Burns Fluid Electrolytes Nursing Care BURN INJURIES 1
Burns Fluid & Electrolytes
Nursing Care BURN INJURIES 1. Identify the mechanism of burn (TYPE) injuries. 2. Describe methods for determining assessment/physiology/ ssessment classification of burns. 3. Differentiate degrees of burn (1 st- 4 th) versus epidermal/superficial, partial and full thickness, deep burns. 4. Determine nursing care based upon the systemic pathological changes associated with burn injury in the first 24 – 48 hours. 5. Identify assessment, nursing diagnoses and management of the burn victim’s airway, breathing and circulation and wounds. 6. Identify the Pain/Nutritional/Rehab requirements for a burns patient.
Mechanism/Burn Type • Thermal - burning of tissue via direct contact with a heat source hot water, flame • Zones of Injury – 1. Zone of coagulation – thrombosis, vasoconstriction, necrosis and cell death – 2. Zone of stasis - low blood flow – 3. Zone of hyperemia - inflammatory response
Mechanism/Burn Type • Chemical - tissue destruction via direct Chemical contact chemical · oxidizing agent: sodium hypo chloride · reducing agent : hydrochloric acid · corrosives : phosphorus · protoplasmic poisons : formic acid · desiccants : sulfuric acid · vesicants : mustard gas · gasoline

Mechanism/Type: Chemical Burn
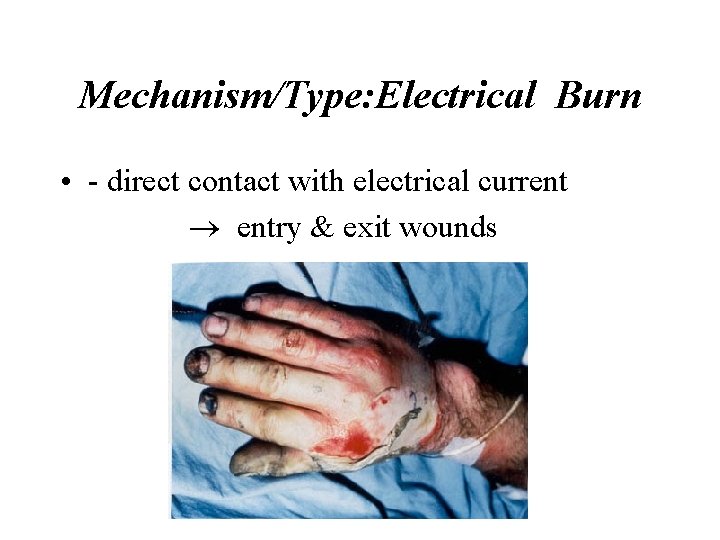
Mechanism/Type: Electrical Burn • - direct contact with electrical current ® entry & exit wounds
Burns Assessment/Physiology/ Classification Assessment Based on: • Depth/Degree of injury, • Percent of body surface areas involved, • Location of the burn, • Association with other injuries.
Burns Physiology/Classification Depth of Burn Assessment Epidermal : destruction epidermis only · reddened, · blanches to pressure, · no blisters · painful · healing 3 -5 days · no scarring
Burns Physiology & Classification Depth/Degree of Injury • First Degree: superficial, epidermal damage – erythematous & painful due to intact nerve endings – heal in 5 -10 days – pain resolves within 3 days – no residual scarring
