CALCIUM METABOLISM ITS ROLE IN PROSTHODONTICS Contents Introduction
CALCIUM METABOLISM & ITS ROLE IN PROSTHODONTICS
Contents Introduction Daily requirements Sources Absorption of calcium Factors affecting absorption of calcium Calcium balance Functions of calcium Calcium in cells Calcium in blood Factors regulating blood calcium level -Vitamin D
-Parathyroid hormone -Calcitonin • Conditions arising from irregularities in calcium metabolism Prosthodontic management of diseases Summary Conclusion
Introduction Calcium is a very important mineral in our body. It provides rigidity to our bones, muscle contraction, affects permeability of cells, blood clotting mechanism etc Metabolism of calcium is intimately associated with parathyroid hormone, calcitonin & Vitamin D
Importance of studying calcium metabolism has increased because : (i) In old people, one of the major causes happens to be osteoporosis which can cause fracture of bones (ii) Calcium play vital roles in contraction of heart as well as skeletal muscles and smooth muscles. Physiology, 3 rd Edition. Robert Berne
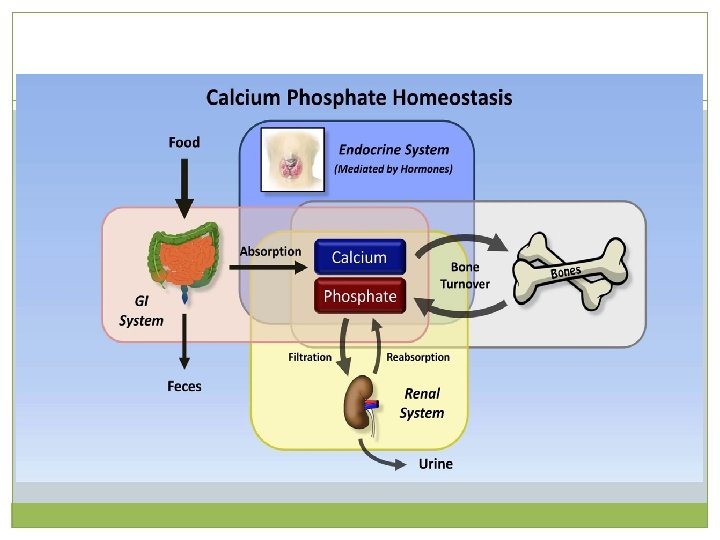
Distribution Total calcium in the human body is about 1 to 1. 5 kg. 99% of it is in bone in the form of calcium phosphate. The small minority of calcium in plasma exists in 3 forms-45% in free ionized form -45% bound to proteins (predominantly albumin) -10% complexed with anions (citrate, sulfate, phosphate) Physiology, 3 rd Edition. Robert Berne
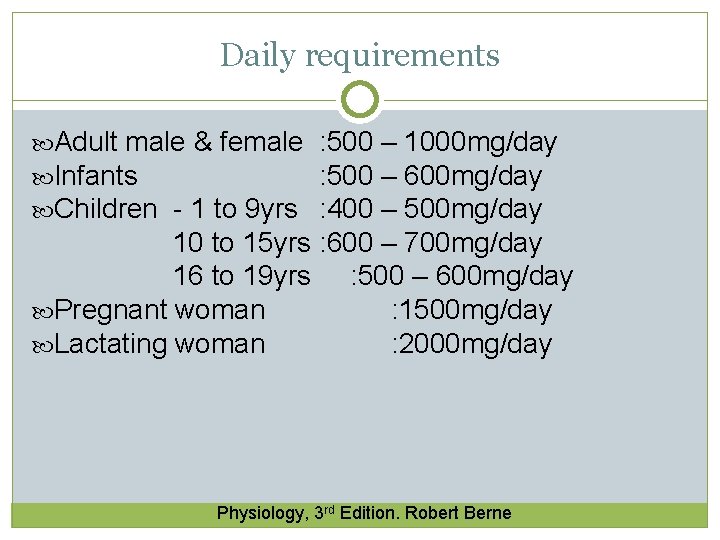
Daily requirements Adult male & female Infants Children - 1 to 9 yrs : 500 – 1000 mg/day : 500 – 600 mg/day : 400 – 500 mg/day 10 to 15 yrs : 600 – 700 mg/day 16 to 19 yrs : 500 – 600 mg/day Pregnant woman : 1500 mg/day Lactating woman : 2000 mg/day Physiology, 3 rd Edition. Robert Berne
Sources Milk and milk products are excellent sources of food calcium. Other sources include hard water, eggs, cheese and green vegetables. Physiology, 3 rd Edition. Robert Berne
Functions of calcium Activation of enzymes: -Calmodulin is a calcium binding regulatory protein. Calmodulin can bind with 4 calcium ions. -Calcium binding leads to activation of enzymes. Calmodulin is part of various regulatory kinases. Review of Medical Physiology. 17 th Edition. William Ganong
-Calmodulin dependent enzymes are: Adenyl cyclase Ca++ dependent protein kinases Ca++ Mg+ ATPase Glycogen synthase Myosin kinase Phospholipase C Pyruvate dehydrogenase Review of Medical Physiology. 17 th Edition. William Ganong
Muscles: -Calcium mediates excitation & contraction of muscle fibers. Upon getting the neural signal, calcium is released from sarcoplasmic reticulum -Calcium activates ATPase, increases reaction of actin & myosin and facilitates excitationcontraction coupling -The trigger of muscle contraction is the interaction of calcium with Troponin C Review of Medical Physiology. 17 th Edition. William Ganong
Nerves: Calcium is necessary for transmission of nerve impulses from pre-synaptic to post-synaptic region Secretion of hormones: Calcium mediates secretion of insulin, parathroid hormones etc from Myocardium: Ca++ prolongs systole. the cells Review of Medical Physiology. 17 th Edition. William Ganong
