BURNS Burn Injury Tissue destruction can lead to

BURNS
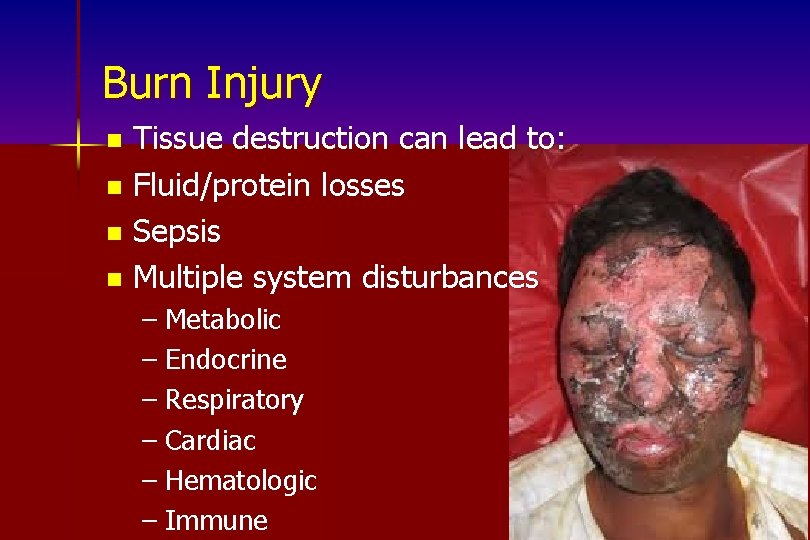
Burn Injury Tissue destruction can lead to: n Fluid/protein losses n Sepsis n Multiple system disturbances n – Metabolic – Endocrine – Respiratory – Cardiac – Hematologic – Immune
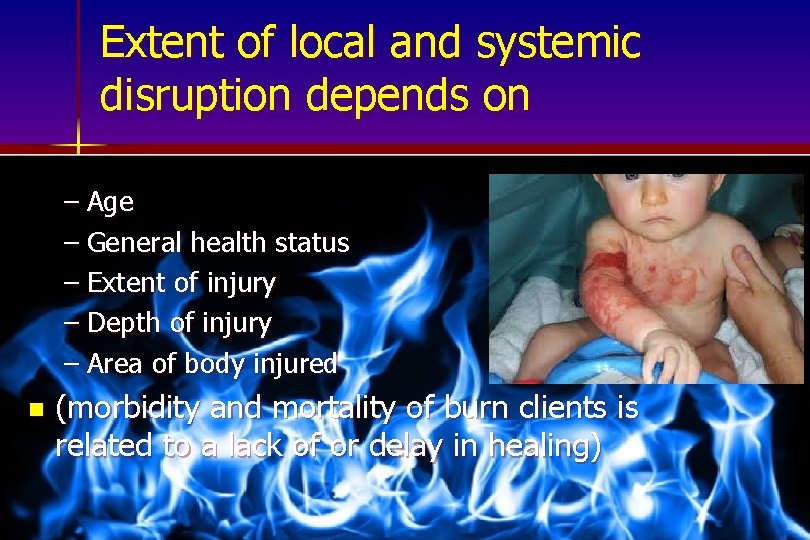
Extent of local and systemic disruption depends on – Age – General health status – Extent of injury – Depth of injury – Area of body injured n (morbidity and mortality of burn clients is related to a lack of or delay in healing)
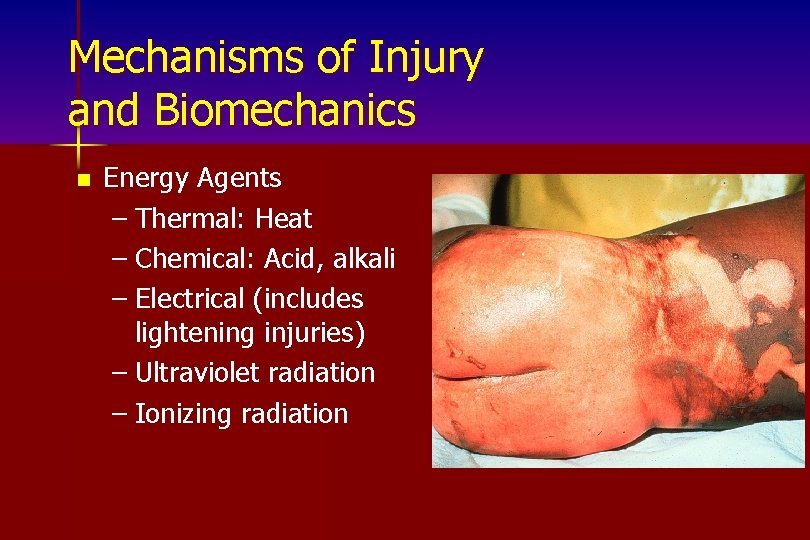
Mechanisms of Injury and Biomechanics n Energy Agents – Thermal: Heat – Chemical: Acid, alkali – Electrical (includes lightening injuries) – Ultraviolet radiation – Ionizing radiation
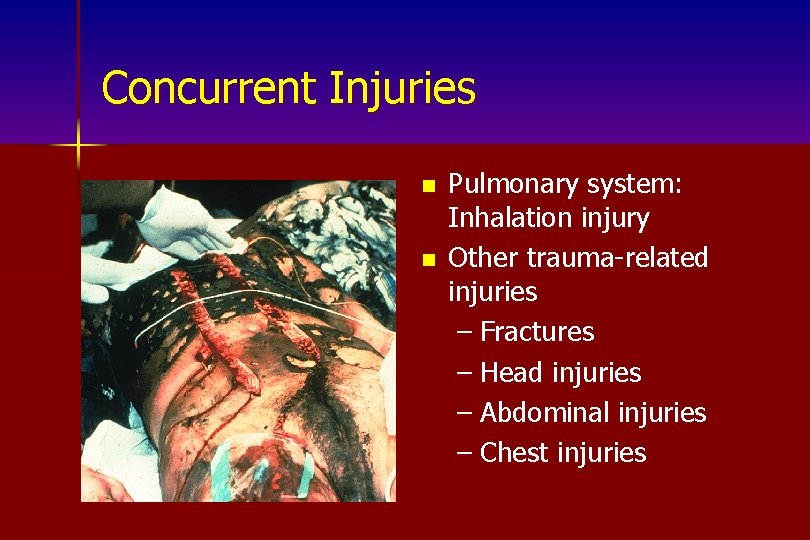
Concurrent Injuries n n Pulmonary system: Inhalation injury Other trauma-related injuries – Fractures – Head injuries – Abdominal injuries – Chest injuries
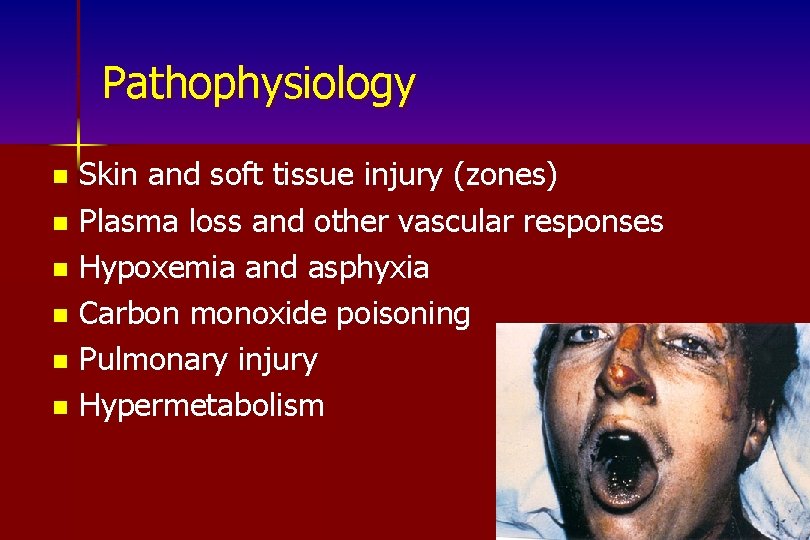
Pathophysiology Skin and soft tissue injury (zones) n Plasma loss and other vascular responses n Hypoxemia and asphyxia n Carbon monoxide poisoning n Pulmonary injury n Hypermetabolism n
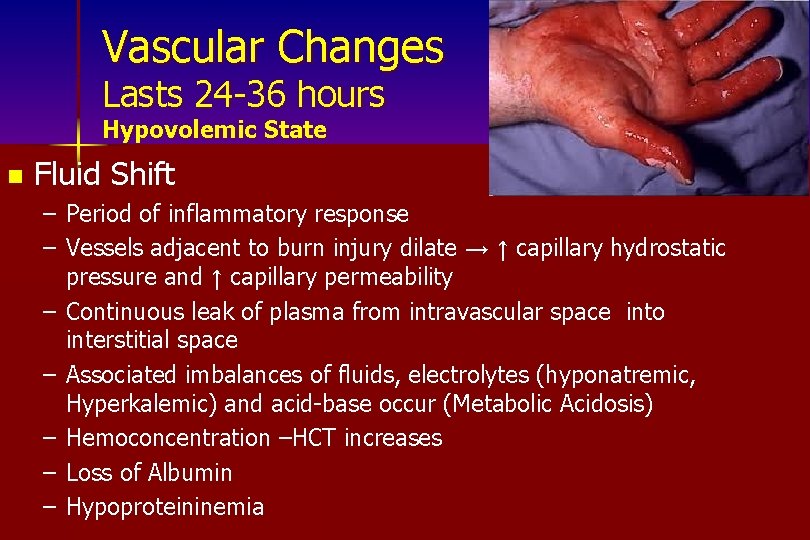
Vascular Changes Lasts 24 -36 hours Hypovolemic State n Fluid Shift – Period of inflammatory response – Vessels adjacent to burn injury dilate → ↑ capillary hydrostatic pressure and ↑ capillary permeability – Continuous leak of plasma from intravascular space into interstitial space – Associated imbalances of fluids, electrolytes (hyponatremic, Hyperkalemic) and acid-base occur (Metabolic Acidosis) – Hemoconcentration –HCT increases – Loss of Albumin – Hypoproteininemia
Diuretic Stage 48 -72 hours postburn Fluid remobilization Capillary leak ceases and fluid shifts back into the circulation n Restores fluid balance and renal perfusion n – Increased urine formation and diuresis; HCO 3 lost in Urine n Continued electrolyte imbalances – Hyponatremia – Hypokalemia n Hemodilution –low HCT, decr K+ (moves back or excreted) n FLUID OVERLOAD !!!! Watch for it!!!!
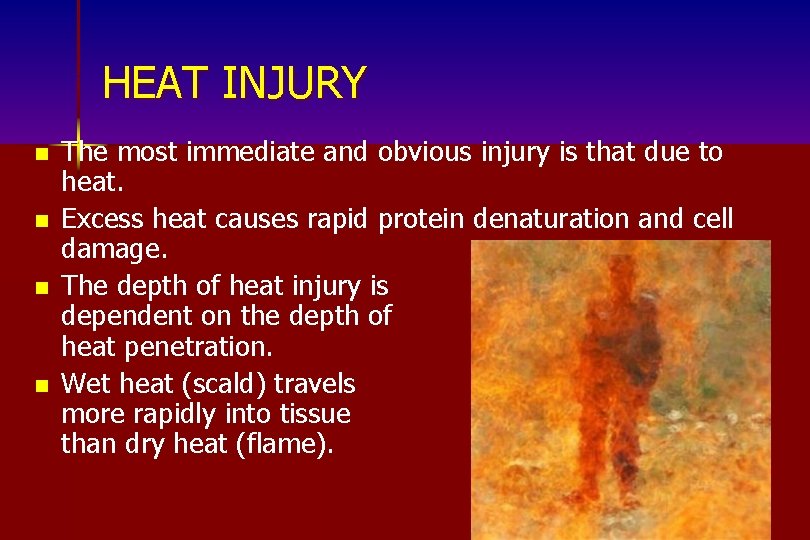
HEAT INJURY n n The most immediate and obvious injury is that due to heat. Excess heat causes rapid protein denaturation and cell damage. The depth of heat injury is dependent on the depth of heat penetration. Wet heat (scald) travels more rapidly into tissue than dry heat (flame).
