Ca CHANNEL BLOCKERS Classificatio Dihydropyridines Nifedipine Nicardipine Amlodepine
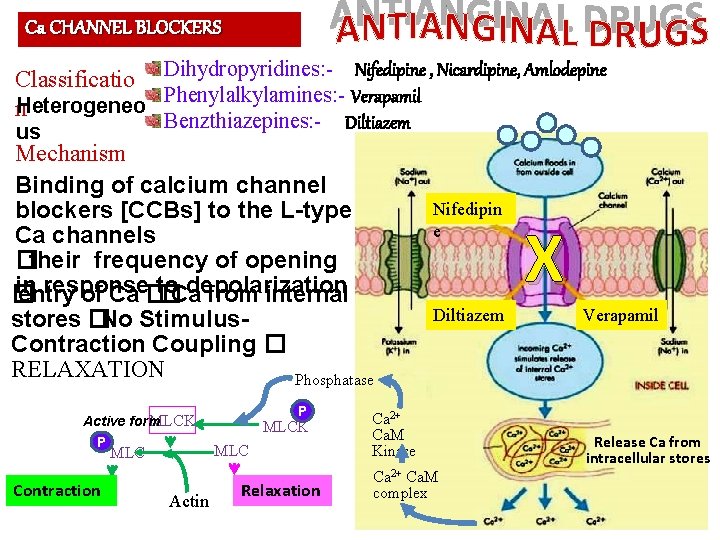
Ca CHANNEL BLOCKERS Classificatio Dihydropyridines: - Nifedipine , Nicardipine, Amlodepine Phenylalkylamines: - Verapamil n. Heterogeneo Benzthiazepines: - us Diltiazem Mechanism Binding of calcium channel blockers [CCBs] to the L-type Ca channels �their frequency of opening in response to depolarization � entry of Ca � �Ca from internal stores �No Stimulus. Contraction Coupling � RELAXATION Phosphatase P MLCK Active form P Contraction MLC Actin Relaxation Nifedipin e Diltiazem Ca 2+ Ca. M Kinase Ca 2+ Ca. M complex X Verapamil Release Ca from intracellular stores
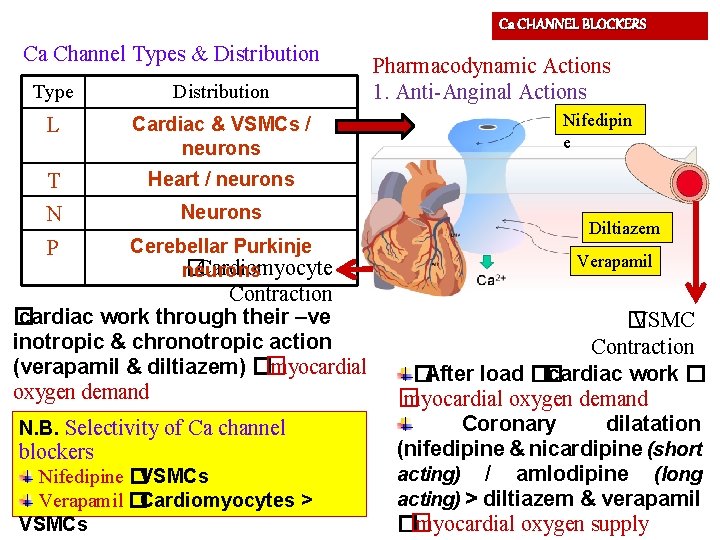
Ca CHANNEL BLOCKERS Ca Channel Types & Distribution Type Distribution L Cardiac & VSMCs / neurons T Heart / neurons N Neurons P Cerebellar Purkinje �Cardiomyocyte neurons Contraction � cardiac work through their –ve inotropic & chronotropic action (verapamil & diltiazem) �� myocardial oxygen demand N. B. Selectivity of Ca channel blockers Nifedipine �VSMCs Verapamil �Cardiomyocytes > VSMCs Pharmacodynamic Actions 1. Anti-Anginal Actions Nifedipin e Diltiazem Verapamil � VSMC Contraction �After load �� cardiac work � � myocardial oxygen demand Coronary dilatation (nifedipine & nicardipine (short acting) / amlodipine (long acting) > diltiazem & verapamil �� myocardial oxygen supply
