C 35 SPINA BIFIDA IN UTERO OBJECTIVES Describe

C 35 SPINA BIFIDA IN UTERO
OBJECTIVES Describe the function of the spinal cord Discuss different treatment options Examine spina bifida in fetal development Explain the role of imaging in the diagnosis process Discuss the different severities of spina bifida Discover how spina bifida is detected in utero Summarize the risk factors of treating spina bifida Identify the prognosis of spina bifida
THESIS v. Spina Bifida is a disease of the spinal cord that can be developed in utero and detected by medical imaging to provide treatment before birth and increase the quality of life for the fetus.
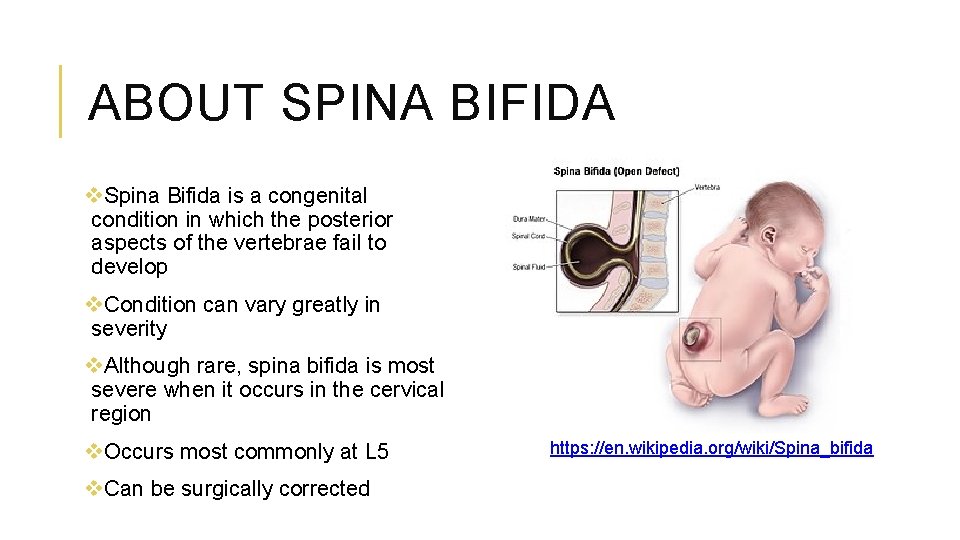
ABOUT SPINA BIFIDA v. Spina Bifida is a congenital condition in which the posterior aspects of the vertebrae fail to develop v. Condition can vary greatly in severity v. Although rare, spina bifida is most severe when it occurs in the cervical region v. Occurs most commonly at L 5 v. Can be surgically corrected https: //en. wikipedia. org/wiki/Spina_bifida
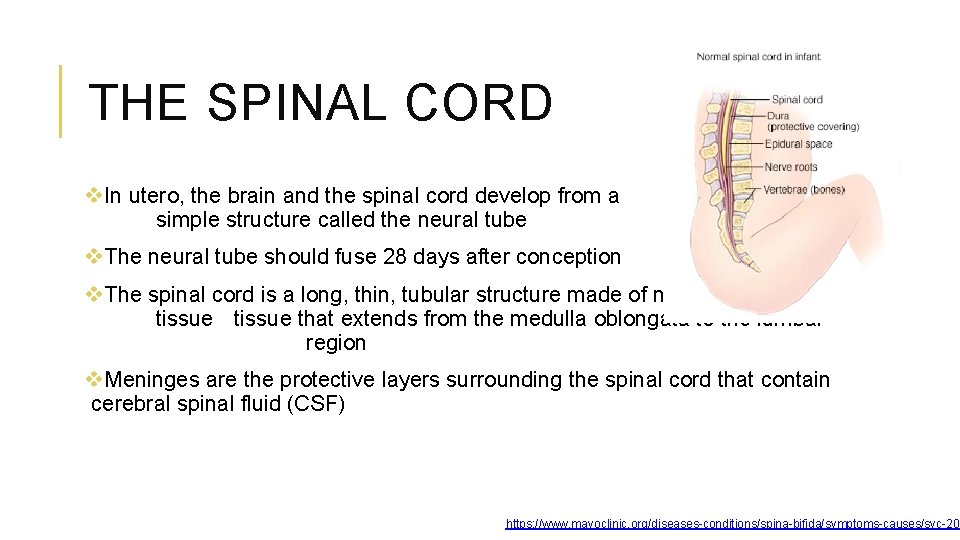
THE SPINAL CORD v. In utero, the brain and the spinal cord develop from a simple structure called the neural tube v. The neural tube should fuse 28 days after conception v. The spinal cord is a long, thin, tubular structure made of nervous tissue that extends from the medulla oblongata to the lumbar region v. Meninges are the protective layers surrounding the spinal cord that contain cerebral spinal fluid (CSF) https: //www. mayoclinic. org/diseases-conditions/spina-bifida/symptoms-causes/syc-203