Burns Physiology & Classification Depth/Degree of Injury • Second Degree: partial thickness, epidermis/ dermis • superficial burns – moist, blister; • deeper burns - white and dry, blanch with pressure, and have reduced pain • heal in 10 -14 days • can develop into third degree burns with infection, edema, inflammation and ischemia • treatment varies with degree of involvement - grafting is indicated for deep burns
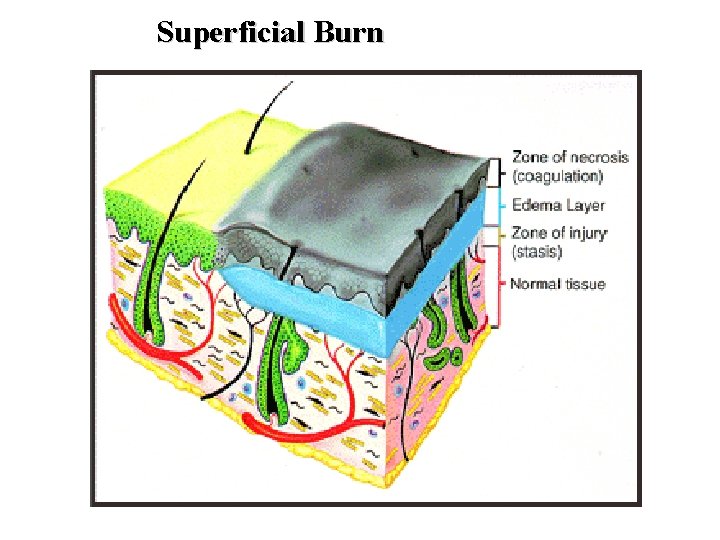
Superficial Burn
Burns Physiology / Classification Depth of Burn Assessment Partial Thickness Superficial destruction epidermis to upper dermis · bright red to pale ivory, blistered or weeping, blanches to pressure · sensitive to pain, pressure temperature · healing 14 -21 days , no scarring
Burns Physiology/Classification Depth of Burn Assessment Partial Thickness deep destruction epidermis to deep dermis · mottled · white & waxy · blistering · diminished sensation to light pressure · healing months-weeks/usually scarring
Burns Physiology & Classification Depth/Degree of Injury • Third Degree: Third Degree full-thickness, most severe of burns • results in necrosis and avascular areas • tough, waxy, brownish leathery surface with eschar, numb to touch • grafting required • usually have permanent impairment
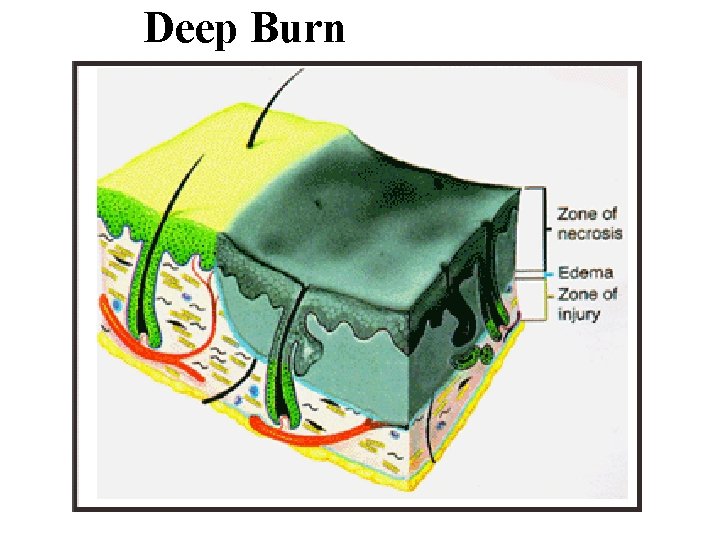
Deep Burn
Burns Physiology & Classification Depth/Degree of Injury • Fourth Degree: • full-thickness as well as adjacent structures such as fat, fascia, muscle or bone • reconstructive surgery is indicated • severe disfigurement is common
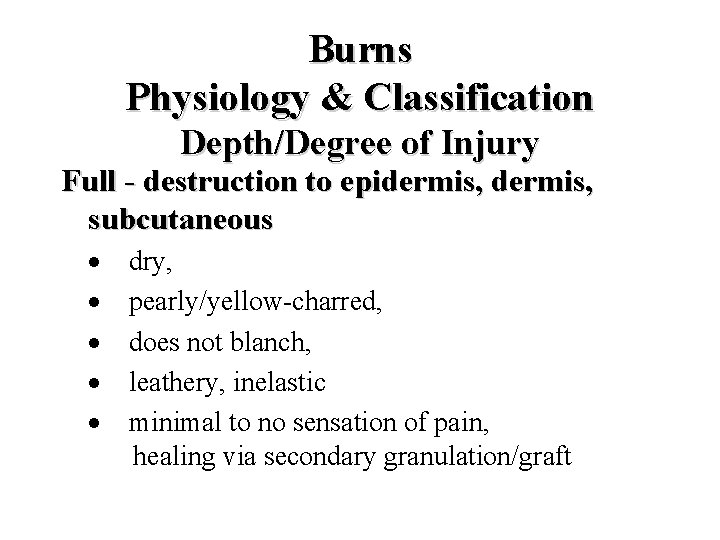
Burns Physiology & Classification Depth/Degree of Injury Full - destruction to epidermis, subcutaneous · dry, · pearly/yellow-charred, · does not blanch, · leathery, inelastic · minimal to no sensation of pain, healing via secondary granulation/graft
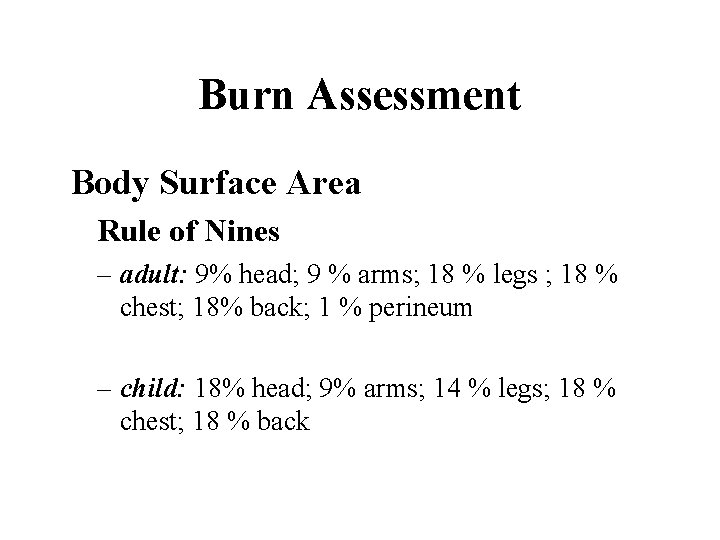
Burn Assessment Body Surface Area Rule of Nines – adult: 9% head; 9 % arms; 18 % legs ; 18 % chest; 18% back; 1 % perineum – child: 18% head; 9% arms; 14 % legs; 18 % chest; 18 % back
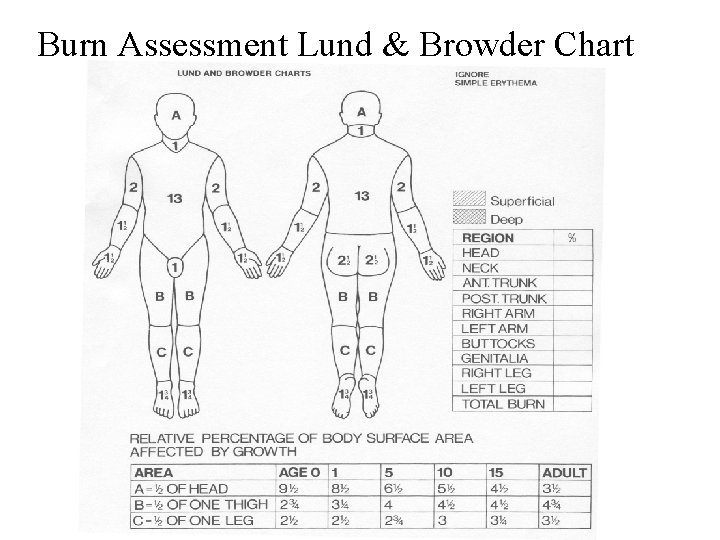
Burn Assessment Lund & Browder Chart
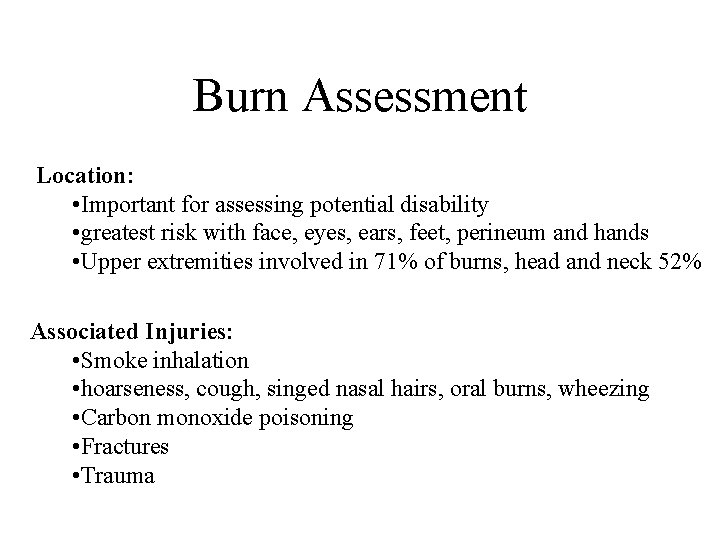
