and guidance.
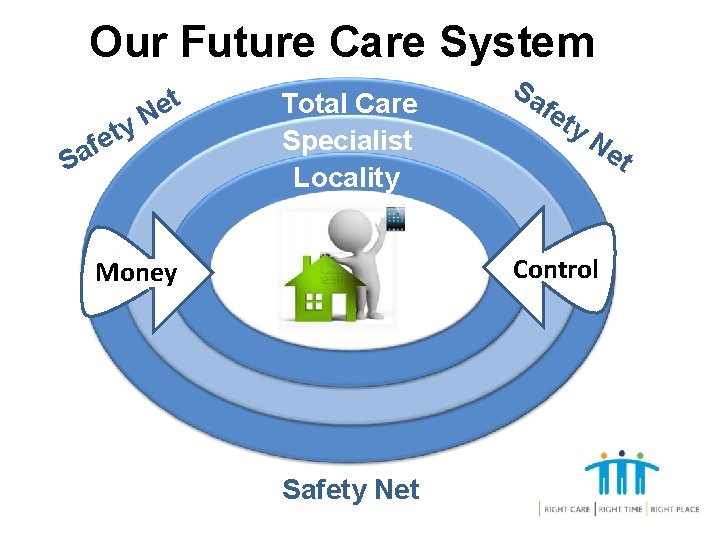
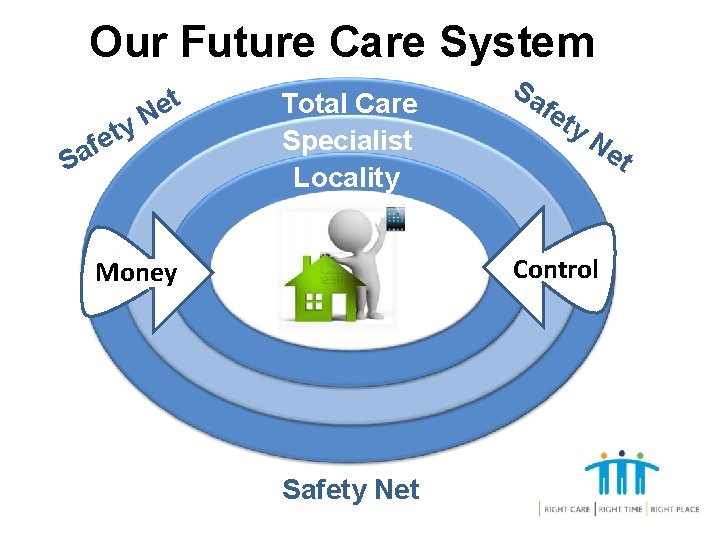
Our Future Care System Sa y t e f t e N Total Care Specialist Locality Sa fe ty Ne t Control Money Safety Net

Why are we here / Why Now? • National Clinical Advisory Team report from last summer • Parliamentary interest in September 2013 and adjournment debate in December 2013. • Media interest over the last three months Time to start talking
The Strategic Outline Case is a provider response to the Strategic Review
Commissioners’ Responsibilities • We need to make YOU feel part of designing the future • Engage the population • Statutory duty to lead the consultation • Make the final decision about services for our population.
Key points • No decision has been taken about which hospital would be the planned care site and which the unplanned site • Whatever happens, there will be some level of unplanned care provision at each hospital • We are about to undergo a mutually agreed thorough pre-consultation engagement process to identify options for consultation • Recent media coverage has not, in many instances, reflected the true position

Key points • The strategic review is about much more than the configuration of acute (including A&E) services • It is about the transformation of virtually all health and social care • We want to talk about this wider transformation with patients, public and staff - not just the scenarios identified by providers • Only then will firm proposals for consultation be identified
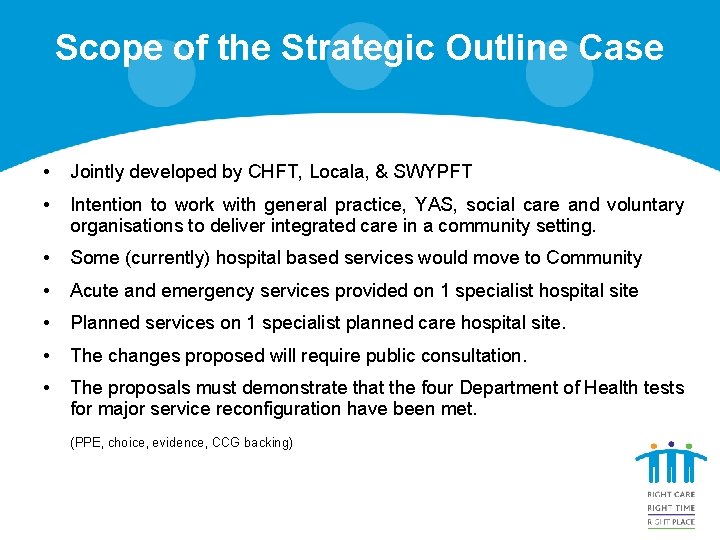
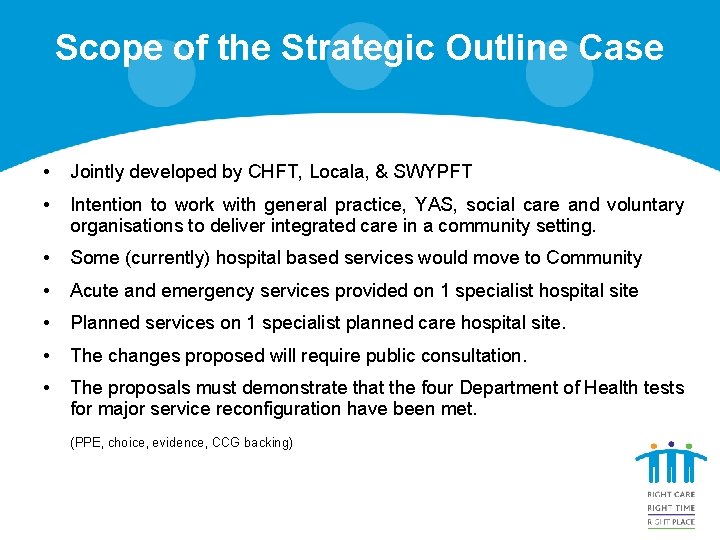