Coagulation: Calcium is known as Factor IV in blood coagulation cascade. Prothrombin contains gamma-carboxy glutamate residues which are chelated by Ca++ during the thrombin formation Bone & Teeth: The bulk quantity is used for bone & teeth formation. Bones also act as reservoir of calcium in the body. Osteoblasts induce bone deposition & osteoclasts induce bone demineralization. Textbook of biochemisry for dental students, D M Vasudevan
Absorption of calcium Absorption is taking place from the first & second part of the duodenum Absorption requires a carrier protein, helped by calcium-dependent ATPase Physiology, 3 rd Edition. Robert Berne
Site of Absorption of calcium occurs mainly from upper jejunum and duodenum. The absorption is by : -A carrier mediated mechanism: The carrier molecule (calbindin) resides in the "brush border" of the jejunal mucosa. A derivative of Vitamin D 1, 25 DHCC (Calcitriol) facilitates this carrier mediated transport. Physiology, 3 rd Edition. Robert Berne
-Passive Diffusion : Small amount of calcium is also absorbed via passive diffusion i. e. molecules move according to a chemical gradient i. e. from a solution of higher concentration towards a solution of lower concentration. Physiology, 3 rd Edition. Robert Berne
Form of Absorption Soluble inorganic forms are much better absorbed Thus the organic calcium of food is converted into inorganic form before it can be absorbed Insoluble calcium compounds are never absorbed. Therefore presence of phytic acid in cereals produces formation of Ca phytate which is insoluble Calcium phosphates are not absorbed. Physiology, 3 rd Edition. Robert Berne
Factors affecting absorption of calcium Vitamin D: Calcitriol induces the synthesis of the carrier protein (Calbindin) in the intestinal epithelial cells, & so facilitates the absorption of calcium Parathyroid hormone: It increases calcium transport from the intestinal cells Acidity: it favors calcium absorption Physiology, 3 rd Edition. Robert Berne
Phytic acid: It is present in cereals. It reduces uptake of calcium. Cooking reduces phytate content Oxalates: They are present in leafy vegetables, which cause formation of insoluble calcium oxalates; so absorption is reduced Phosphate: High phosphate content will cause precipitation as calcium phosphate Physiology, 3 rd Edition. Robert Berne
Calcium balance Dietary absorption is the only means of obtaining calcium. There are several mechanisms whereby calcium is lost from the body, including renal clearance, excretion of unabsorbed calcium in the faeces, & dermal losses. If the amount of calcium absorbed is greater than the amount lost, excess calcium is deposited in the skeleton. This is referred to as positive calcium balance. Calcium metabolism and osteoporotic ridge resorption: a protein connection, jpd, 1987
If losses exceed absorption, calcium is mobilized from the skeleton to optimally maintain the narrow limits of extracellular fluid calcium, & is referred to as negative calcium balance. A negative calcium balance sustained over a period of time will lead to osteoporosis
