Built to Last The Successful Patient Centered MedicalHome
Built to Last: The Successful Patient Centered Medical-Home (PCMH) Team PCPCC Stakeholders’ Working Meeting April 28, 2009 Guy Mansueto, VP, Phytel Moderator

Our Panelists Richard C. Antonelli, M. D. , M. S. , FAAP Medical Director, Integrated Care Organization, Children's Hospital Boston/ Harvard Medical School Suzanne Mitchell, M. D. M. Sc. Faculty, Boston University School of Medicine Christine Sinsky, M. D. Medical Associates Clinic, Dubuque, Iowa Linda Strand, Pharm. D. , Ph. D. , D. Sc. (Hon) Distinguished Professor, College of Pharmacy, University of Minnesota 2

Successful PCMH Team: What Constitutes Care Coordination in a Pediatric Medical Home? Richard C. Antonelli, M. D. , M. S. , FAAP Medical Director, Integrated Care Organization, Children's Hospital Boston/ Harvard Medical School
Challenges to Implementing Family-Centered Medical Home • TIME, TIME • Lack of organized systems of care with defined roles • Inadequately developed family/patient -professional partnerships • Knowledge – Care pathways – how to change • Lack of Care Coordination function • Lack of awareness of community resources and programs • “Reimbursement” 4
Defining Care Coordination Pediatric care coordination is a patient- and familycentered, assessment-driven, team-based activity designed to meet the needs of children and youth while enhancing the care giving capabilities of families. Care coordination addresses interrelated medical, social, developmental, behavioral, educational, and financial needs in order to achieve optimal health and wellness outcomes. Source: MAKING CARE COORDINATION A CRITICAL COMPONENT OF THE PEDIATRIC HEALTH SYSTEM: A MULTIDISCIPLINARY FRAMEWORK Richard C. Antonelli, Jeanne W. Mc. Allister, and Jill Popp The Commonwealth Fund, April 2009 5
Components of Care Coordination Family-centered and Community-based Proactive, Providing Planned, Comprehensive Care Promotes the Development of Self Management Skills (Care Partnership Support) with Children, Youth and Families Facilitates cross-organizational linkages and relationships Source: MAKING CARE COORDINATION A CRITICAL COMPONENT OF THE PEDIATRIC HEALTH SYSTEM: A MULTIDISCIPLINARY FRAMEWORK Richard C. Antonelli, Jeanne W. Mc. Allister, and Jill Popp The Commonwealth Fund, April 2009