Scope of the Strategic Outline Case • Jointly developed by CHFT, Locala, & SWYPFT • Intention to work with general practice, YAS, social care and voluntary organisations to deliver integrated care in a community setting. • Some (currently) hospital based services would move to Community • Acute and emergency services provided on 1 specialist hospital site • Planned services on 1 specialist planned care hospital site. • The changes proposed will require public consultation. • The proposals must demonstrate that the four Department of Health tests for major service reconfiguration have been met. (PPE, choice, evidence, CCG backing)
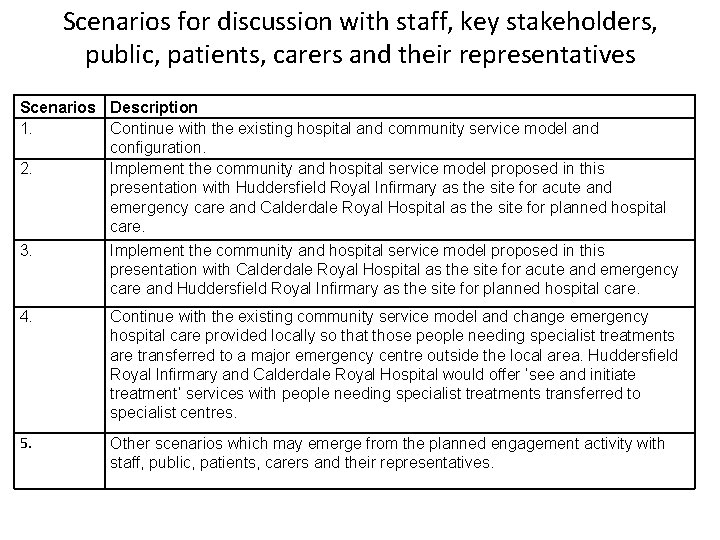
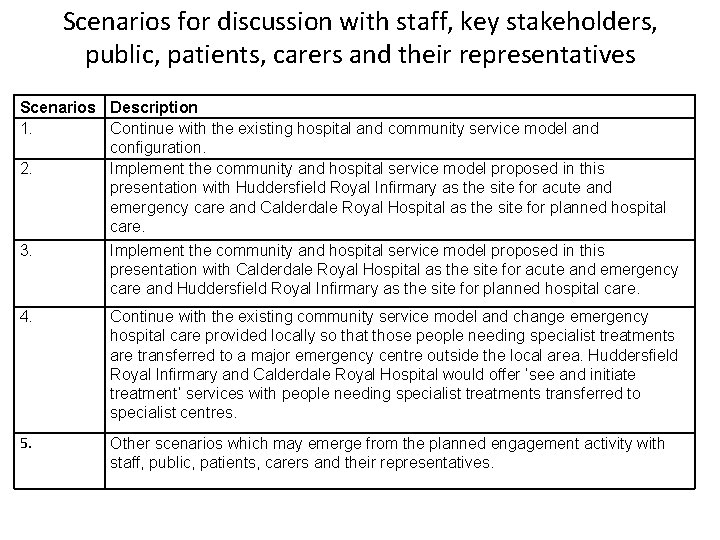
Scenarios for discussion with staff, key stakeholders, public, patients, carers and their representatives Scenarios Description 1. Continue with the existing hospital and community service model and configuration. 2. Implement the community and hospital service model proposed in this presentation with Huddersfield Royal Infirmary as the site for acute and emergency care and Calderdale Royal Hospital as the site for planned hospital care. 3. Implement the community and hospital service model proposed in this presentation with Calderdale Royal Hospital as the site for acute and emergency care and Huddersfield Royal Infirmary as the site for planned hospital care. 4. Continue with the existing community service model and change emergency hospital care provided locally so that those people needing specialist treatments are transferred to a major emergency centre outside the local area. Huddersfield Royal Infirmary and Calderdale Royal Hospital would offer ‘see and initiate treatment’ services with people needing specialist treatments transferred to specialist centres. 5. Other scenarios which may emerge from the planned engagement activity with staff, public, patients, carers and their representatives.