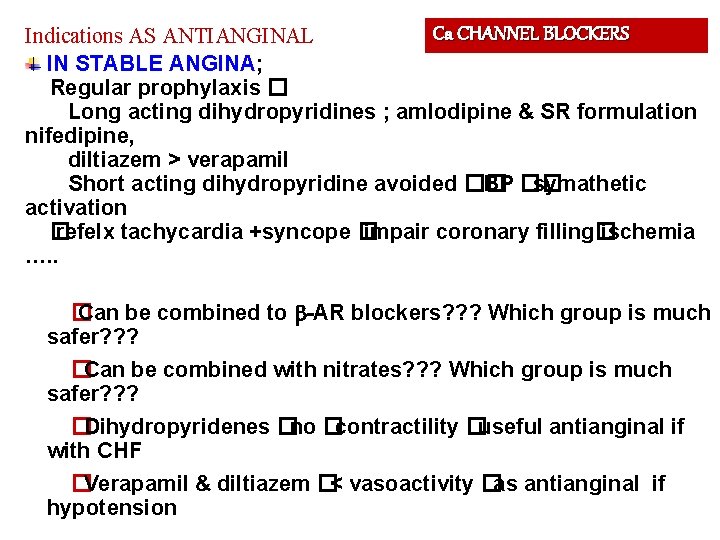
Ca CHANNEL BLOCKERS Indications AS ANTIANGINAL IN STABLE ANGINA; Regular prophylaxis � Long acting dihydropyridines ; amlodipine & SR formulation nifedipine, diltiazem > verapamil Short acting dihydropyridine avoided �� BP �� symathetic activation � refelx tachycardia +syncope � impair coronary filling� ischemia …. . � Can be combined to -AR blockers? ? ? Which group is much safer? ? ? �Can be combined with nitrates? ? ? Which group is much safer? ? ? �Dihydropyridenes �no �contractility �useful antianginal if with CHF �Verapamil & diltiazem �< vasoactivity �as antianginal if hypotension
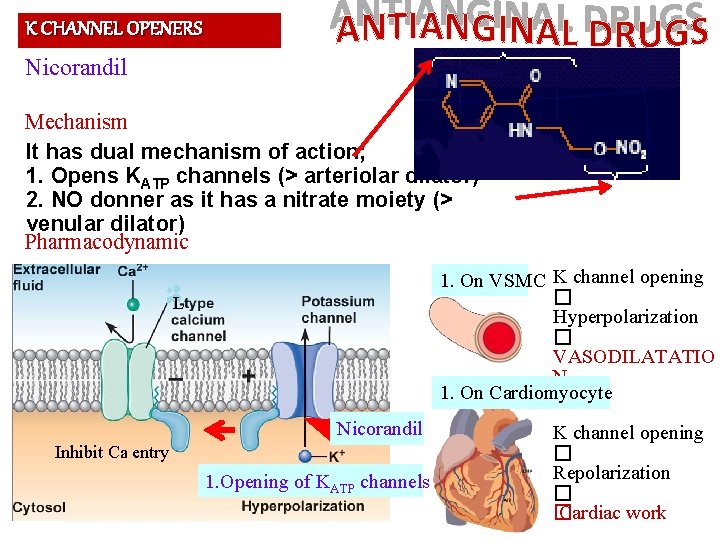
K CHANNEL OPENERS Nicorandil Mechanism It has dual mechanism of action; 1. Opens KATP channels (> arteriolar dilator) 2. NO donner as it has a nitrate moiety (> venular dilator) Pharmacodynamic 1. On VSMC K channel opening � Hyperpolarization � VASODILATATIO N 1. On Cardiomyocyte L Nicorandil Inhibit Ca entry 1. Opening of KATP channels K channel opening � Repolarization � � Cardiac work
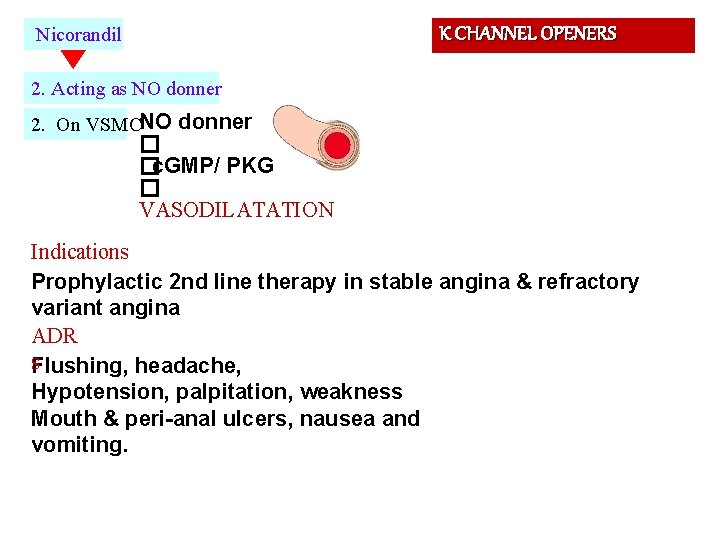