Burn Assessment Location: • Important for assessing potential disability • greatest risk with face, eyes, ears, feet, perineum and hands • Upper extremities involved in 71% of burns, head and neck 52% Associated Injuries: • Smoke inhalation • hoarseness, cough, singed nasal hairs, oral burns, wheezing • Carbon monoxide poisoning • Fractures • Trauma
Hospitalization in Major Burns · >10% surface area in children, elderly · >15% surface area in adults · specific regions - respiratory tract, face, neck, circumferential burns, hands, feet, major joints, genitalia, electrical burns, lightening burns · 3 rd degree burns >3% children, >5% adults
Mortality in Burns · >65% body surface area (BSA) · associated smoke inhalation · infection – >20% BSA with shock and other complications/related sequelae
Collaborative Nursing & Medical Management Pathology of the First 24 hours: · Temperature loss ® hypothermia · Plasma & Protein Loss · Hypovolemia/hemoglobin concentration · Tissue/blood destruction hypoxia · Release hemoglobin pigment/myoglobin ® ¯ GFR & UO · Tissue hypoxia and reduced renal function ® metabolic acidosis · Platelet destruction & of activation clotting cascade via intrinsic/extrinsic pathway ® DIC
Collaborative Nursing & Medical Management Pathology of the Second 48 hours: 1. temperature 2. fluid mobilization to intravascular space 3. renal loss K+ 4 Fluid resuscitation ® Serum Na+ ® dilutional coagulopathy
Collaborative Nursing & Medical Management Wound Care · tetanus toxoid > 50% BSA burn · and/or tetanus immunization · chemical burns – irrigate all burns, cover until initial resuscitation complete · electrical burns – AC current ® Tetany & risk Vent Fib High energy ® check # volts & blunt injuries
Collaborative Burn Management Primary Assessment & Resuscitation Airway check risks – event in an enclosed area, singed eyebrows/nasal hair, hoarse voice, stridor, wheeze, air entry/edema Breathing check risks – event in an enclosed area® evaluate for CO 2 poisoning high Pa. O 2 low Sata. O 2
