BULLOUS DISEASES Vesicles and bullae are accumulations of

BULLOUS DISEASES
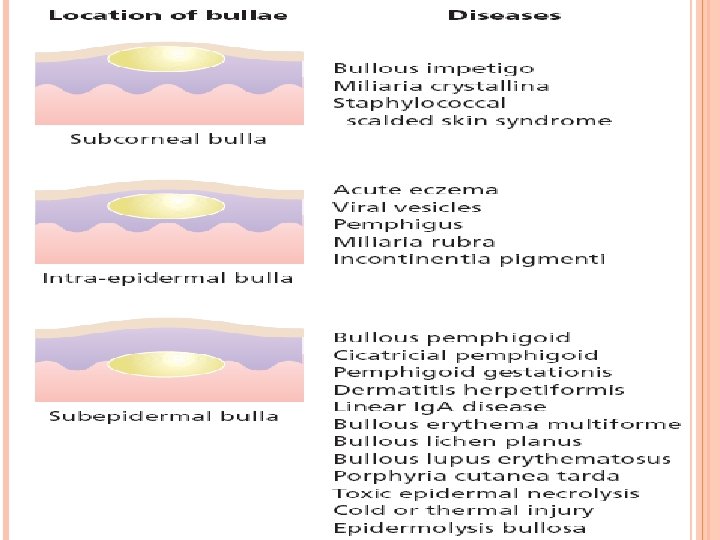
Vesicles and bullae are accumulations of fluid within or under the epidermis. Subepidermal blisters Occur between the dermis and the epidermis. Their roofs are relatively thick and so they tend to be tense and intact. They may contain blood. Intra-epidermal blisters appear within the spinosum cell layer of the epidermis So have thin roofs and rupture easily Leave an oozing denuded surface.
Subcorneal blisters Form just beneath the stratum corneum at the outermost edge of the epidermis Have even thinner roofs Tendency to break is more marked
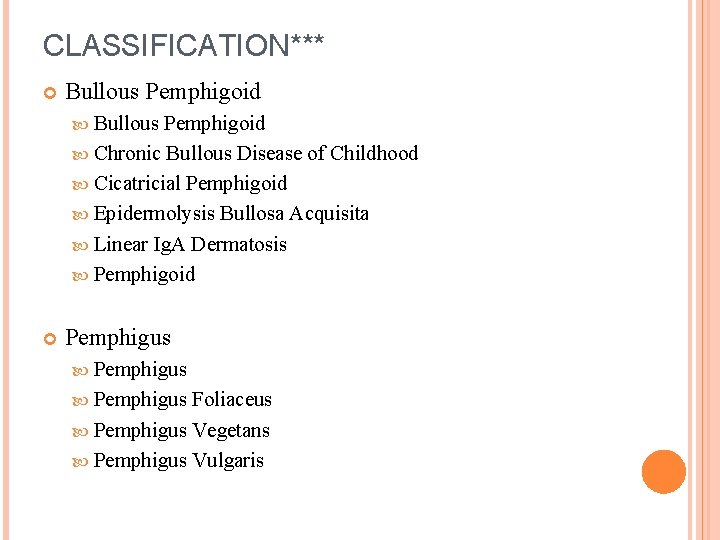
CLASSIFICATION*** Bullous Pemphigoid Chronic Bullous Disease of Childhood Cicatricial Pemphigoid Epidermolysis Bullosa Acquisita Linear Ig. A Dermatosis Pemphigoid Pemphigus Foliaceus Pemphigus Vegetans Pemphigus Vulgaris
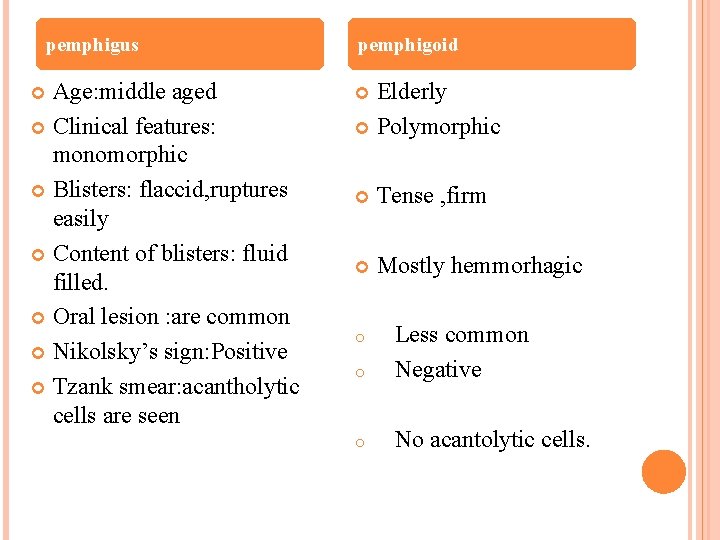
pemphigus Age: middle aged Clinical features: monomorphic Blisters: flaccid, ruptures easily Content of blisters: fluid filled. Oral lesion : are common Nikolsky’s sign: Positive Tzank smear: acantholytic cells are seen pemphigoid Elderly Polymorphic Tense , firm Mostly hemmorhagic o Less common Negative o No acantolytic cells. o
BULLOUS PEMPHIGOID It is an autoimmune disorder, meaning it is caused when the body's immune system malfunctions. The immune system is meant to defend the body against bacteria, viruses, and disease, but instead produces antibodies against healthy tissue, cells and organs. Some patients with BP have other diseases such diabetes and rheumatoid arthritis. Other factors triggering BP include drugs (Furosemide, penicillin), mechanical trauma, and physical traumas (burns from radiation, sun or heat)