Calcium in cells Calcium is mainly extracellular. The cell membrane is generally impermeable to calcium ions. Calcium influx into the cell is by Na+/Ca++ exchange mechanism. The second mechanism is Ca++- H+ - ATPase dependent pump, which expels calcium in exchange for H+ Review of Medical Physiology. 17 th Edition. William Ganong
Calcium in Blood Normal blood level: 9 -11 mg/dl Ionized calcium: about 5 mg/dl of calcium is in ionized form & is metabolically active. (About 4 mg/dl of calcium is bound to proteins in blood & is nondiffusable) Review of Medical Physiology. 17 th Edition. William Ganong
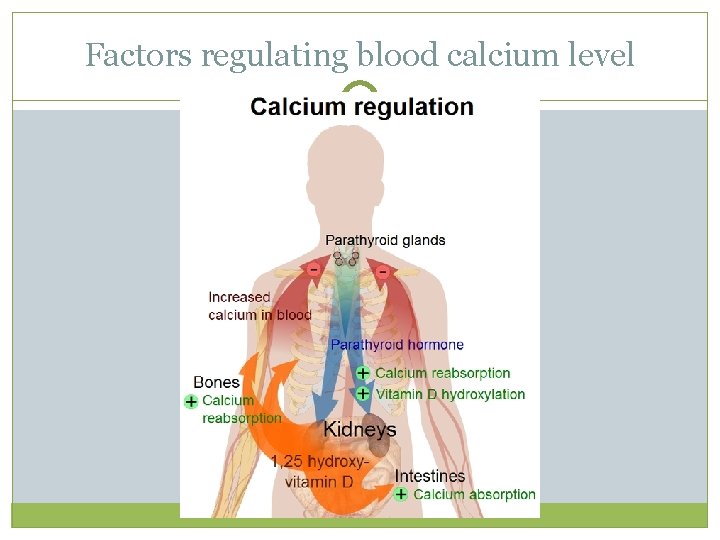
Factors regulating blood calcium level
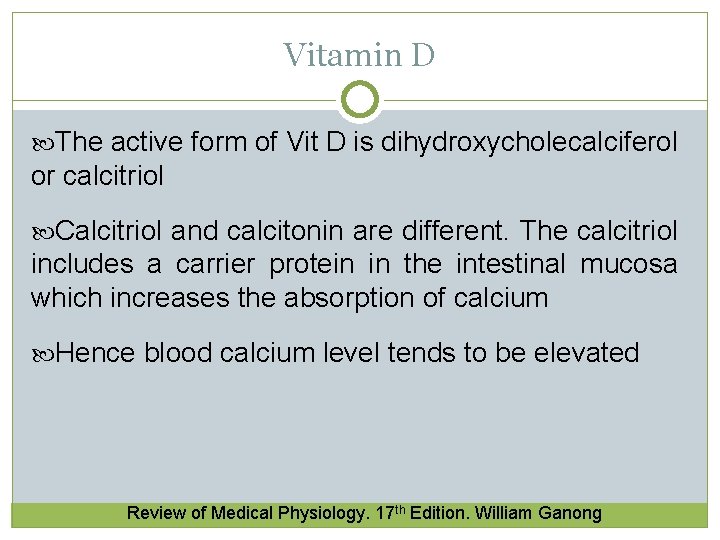
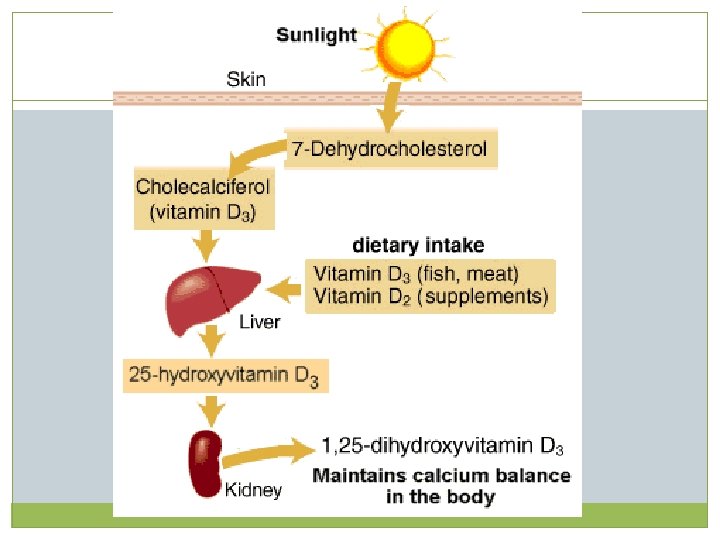
Vitamin D The active form of Vit D is dihydroxycholecalciferol or calcitriol Calcitriol and calcitonin are different. The calcitriol includes a carrier protein in the intestinal mucosa which increases the absorption of calcium Hence blood calcium level tends to be elevated Review of Medical Physiology. 17 th Edition. William Ganong
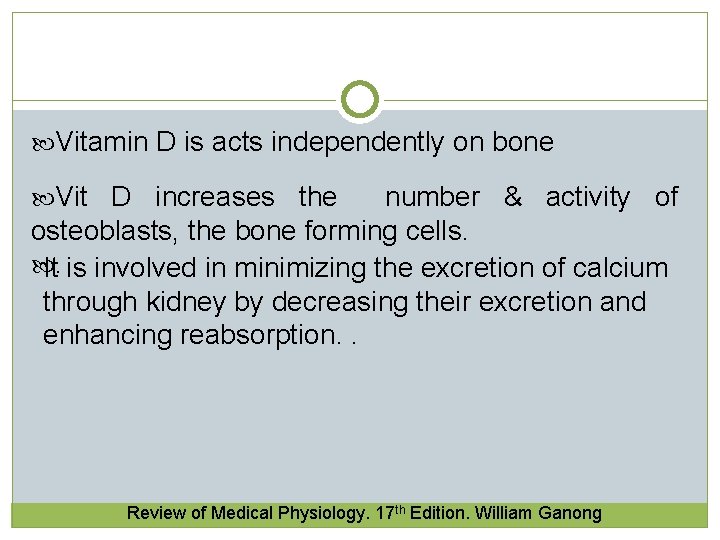
Vitamin D is acts independently on bone Vit D increases the number & activity of osteoblasts, the bone forming cells. It is involved in minimizing the excretion of calcium . through kidney by decreasing their excretion and enhancing reabsorption. . Review of Medical Physiology. 17 th Edition. William Ganong
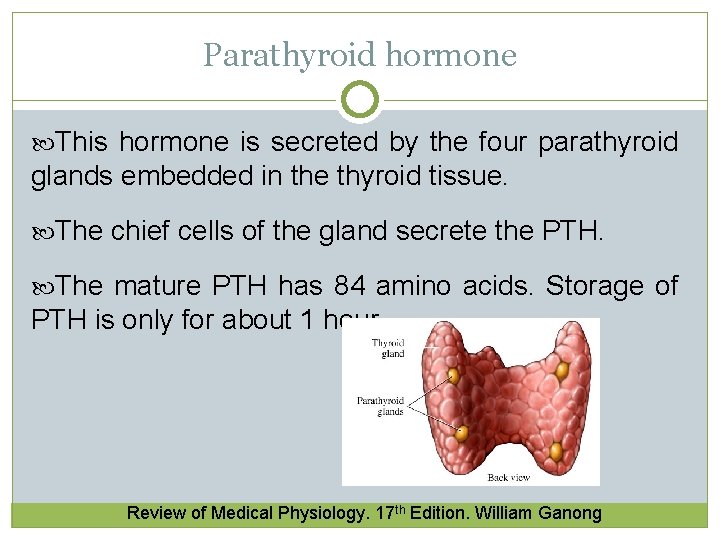
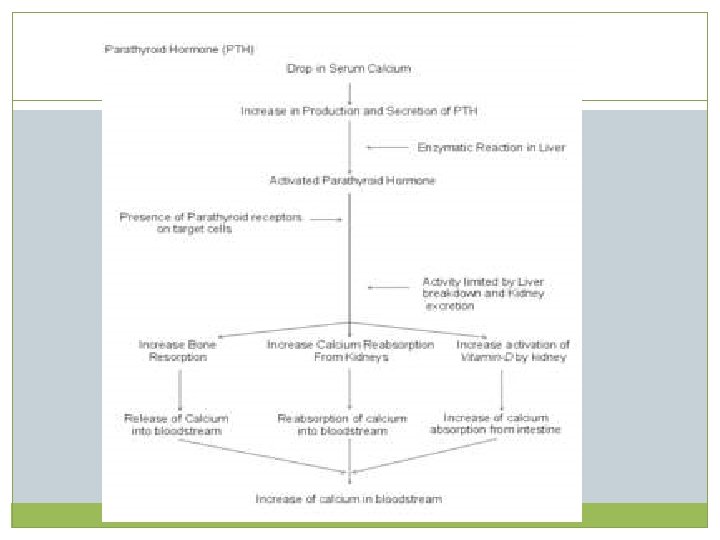
Parathyroid hormone This hormone is secreted by the four parathyroid glands embedded in the thyroid tissue. The chief cells of the gland secrete the PTH. The mature PTH has 84 amino acids. Storage of PTH is only for about 1 hour. Review of Medical Physiology. 17 th Edition. William Ganong
Mechanism of action of PTH Control of release of the hormone is by negative feedback by the ionized calcium in serum PTH & Bones: -In the bone, PTH causes demineralization or decalcification. It induces pyrophosphatase in the osteoclasts -The number of osteoclasts are also increased Review of Medical Physiology. 17 th Edition. William Ganong
-Osteoclasts release lactate into surrounding medium which solubilizes calcium -PTH also causes secretion of collagenase from osteoclasts. -This causes loss of matrix and bone resorption. Review of Medical Physiology. 17 th Edition. William Ganong
PTH and Kidney: -PTH causes decreased renal excretion of calcium and increased excretion of phosphates -The action is mainly through increase in reabsorption of calcium from kidney tubules -it also targets the 1α hydroxylase, whose function is to activate calcitriol. Review of Medical Physiology. 17 th Edition. William Ganong
Calcitonin It is secreted by the thyroid parafollicular or clear cells. Calcitonin is a single chain polypeptide. It contains about 32 amino acids Calcitonin secretion is stimulated by serum calcium Calcitonin level is increased in medullary carcinoma of thyroid and therefore is a tumour marker Review of Medical Physiology. 17 th Edition. William Ganong
Calcitonin decreases serum calcium level. It inhibits resorption of bone It decreases the activity of osteoclasts and increases that of osteoblasts Calcitonin and PTH are directly antagonistic. The PTH and calcitonin together promote the bone growth and remodelling Review of Medical Physiology. 17 th Edition. William Ganong