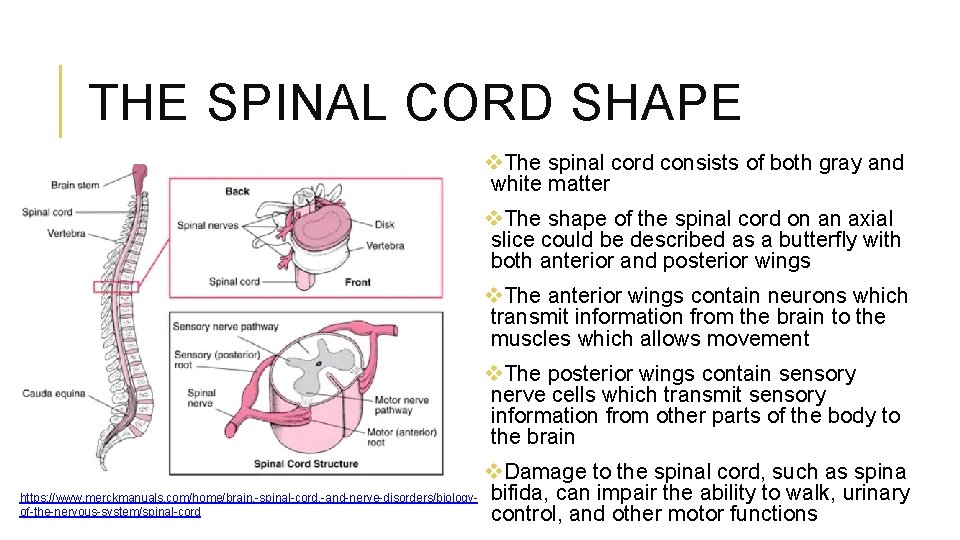
THE SPINAL CORD SHAPE v. The spinal cord consists of both gray and white matter v. The shape of the spinal cord on an axial slice could be described as a butterfly with both anterior and posterior wings v. The anterior wings contain neurons which transmit information from the brain to the muscles which allows movement v. The posterior wings contain sensory nerve cells which transmit sensory information from other parts of the body to the brain v. Damage to the spinal cord, such as spina https: //www. merckmanuals. com/home/brain, -spinal-cord, -and-nerve-disorders/biology- bifida, can impair the ability to walk, urinary of-the-nervous-system/spinal-cord control, and other motor functions
SEVERITIES OF SPINA BIFIDA There are three different forms of spina bifida: v. Occulta v. Meningocele v. Myelomeningocele

SEVERITIES OF SPINA BIFIDA: OCCULTA v. Most mild form of Spina Bifida v. A defect occurs on the posterior arch of the vertebrae but there is no protrusion of the spinal cord or the meninges v. No nerve damage and no major impairment of quality of life of the fetus https: //medicaldialogues. in/new-smartphone-app-to-help-spinabifida-patients v. A sign of spina bifida occulta after birth can be visualized by a patch of hair growth at the site of where the defect occurred