BULLOUS PEMPHIGOID*** Epidemiology Age of onset- elderly Men and women affected equally Pathophysiology Autoimmune Subepidermal Blistering Symptoms Pruritus Lesions may be tender at borders Signs Initial Urticarial eruption Develops into large tense bullae after weeks to months Contain clear fluid or may at times be hemorrhagic Diffuse cutaneous involvement Often involves lower legs, forearms, thighs, groin Also involves abdomen Mucosa much less affected than in pemphigous vulgaris No scar formation Milia formation as lesion heals
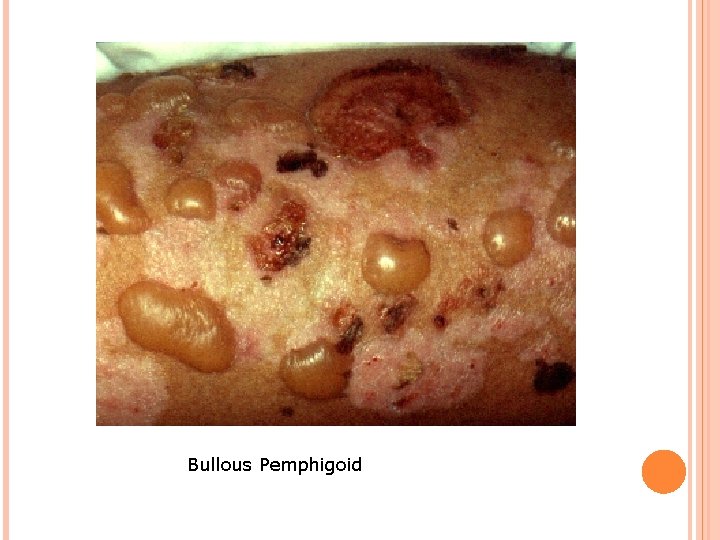
Bullous Pemphigoid
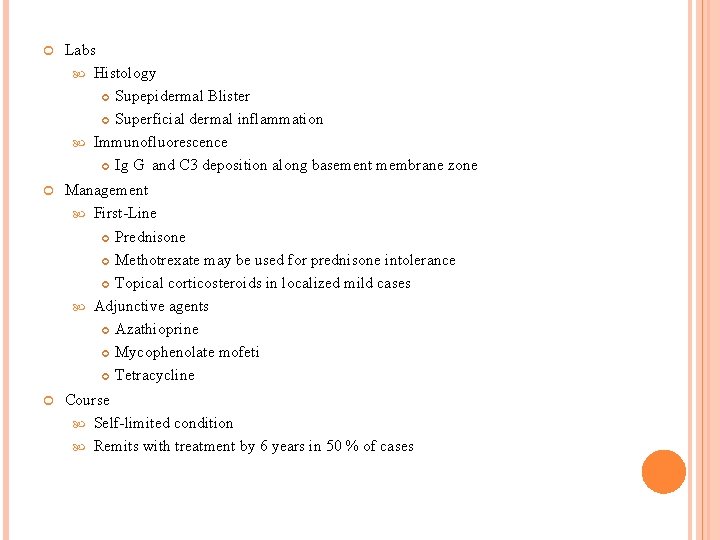
Labs Histology Supepidermal Blister Superficial dermal inflammation Immunofluorescence Ig G and C 3 deposition along basement membrane zone Management First-Line Prednisone Methotrexate may be used for prednisone intolerance Topical corticosteroids in localized mild cases Adjunctive agents Azathioprine Mycophenolate mofeti Tetracycline Course Self-limited condition Remits with treatment by 6 years in 50 % of cases
CHRONIC BULLOUS DISEASE OF CHILDHOOD Epidemiology Age of Onset: Under age 5 years Pathophysiology Autoimmune bullous disorder Variant of Linear Ig. A Dermatosis (seen in adults) Symptoms Pruritus and burning sensation Signs Tense inflamed Blisters over red base May appear as collarettes of Blisters Distribution Most commonly found on genitalia Also may involves face and perioral skin Oral Mucosa involved in 50% of cases