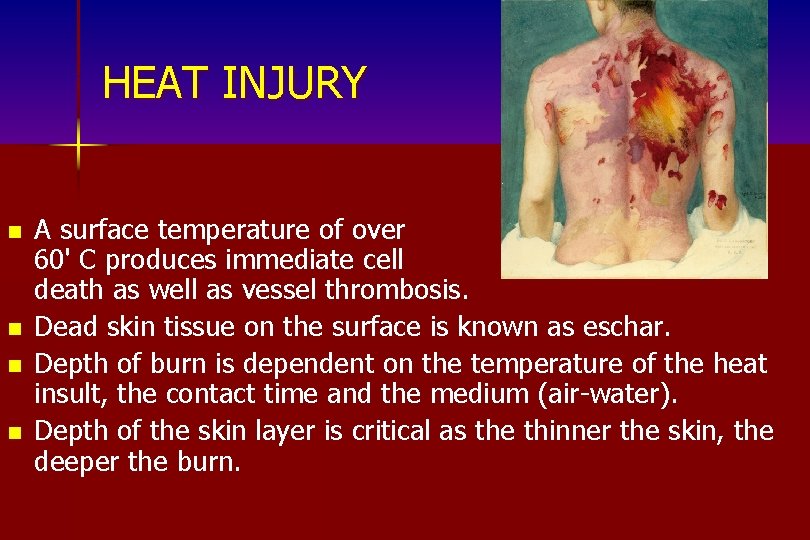
HEAT INJURY n n A surface temperature of over 60' C produces immediate cell death as well as vessel thrombosis. Dead skin tissue on the surface is known as eschar. Depth of burn is dependent on the temperature of the heat insult, the contact time and the medium (air-water). Depth of the skin layer is critical as the thinner the skin, the deeper the burn.

n The inflammatory response initiated by the heat injury is responsible for further early tissue damage, increased capillary permeability and in large part responsible for the later wound conversion if inflammation becomes excessive.
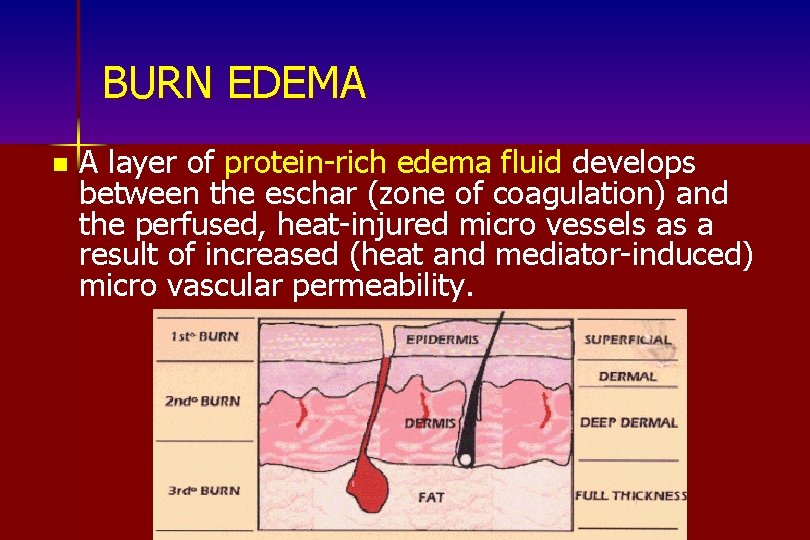
BURN EDEMA n A layer of protein-rich edema fluid develops between the eschar (zone of coagulation) and the perfused, heat-injured micro vessels as a result of increased (heat and mediator-induced) micro vascular permeability.
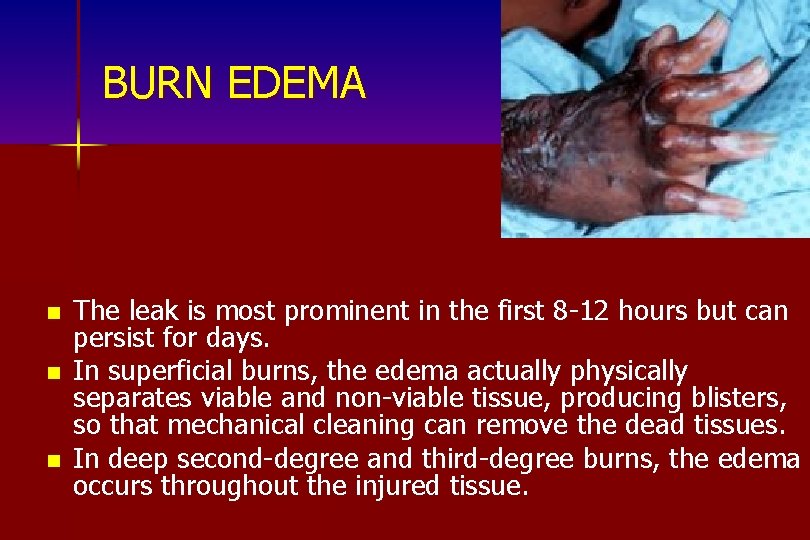
BURN EDEMA n n n The leak is most prominent in the first 8 -12 hours but can persist for days. In superficial burns, the edema actually physically separates viable and non-viable tissue, producing blisters, so that mechanical cleaning can remove the dead tissues. In deep second-degree and third-degree burns, the edema occurs throughout the injured tissue.
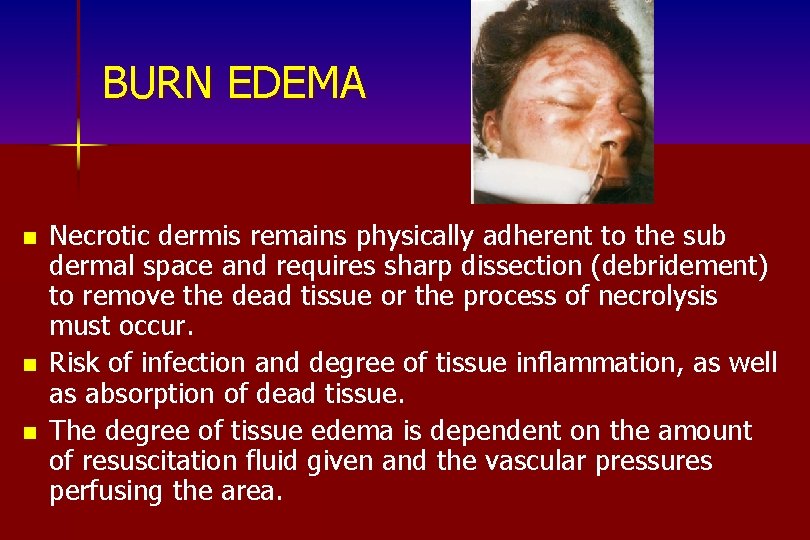
BURN EDEMA n n n Necrotic dermis remains physically adherent to the sub dermal space and requires sharp dissection (debridement) to remove the dead tissue or the process of necrolysis must occur. Risk of infection and degree of tissue inflammation, as well as absorption of dead tissue. The degree of tissue edema is dependent on the amount of resuscitation fluid given and the vascular pressures perfusing the area.
INFLAMMATION INDUCED WOUND INJURY Protease Release Injuring Healing Tissue and Deactivating Growth Factors n Oxidants Release Injuring Cells, Denaturing Proteins, and Activating Inflammation n Consumption of Wound Oxygen by Neutrophils Leading to Tissue Hypoxia n Increasing Stimulus to Fibrosis n
ISCHEMIA INDUCED INJURY n n Instant surface vascular thrombosis occurs along with cell death from the heat insult. Ischemia does not play a role in the initial surface necrosis. However, the injured capillaries below the surface, where tissue is still viable, can continue to thrombose due to initial heat and subsequent mediator injury, to endothelial cells, causing further ischemia and further tissue necrosis. Systemic hypovolemia or local impairment in perfusion due to constricting eschar or edema will produce the same effect.
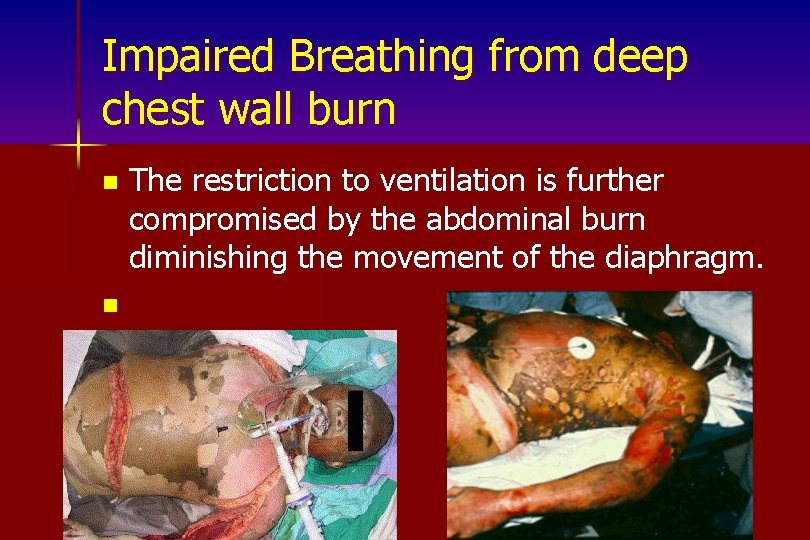
Impaired Breathing from deep chest wall burn n n The restriction to ventilation is further compromised by the abdominal burn diminishing the movement of the diaphragm.