K CHANNEL OPENERS Nicorandil 2. Acting as NO donner 2. On VSMCNO donner � �c. GMP/ PKG � VASODILATATION Indications Prophylactic 2 nd line therapy in stable angina & refractory variant angina ADR s Flushing, headache, Hypotension, palpitation, weakness Mouth & peri-anal ulcers, nausea and vomiting.
DRUGS USED IN TREATMENT OF ANGINA
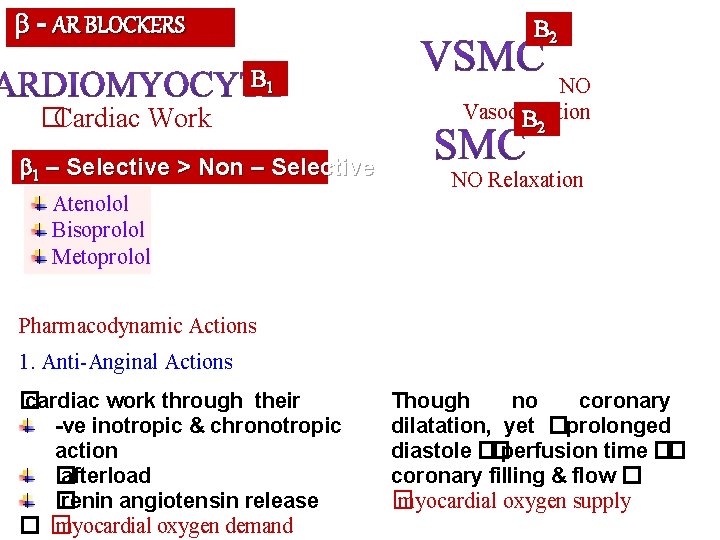
- AR BLOCKERS B 2 B 1 �Cardiac Work 1 – Selective > Non – Selective Atenolol Bisoprolol Metoprolol NO Vasodilatation B 2 NO Relaxation Pharmacodynamic Actions 1. Anti-Anginal Actions � cardiac work through their -ve inotropic & chronotropic action � afterload � renin angiotensin release �� myocardial oxygen demand Though no coronary dilatation, yet �prolonged diastole ��perfusion time �� coronary filling & flow � � myocardial oxygen supply
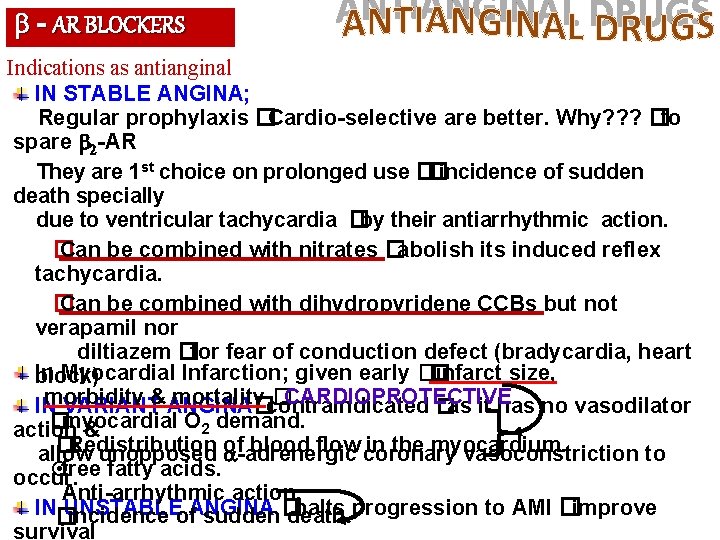
- AR BLOCKERS Indications as antianginal IN STABLE ANGINA; Regular prophylaxis �Cardio-selective are better. Why? ? ? �to spare 2 -AR They are 1 st choice on prolonged use ��incidence of sudden death specially due to ventricular tachycardia �by their antiarrhythmic action. � Can be combined with nitrates �abolish its induced reflex tachycardia. � Can be combined with dihydropyridene CCBs but not verapamil nor diltiazem �for fear of conduction defect (bradycardia, heart In Myocardial Infarction; given early �� infarct size, block) morbidity mortality contraindicated �CARDIOPROTECTIVE IN VARIANT&ANGINA� �as it has no vasodilator �myocardial O 2 demand. action & �Redistribution blood flow coronary in the myocardium. allow unopposed of -adrenergic vasoconstriction to ¤free fatty acids. occur. Anti-arrhythmic action. IN� UNSTABLE halts progression to AMI �improve incidence of. ANGINA sudden � death. survival
- AR BLOCKERS Precautions - blockers should be withdrawn gradually as sudden stoppage �give rise to a withdrawal manifestations: Rebound angina, arrhythmia, myocardial infarction & hypertension WHY ? �Up-regulation of -receptors. Non-selective are better avoided as they blocks vasodilatory effects of sympathetic stimulation �� afterload & �oxygen consumption. Not used in variant angina �worsen symptoms and aggrevate condition Given to diabetics with ischemic heart disease �[Benefits > hazards) & ACE inhibitor must too be added specially in ACSs
DRUGS USED IN TREATMENT OF ANGINA
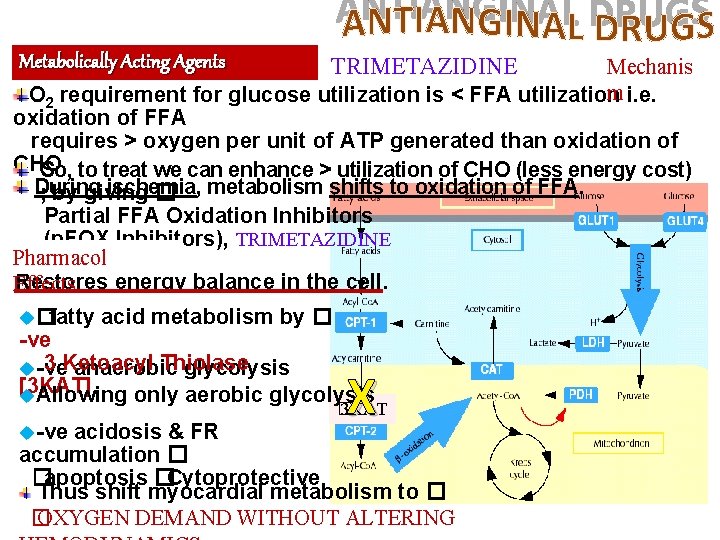
Metabolically Acting Agents TRIMETAZIDINE Mechanis m i. e. O 2 requirement for glucose utilization is < FFA utilization oxidation of FFA requires > oxygen per unit of ATP generated than oxidation of CHO. So, to treat we can enhance > utilization of CHO (less energy cost) During ischemia, ; by giving � metabolism shifts to oxidation of FFA. Partial