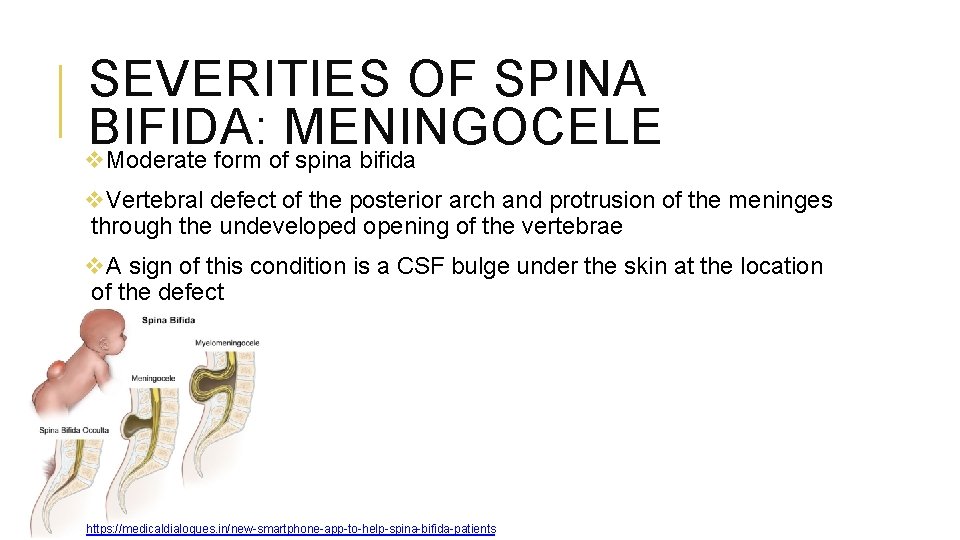
SEVERITIES OF SPINA BIFIDA: MENINGOCELE v. Moderate form of spina bifida v. Vertebral defect of the posterior arch and protrusion of the meninges through the undeveloped opening of the vertebrae v. A sign of this condition is a CSF bulge under the skin at the location of the defect https: //medicaldialogues. in/new-smartphone-app-to-help-spina-bifida-patients
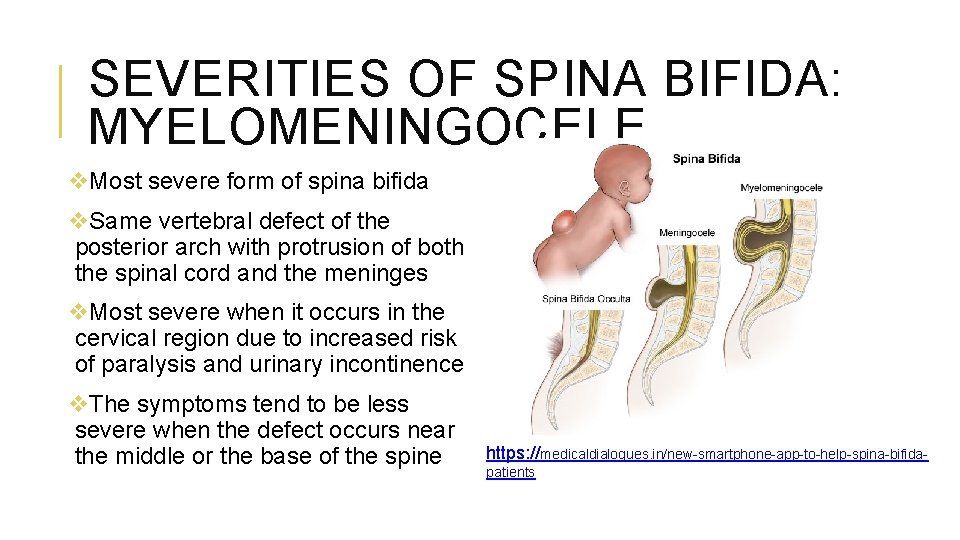
SEVERITIES OF SPINA BIFIDA: MYELOMENINGOCELE v. Most severe form of spina bifida v. Same vertebral defect of the posterior arch with protrusion of both the spinal cord and the meninges v. Most severe when it occurs in the cervical region due to increased risk of paralysis and urinary incontinence v. The symptoms tend to be less severe when the defect occurs near the middle or the base of the spine https: //medicaldialogues. in/new-smartphone-app-to-help-spina-bifidapatients
DIAGNOSING SPINA BIFIDA IN UTERO: BLOOD TEST v. Spina bifida is suspected after a routine blood test at 15 weeks gestation v. Blood test is used to detect the amount of alpha fetoprotein (AFP) in the mother’s blood v. Abnormal levels of AFP can indicate a birth defect such as spina bifida