Calcitonin, Calcitriol and PTH When blood calcium tends to lower, PTH secretion is stimulated and calcitonin is inhibited; bone demineralization leads to entry of more calcium into blood. When blood calcium is increased, PTH is inhibited and calcitonin is secreted, causing more entry of calcium into bone Review of Medical Physiology. 17 th Edition. William Ganong

Conditions arising from irregularities in calcium metabolism
Hypercalcemia The term denotes that the blood calcium level is more than 12 mg/dl. The major cause is hyperparathyroidism Causes are- primary and secondary hyperparathyroidism, cancer, vitamin D disorders, kidney failure, milk alkali syndrome. There is osteoporosis and bone resorption. Pathological fracture of bone may result. Review of Medical Physiology. 17 th Edition. William Ganong
Signs and symtoms are- - stones (renal or biliary) -bones(bone pain) -groans(abdominal pain, nausea, vomiting) -thrones (poluria) -psychiatric overtones(depression , anxiety) Review of Medical Physiology. 17 th Edition. William Ganong
Hypocalcemia & Tetany When serum calcium level is less than 8. 8 mg/dl, it is hypocalcemia If serum calcium level is less than 8. 5 mg/dl, there will be mild tremors If it is lower than 7. 5 mg/dl, tetany, a life- threatening condition will result Tetany may be due to accidental removal of parathyroid glands Review of Medical Physiology. 17 th Edition. William Ganong
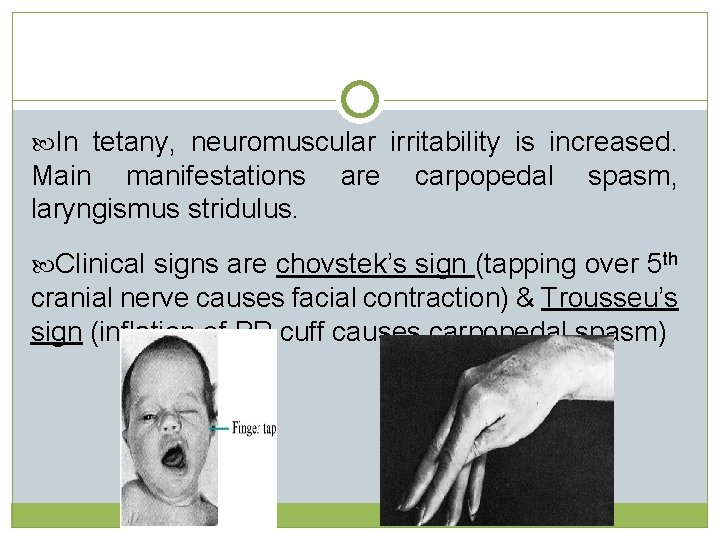
In tetany, neuromuscular irritability is increased. Main manifestations are carpopedal spasm, laryngismus stridulus. Clinical signs are chovstek’s sign (tapping over 5 th cranial nerve causes facial contraction) & Trousseu’s sign (inflation of BP cuff causes carpopedal spasm)
Oral manifestations -The two most frequent dental abnormalities are enamel hypoplasia (enamel is thin), delayed eruption, and there may be multiple unerupted teeth.
Treatment of hypocalcemia -The main treatments available for these patients is Vitamin D or its analogs, calcium salts and drugs that increase renal tubular reabsorption of calcium, to obtain adequate, normal serum calcium levels.
Dental management - Dental management will be the prevention of caries with periodic check-up, advice regarding diet and oral hygiene instructions. -As pulp chamber are large, caries easily involve the pulp causing pulpitis, requiring endodontic treatment. -Delayed eruption and hypodontia cause malposition and has to be treated by orthodontics.
Vitamin D deficiency Rickets l. Occurs in children between 6 months to 2 years of age. l. Affects long bones. l. Lack of calcium causes failure of mineralization resulting into formation of cartilagenous form of bone. Review of Medical Physiology. 17 th Edition. William Ganong
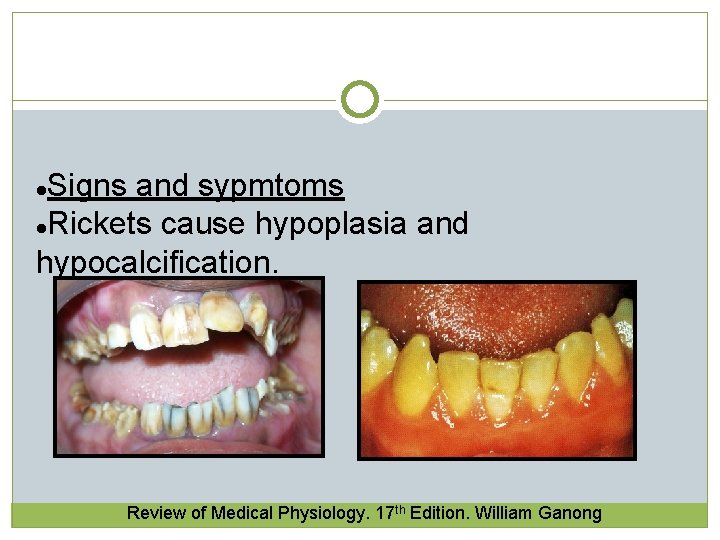
Signs and sypmtoms l. Rickets cause hypoplasia and hypocalcification. l Review of Medical Physiology. 17 th Edition. William Ganong
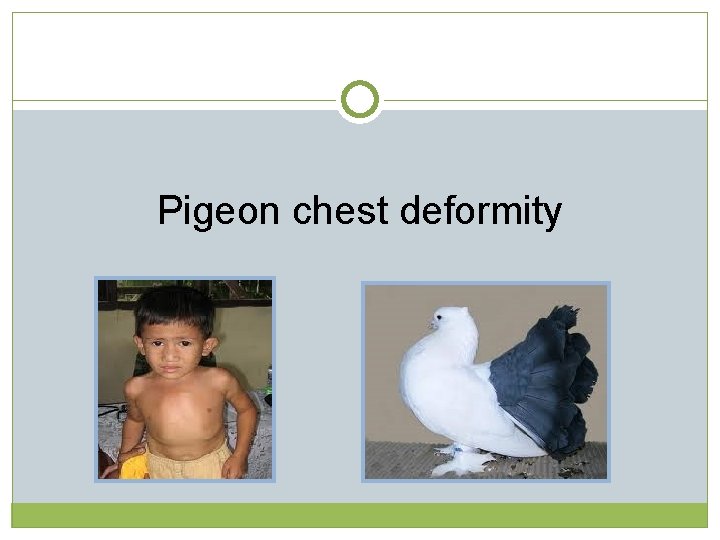
Pigeon chest deformity
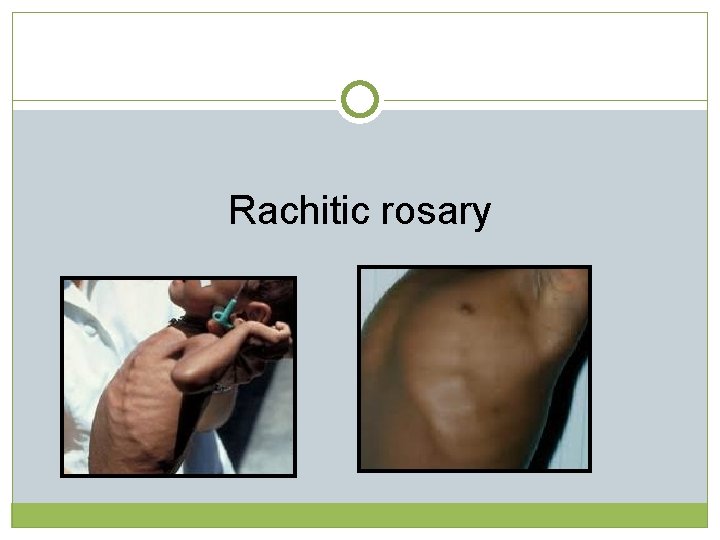
Rachitic rosary
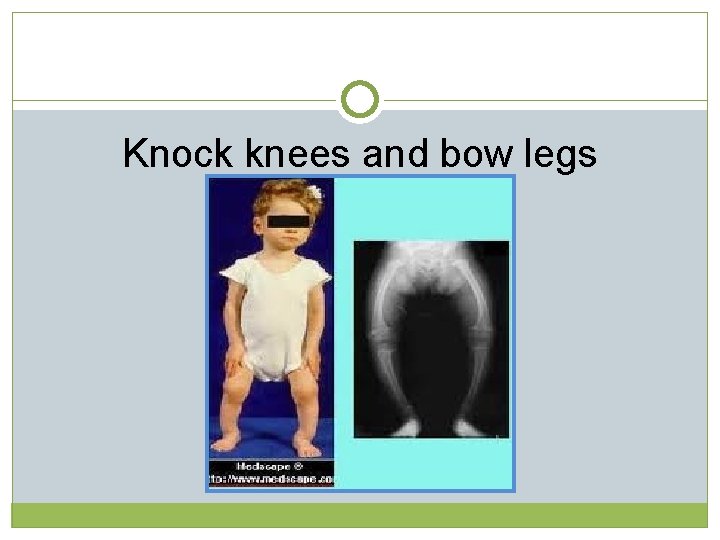
Knock knees and bow legs
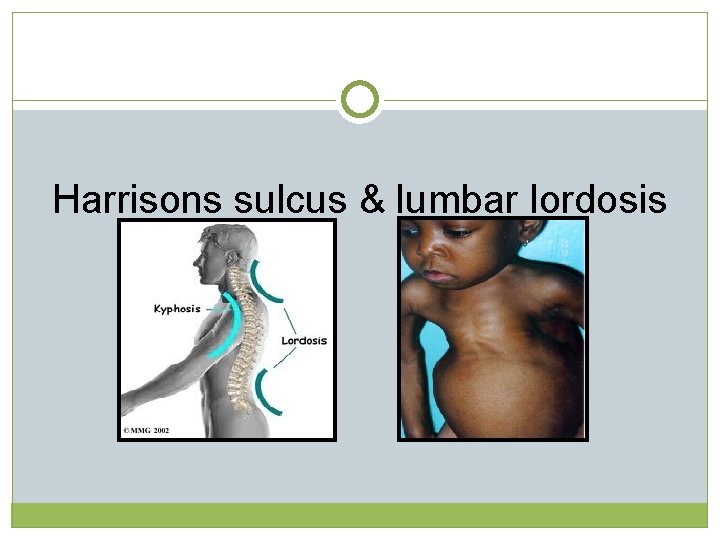
Harrisons sulcus & lumbar lordosis