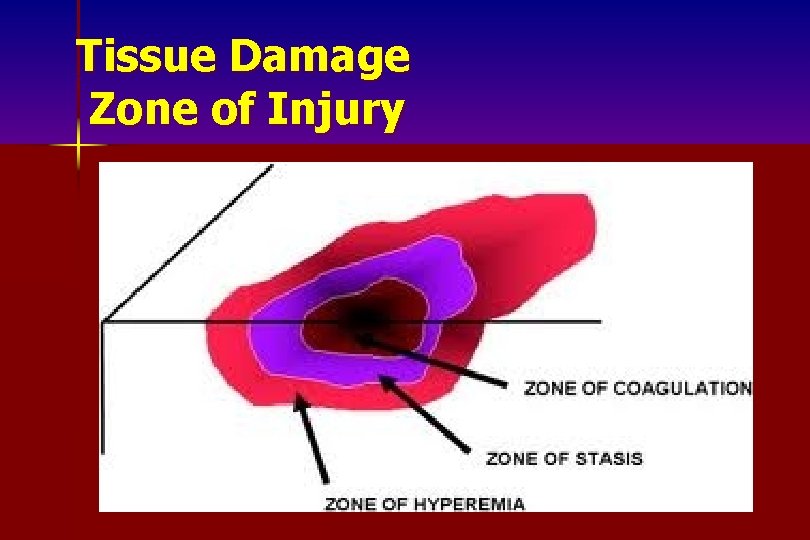
Tissue Damage Zone of Injury
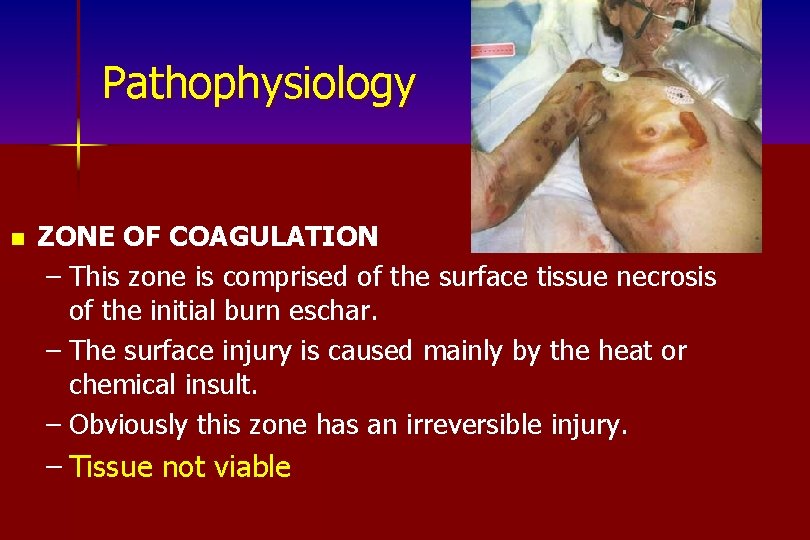
Pathophysiology n ZONE OF COAGULATION – This zone is comprised of the surface tissue necrosis of the initial burn eschar. – The surface injury is caused mainly by the heat or chemical insult. – Obviously this zone has an irreversible injury. – Tissue not viable
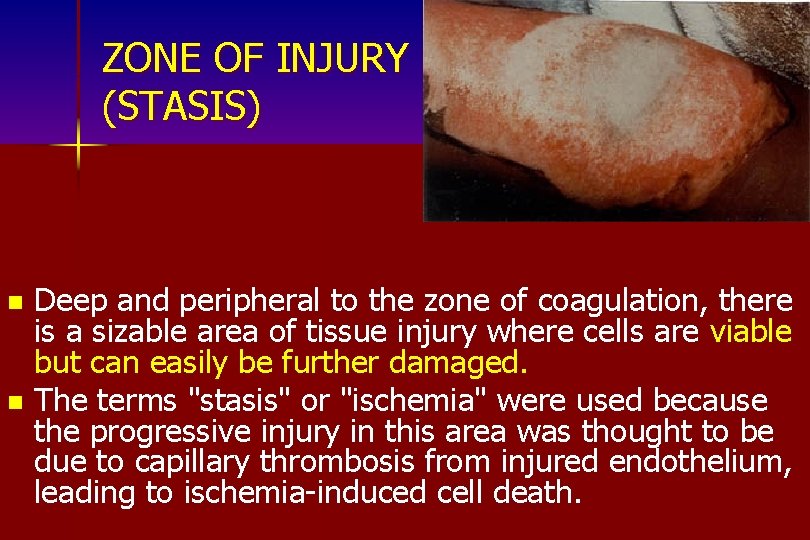
ZONE OF INJURY (STASIS) Deep and peripheral to the zone of coagulation, there is a sizable area of tissue injury where cells are viable but can easily be further damaged. n The terms "stasis" or "ischemia" were used because the progressive injury in this area was thought to be due to capillary thrombosis from injured endothelium, leading to ischemia-induced cell death. n
ZONE OF INJURY (STASIS) Fibrin deposition, vasoconstriction, and thrombosis indeed do occur, most likely as a result of continued release of mediators. n However, early epithelial cell death in this area, unrelated to blood flow, is reported to be quite high, leading to slowing of healing. n Epithelial cells are particularly prone to environmental insults such as desiccation- and inflammation-induced injury. n This zone is most prominent in mid-to-deep-dermal burns where there is less reserve in the remaining viable cells and less blood flow. n
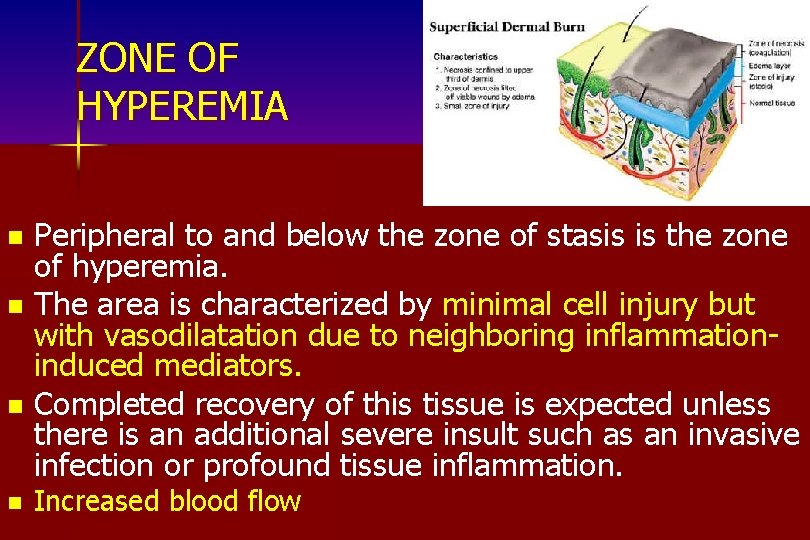
ZONE OF HYPEREMIA Peripheral to and below the zone of stasis is the zone of hyperemia. n The area is characterized by minimal cell injury but with vasodilatation due to neighboring inflammationinduced mediators. n Completed recovery of this tissue is expected unless there is an additional severe insult such as an invasive infection or profound tissue inflammation. n n Increased blood flow
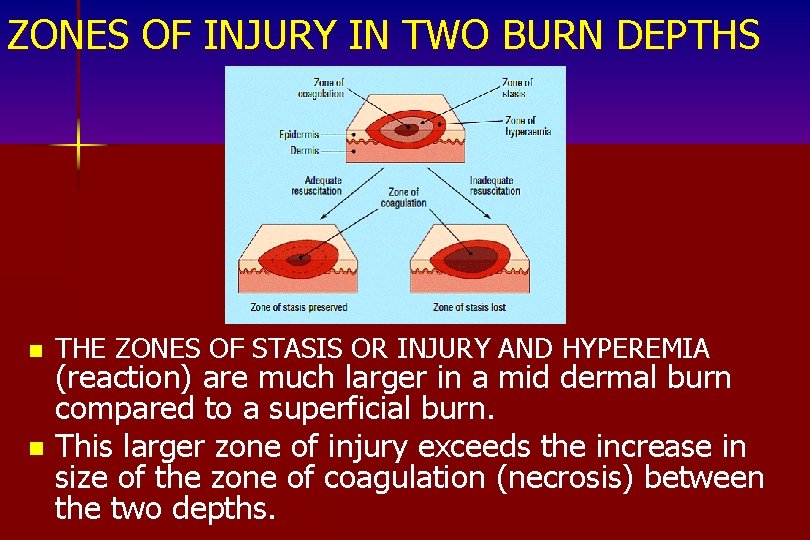
ZONES OF INJURY IN TWO BURN DEPTHS n THE ZONES OF STASIS OR INJURY AND HYPEREMIA (reaction) are much larger in a mid dermal burn compared to a superficial burn. n This larger zone of injury exceeds the increase in size of the zone of coagulation (necrosis) between the two depths.
Factors Increasing Zone of Injury lower blood flow with a deeper burn n increased risk of infection with deeper burn n presence of surface necrotic tissue n
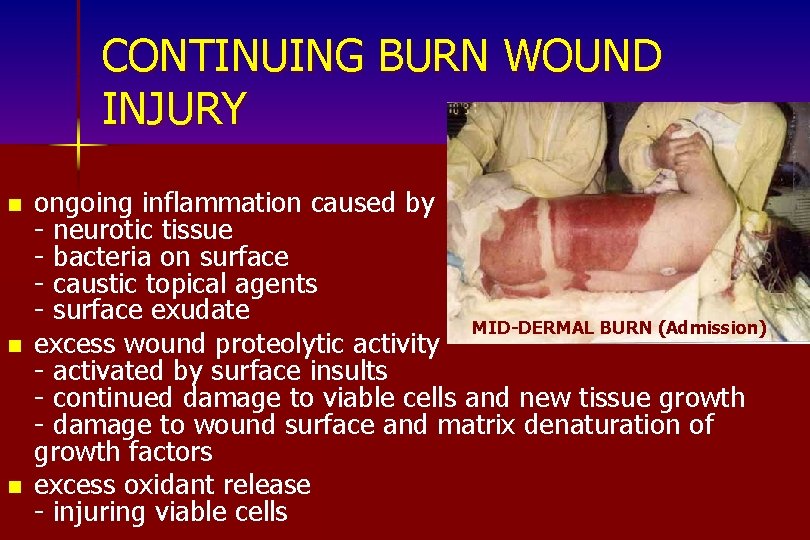
CONTINUING BURN WOUND INJURY n n n ongoing inflammation caused by - neurotic tissue - bacteria on surface - caustic topical agents - surface exudate MID-DERMAL BURN (Admission) excess wound proteolytic activity - activated by surface insults - continued damage to viable cells and new tissue growth - damage to wound surface and matrix denaturation of growth factors excess oxidant release - injuring viable cells

MID-DERMAL BURN (2 Days later)
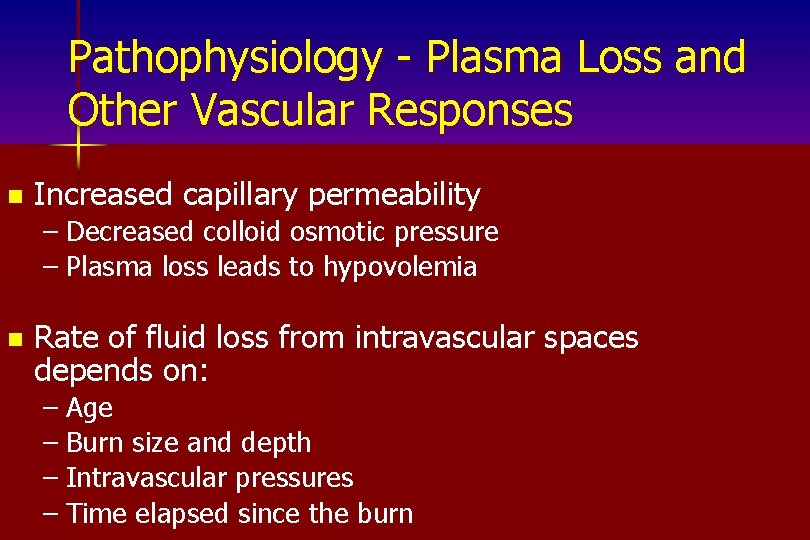
Pathophysiology - Plasma Loss and Other Vascular Responses n Increased capillary permeability – Decreased colloid osmotic pressure – Plasma loss leads to hypovolemia n Rate of fluid loss from intravascular spaces depends on: – Age – Burn size and depth – Intravascular pressures – Time elapsed since the burn
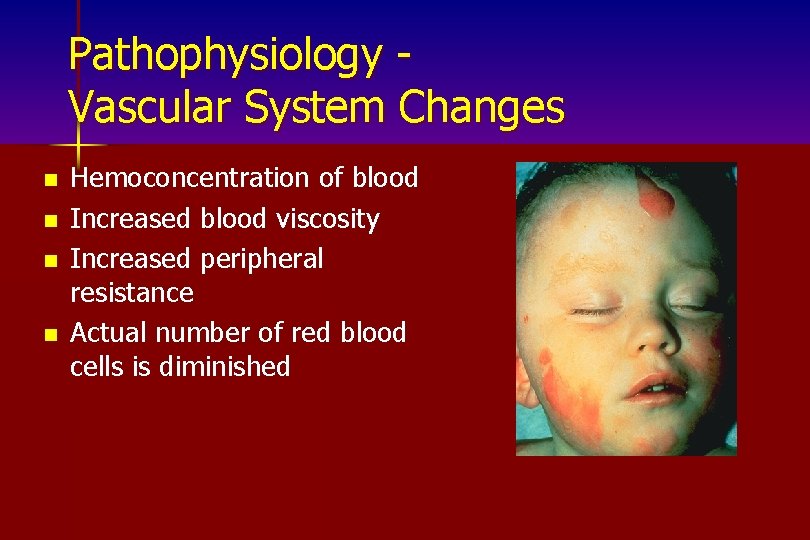
Pathophysiology Vascular System Changes n n Hemoconcentration of blood Increased blood viscosity Increased peripheral resistance Actual number of red blood cells is diminished
