Calcium homeostasis and pathologies What are the physiological
- Slides: 16
Calcium homeostasis and pathologies
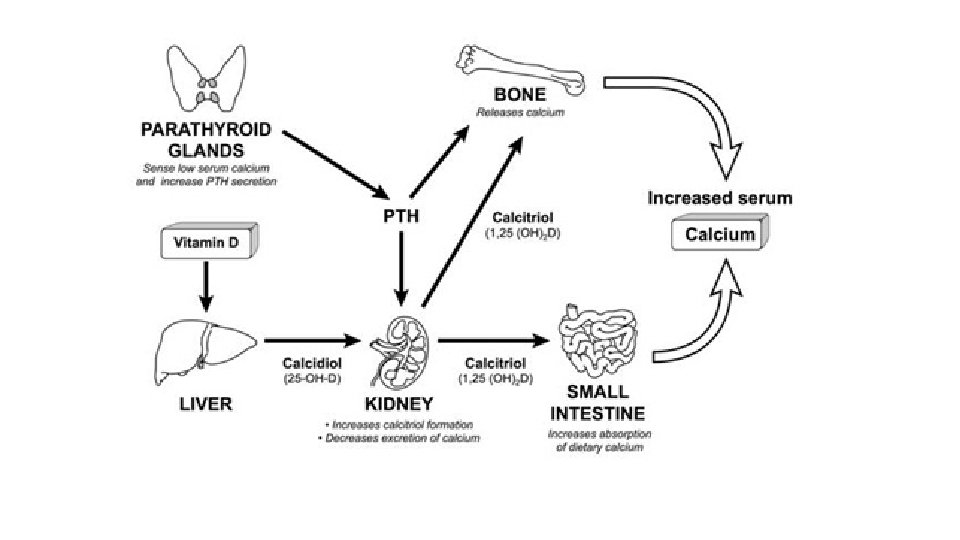
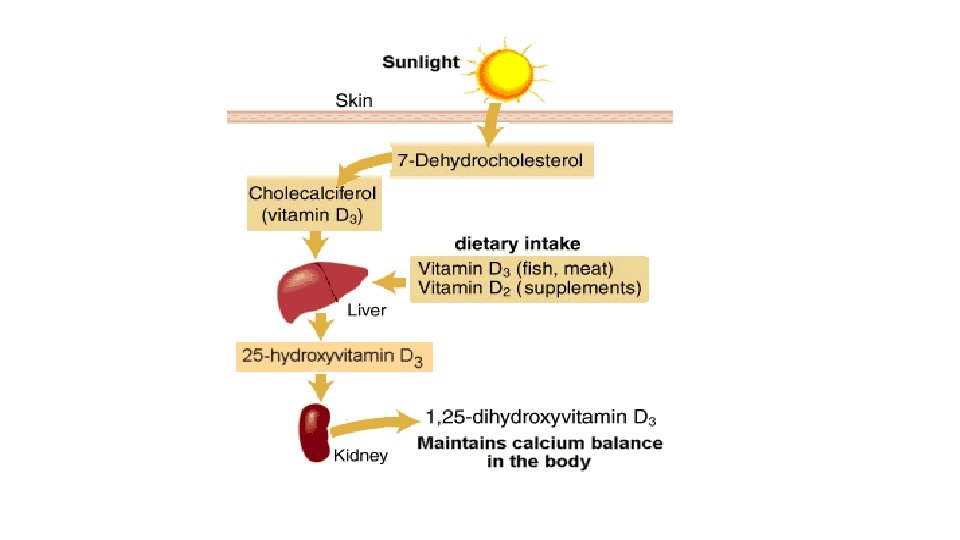
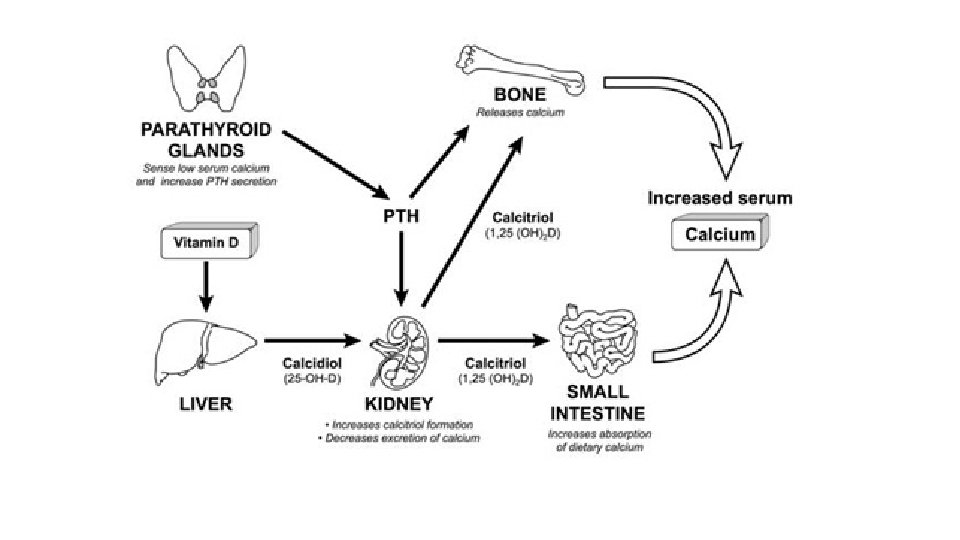
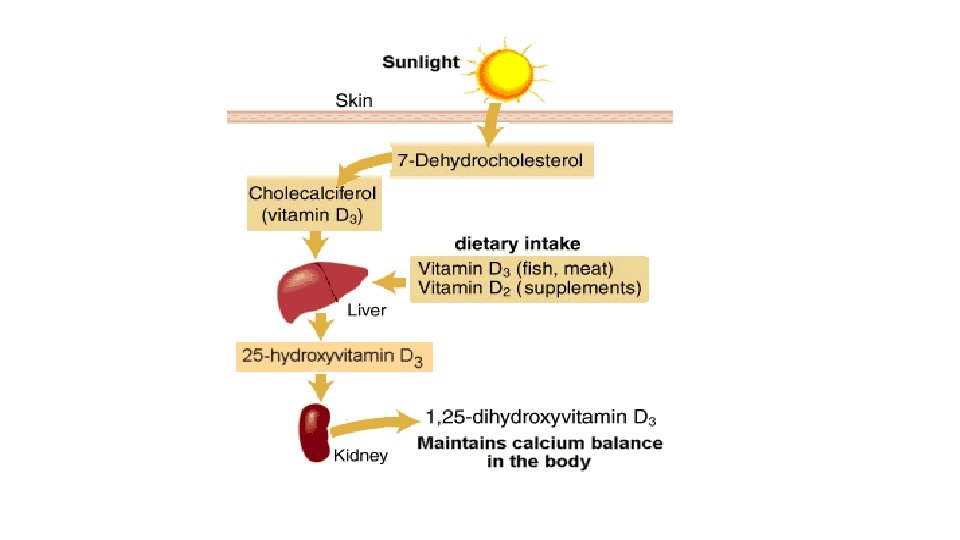
• What are the physiological functions of calcium ? • Is calcium considered a clotting factor ? If yes which one ? • What is the normal range of calcium in the body ? • In which form is it circulating in the blood ? What part of the circulating calcium is responsible for it’s physiological role ? • How do acid –base disorders affect calcium homeostasis ? • How is the calcium level maintained at it’s normal physiological range ?