Dental Treatment -Common treatments performed on patients with rickets include full mouth pulpectomies, placement of posterior stainless steel crowns, and anterior composite resin restorations.
Osteomalacia is softening of the bones, caused by not having enough vitamin D or by problems with the metabolism (breakdown and use) of this vitamin. l. These softer bones have a normal amount of collagen that gives the bones its structure, but they are lacking in calcium l Review of Medical Physiology. 17 th Edition. William Ganong
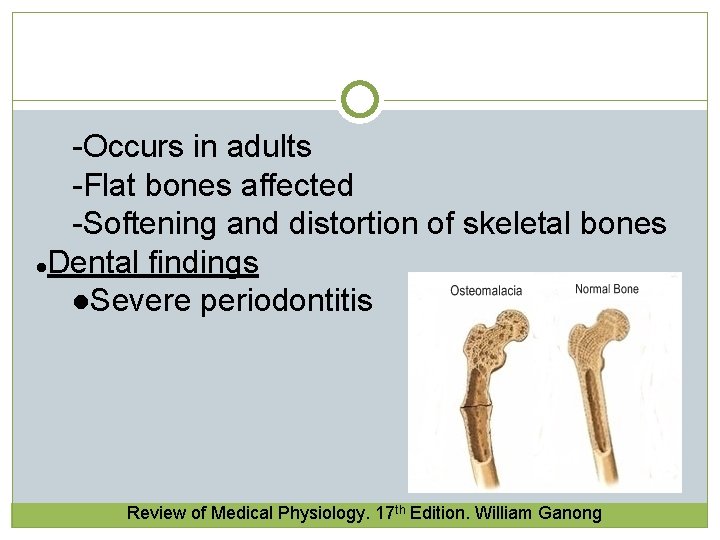
-Occurs in adults -Flat bones affected -Softening and distortion of skeletal bones l. Dental findings l. Severe periodontitis Review of Medical Physiology. 17 th Edition. William Ganong
Hyperparathyroidism They are of two types- -primary and secondary Primary hyperparathyroidism. Usually caused by a tumor or hyperplasia of the gland that produces an increase in PTH secretion resulting in hypercalcemia and hypophosphatemia. - Oral manifestations of parathyroid disorders and its dental management, journal of dental and allied sciences, 2014
Secondary hyperparathyroidism. When the parathyroid glands are stimulated to produce increased amounts of hormones to correct abnormally low serum calcium levels in different physiologic or pathologic conditions like renal failure, intestinal malabsorption syndrome, decrease of Vitamin D production, thus resulting in parathyroid hyperplasia. - Oral manifestations of parathyroid disorders and its dental management, journal of dental and allied sciences, 2014
Metastatic calcifications seen in subcutaneous soft tissues, sclera, dura and region around joints. l l Brown tumor. l Affect mandible, clavicles, ribs and pelvis. Osteitis fibrosa cystica- develops from central degeneration and fibrosis of long standing brown tumor. l Review of Medical Physiology. 17 th Edition. William Ganong
Signs and symptoms -subperiosteal resorption of the phalanges of the index and middle fingers -musculoskeletal problems (weakness, back pain, muscle soreness), gastrointestinal complaints, e. g. , vomiting, nausea, constipation, loss of appetite. -bone disease Review of Medical Physiology. 17 th Edition. William Ganong
Oral manifestations - brown tumor, loss of bone density, mobile teeth, drifting of teeth, complaint of vague jaw bone pain, sensitive teeth in mastication and percussion, soft tissue calcifications and dental abnormalities such as development defects, alterations in dental eruption Oral manifestations of parathyroid disorders and its dental management, journal of dental and allied sciences, 2014
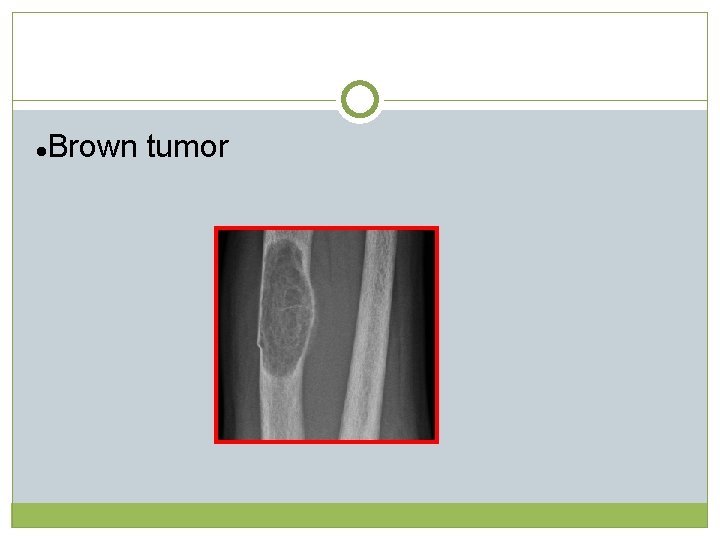
l Brown tumor
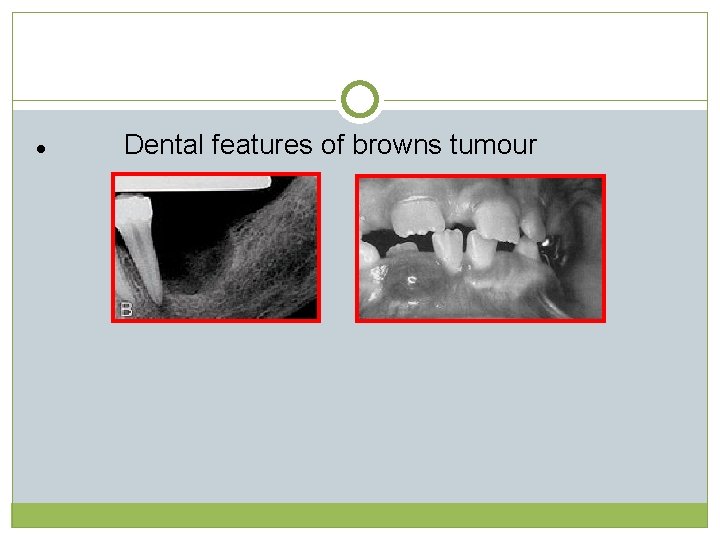
Dental features of browns tumour l
l Loss of lamina dura
Dental management -The clinical management of these patients does not require any special consideration. We should know that there is a higher risk of bone fracture, so we must take precaution in surgical treatments Oral manifestations of parathyroid disorders and its dental management, journal of dental and allied sciences, 2014