Course Resolves within 2 years of onset in most cases Histology Subepidermal Blisters Inflammatory infiltrates at basement membrane zone Immunofluorescence Ig. A deposition along basement membrane Management First Line: Dapsone or Sulfapyridine (requires G 6 PD and monitoring of CBC) Adjunct: Low dose prednisone initially
CICATRICIAL PEMPHIGOID *** Epidemiology Incidence (rare): 1 in 12, 000 to 20, 000 Ages affected: 60 to 80 years Gender predominance: Women by male ratio of 2: 1 Pathophysiology Autoimmune bullous condition Associated conditions Stevens-Johnson Syndrome Medications Topical Glaucoma medications Practolol Clonidine Signs Blistering of mucus membranes Blister ruptures within hours of formation Painful Erosion
MOST EROSIONS HEAL WITHOUT SCARRING Most common sites of involvement Oral Mucosa (most often buccal and palatal mucosa) Results in erosive Gingivitis Conjunctiva (usually bilateral) Results in chronic Conjunctivitis and scarring Other sites of involvement Skin (usually non-scarring) Scalp (Cicatricial Alopecia) Pharynx and larynx External genitalia Nasal mucosa Anus Esophagus
Labs: Histology Subepidermal bulla Perivascular inflammatory cell infiltrates Fibrosis distinguishes from Bullous Pemphigoid Immunofluorescence with Ig. G, C 3, Ig. A deposits Forms linear band at Basement Membrane Zone Differential Diagnosis Bullous Pemphigoid Epidermolysis Bullosa Acquisita(EBA) Linear Ig. A Bullous Dermatosis(LABD) Systemic Lupus Erythematosus Pseudopemphigoid Pemphigus
MANAGEMENT: Early aggressive treatment First-Line: Prednisone 0. 5 to 0. 75 mg/kg/day x 6 months Ocular Involvement: Azathioprine or Cyclophosphamide Skin Involvement: Topical Corticosteroids Oral Involvement Dapsone Corticosteroid gel Dexamethasone mouthwash Complications Ocular Lesions may result in blindness Laryngeal stricture Esophageal Stricture Supraglottic Stenosis