FFA Oxidation Inhibitors (p. FOX Inhibitors), TRIMETAZIDINE Pharmacol Restores energy balance in the cell. Effects u� fatty acid metabolism by � -ve 3 Ketoacyl Thiolase u-ve anaerobic glycolysis [3 KAT] u. Allowing only aerobic glycolysis u-ve X � 3 KAT acidosis & FR accumulation � �apoptosis �Cytoprotective Thus shift myocardial metabolism to � � OXYGEN DEMAND WITHOUT ALTERING
Metabolically Acting Agents Indication Used when ever needed as add on therapy to nitrates, CCBs or -blockers ADRs �GIT disturbances Contraindication Hypersensitivity reaction s In pregnancy & lactation Ranolazine Newly introduced. Considered one of the metabolically acting agents like trimetazedine. + affects Na dependent-Ca Channels �prevents Ca load �� apoptosis �cardioprotective. It prolongs the QT interval so not given with; Class Ia & III antiarrhthmics Toxicity develops due to interaction with CYT 450 inhibitors as; diltiazem, verapamil, ketoconazole, macrolide antibiotics,
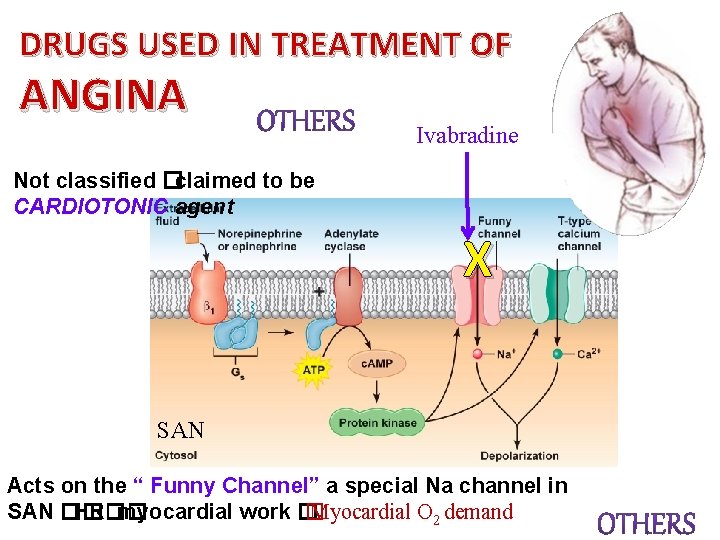
DRUGS USED IN TREATMENT OF ANGINA Ivabradine Not classified �claimed to be CARDIOTONIC agent X SAN Acts on the “ Funny Channel” a special Na channel in SAN �� HR�� myocardial work � � Myocardial O 2 demand
DRUGS USED IN TREATMENT OF ANGINA Aspirin / Other antiplatelets Statins ACE Inhibitors -AD blockers Main Stay of Prophylactic Treatment Halt progression Prevent acute insults