Osteoporosis After the age of 40 -45, calcium absorption is reduced and calcium excretion is increased, so, there is a net negative balance for calcium This is reflected in demineralization After the age of 60, osteoporosis is seen Reduced bone strength and an increased risk of fractures Calcium metabolism and osteoporotic ridge resorption, JPD, 1987
Osteoporosis may be defined simply as a condition of insufficient bone This deficiency undermines skeletal strength, resulting in fractures that occur with minimal stress in the spine, distal radius & ulna & in the femoral neck A complete array of etiologic factors in primary osteoporosis have been identified Calcium metabolism and osteoporotic ridge resorption, JPD, 1987
Those include Decreased estrogen levels in postmenopausal women Inactivity Alcohol abuse High phosphate diets Low calcium diets Vit D deficiency Corticosteroids Smoking Caffeine intake Dietary protein imbalance Stress Calcium metabolism and osteoporotic ridge resorption, JPD, 1987
Treatment – -Estrogen therapy remains controversial because of uncertainty about long-term benefits -Vit D is another widely used therapeutic adjunct because of its important role in bone metabolism -The most controversial experimental therapy is the use of fluoride.
Fluoridic bone displays increased crystallinity, which may actually result in decreased elasticity predisposing to fracture Increasing calcium intake by means of dairy foods & supplementation is the most practiced method in the prevention & management of osteoporosis to optimize calcium balance Calcium metabolism and osteoporotic ridge resorption, JPD, 1987
Increased intake of proteins in the diet has a calciuretic excretion) effect (increased urinary calcium By the time osteoporosis is generally diagnosed, 50 -75% of the original bone material has been lost from the skeleton Therapeutic & preventive measures, such as increased calcium supplementation with a watch on dietary protein intake are helpful Calcium metabolism and osteoporotic ridge resorption, JPD, 1987
Recommendations relevant to the prevention & management of osteoporosis are: i. Avoid a high protein diet & maintain daily protein intake levels of 50 -60 grams to promote a positive calcium balance ii. Maintain the RDA of 800 mg of calcium for men & nonpregnant women Calcium metabolism and osteoporotic ridge resorption, JPD, 1987
iii. Participate in regular exercise appropriate to age & health status programs iv. Avoid risk factors related to osteoporosis such as smoking, excessive alcohol, & the generous use of caffeine- containing beverages Calcium metabolism and osteoporotic ridge resorption, JPD, 1987
Calcium and vitamin D supplements Office of dietary supplements recommend that no more than 600 mg of calcium should be taken at a time because calcium absorbed decreases with increase in amount of calcium in the supplements. They cause bloating and constipation in some people and so taking them with food helps nullify these side effects. Different forms of supplements are-calcium carbonate, calcium citrate and calcium lactate
For adults 5 micrograms of vitamin D is the recommended dietary allowance that may prevent osteomalacia in the absence of sunlight. Hazards and toxicity excessive consumption leads to milk alkali syndrome with symptoms ranging from hypercalcemia to renal failure.