Commissioners’ Questions – 1 of 2 • Finance Estate requirements, affordability & confidence to achieve savings • Clinical Stds What are they? Risks to current & clinical evidence base • Location Support from YAS, journey times, parking, gritting & community offer • Primary Care Resource, activity shift, engagement • Staff Commitment, & impact on workforce. • Phasing Community before acute services
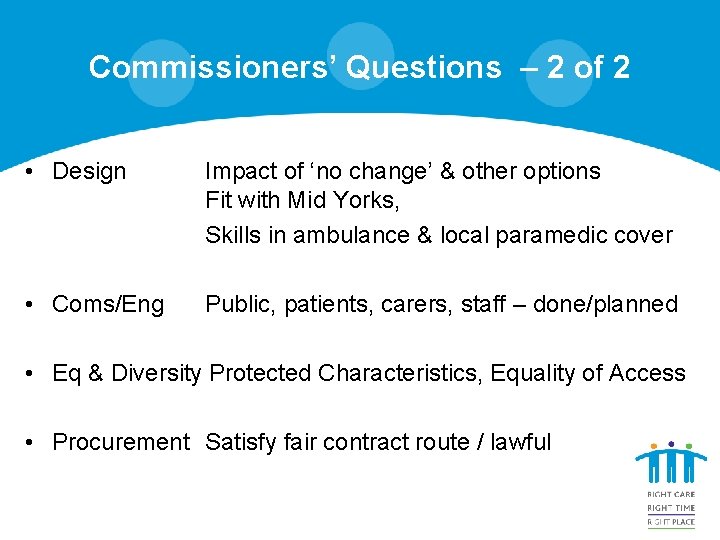
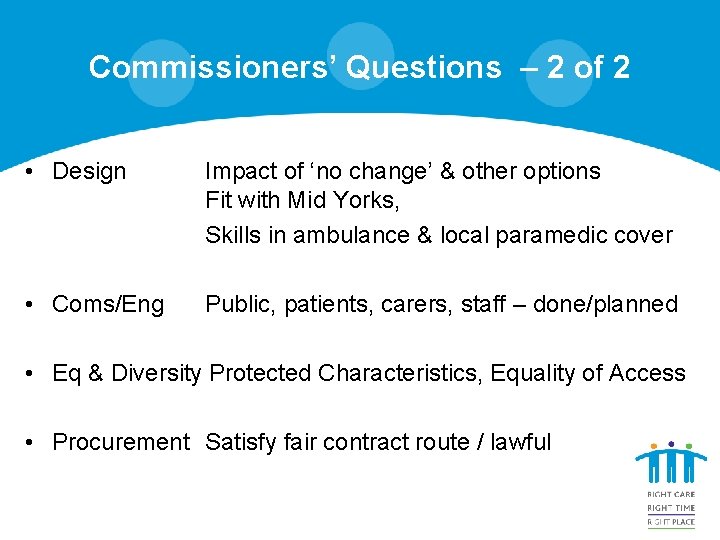
Commissioners’ Questions – 2 of 2 • Design Impact of ‘no change’ & other options Fit with Mid Yorks, Skills in ambulance & local paramedic cover • Coms/Eng Public, patients, carers, staff – done/planned • Eq & Diversity Protected Characteristics, Equality of Access • Procurement Satisfy fair contract route / lawful
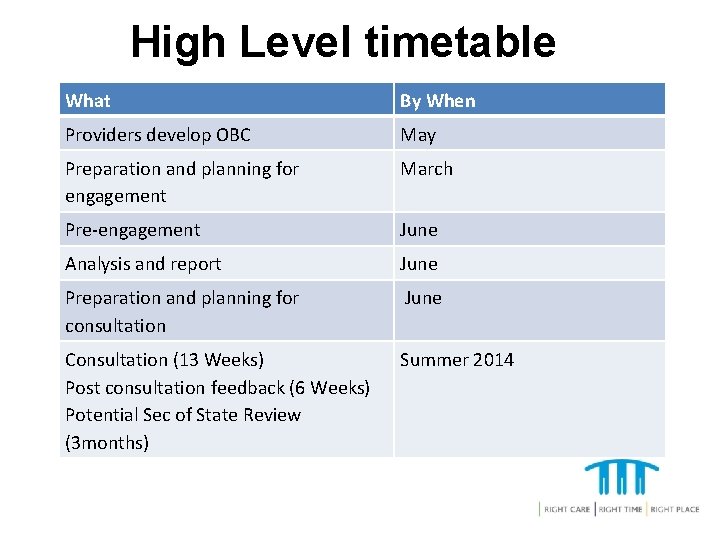
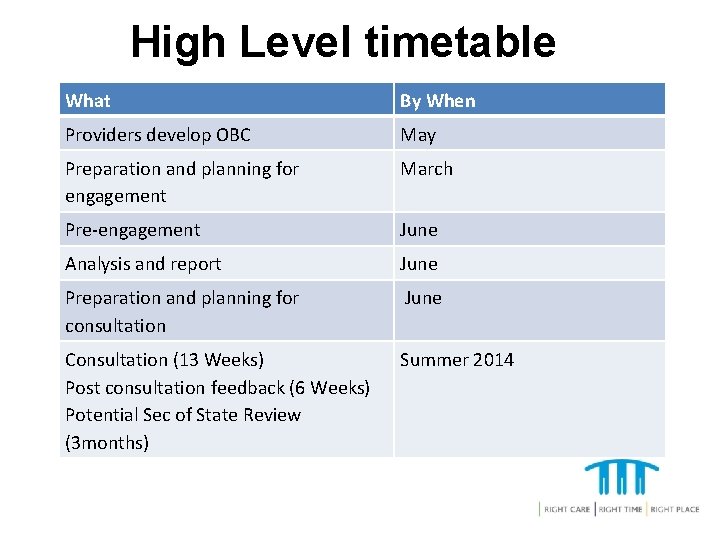
High Level timetable What By When Providers develop OBC May Preparation and planning for engagement March Pre-engagement June Analysis and report June Preparation and planning for consultation June Consultation (13 Weeks) Post consultation feedback (6 Weeks) Potential Sec of State Review (3 months) Summer 2014
Next Steps - Engagement already in place • Local Councillors and MPs • Overview and Scrutiny Committees and Health and Well Being Boards • A dedicated website • A Reference Group – 90 organisations • PALS and complaints services • Healthwatch • Staff and member practices • Existing consumer websites
Next Steps – Engagement what we need to do • • Drop in sessions x 9 Road show activity – 10 central locations Comments cards & boxes for anonymity Media & communications – posters, contact points, social media feeds, media releases • Existing networks

Question Time
 Calderdale framework
Calderdale framework Gm health and social care partnership
Gm health and social care partnership Alton cars mansfield
Alton cars mansfield Architectural design in huddersfield
Architectural design in huddersfield Keyword research huddersfield
Keyword research huddersfield Apa referencing huddersfield
Apa referencing huddersfield Castle hill school huddersfield
Castle hill school huddersfield Handelsbanken huddersfield
Handelsbanken huddersfield Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing Greater columbia accountable community of health
Greater columbia accountable community of health District integrated health and family welfare society
District integrated health and family welfare society Social thinking social influence social relations
Social thinking social influence social relations Social thinking social influence social relations
Social thinking social influence social relations Health systems building blocks
Health systems building blocks Qi integrated health
Qi integrated health Ihias
Ihias Integrated public health information system
Integrated public health information system Integrated primary health care model
Integrated primary health care model Ethical business strategies
Ethical business strategies Integrative social contracts theory maintains that
Integrative social contracts theory maintains that Example of universal principles
Example of universal principles What is appraisal in health and social care
What is appraisal in health and social care Verna and sam coursework
Verna and sam coursework