Care Coordination Functions • • • Provides separate visits and care coordination interactions Manages continuous communications Completes/analyzes assessments Develops care plans with families Manages/tracks tests, referrals, and outcomes Coaches patients/families Integrates critical care information Supports/facilitates care transitions Facilitates team meetings Uses health information technology
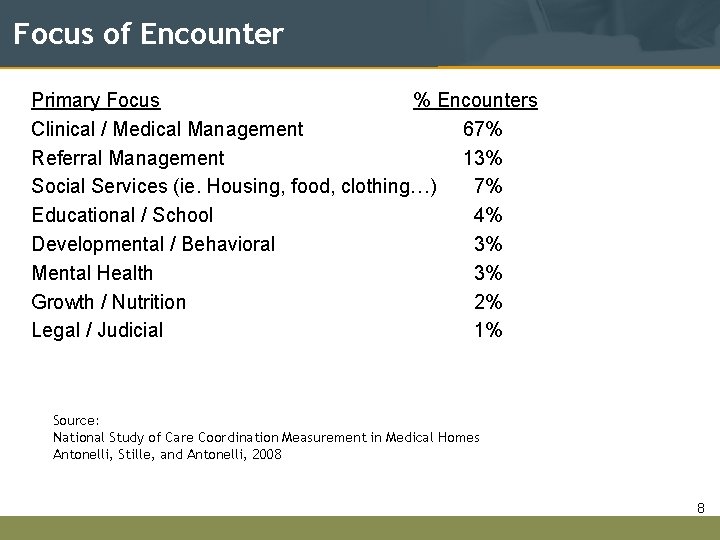
Focus of Encounter Primary Focus % Encounters Clinical / Medical Management 67% Referral Management 13% Social Services (ie. Housing, food, clothing…) 7% Educational / School 4% Developmental / Behavioral 3% Mental Health 3% Growth / Nutrition 2% Legal / Judicial 1% Source: National Study of Care Coordination Measurement in Medical Homes Antonelli, Stille, and Antonelli, 2008 8

Prevented Outcome The CCMT allows only one outcome prevented per encounter. 32% of total 3855 CC encounters prevented something. Of the 1232 CC Encounters where prevention was noted as an outcome: Outcome Prevented Visit to Pediatric Office / Clinic Emergency Department Visit Subspecialist Visit Hospitalization Lab / X-Ray Specialized Therapies # CC Encounters 714 323 124 47 16 8 Percentage 58% 26% 10% 4% 1% 1% 62% of RN CC Encounters prevented something. 33% of MD CC Encounters prevented something. RNs are responsible for coding 81% of the Emergency Department preventions and 63% of the sick office visit preventions. 9
Implications for Policy and Practice • Re-examine the traditional, office-based interaction • Service unit for primary care in PCMH must include CC • Service unit must value non-face-to-face care provided by non-MD staff supporting care coordination • Use Care Plans to drive (and to monitor) care provision • All PCMH team members function at “the top of their license” • Multiplicity of demands for CC demands participation by integrated team: MD, NP/PA, RN, LPN, MA, pharmacy, community partners (eg, dental, mental; education) • All aspects of system performance transparent to families and payers/ purchasers 10