Prosthodontic management of the diseases
-While fabricating the removable dentures the main area of focus should be on reduction of the forces on residual ridge. -Mucostatic or open mouth impression techniques, selective pressure impression technique, should be employed to reduce mechanical forces while impression making. -Semi anatomic or non anatomic teeth with narrow buccolingual width should be selected. Osteoporosis: its prosthodontic considerations –a review, JCDR, 2015
Optimal use of soft liners, extended tissue intervals by keeping the dentures out of mouth for 10 hours a day can be advised. While fabricating fixed partial denture in periodontally compromised abutments it may accelerate the bone loss in osteoporotic patients. So, the fabrication of FPD should follow treatment of osteoporosis rather than preceding it. Osteoporosis: its prosthodontic considerations –a review, JCDR, 2015
Impression Techniques for Resorbed Ridges The different techniques available are: 1. The Functional Impression Technique 2. The Neutral Zone Technique Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
Functional Impression Technique Functional impression can be used very effectively to create stability in cases exhibiting extreme resorption Though retention is usually poor in such cases yet the clinician can set out to achieve stability in these patients The prosthesis should remain stable within the oral cavity and not move at the slightest movement of the tongue Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
A functional impression can be made after doing the border moulding using a stable custom tray Temporary soft liners and tissue conditioners can be used as functional impression materials as they exhibit the property of delayed setting and a continuous over a longer period of time thereby recording all possible movements of the mandibular musculature. Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
The extensions of the custom tray should be verified accurately and border moulding done After completion of the procedure, instead of using the regular impression material for making definitive impressions, a functional impression material can be used The material is mixed and placed on the impression surface of the custom tray Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
The material is initially moulded using the regular movements of secondary impression making technique Once the material attains an initial set, the patient is instructed to read a news paper aloud, drink water 3 -4 times and swallow saliva at regular intervals and other daily chores The functional impression material stays within the oral cavity for a period of 45 -60 min. All oral activities of the patient are encouraged Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci
Once the material has achieved a final set, the tray is removed and the impression is poured The cast obtained is used as a master cast for fabrication of prosthesis Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
Neutral Zone Impression Technique Though all of us realize the importance of neutral zone yet no one tries to use it for increasing the stability in complete denture prosthesis If done correctly, the neutral zone can increase the stability and retention to a great extent Recording the neutral zone is itself quite simple Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
After taking jaw relations, the maxillary and mandibular cast is mounted using a face bow transfer Thereafter, the mandibular wax rim is cut off and wire loops in the shape of letter “v” are made on the lower record base up to the height of the mandibular wax rim Now the maxillary record base is placed in the oral cavity Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
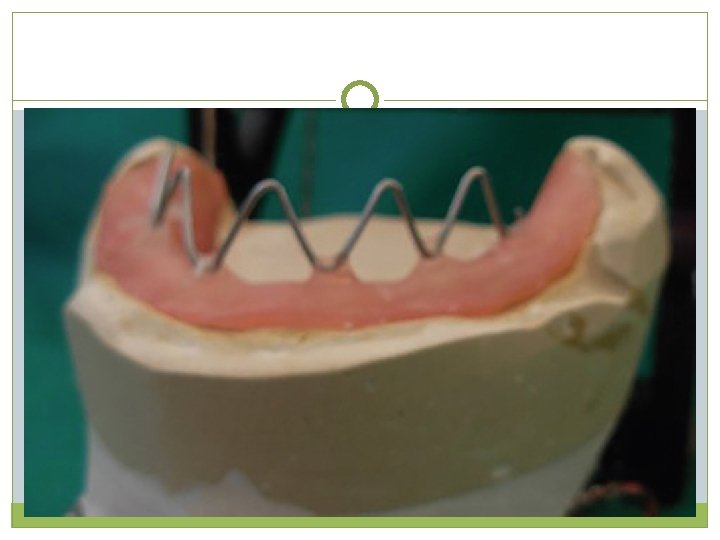
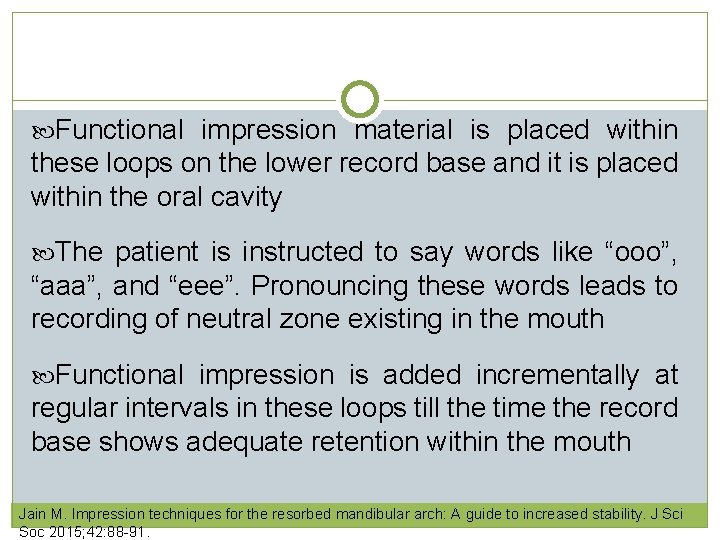
Functional impression material is placed within these loops on the lower record base and it is placed within the oral cavity The patient is instructed to say words like “ooo”, “aaa”, and “eee”. Pronouncing these words leads to recording of neutral zone existing in the mouth Functional impression is added incrementally at regular intervals in these loops till the time the record base shows adequate retention within the mouth Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
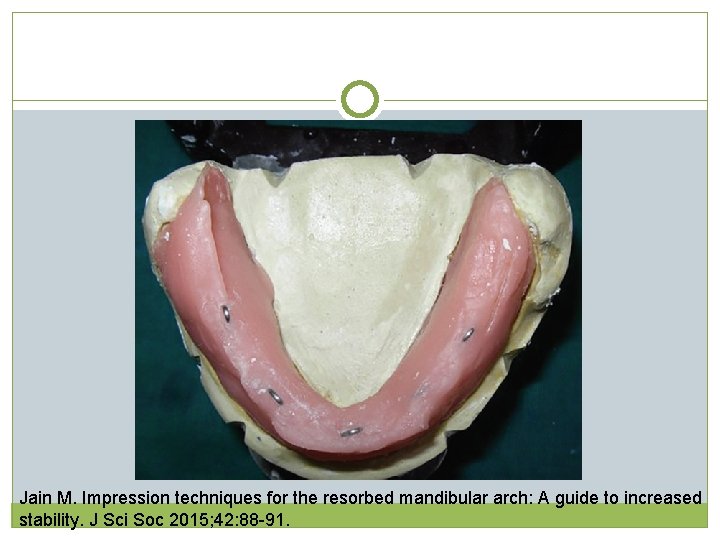
Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
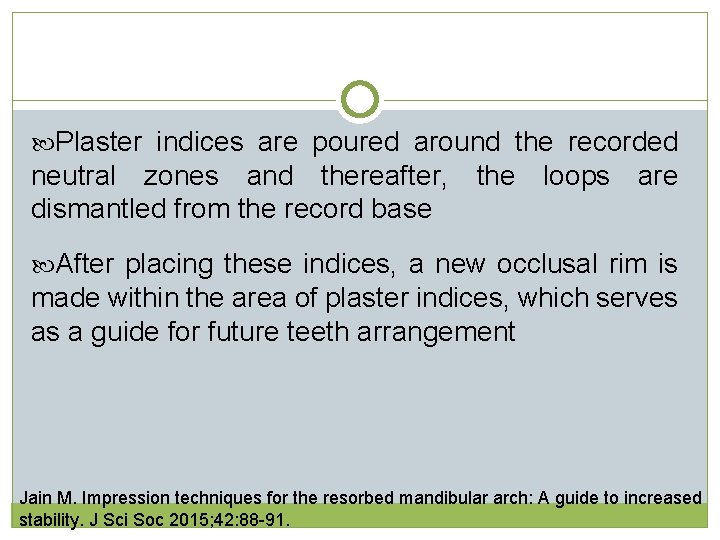
Plaster indices are poured around the recorded neutral zones and thereafter, the loops are dismantled from the record base After placing these indices, a new occlusal rim is made within the area of plaster indices, which serves as a guide for future teeth arrangement Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
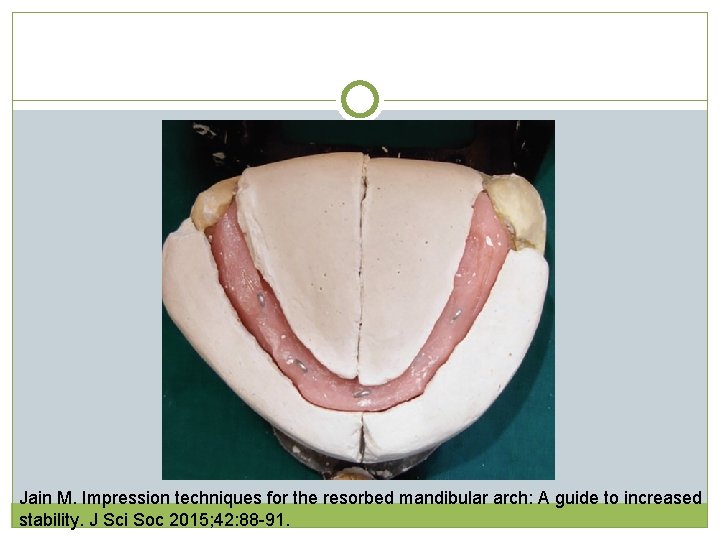
Jain M. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91.