DIAGNOSING SPINA BIFIDA IN UTERO: ULTRASOUND v. The results of an abnormal blood test will encourage the ordering doctor to recommend a high resolution fetal ultrasound v. Ultrasound is the primary medical imaging procedure to detect spina bifida v. Performed by a licensed sonographer using sound waves to detect defects in the fetal spine https: //www. ultrasound-images. com/fetal-spine/
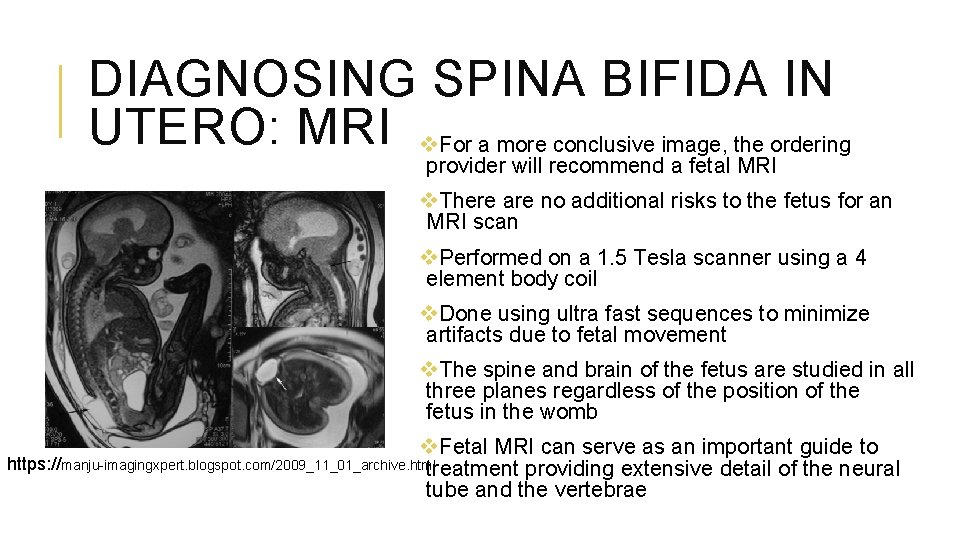
DIAGNOSING SPINA BIFIDA IN UTERO: MRI v. For a more conclusive image, the ordering provider will recommend a fetal MRI v. There are no additional risks to the fetus for an MRI scan v. Performed on a 1. 5 Tesla scanner using a 4 element body coil v. Done using ultra fast sequences to minimize artifacts due to fetal movement v. The spine and brain of the fetus are studied in all three planes regardless of the position of the fetus in the womb v. Fetal MRI can serve as an important guide to https: //manju-imagingxpert. blogspot. com/2009_11_01_archive. html treatment providing extensive detail of the neural tube and the vertebrae
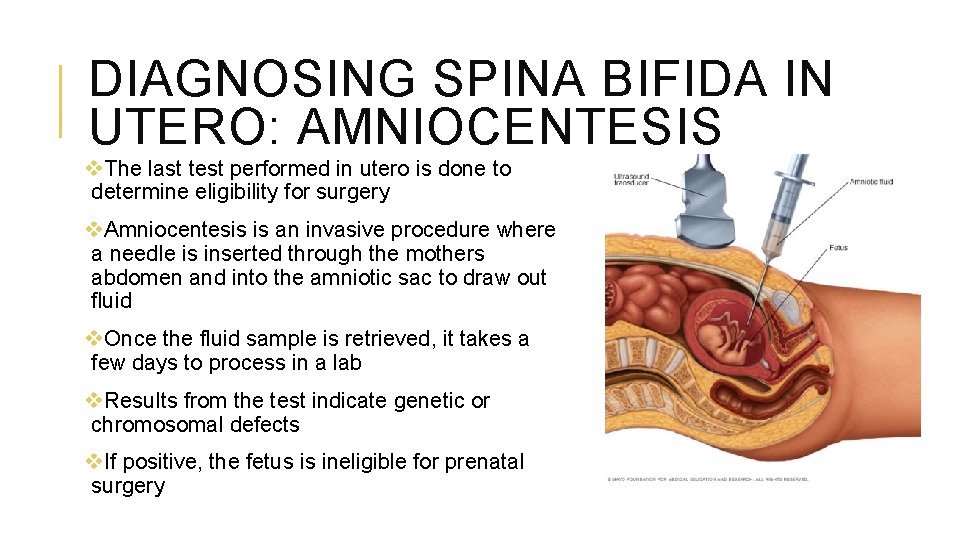
DIAGNOSING SPINA BIFIDA IN UTERO: AMNIOCENTESIS v. The last test performed in utero is done to determine eligibility for surgery v. Amniocentesis is an invasive procedure where a needle is inserted through the mothers abdomen and into the amniotic sac to draw out fluid v. Once the fluid sample is retrieved, it takes a few days to process in a lab v. Results from the test indicate genetic or chromosomal defects v. If positive, the fetus is ineligible for prenatal surgery