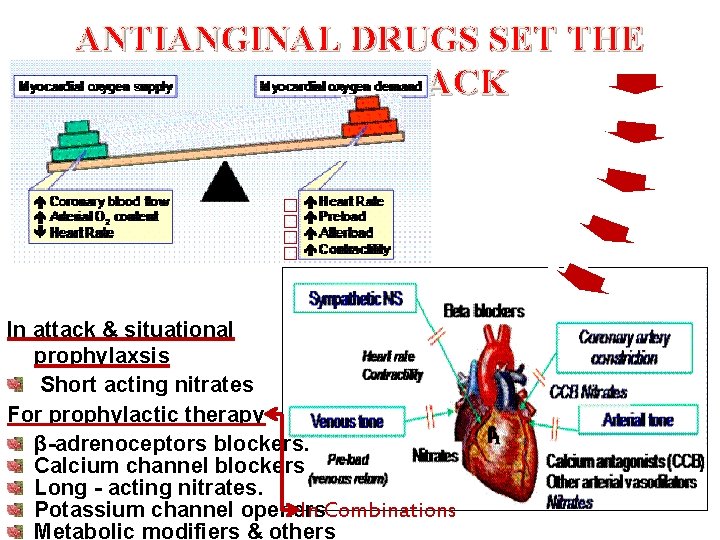
ANTIANGINAL DRUGS SET THE BALANCE BACK � � In attack & situational prophylaxsis Short acting nitrates For prophylactic therapy β-adrenoceptors blockers. Calcium channel blockers Long - acting nitrates. Potassium channel openers In Combinations Metabolic modifiers & others
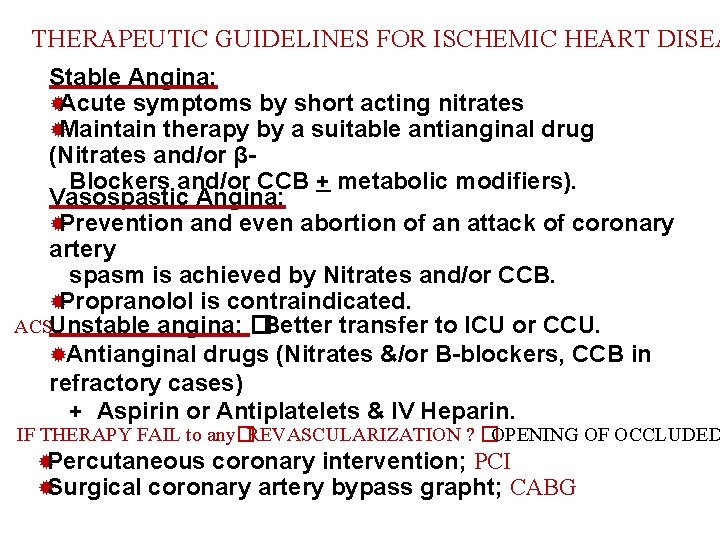
THERAPEUTIC GUIDELINES FOR ISCHEMIC HEART DISEA Stable Angina: ®Acute symptoms by short acting nitrates ®Maintain therapy by a suitable antianginal drug (Nitrates and/or βBlockers and/or CCB + metabolic modifiers). Vasospastic Angina: ®Prevention and even abortion of an attack of coronary artery spasm is achieved by Nitrates and/or CCB. ®Propranolol is contraindicated. ACSUnstable angina: � Better transfer to ICU or CCU. ®Antianginal drugs (Nitrates &/or B-blockers, CCB in refractory cases) + Aspirin or Antiplatelets & IV Heparin. IF THERAPY FAIL to any�REVASCULARIZATION ? �OPENING OF OCCLUDED ®Percutaneous coronary intervention; PCI ®Surgical coronary artery bypass grapht; CABG
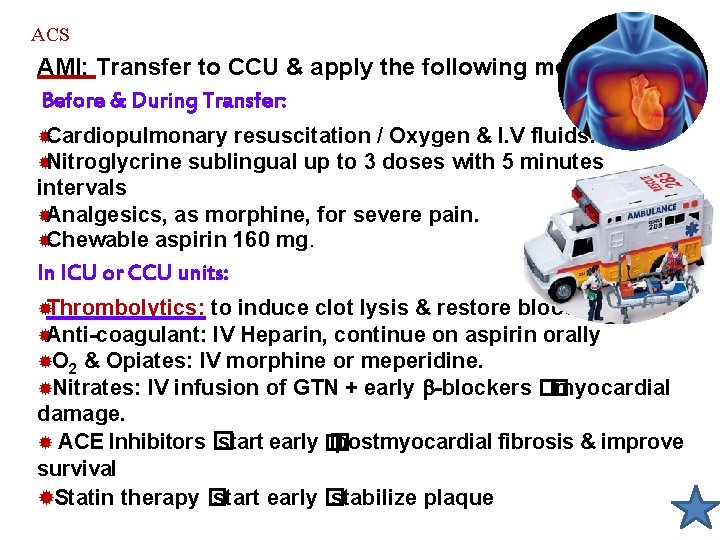