Pathophysiology Hypoxemia/Asphyxia Reduction in fraction of inspired oxygen leads to arterial hypoxemia n Asphyxia occurs when the blood has a decreased amount of oxygen and an increase in carbon dioxide in the blood and tissues n

Pathophysiology Carbon Monoxide Poisoning n n n Carbon monoxide is a tasteless, odorless, colorless gas that is present in the smoke of combustion of organic materials Carbon monoxide binds to oxygen binding sites on hemoglobin molecules; oxygen carrying capacity reduced Carbon monoxide also affects the cardiac muscle since it binds with myoglobin
Pathophysiology Pulmonary Injury n n Occurs when inhaled particles enter the lung Accumulation of debris and secretions results in: – Airway obstruction – Atelectasis – Impaired ciliary clearance n Sequelae: Pulmonary edema, pneumonia
Pathophysiology Hypermetabolism Increased basal metabolic rate due to autonomic nervous system response n Influences n – Age – Ambient temperature – Anxiety – Activity – Infection (late)
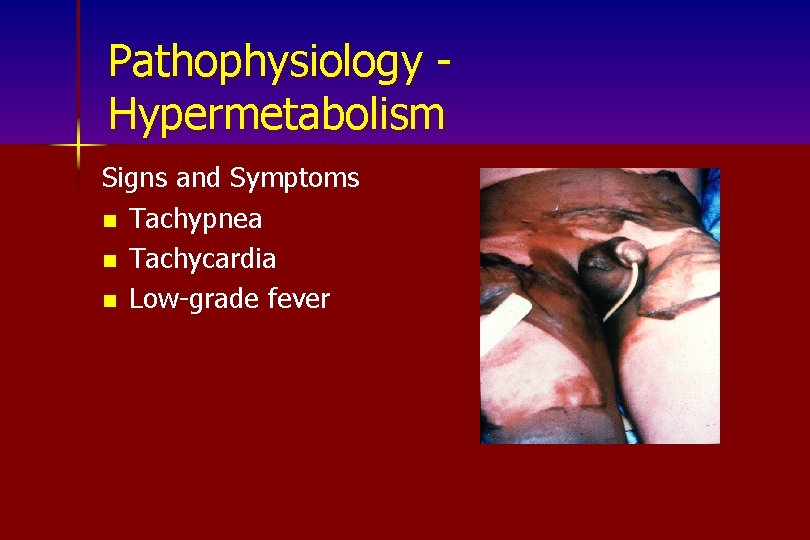
Pathophysiology Hypermetabolism Signs and Symptoms n Tachypnea n Tachycardia n Low-grade fever
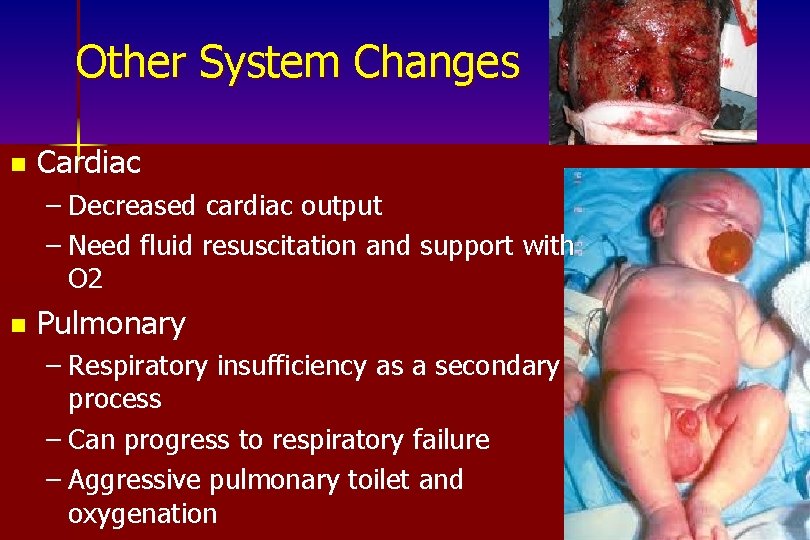
Other System Changes n Cardiac – Decreased cardiac output – Need fluid resuscitation and support with O 2 n Pulmonary – Respiratory insufficiency as a secondary process – Can progress to respiratory failure – Aggressive pulmonary toilet and oxygenation
Other System Changes n Gastrointestinal – Decreased or absent motility (may need NG tube) – Curling’s ulcer formation – H 2 histamine blockers, mucoprotectants and enteral nutrition
Other System Changes n Metabolic – Hypermetabolic state n Increased oxygen and calorie requirements n Increase in core body temperature n Immunologic – Loss of protective barrier – Increased risk of infection – Suppression of humoral and cell-mediated immune responses
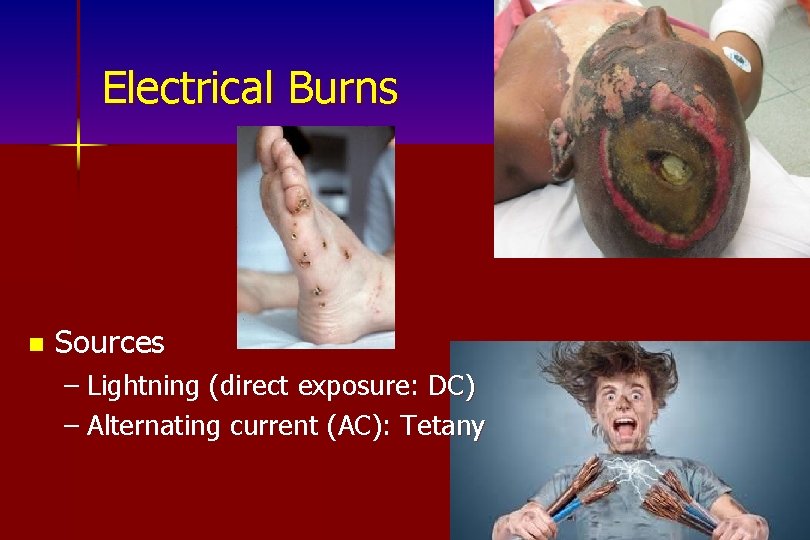
Electrical Burns n Sources – Lightning (direct exposure: DC) – Alternating current (AC): Tetany
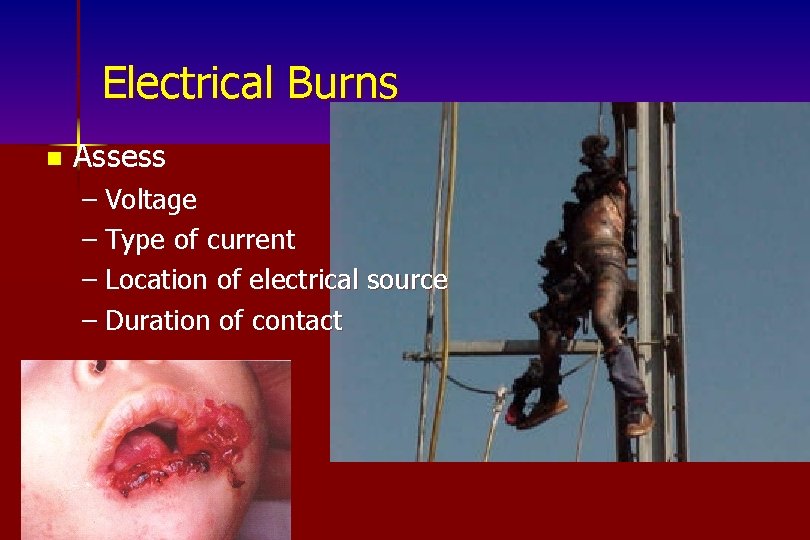
Electrical Burns n Assess – Voltage – Type of current – Location of electrical source – Duration of contact
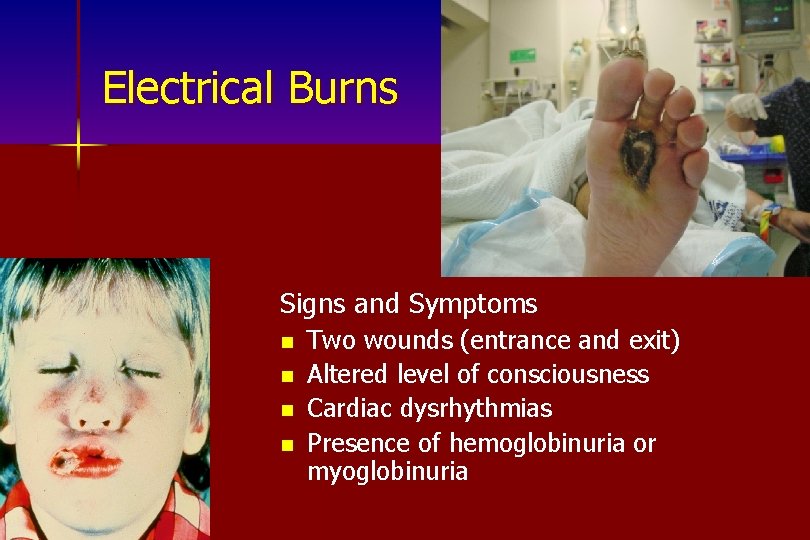
Electrical Burns Signs and Symptoms n n Two wounds (entrance and exit) Altered level of consciousness Cardiac dysrhythmias Presence of hemoglobinuria or myoglobinuria
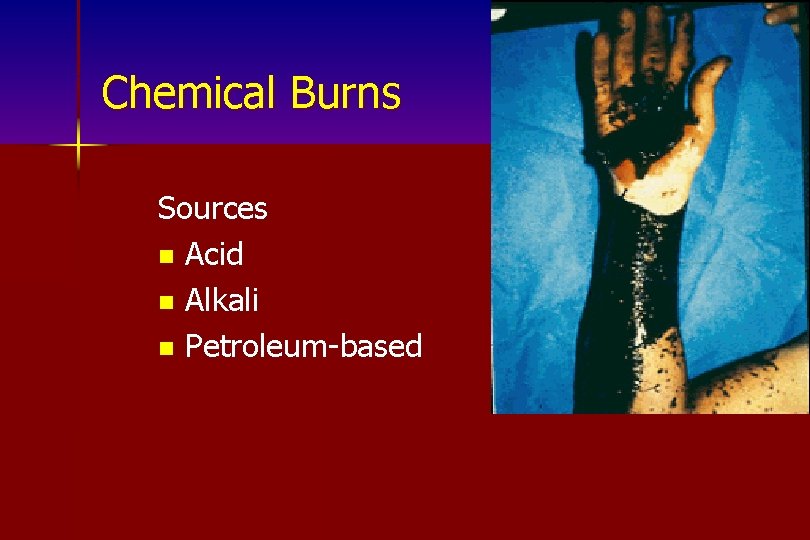
Chemical Burns Sources n Acid n Alkali n Petroleum-based

Chemical Burns Assess n Identify causes n Contact poison center n Extent of injury progression
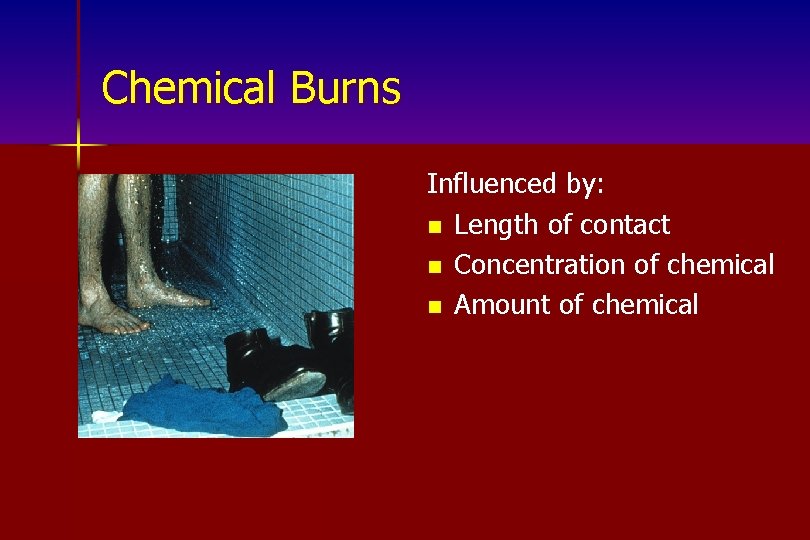
Chemical Burns Influenced by: n Length of contact n Concentration of chemical n Amount of chemical
Chemical Burns Signs and Symptoms n Erythema n Edema n Blisters n Tissue necrosis n Pain
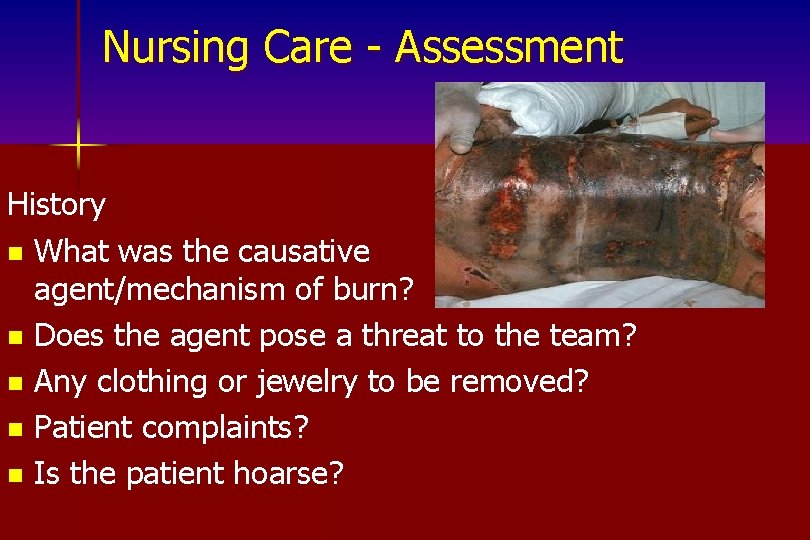
Nursing Care - Assessment History n What was the causative agent/mechanism of burn? n Does the agent pose a threat to the team? n Any clothing or jewelry to be removed? n Patient complaints? n Is the patient hoarse?
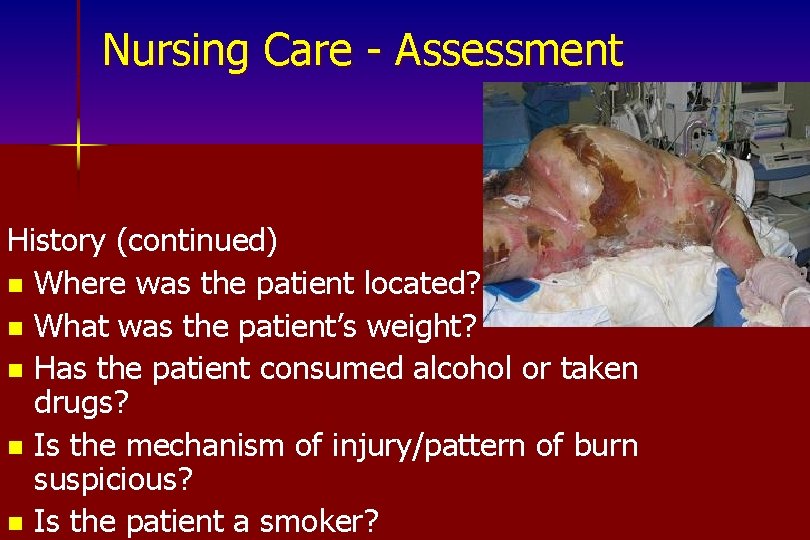