WHO IS ELIGIBLE FOR TREATMENT? v. Based on a landmark national study, Management of Myelomeningocele study (MOMS) v. Compared both prenatal and postnatal repairs of myelomeningocele in 183 patients v. Those excluded from this study are those with more mild cases of spina bifida and fetus with other conditions such as genetic or chromosomal defects
TREATMENT v. Traditional treatment for spina bifida is postnatal surgery almost immediately after birth v. Due to advancements in technology, those that qualify are able to receive prenatal surgery v. Prenatal surgery is performed around 23 -25 weeks gestation v. Mother receives anesthesia which then relaxes the uterus and gives a dose of anesthesia to the fetus https: //www. smithsonianmag. com/smartnews/psychological-effects-waking-anesthesia 180952796/
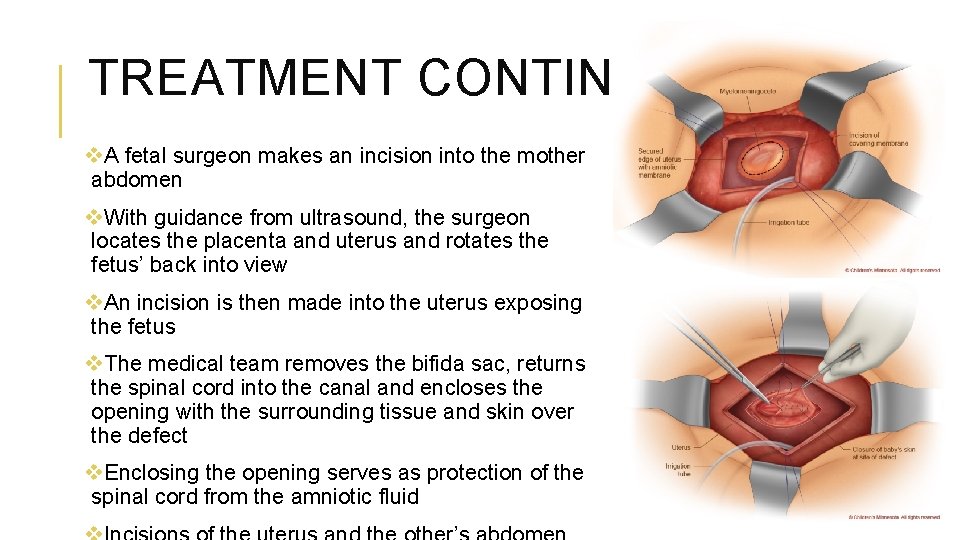
TREATMENT CONTINUED v. A fetal surgeon makes an incision into the mother abdomen v. With guidance from ultrasound, the surgeon locates the placenta and uterus and rotates the fetus’ back into view v. An incision is then made into the uterus exposing the fetus v. The medical team removes the bifida sac, returns the spinal cord into the canal and encloses the opening with the surrounding tissue and skin over the defect v. Enclosing the opening serves as protection of the spinal cord from the amniotic fluid