Successful PCMH Team: The Patient / Family as Team Members Suzanne Mitchell, M. D. M. Sc. Faculty, Boston University School of Medicine
A Structured Approach to Relationship-Centered Care • • Build Relationships / Serve Collaborate Educate Negotiate 12
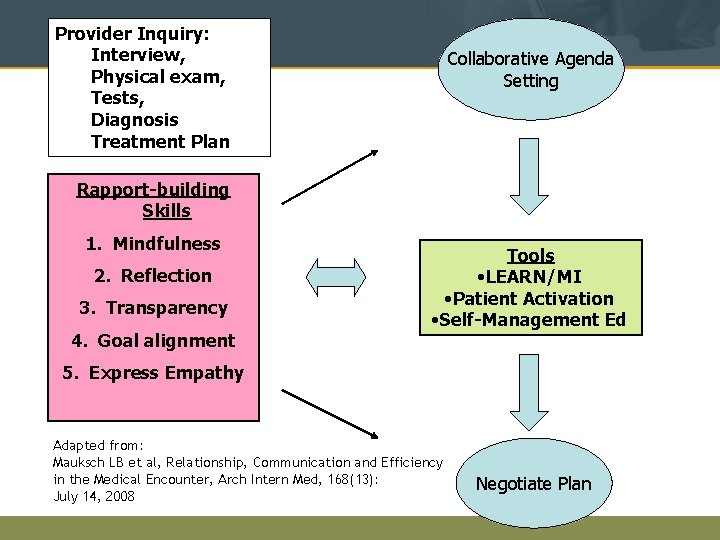
Provider Inquiry: Interview, Physical exam, Tests, Diagnosis Treatment Plan Collaborative Agenda Setting Rapport-building Skills 1. Mindfulness 2. Reflection 3. Transparency 4. Goal alignment Tools • LEARN/MI • Patient Activation • Self-Management Ed 5. Express Empathy Adapted from: Mauksch LB et al, Relationship, Communication and Efficiency in the Medical Encounter, Arch Intern Med, 168(13): July 14, 2008 Negotiate Plan
Tools and Techniques • Collaborative Agenda Setting • LEARN Interview Model – Active Listening Skills – Eliciting the Explanatory Models – Motivational Interviewing • Self-Management Ed. 14
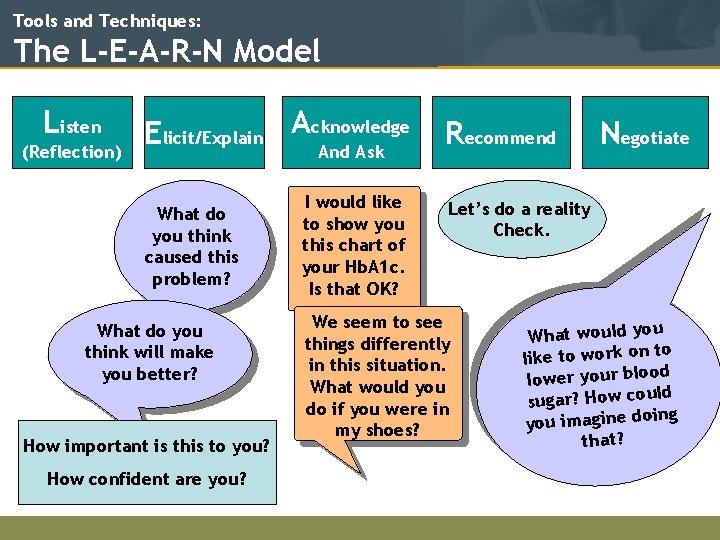
Tools and Techniques: The L-E-A-R-N Model Listen (Reflection) Elicit/Explain Acknowledge And Ask What do you think caused this problem? What do you think will make you better? How important is this to you? How confident are you? I would like to show you this chart of your Hb. A 1 c. Is that OK? Recommend Negotiate Let’s do a reality Check. We seem to see things differently in this situation. What would you do if you were in my shoes? What would you to like to work on d lower your bloo ld sugar? How cou g you imagine doin that?
Tools and Techniques: Self-Management Education • Patients identify their problems • Problem-solving skills • Decision-Making Techniques • Builds and Relies on Self-Efficacy • Addresses: – – – Communication Skills, Life. Style Changes, Medication Adherence, Mood Challenges, Assessing New Treatments Source: Bodenheimer et al JAMA November 20, 2002—Vol 288, No. 19 16
Tools and Techniques: Action Plans Fuel Motivation • Action plans are developed by patients - not providers. • The action plans build confidence that fuels internal motivation. 17