Nursing Care - Assessment History (continued) n Where was the patient located? n What was the patient’s weight? n Has the patient consumed alcohol or taken drugs? n Is the mechanism of injury/pattern of burn suspicious? n Is the patient a smoker?
Nursing Care Physical Assessment Inspection n Determine airway patency and breathing effectiveness n Nasopharynx and oropharynx n Singed nasal, facial, and eyebrow hairs
Nursing Care Physical Assessment Inspection (continued) n Burns and edema n Count respiratory rate, determine breathing pattern, watch expansion of chest during inspiration
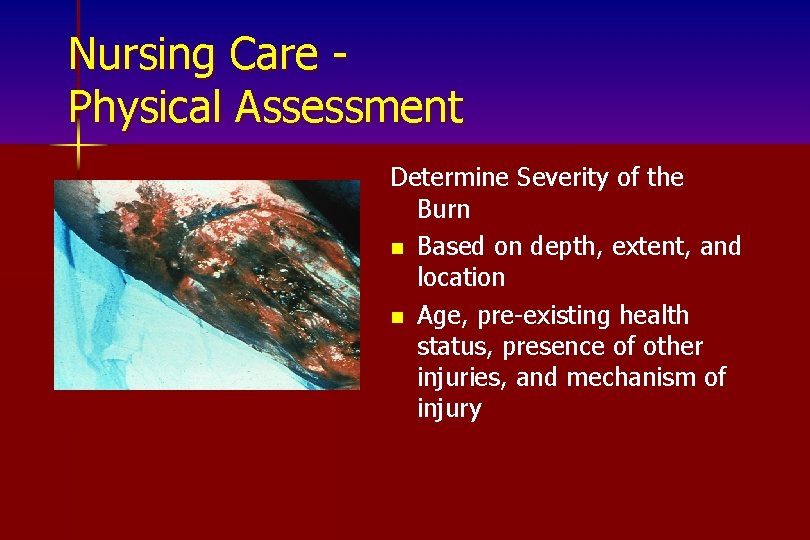
Nursing Care Physical Assessment Determine Severity of the Burn n Based on depth, extent, and location n Age, pre-existing health status, presence of other injuries, and mechanism of injury
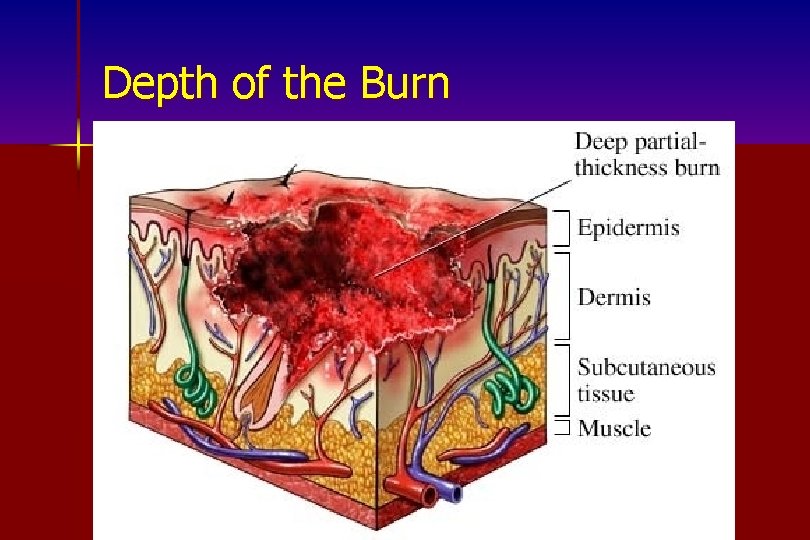
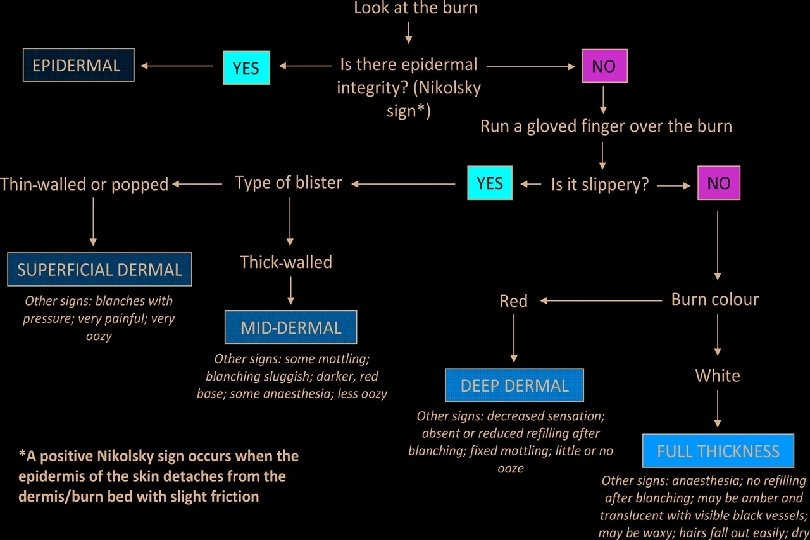
Depth of the Burn
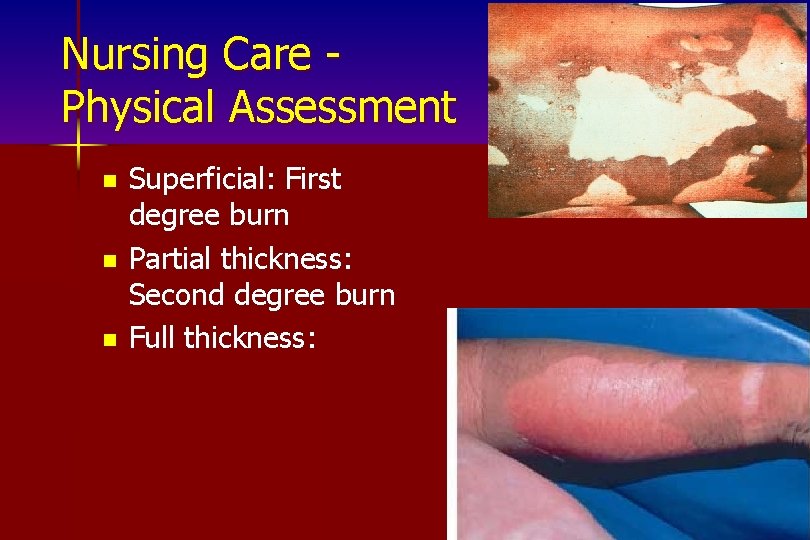
Nursing Care Physical Assessment n n n Superficial: First degree burn Partial thickness: Second degree burn Full thickness:

Depth of Burn n Superficial partial-thickness – Erythematous and moist with vesicles – painful n Deep partial-thickness – Red and waxy without blisters – Moderate edema, lesser degree of pain – Hypoxia and ischemia can cause extension of wound

PARTIAL THICKNESS BURN
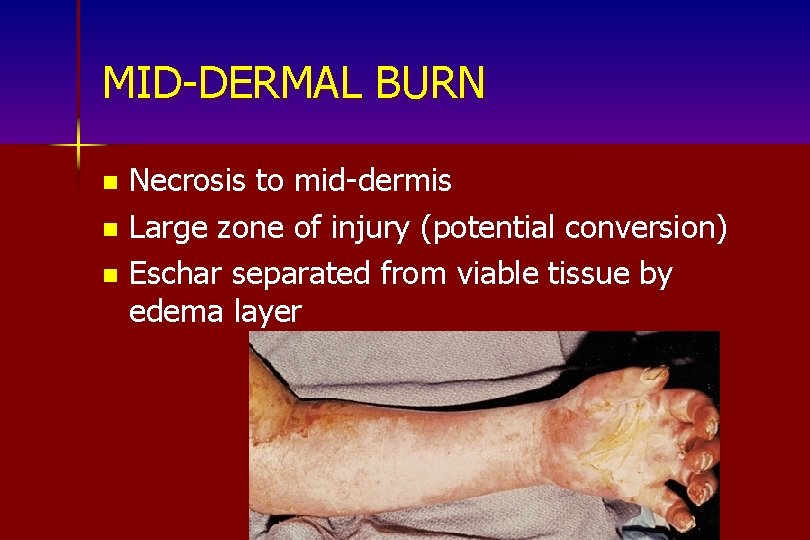
MID-DERMAL BURN Necrosis to mid-dermis n Large zone of injury (potential conversion) n Eschar separated from viable tissue by edema layer n

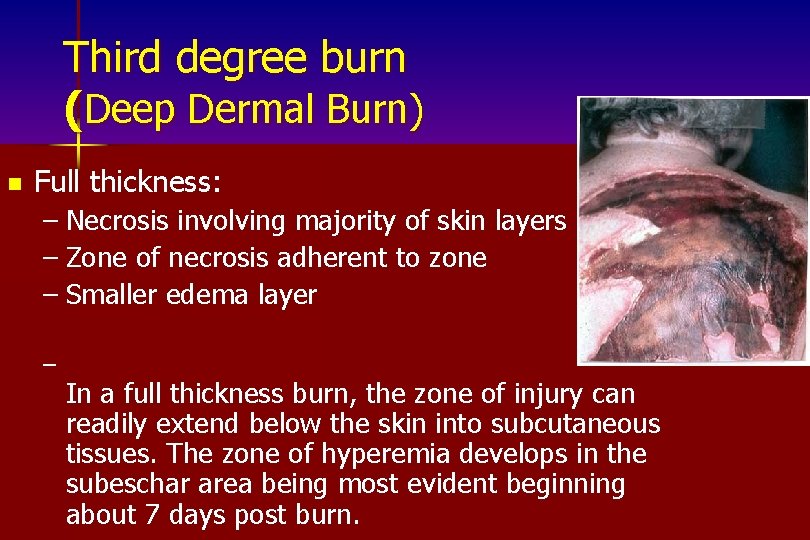
Third degree burn (Deep Dermal Burn) n Full thickness: – Necrosis involving majority of skin layers – Zone of necrosis adherent to zone – Smaller edema layer – In a full thickness burn, the zone of injury can readily extend below the skin into subcutaneous tissues. The zone of hyperemia develops in the subeschar area being most evident beginning about 7 days post burn.
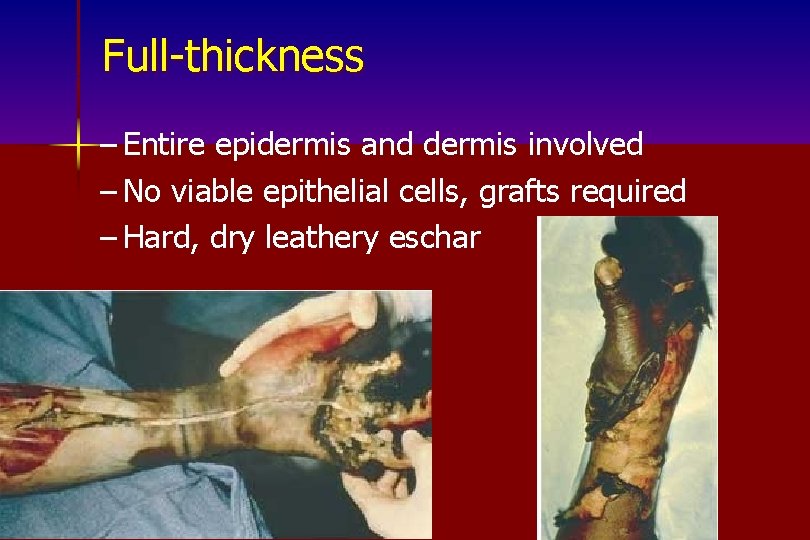
Full-thickness – Entire epidermis and dermis involved – No viable epithelial cells, grafts required – Hard, dry leathery eschar


Deep full-thickness – Extend beyond skin into underlying fascia and tissues – Muscle, bone and tendon damage with exposure to surface – Blackened and depressed, little or no sensation – Early excision and grafting beneficial
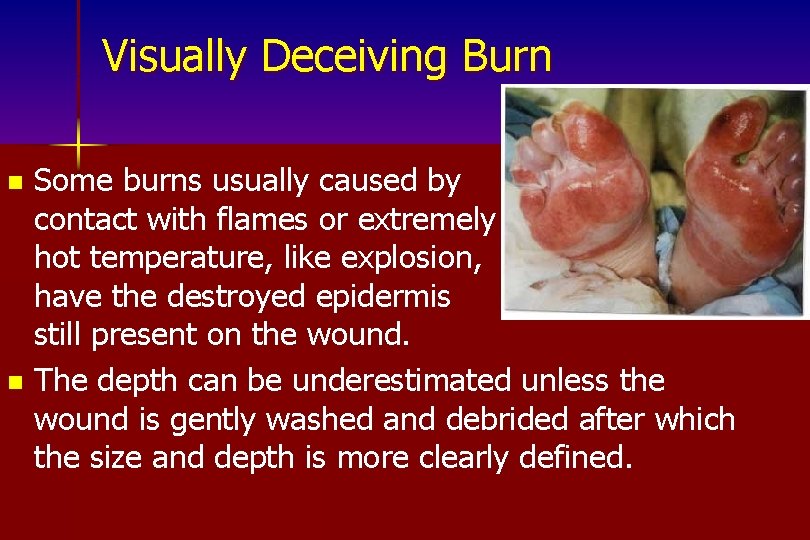
Visually Deceiving Burn Some burns usually caused by contact with flames or extremely hot temperature, like explosion, have the destroyed epidermis still present on the wound. n The depth can be underestimated unless the wound is gently washed and debrided after which the size and depth is more clearly defined. n
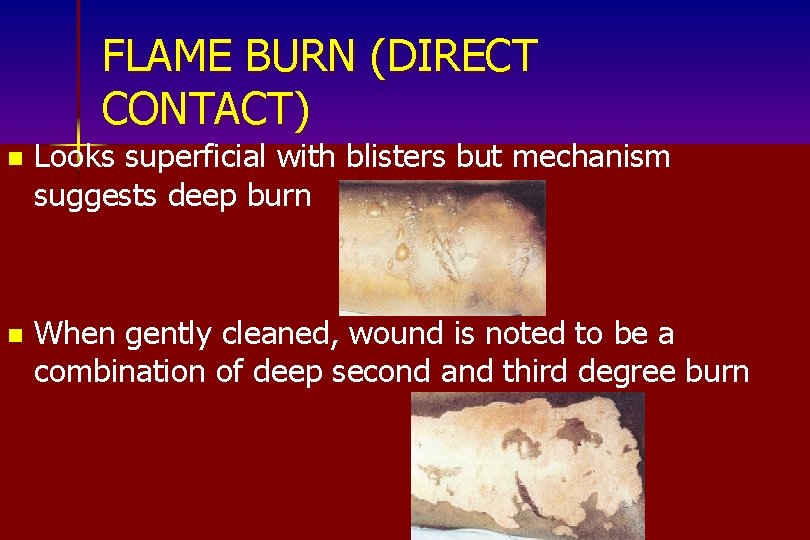
FLAME BURN (DIRECT CONTACT) n Looks superficial with blisters but mechanism suggests deep burn n When gently cleaned, wound is noted to be a combination of deep second and third degree burn
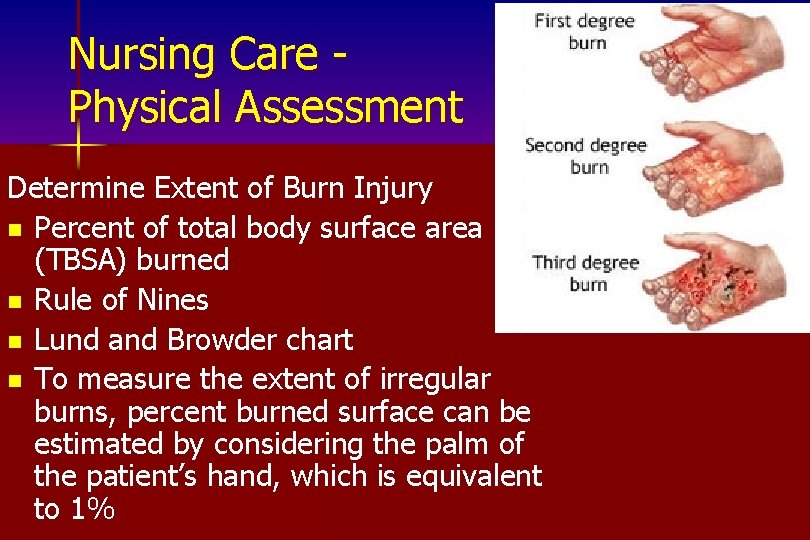
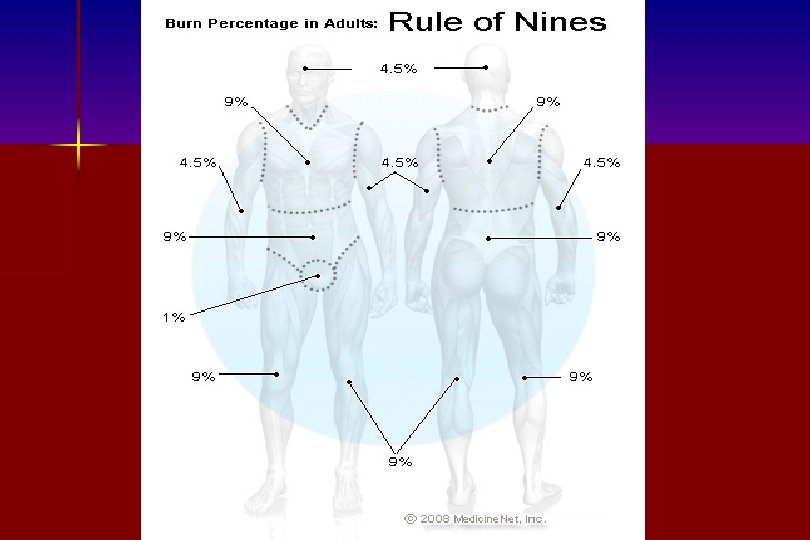
Nursing Care Physical Assessment Determine Extent of Burn Injury n Percent of total body surface area (TBSA) burned n Rule of Nines n Lund and Browder chart n To measure the extent of irregular burns, percent burned surface can be estimated by considering the palm of the patient’s hand, which is equivalent to 1%