EPIDERMOLYSIS BULLOSA ACQUISITA** Epidemiology Mean age of onset: 50 years Few isolated cases of children seen Pathophysiology Autoimmune Subepidermal Blistering condition Signs Trauma prone areas more commonly affected Tense Blisters and Erosions over extensor surfaces Knuckles Dorsal hands Elbows Knees Ankles Mucosal involvement Oral, nasal, and esophageal mucosa Conjunctival mucosa
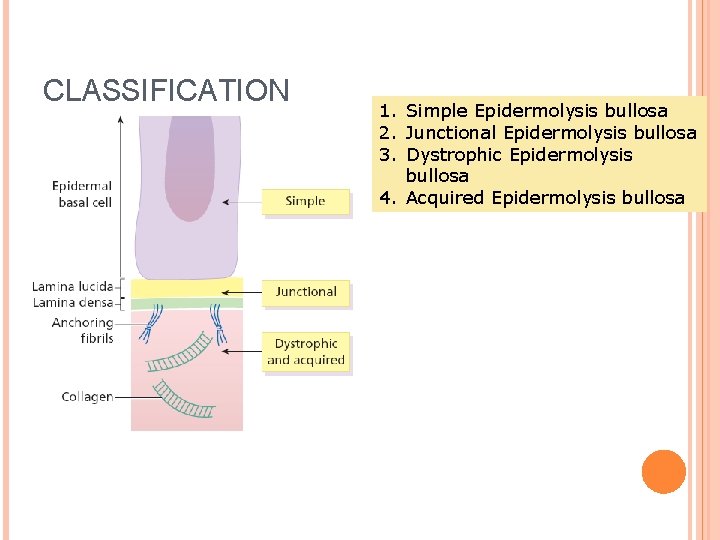
CLASSIFICATION 1. Simple Epidermolysis bullosa 2. Junctional Epidermolysis bullosa 3. Dystrophic Epidermolysis bullosa 4. Acquired Epidermolysis bullosa
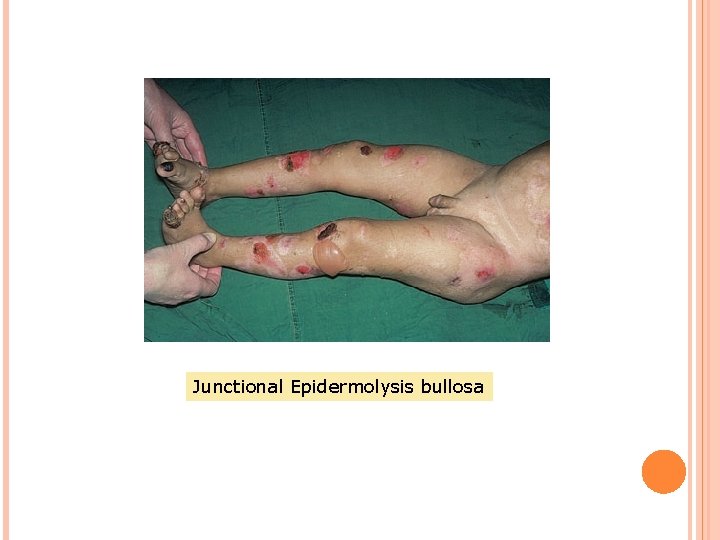
Junctional Epidermolysis bullosa
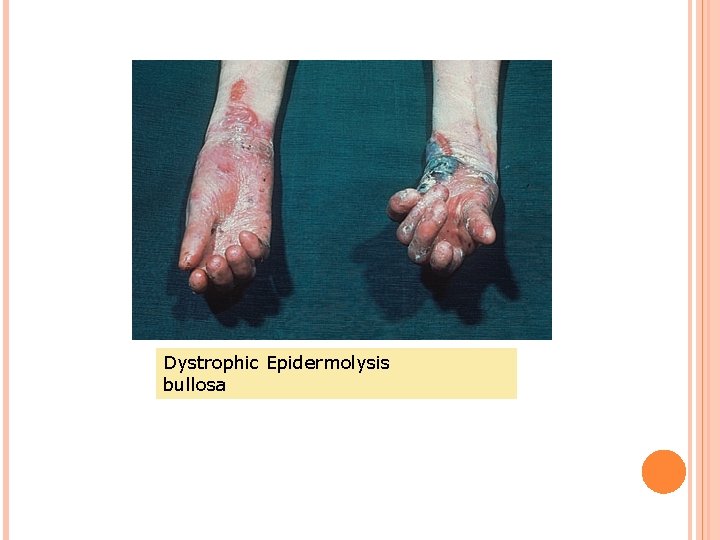
Dystrophic Epidermolysis bullosa
LINEAR IGA DERMATOSIS Epidemiology Onset over age 30 years Pathophysiology Ig. A mediated dermatosis mediated by Ig. A and causes "sausage-like" lobulated blisters arranged at the outer edges of flattened erythematous patches. Autoimmune bullous disorder Variant of Chronic Bullous Disease of Childhood
Symptoms Pruritus Signs Annular Lesions Papules (may be excoriated and crusted) Vesicles Bullae Distribution Symmetric involvement on extensor surfaces Elbows, knees, and buttocks affected Mucosa involvement may occur (Conjunctiva, oral)
Labs Histology Subepidermal Blister with inflammatory infiltrate Immunofluorescence Ig. G deposits at dermal-epidermal junction Complications Scarring skin lesions (with associated Milia) Differential Diagnosis Porphyria cutanea tarda Hereditary Epidermolysis bullosa Bullous Pemphigoid Course Chronic waxing and waning course
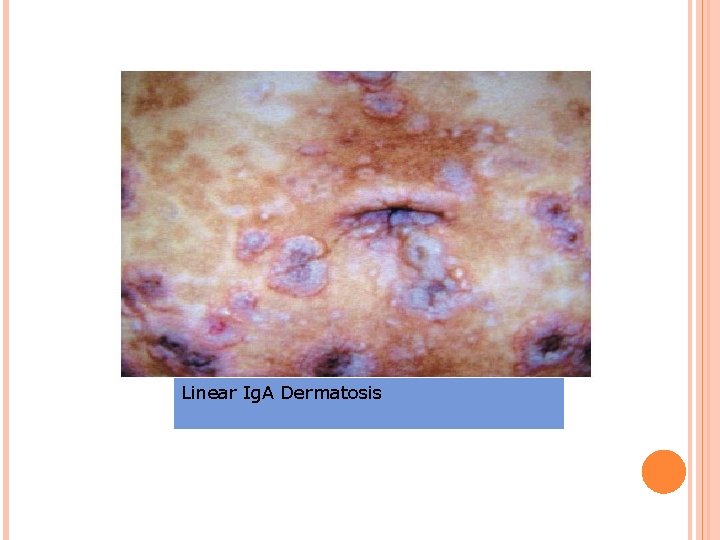
Linear Ig. A Dermatosis
- Slides: 25