RECOVERY FROM PRENATAL SURGERY v. Mother must remain in the hospital for 3 -5 days for monitoring v. Mother is put on bed rest for 3 -4 weeks post-op to prevent preterm labor v. Weekly ultrasound appointments and doctor appointments for close monitoring are required v. Goal after treatment is to carry the baby to 36 weeks and plan for a cesarean birth v. Infants must remain in the hospital for one week for observation after birth v. Discharge from the hospital is attained if the baby is feeding and growing properly
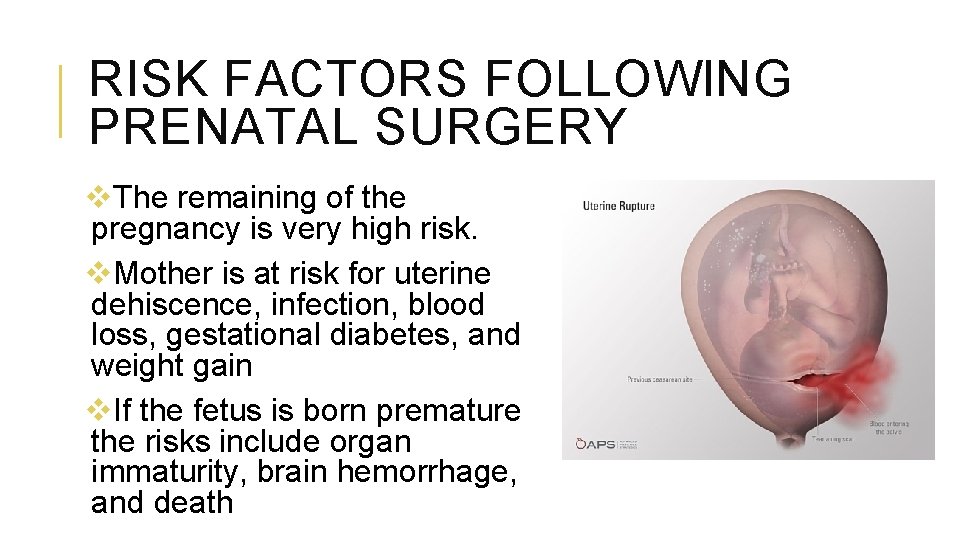
RISK FACTORS FOLLOWING PRENATAL SURGERY v. The remaining of the pregnancy is very high risk. v. Mother is at risk for uterine dehiscence, infection, blood loss, gestational diabetes, and weight gain v. If the fetus is born premature the risks include organ immaturity, brain hemorrhage, and death
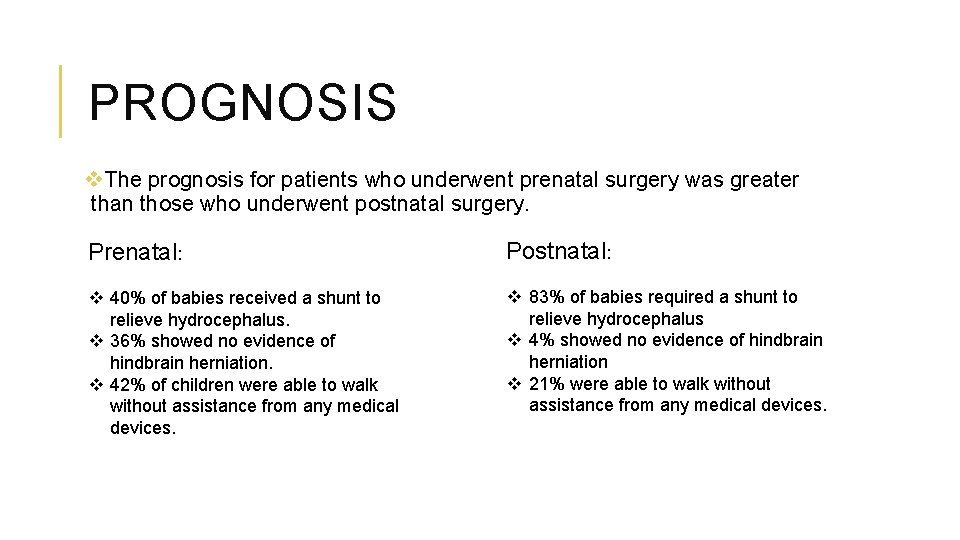
PROGNOSIS v. The prognosis for patients who underwent prenatal surgery was greater than those who underwent postnatal surgery. Prenatal: Postnatal: v 40% of babies received a shunt to relieve hydrocephalus. v 36% showed no evidence of hindbrain herniation. v 42% of children were able to walk without assistance from any medical devices. v 83% of babies required a shunt to relieve hydrocephalus v 4% showed no evidence of hindbrain herniation v 21% were able to walk without assistance from any medical devices.