The Rule of Nines
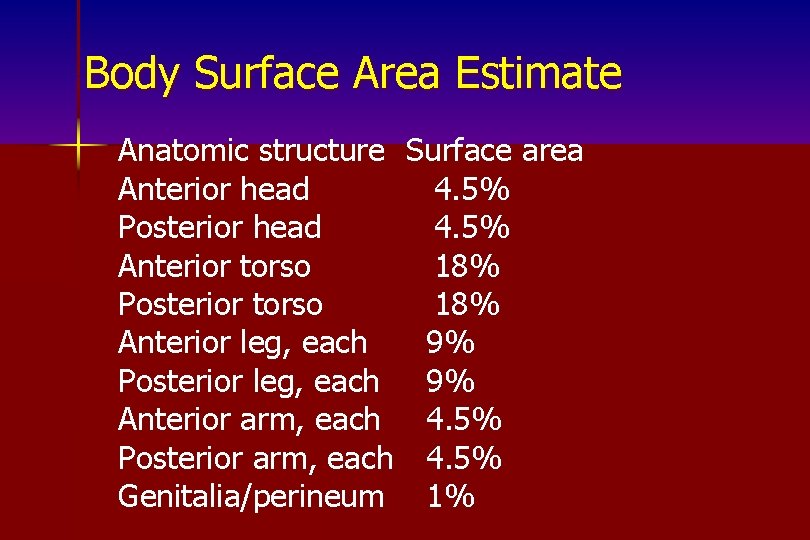
Body Surface Area Estimate Anatomic structure Surface area Anterior head 4. 5% Posterior head 4. 5% Anterior torso 18% Posterior torso 18% Anterior leg, each 9% Posterior leg, each 9% Anterior arm, each 4. 5% Posterior arm, each 4. 5% Genitalia/perineum 1%
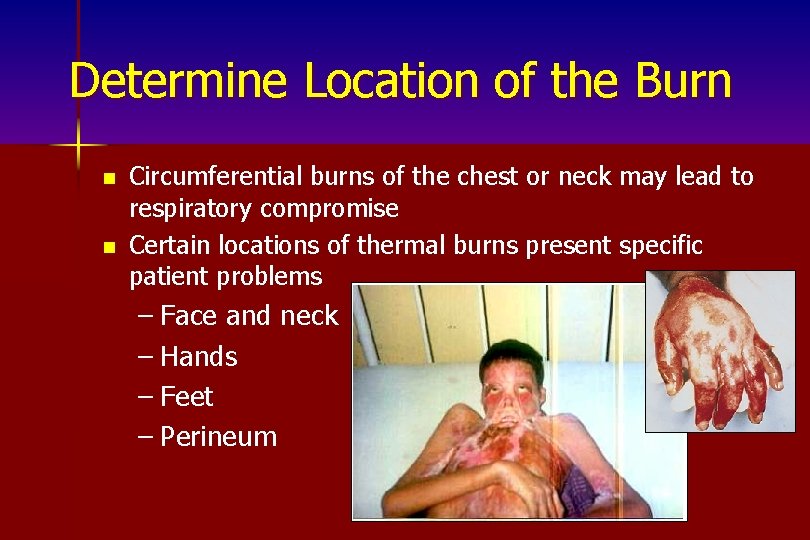
Determine Location of the Burn n n Circumferential burns of the chest or neck may lead to respiratory compromise Certain locations of thermal burns present specific patient problems – Face and neck – Hands – Feet – Perineum
Nursing Care Physical Assessment Auscultation n Breath sounds n Pulses in burned digits with a Doppler Ultrasonic Flow Meter
Nursing Care Physical Assessment Palpation n Peripheral pulses n Extremities to determine sensory function and neurovascular compromise n Feel temperature of the skin to determine peripheral perfusion status
Diagnostic Procedures n n n Radiographic Studies – Chest Laboratory Studies – Arterial blood gases, carboxyhemoglobin, p. H, and Sa. O 2 – Urinalysis, hemoglobin, myoglobin Other – Pulse oximetry – Fiberoptic, flexible bronchoscopy
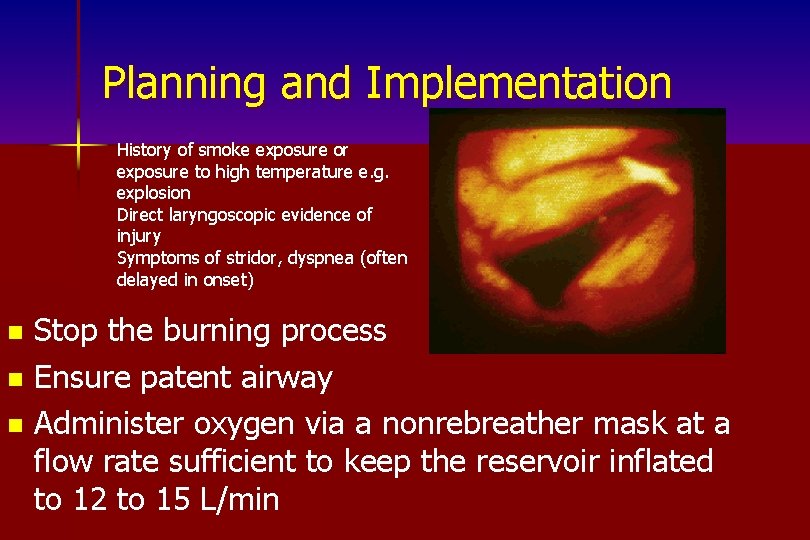
Planning and Implementation History of smoke exposure or exposure to high temperature e. g. explosion Direct laryngoscopic evidence of injury Symptoms of stridor, dyspnea (often delayed in onset) Stop the burning process n Ensure patent airway n Administer oxygen via a nonrebreather mask at a flow rate sufficient to keep the reservoir inflated to 12 to 15 L/min n
Planning and Implementation n Assist ventilation (positive end expiratory pressure or continuous positive airway pressure) Cannulate 2 veins with large bore 14 - or 16 -gauge catheters and initiate infusion of a warmed intravenous solution Infuse 2 to 4 ml/kg x % of TBSA burned – Give within the first 24 hours – Give 1/2 in the first 8 hours postburn
Fluid Resuscitation Protocol n n n n Establish and maintain adequate Circulation Burns >20% TBS require initial fluid resuscitation Use at least one large bore intravenous catheter. Begin Ringer’s Lactate. Estimate initial rate according to the estimated percent of total body skin surface burned (%TBS). Estimated body weight 2 cc-4 cc/kg/%TBS burn in 24 hours giving half of the estimate in first 8 hours, remaining last 16 hours
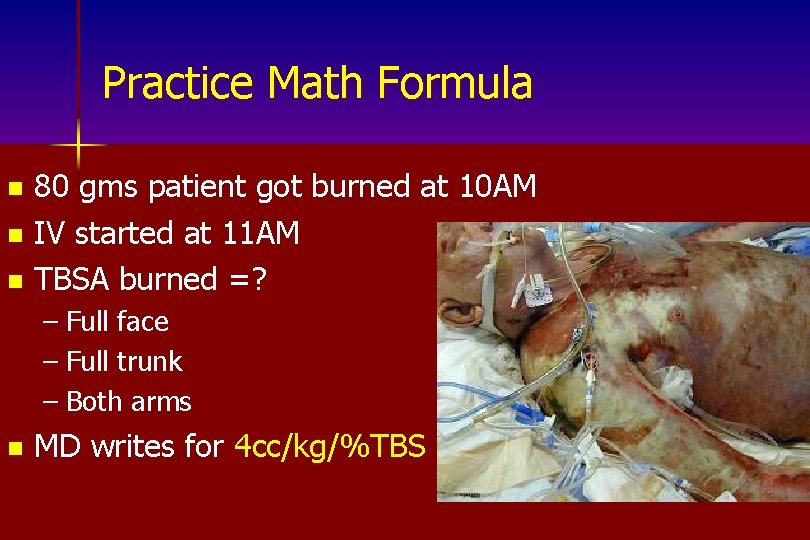
Practice Math Formula 80 gms patient got burned at 10 AM n IV started at 11 AM n TBSA burned =? n – Full face – Full trunk – Both arms n MD writes for 4 cc/kg/%TBS
Fluid Resuscitation Protocol n n n Foley catheter- Nasogastric tube Maintain: Blood Pressure>90 systolic Urine output 0. 5 -1. 0 ml/kg/hr Pulse <130 Temperature >37°C Modify protocol in the presence of massive burns, inhalation injury, shock, and in elderly patients: Fluid requirements are greater to prevent burn shock- Include colloid: either Hespan or Albumin in the patients from the beginning
Planning and Implementation n n n Administer analgesic medications Insert an indwelling catheter Insert a gastric tube Apply cool, saline-moistened, sterile dressings to TBSA burns < 10% Cover burns > 10% TBSA with a clean, dry sheet Keep the patient warm