ACS AMI: Transfer to CCU & apply the following measures: Before & During Transfer: ®Cardiopulmonary resuscitation / Oxygen & I. V fluids. ®Nitroglycrine sublingual up to 3 doses with 5 minutes intervals ®Analgesics, as morphine, for severe pain. ®Chewable aspirin 160 mg. In ICU or CCU units: ®Thrombolytics: to induce clot lysis & restore blood flow ®Anti-coagulant: IV Heparin, continue on aspirin orally ®O 2 & Opiates: IV morphine or meperidine. ®Nitrates: IV infusion of GTN + early -blockers �� myocardial damage. ® ACE Inhibitors � start early � � postmyocardial fibrosis & improve survival ®Statin therapy � start early � stabilize plaque
GOOD LUCK
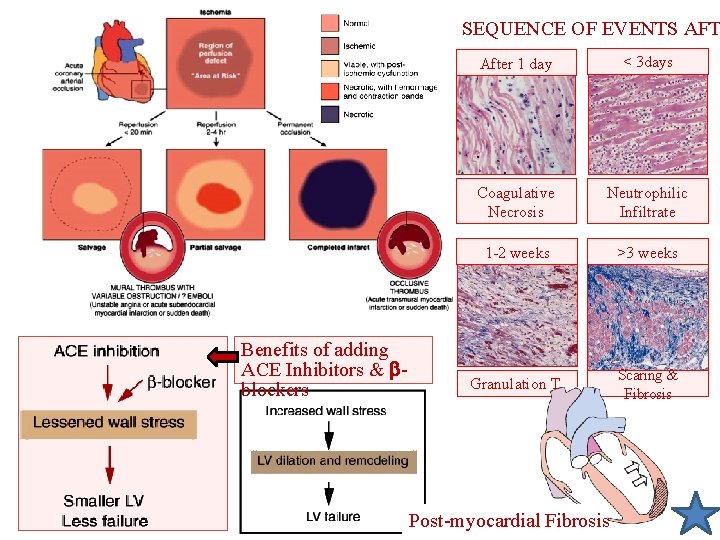
SEQUENCE OF EVENTS AFT Benefits of adding ACE Inhibitors & blockers After 1 day < 3 days Coagulative Necrosis Neutrophilic Infiltrate 1 -2 weeks >3 weeks Granulation T. Scaring & Fibrosis Post-myocardial Fibrosis
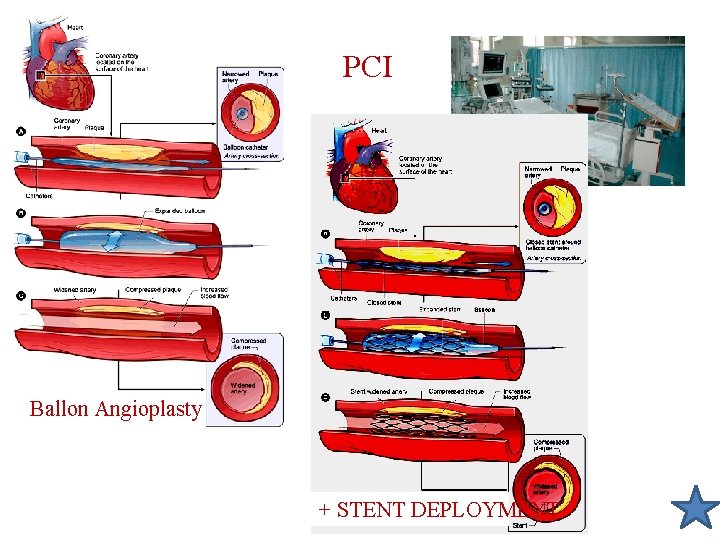
PCI Ballon Angioplasty + STENT DEPLOYMENT
A 60 -year-old man comes into the office complaining of chest pains that primarily occur in the early morning and do not appear to be associated with stress or exercise. Following coronary angiography and a positive ergonovine test you determine that this patient has angina pectoris as a result of coronary artery spasm.
Q 1 • How would you treat the patient to alleviate the acute attacks when they occur ?
Q 2 • How would you treat chronically to prevent their reoccurrence?
- Slides: 23