Collaborative Burn Management Circulation : Assessment & Resuscitation Parkland Formula – one of the most commonly used: First 24 hours an isotonic solution (Ringers Lactate)4 m. L/kg x TBSA% divide into 8 hour periods - first 50% in 8 hours - next 25% in 8 hours - final 25% in 8 hours urinary output should be 50 -70 m. L/hr (1 m. L/kg) in the first 24 hours
Collaborative Burn Management Circulation Con’t: : Assessment & Resuscitation Second 24 hours Colloid/plasma is delivered 0. 5 m. L/kg x TBSA for the next 8 hours. At 32 hours: 5% Dextrose + nutritional replacement require serial measurement serum electrolytes, urea, hematocit, blood albumin, urinary N+.
Nursing Diagnoses • • • Altered Tissue Perfusion Fluid & Electrolyte Imbalance Risk for Infection Altered Comfort: Pain Altered Nutritional: Less than Body Requirements (more Calories needed) • Body Image Change : Loss? : Role?
Nursing Care • IV access (Multiple) • Manage perfusion needs by parameters of CVP, Urinary Output • Pain management – once vital signs have stabilized, pain medication should be used (ie morphine, or meperidine, fentanyl, benzodiazepines as indicated ) – Morphine or Fentanyl Drip
Nursing Care of Ulcer/Pain/Tetanus • Curlings ulcer prophylaxis (Peptic Ulcer) – An H 2 blocker (cimetidine, ranitidine, famotidine) start first 6 hours – antacids are no longer recommended - the patient should be kept NPO – with burns > 15% of BSA, an NG (OG) tube and bladder catheter should be placed • Tetanus – immunization if out of date
Nursing Care of Burn Wounds • Wound Care (Sterile Technique) – Debridement – Anti-microbial Application • silver sulfadiazine (Silvadine) • mafenide acetate (Sulfamylon) – Closed dressing except face & perineum – Wound cover • synthetic, biological – Graft • Wound Allograft • Split thickness skin graft • full thickness graft
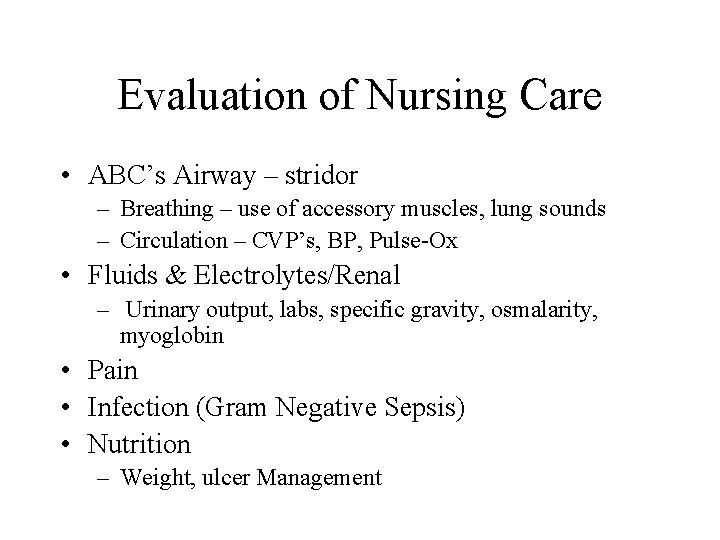
Evaluation of Nursing Care • ABC’s Airway – stridor – Breathing – use of accessory muscles, lung sounds – Circulation – CVP’s, BP, Pulse-Ox • Fluids & Electrolytes/Renal – Urinary output, labs, specific gravity, osmalarity, myoglobin • Pain • Infection (Gram Negative Sepsis) • Nutrition – Weight, ulcer Management
- Slides: 34