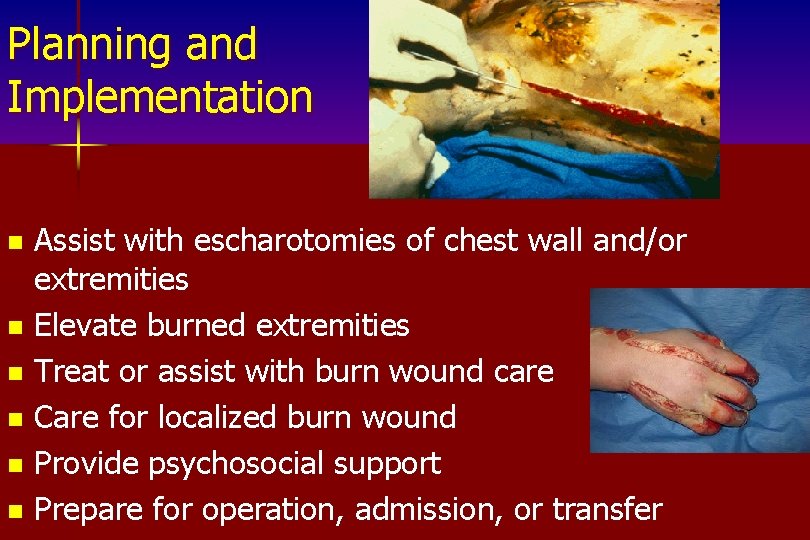
Planning and Implementation Assist with escharotomies of chest wall and/or extremities n Elevate burned extremities n Treat or assist with burn wound care n Care for localized burn wound n Provide psychosocial support n Prepare for operation, admission, or transfer n
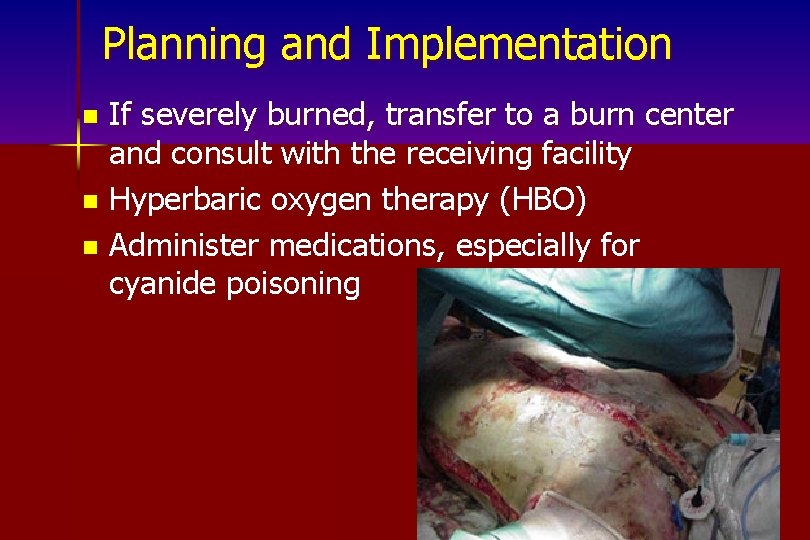
Planning and Implementation If severely burned, transfer to a burn center and consult with the receiving facility n Hyperbaric oxygen therapy (HBO) n Administer medications, especially for cyanide poisoning n
Interventions n Non-surgical n Ineffective Breathing Pattern – Airway maintenance – Promotion of ventilation – Monitoring gas exchange – Oxygen therapy – Drug therapy – Positioning and deep breathing n Surgical – Tracheostomy – Chest tubes – escharotomy
Acute Pain Interventions: n Non-surgical n – Drug therapy (opioids) (anesthetic agents) – Complimentary/alternative therapies – Environmental manipulation n Surgical – Early surgical excision of burn wound

Impaired Skin Integrity Wound Care Management Non-surgical n Debridement n – Mechanical – Enzymatic Cleaning n Stimulating granulation and revascularization n Dressings n
n Standard Dressings – Multiple gauze layers over topical agent or antibiotic Biologic n Homograft (allograft) from cadaver n – Heterograft (xenograft) from animal (pig) – Amniotic membrane – Cultured skin n Artificial skin – Two-layer product which creates an artificial dermis n Synthetic dressing – Solid silicone and plastic membrane – Can see through to monitor wound status
Risk for Infection n Non-surgical management – Drug therapy n Tetanus Toxoid and Topical Antimicrobials n Organism specific drugs Isolation n Environmental manipulation n Secondary prevention/early detection n Surgical management n – Aggressive surgical incision of infected wound
Additional Interventions n Imbalanced Nutrition – Calculate calorie needs and provide adequate calories and nutrients – Calorie requirements can exceed 5000 per day n Impaired mobility – Interventions to maintain pre-burn ROM and prevent contractures n Disturbed Body Image – Grief counseling – Encouraging independence
Nursing Interventions for an Electrical Burn n n Monitor p. H, Pa. O 2, Pa. CO 2, Sp. O 2, bicarbonate Infuse intravenous fluids at 70 to 100 ml/hr Observe color of urine for myoglobin Monitor cardiac rate and rhythm Monitor for signs and symptoms of compartment syndrome
Nursing Interventions for a Chemical Burn n n n Assure protection of trauma team Irrigate burned area Do not waste time identifying agent Phenol should be irrigated with water Hydrofluoric burns: Topical application of 5% calcium gluconate-based gel Cool tar/asphalt burns and use petroleum products
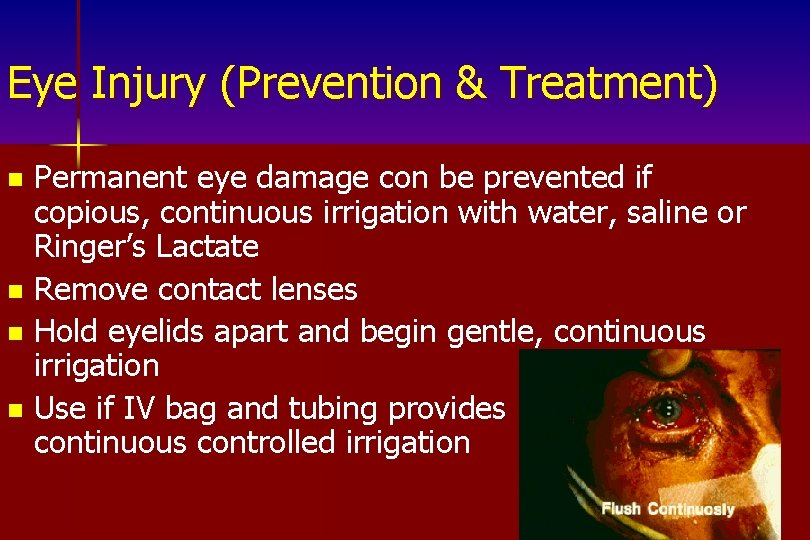
Eye Injury (Prevention & Treatment) Permanent eye damage con be prevented if copious, continuous irrigation with water, saline or Ringer’s Lactate n Remove contact lenses n Hold eyelids apart and begin gentle, continuous irrigation n Use if IV bag and tubing provides continuous controlled irrigation n
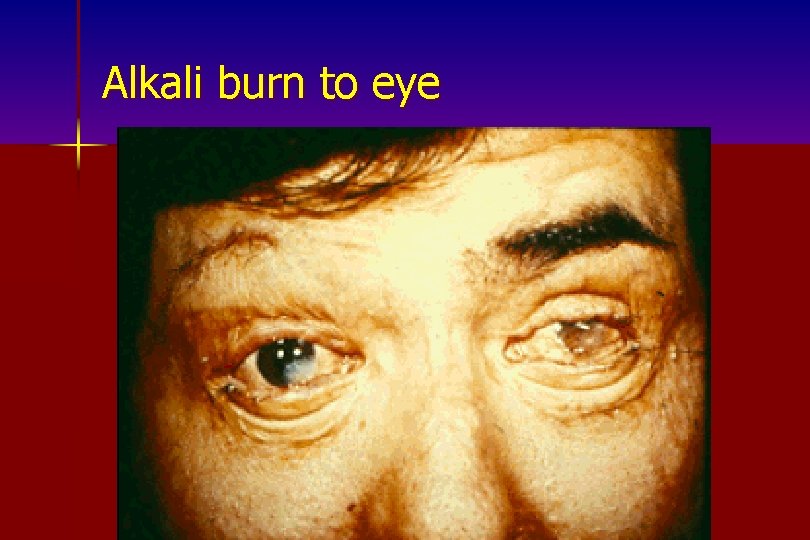
Alkali burn to eye