Conclusion Disturbances in calcium intake and excretion result in deranged metabolism accounting for abnormal serum levels. As a result of the essential role played by these minerals in intra and extracellular metabolism is disturbed, the clinical manifestations of related disease states are extensive. Thus, an understanding of the basic mechanism of calcium metabolism and pathophysiology of various related disorders is helpful in guiding therapeutic decisions.
References Physiology, 3 rd Edition. Robert Berne Review of Medical Physiology. 17 th Edition. William Ganong Textbook of biochemistry for dental students, D M vasudevan. Impression techniques for the resorbed mandibular arch: A guide to increased stability. J Sci Soc 2015; 42: 88 -91
Osteoporosis: its prosthodontic considerations –a review, JCDR, 2015 Calcium metabolism and osteoporotic ridge resorption, JPD, 1987
Calcium and dental implants • The alterations in bone metabolism associated to osteoporosis can also impair bone healing around dental implants and affect their osseointegration. • Some animal studies have confirmed a reduced bone-to-implant contact, reduced mechanical properties, and a delay in bone healing in osteoporotic-like conditions. • It is not an absolute contraindication for implants. The effect of osteoporosis on dental treatments. AUGUST 12, 2015 BY IMPLANT PRACTICE US
• Dental implants can be successfully placed in osteoporotic patients, but clinicians should follow a few recommendations for a more predictable outcome. • Clinicians should assess and try to control risk factors that can affect bone metabolism and bone density such as -deficiencies of vitamin D and calcium, smoking, alcohol abuse, the presence of systemic diseases (such as diabetes mellitus). The effect of osteoporosis on dental treatments. AUGUST 12, 2015 BY IMPLANT PRACTICE US
• The clinician should take into consideration under preparation of the site longer healing periods before siting the prosthesis and a careful implant/bone loading distribution. • Jaw bone mineral density can be assessed using computed tomography
• The use of phosphate ceramic-coated implants, hydroxyapatite-coated implants, bisphonate-coated implants, and hydrophilic titanium surfaces promote better bone healing when the host bone is osteoporotic, but this data is yet to be thoroughly investigated.
Effect of osteoporosis medications on the success/survival of dental implants • Several medications have been used to treat osteoporotic patients. Antiresorptive treatments slow bone loss and bone anabolic agents stimulate bone formation. • Bisphonates, and in particular alendronate, are antiresorptive medications for osteoporosis and represent the gold standard in fracture prophylaxis. • They can be administered either orally or intravenously. The effect of osteoporosis on dental treatments AUGUST 12, 2015 BY IMPLANT PRACTICE US
• These medications inhibit the formation and activation of osteoclasts and induce their apoptosis, thus reducing bone turnover. • They may potentially reduce the regenerative capacity of bone around dental implants, • The slower osseous remodeling allows more time for secondary mineralization, so that there is an increase in bone density and stiffness,
together with an increase in microdamage of bone • Intravenous bisphonate treatment in cancer patients is an absolute contraindication for implant placement. • Osteoporosis treatment with oral bisphonates is not considered an absolute contraindication for dental implants • Vitamin D has no effect on osseointegration of implants in diabetic rats
Complications caused by bisphonates • One of the most serious complications that have been related to the use of bisphonates is the development of osteonecrosis of the jaws. • To reduce the incidence of osteonecrosis before an implant surgery, risk factors that increase the possibility of developing serious complications should be identified such as -smoking
-oral mucosal irritation associated to denture wearing -periodontitis -treatment with corticosteroids -diabetes mellitus • Furthermore, it is important to reduce the surgical trauma as much as possible, to use abundant irrigation when drilling the bone, and to suture in order to promote primary intention closure of the wound
A study was conducted on 5 edentulous patients. Branemark Ti. Unite 3. 75 mm diameter implants were used. Each patient recieved 6 control implants and 1 bisphonate coated implant. In all the 5 patients, bisphonate implants had the Bisphonate-coated titanium screws as dental implants in patients. Per highest ISQ value. Aspenberg , Jahanmehr Abtahi, Pentti Tengvall.
Calcium phosphate coating on implants • Metal implants have been coated with layers of calcium phosphates mainly composed of hydroxyapatite. Following implantation, the release of calcium phosphate into the peri-implant region increases the saturation of body fluids and precipitates a biological apatite onto the surface of the implant. Surface treatments of titanium dental implants for rapid osseointegration L. Le Guéhennec et al Dent mat , july 2007
• This layer of biological apatite might contain endogenous proteins and serve as a matrix for osteogenic cell attachment and growth. • The bone healing process around the implant is therefore enhanced by this biological apatite layer • The biological fixation of titanium implants to bone tissue is faster with a calcium phosphate coating than without. Surface treatments of titanium dental implants for rapid osseointegration L. Le Guéhennec et al Dent mat , july 2007
Conclusion • The available evidence on the risks associated with the treatment of osteoporotic patients is poor and needs further investigation. • Both the pathogenesis and the medications of osteoporosis can interfere with the success of dental treatments involving osseous healing of the jawbones. • There is no absolute contraindication in placing dental implants in osteoporotic patients, but a
longer osseointegration healing period should be taken into consideration. A correct patient selection is also crucial. • The association between BP use and osteonecrosis of the jaw should not be overlooked. • Attention should be paid to ensure an atraumatic surgical technique, an adequate postoperative control, and an adequate occlusal adjustment of the prosthesis.
- Slides: 106