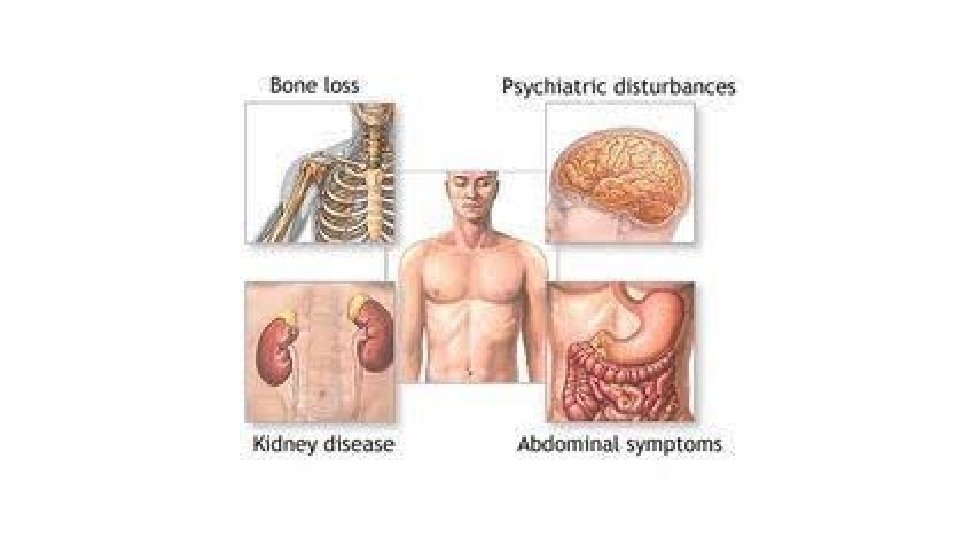
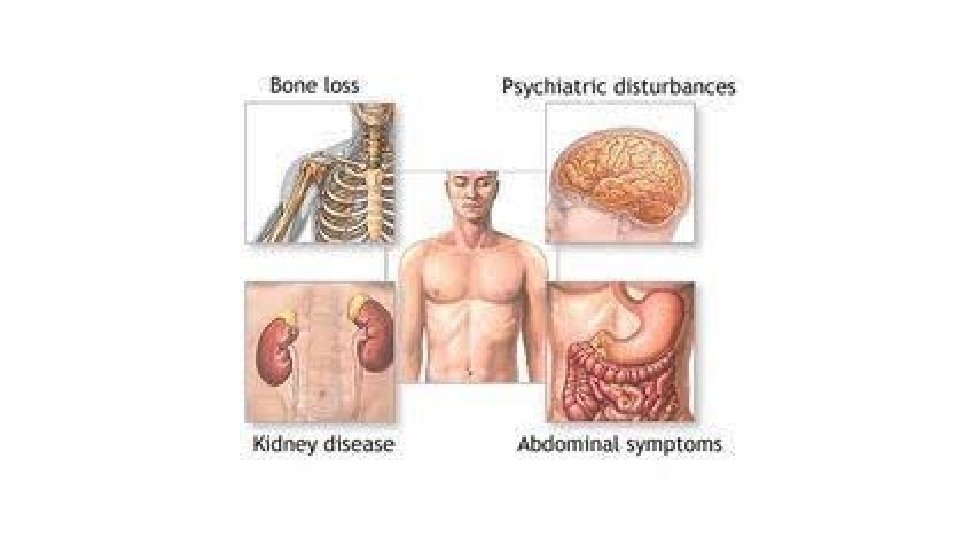
Hypercalcemia • What are the clinical manifestations of hypercalcemia ? • What are the possible causes of hypercalcemia and how are they classified ? • What are the steps to diagnose the cause of hypercalcemia ? • What is the most common cause of hypocalcemia in outpatient vs. hospital settings ? • Name medications known to cause hypercalcemia ? • How does lithium cause hypercalcemia ? • What are the possible mechanisms behind hypercalcemia of malignancy ? What are the common malignancies as culprits of each type ?
Causes of hypercalcemia , classification
Treatment • What are the steps in management of a patient with acute hypercalcemic crisis ? • What are the indications for parathyroidectomy in hyperparathyroidism ? ( chronic management ) • How is the treatment of hypercalcemia caused by granulomatous disease different from other mechanisms ?