Evaluation and Ongoing Assessment Monitor pulmonary status n Monitor urinary output n Assess peripheral circulation n Assess progression of edema formation n
Burn injuries that should be referred to a burn unit includes the following: n n n Partial thickness burns greater than 10% total body surface area (TBSA). Burns that involve the face, genitalia, perineum or major joints Third degree burns in any age group. Electrical burns including lightening injury Chemical burns including lightening injury Inhalation injury. Children with any of the above burn injuries.
Burn injuries that should be referred to a burn unit includes the following: n n n pre-existing medical disorders that could complicate management. traumatic injury (such as fractures) in which the burn injury poses the greatest risk of morbidity or mortality. If the trauma poses the greater immediate risk, then the patient must be initially stabilized in the nearest appropriate facility before being transferred to a burn unit. Any burned children if the hospital initially receiving the patient does not have qualified personnel or equipment for children.
Emergent Phase n Goals: – Maintain open airway – Ensure adequate breathing/circulation – Limit extent of injury – Maintain function of vital organs – Prevent potential complications
Acute Phase n Interventions aimed at: – Maintenance of cardiovascular/respiratory system – Nutritional status – Burn wound care – Pain control – Psychosocial interventions
Rehabilitative Phase n Emphasis: – Psychological adjustment of client – Prevention of scars and contractures – Resumption of pre-burn activity Work n Family n Social n
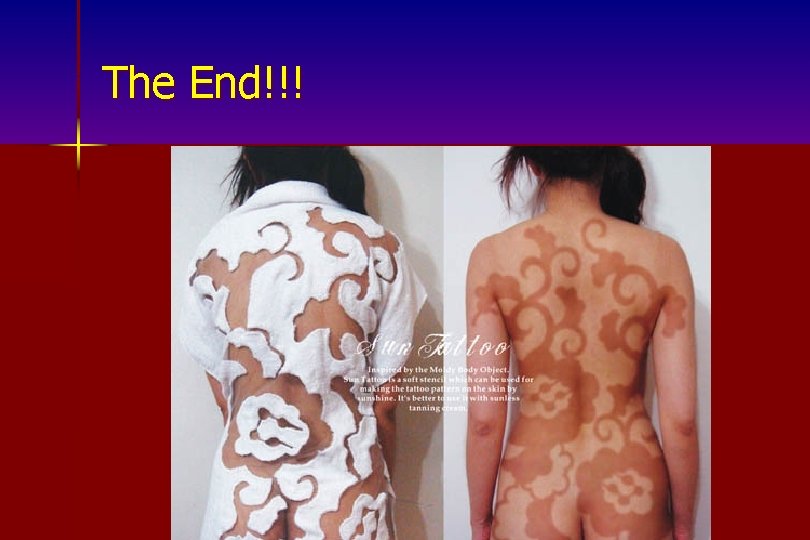
The End!!!
Recapping …….
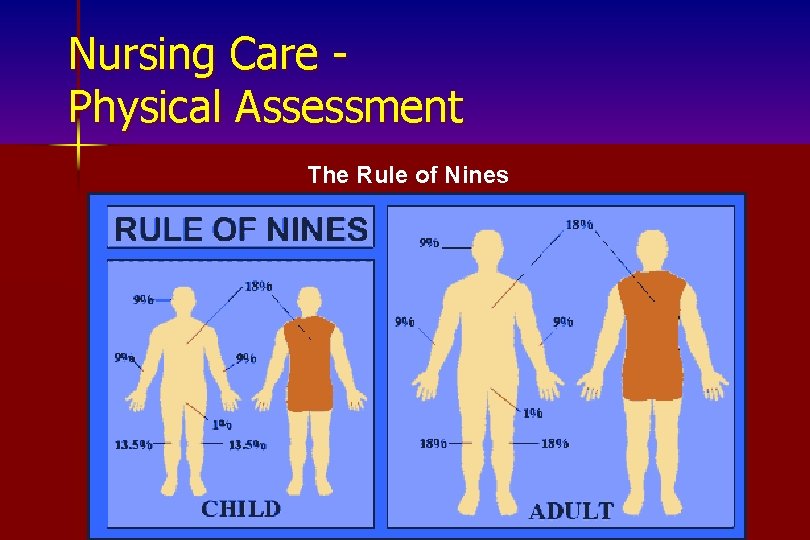
Nursing Care Physical Assessment The Rule of Nines
Clinical Manifestations of Burns n Respiratory – Direct airway injury – Carbon monoxide poisoning – Thermal injury – Smoke poisoning – Pulmonary fluid overload – External factors n Cardiovascular – Hypovolemic shock and ↓ cardiac output – Impaired circulation/tissue perfusion – Potential for ECG changes
n Renal/urinary – Changes R/T ↓ renal perfusion and debris – Fluid shift– ↓ GFR and urine output – Fluid remobilization– ↑ GFR and diuresis – Tubular blockage from myoglobin and uric acid – Fluid resuscitation should maintain output at 30 -50 m. L/hour n Integumentary – Size of injury is important to diagnosis and prognosis n “Rule of Nines” n Lund-Browder method – Specific treatments dependent upon depth of injury
Compensatory Responses n Inflammatory Compensation – Initiates healing – Contributes to fluid shift (↑ capillary permeability) – Local tissue reaction due to release of chemicals by wbc’s n Sympathetic Nervous System Compensation – Stress Response
Treatment Decreased CO, Deficient Fluid Volume, & Ineffective Tissue Perfusion n Interventions: n Non-surgical n – IV fluid therapy – Plasma exchange – Drug therapy n Surgical – Escharotomy
Phases of Burn Injury n Emergent – First 48 hours n Acute – Approximately 48 hours after injury to complete wound closure n Rehabilitative – Begins with wound closure and ends when client returns to highest possible level of functioning
- Slides: 101