Relationship-Centered Care • Reduces Patient Anxiety • Promotes Patient-centered Treatment Goals • Enhances Self-Efficacy • Optimizes Use of Resources • Improves Quality of Care • Restores Provider Commitment and Prevents Burn-out 18
Successful PCMH Team: Nurse-Physician Partnerships Christine A. Sinsky, MD Medical Associates Clinic and Health Plans

Patient Centered Medical Home
Integrated, Continuous Care Build-in rather than Carve-out Office Visit Nurse-MD Team Between Efficiencies and care Visit Care coordination 1. 5 nurses: MD
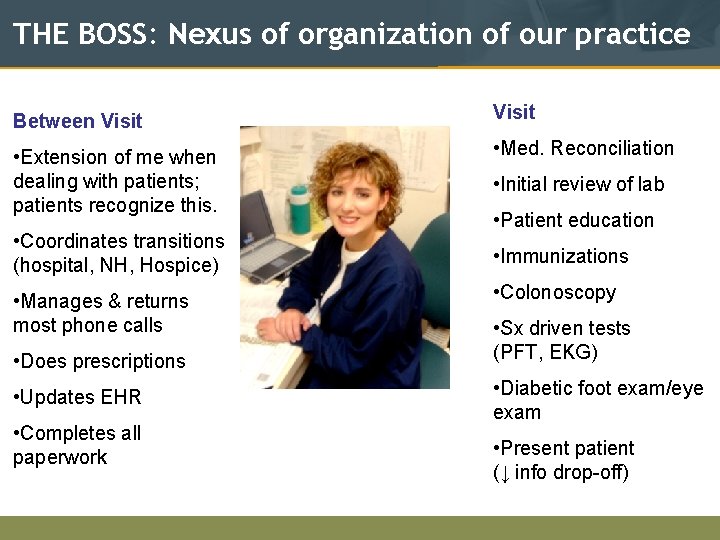
THE BOSS: Nexus of organization of our practice Between Visit • Extension of me when dealing with patients; patients recognize this. • Med. Reconciliation • Coordinates transitions (hospital, NH, Hospice) • Manages & returns most phone calls • Does prescriptions • Updates EHR • Completes all paperwork • Initial review of lab • Patient education • Immunizations • Colonoscopy • Sx driven tests (PFT, EKG) • Diabetic foot exam/eye exam • Present patient (↓ info drop-off)
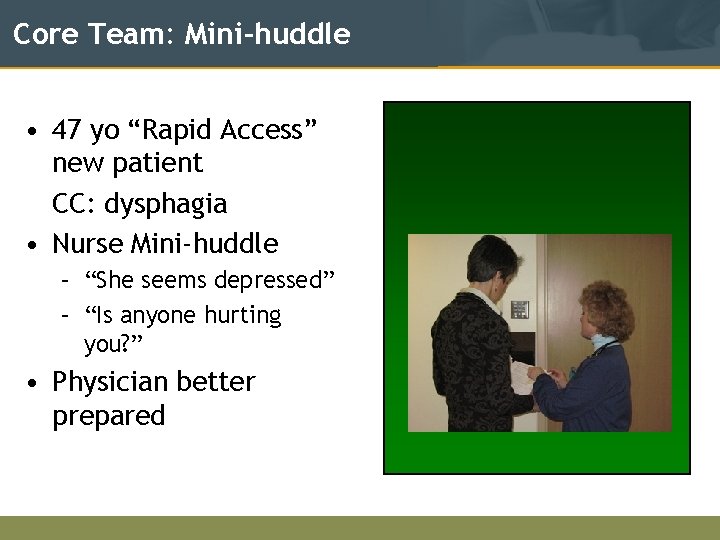
Core Team: Mini-huddle • 47 yo “Rapid Access” new patient CC: dysphagia • Nurse Mini-huddle – “She seems depressed” – “Is anyone hurting you? ” • Physician better prepared
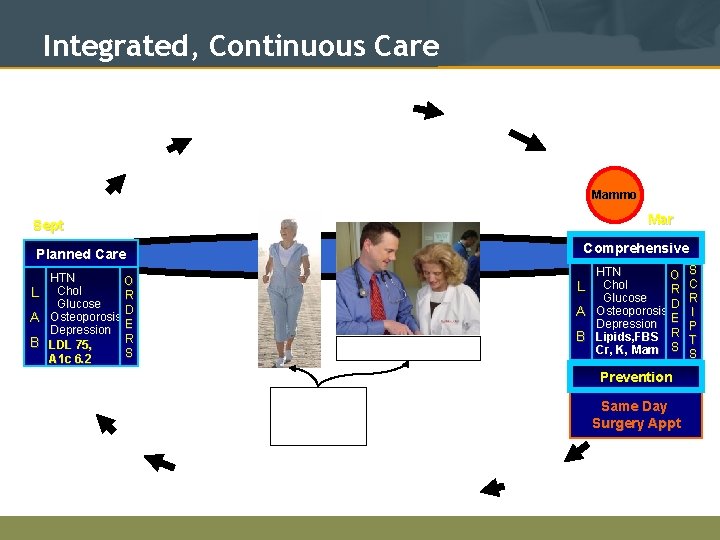
Integrated, Continuous Care Lab Mammo Mar Sept Comprehensive Planned Care HTN O L Chol R Glucose D A Osteoporosis E Depression R B LDL 75, S A 1 c 6. 2 L A Nurse-MD Team B HTN O Chol R Glucose D Osteoporosis Depression E Lipids, FBS R Cr, K, Mam S Prevention Efficiencies and care coordination Same Day Surgery Appt S C R I P T S
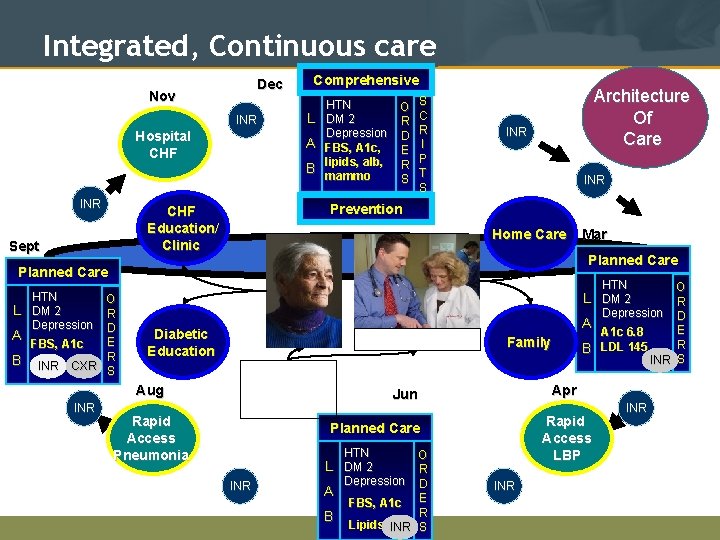
Integrated, Continuous care Dec Nov INR Hospital CHF INR Comprehensive L A B S C R I P T S Architecture Of Care INR Prevention CHF Education/ Clinic Sept HTN O DM 2 R Depression D FBS, A 1 c, E lipids, alb, R mammo S INR Home Care Planned Care HTN L DM 2 Depression HTN O R D A E FBS, A 1 c B INR CXR R S O R Depression D A E A 1 c 6. 8 R B LDL 145 INR S L DM 2 Diabetic Education Aug INR Mar Rapid Access Pneumonia Nurse-MD Team Efficiencies and care coordination Family Apr Jun Rapid Access LBP Planned Care HTN O R Depression D A FBS, A 1 c E R B Lipids INR S L DM 2 INR INR