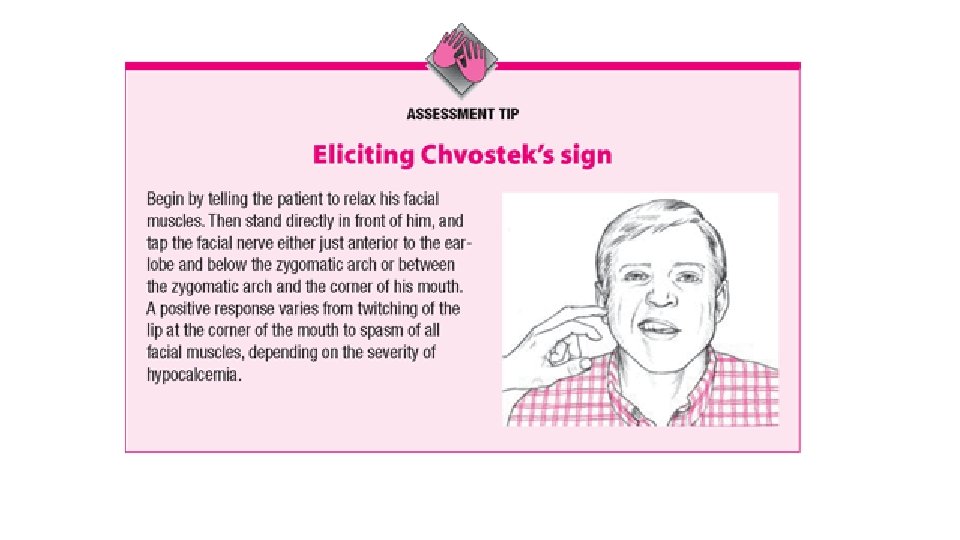
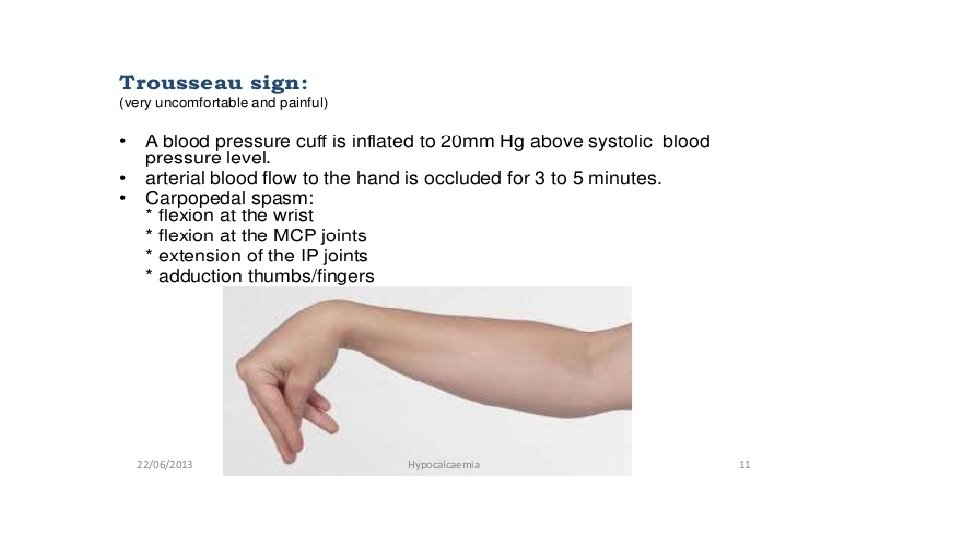
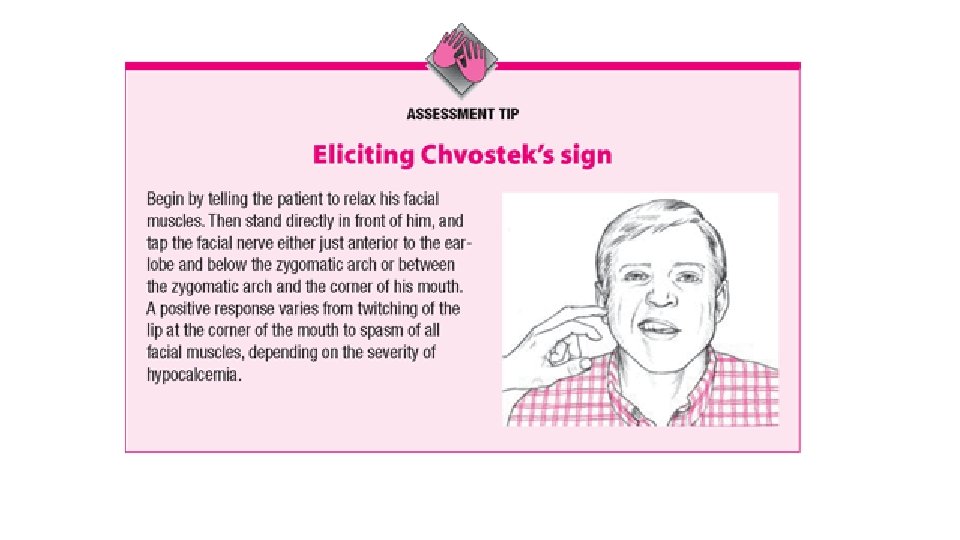
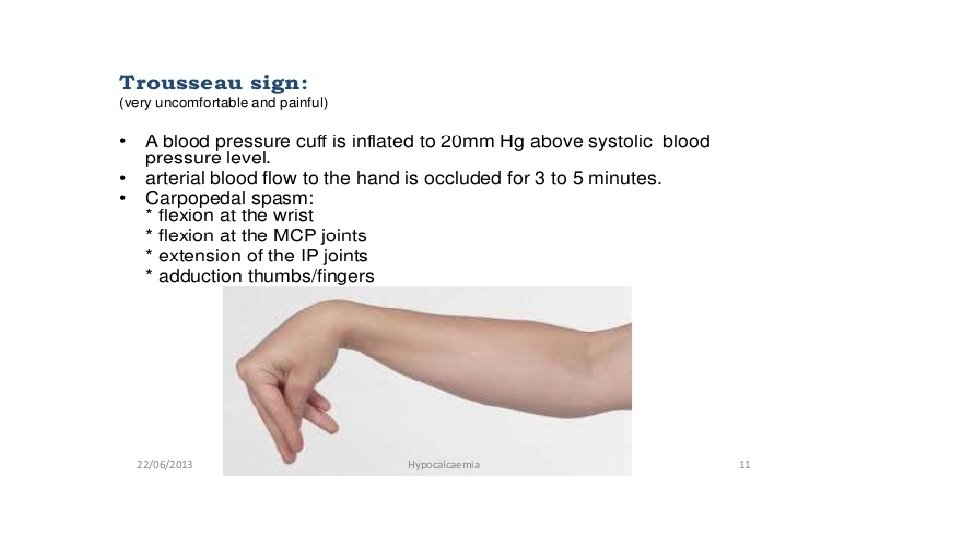
Hypocalcemia • What are the acute manifestations of hypocalcemia ? How is it managed acutely ? • What is hyperventilation syndrome and how does it lead to the same clinical presentation as hypocalcemia , despite normal serum total calcium level ? how is it managed ?