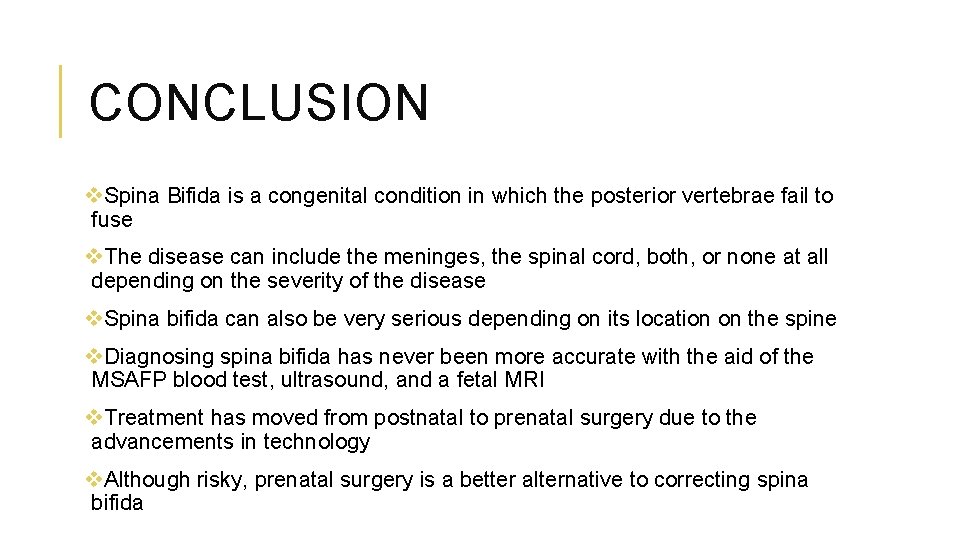
CONCLUSION v. Spina Bifida is a congenital condition in which the posterior vertebrae fail to fuse v. The disease can include the meninges, the spinal cord, both, or none at all depending on the severity of the disease v. Spina bifida can also be very serious depending on its location on the spine v. Diagnosing spina bifida has never been more accurate with the aid of the MSAFP blood test, ultrasound, and a fetal MRI v. Treatment has moved from postnatal to prenatal surgery due to the advancements in technology v. Although risky, prenatal surgery is a better alternative to correcting spina bifida
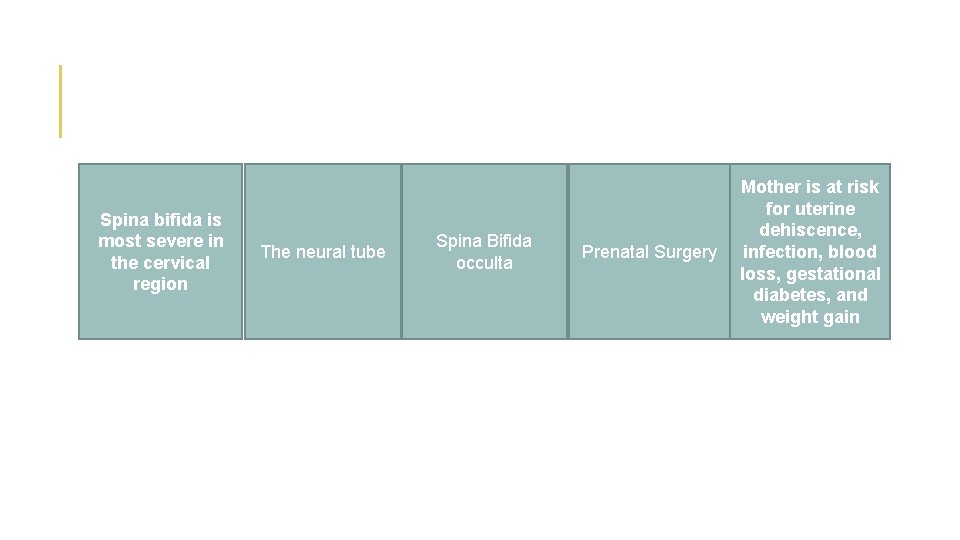
Where on the Spina is spine bifida is spina most severe bifida most in thesevere? cervical region The spinal cord What is the most Spinaform Bifida and develop mild of Thebrain neural tube occulta from what in spina bifida? utero? Which treatment option has a Prenatal Surgery better prognosis? Mother is at risk for uterine What are the dehiscence, risks of the infection, blood mother after loss, gestational surgery? and diabetes, weight gain
REFERENCES Bontrager, K. L. , & Lampignano, J. P. (2014). Textbook of radiographic positioning and related anatomy. St. Louis, MO: Elsevier/Mosby. Children's Hospital. (n. d. ). About Fetal Surgery for Spina Bifida (Myelomeningocele). Retrieved March 24, 2020, from https: //www. chop. edu/treatments/fetal surgery-spina-bifida/about Children's Minnesota. (n. d. ). Spina Bifida Treatment. Retrieved March 24, 2020, from https: //www. childrensmn. org/services/care-specialties-departments/fetal- medicine/conditions-and- services/spina-bifida /? gclid=Cj 0 KCQjw 9 Zzz. BRCKARIs. ANw. Xae. JHea 6 t 5 W 1 IMR_Zu. Etb. Ie 99 x. Nth. WJn 8 H 26 Fbw 3 w. Uc. AT 7 mr 2 xn. Uu. Ms. Ia. An 8 - EALw_wc. B Goldman, S. A. (2018, March). Spinal Cord - Brain, Spinal Cord, and Nerve Disorders. Retrieved March 24, 2020, from https: //www. merckmanuals. com/home/brain, -spinal-cord, - and nerve-disorders/biology-of-the-nervous-system/spinal-cord Keshavamurthy, J. (n. d. ). Spina bifida: cervical spine: Radiology Case. Retrieved March 24, 2020, from https: //radiopaedia. org/cases/spina-bifida-cervical-spine? lang=us Mayo Clinic. (2019, December 17). Spina bifida. Retrieved March 24, 2020, from https: //www. mayoclinic. org/diseases-conditions/spina-bifida/care-at-mayo-clinic/mac 20377871? mc_id=google&campaign=920819937&geo=9018818&kw=spina bifida surgery&ad=414772754380&network=g&sitetarget =&adgroup=48738350351&extension=&target=kwd 344645592940&matchtype=p&device=c&account=6561937437&placementsite=minnesota&gclid=Cj 0 KCQjw 9 Zzz. BRCKARIs. ANw. Xae. Iy. Eu. BTh. MAm-z 3 a. G 6 o. Y 1 Po. DPTt o. RSk. Xxlr. Qj. E_Aspdb. QQeo. Ivihx. Ea. Aocg. EALw_wc. B NIHR. (2017, April 4). MRI scans help confirm ultrasound diagnosis of fetal brain abnormalities. Retrieved March 24, 2020, from https: //discover. dc. nihr. ac. uk/content/signalfetal-brain-abnormalities 000404/mri-scans-help-confirm-ultrasound-diagnosis-of- Woźniak, M. M. (2012). What are the risks of ultrasound and MRI to a fetus? Retrieved March 24, 2020, from https: //www. openaccessjournals. com/articles/what-are-the-risks-offetus. pdf ultrasound-and-mri-to-the-
- Slides: 23