At the center of the PCMH are face-to-face healing relationships. Patient: Nurse: Physician Patient: Physician 26

Successful PCMH Team: Medication Management in Medical Home Linda M. Strand, Pharm. D. , Ph. D. , D. Sc. (Hon) Distinguished Professor, College of Pharmacy University of Minnesota And Consultant, Medication Management Systems, Inc. Discloser: Founding Member of the Board of Directors Medication Management Systems, Inc
Roles of the Pharmacist Dispensing Clinical pharmacist Medication therapy management
Definitions of Medication Therapy Management 1. APh. A Consensus Statement 2. American Medical Association 3. Minnesota Legislation for Minnesota Medicaid
Medication Management in Medical Home 1. Patient specific 2. Involves an assessment of drug-related needs, care plan to resolve drug therapy problems and follow-up to determine actual impact 3. Comprehensive 4. Coordinated with other team members 5. Adds unique value to care
Practice Settings for Medication Management Clinic Practices Telephonic services Retail Settings
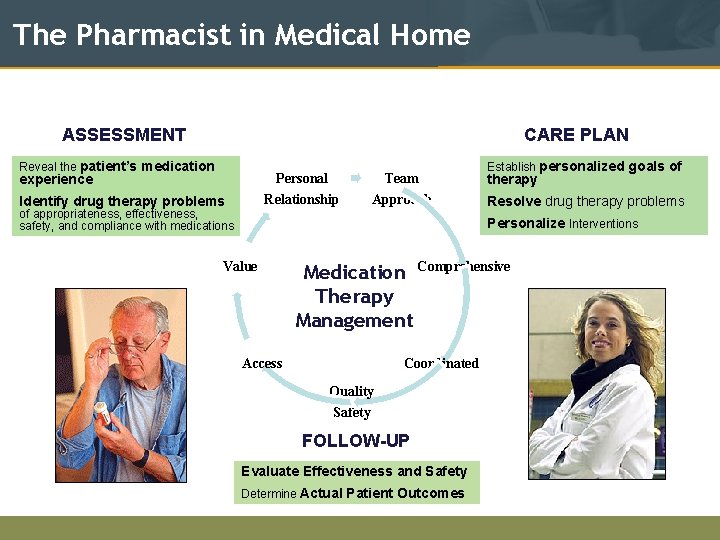
The Pharmacist in Medical Home ASSESSMENT CARE PLAN Reveal the patient’s medication Personal Relationship experience Identify drug therapy problems Team Approach of appropriateness, effectiveness, safety, and compliance with medications Establish personalized goals of therapy Resolve drug therapy problems Personalize Interventions Value Medication Comprehensive Therapy Management Access Coordinated Quality Safety FOLLOW-UP Evaluate Effectiveness and Safety Determine Actual Patient Outcomes
Panelist Q&A Richard C. Antonelli, M. D. , M. S. , FAAP Medical Director, Integrated Care Organization, Children's Hospital Boston/ Harvard Medical School Suzanne Mitchell, M. D. M. Sc. Faculty, Boston University School of Medicine Christine Sinsky, M. D. Medical Associates Clinic, Dubuque, Iowa Linda Strand, Pharm. D. , Ph. D. , D. Sc. (Hon) Distinguished Professor, College of Pharmacy, University of Minnesota 33
Thank You! 34