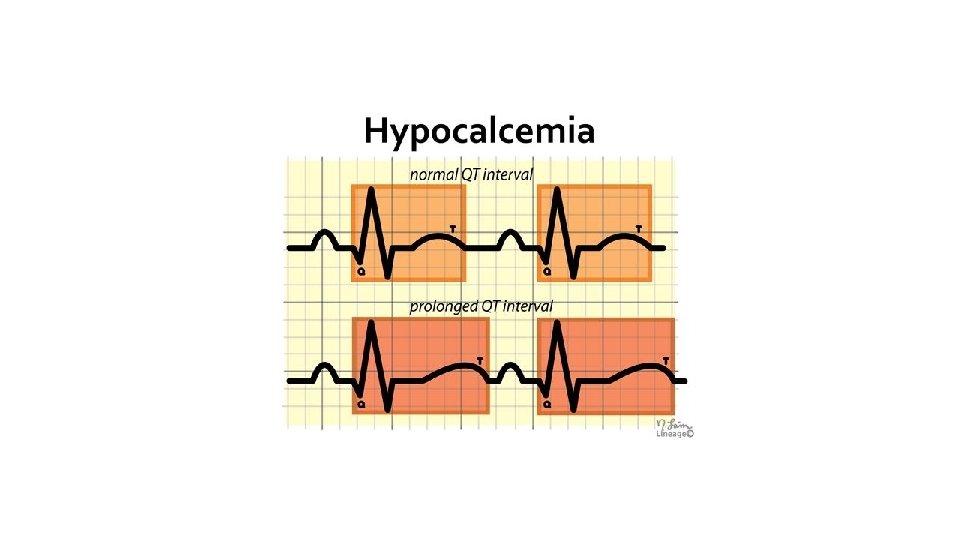
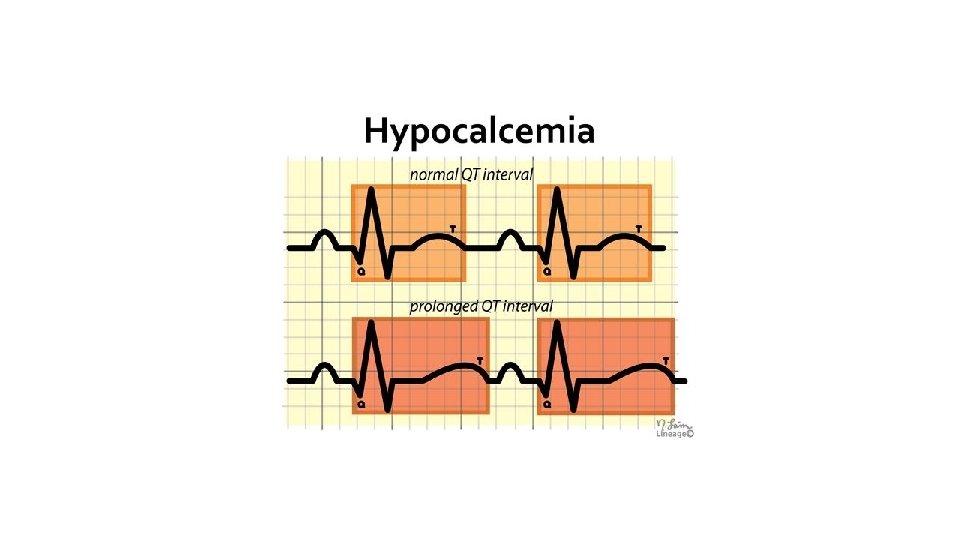
Management of acute hypocalcemia • In patients with marked hypocalcemia , calcium should be delivered by slow continuous intravenous infusion ( for example , calcium gluconate as 0. 5 -1. 5 mg elemental calcium /kg body weight / hour till symptoms subside , With continuous cardiac monitoring , especially QT interval.
Approach to chronic hypocalcemia • What is the most common acquired cause of hypoparathyroidism ? • Mention other possible causes of hypoparathyroidism ? • Mention a congenital cause ? • How does hemochromatosis cause hypocalcemia ? • Mention 5 causes of hypocalcemia with normal or high PTH levels with the mechanism behind each of them ?
Management of chronic hypocalcemia • Why is the target calcium kept at the lower limit of normal not to be exceeded in patients with hypoparathyroidism ?
Thank you