References: Care Coordination • Mc. Pherson, M. , Arango, P. , Fox, H. , et al. (1998). A new definition of children with special health care needs. Pediatrics, 102, 137– 140 • Porter, M. and Teisberg, E. , Redefining Health Care: Creating Value -Based Competition on Results. Harvard Business School Press, 2006. • Antonelli, R, Mc. Allister, J, and Popp, J. Making Care Coordination a Critical Component of the Pediatric Health System: A Multidisciplinary Framework, April, 2009, The Commonwealth Fund. 35
References: Care Coordination (cont. ) • Antonelli, R. and Antonelli, D. , Providing a Medical Home: The Cost of Care Coordination Services in a Community-Based, General Pediatric Practice, Pediatrics, Supplement, May, 2004. • Antonelli, R. , Stille, C. and Freeman, L. , Enhancing Collaboration Between Primary and Subspecialty Care Providers for CYSHCN, Georgetown Univ. Center for Child and Human Development, 2005 • Antonelli, RC, Stille, C, and Antonelli, DM, Care coordination for children and youth with special health care needs: A descriptive, multisite study of activities, personnel costs, and outcomes. Pediatrics. 2008 Jul; 122(1): e 209 -16. • Turchi, R, Gatto, M, and Antonelli, R, Children and Youth with Special Health Care Needs: There is No Place Like (a Medical) Home, Curr Opin Pediatr 2007, 19: 503. 36
Links to Resources: Relationship-Centered Care • Stanford Self-Management Education Program http: //patienteducation. stanford. edu/programs /cdsmp. html • http: //motivationalinterview. org • Kleinman A, Eisenberg L, Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978; 88(2): 251 -258 37
Links to Resources: Medication Management in Medical Home 1. Kuo GM et. al. Collaborative drug therapy management services and reimbursement in a family medicine clinic. Am J Health-Syst Pharm. 2004; 61: 343 -54. 2. Nkansah NT et. al. Clinical outcomes of patients with diabetes mellitus receiving medication management by pharmacists in an urban private physician practice. Am J Health-Syst Pharm. 2008; 65: 145 -9. 3. Isetts, et. al. Clinical and economic outcomes of medication therapy management services: The Minnesota Experience. J Am Pharm Assoc 2008; 48: 203 -211. 4. Isetts, et. al. Quality assessment of a collaborative approach. Arch Int Med 2003; 163: 1813 -20.
- Slides: 38