Building Toward a National e Health Future Andy
Building Toward a National e. Health Future Andy Bond Manager Interoperability and Standards
NEHTA’s purpose Lead the uptake of e. Health systems of national significance; and coordinate the progression and accelerate the adoption of e. Health by delivering urgently needed integration infrastructure and standards for health information
The Health Reform Agenda and National e. Health Strategy e. Health is one of the eight main elements of the National Health Reform agenda. It is one of the most important opportunities to: • Improve the quality and safety of healthcare • Reduce waste and inefficiency • Improve continuity and health outcomes for patients
The facts speak for themselves • Australia’s life expectancy is one of the highest in the world, second only to Japan • In 1996, chronic disease accounted for 80 per cent of the burden of disease, measured in terms of loss of years and quality of life • Over three million Australians, or nearly one in seven, suffer from chronic disease • Health expenditure as a proportion of Australian GDP has more than doubled over the last four and a half decades from 3. 8% to 9%
Impact on consumers • It is estimated 5, 000 Australians die each year due to adverse medical events. 1 • Up to one in six (18%) medical errors are due to inadequate patient information. 2 • Nearly one in three (30%) unplanned hospital admissions in those over 75 years are associated with prescribing errors. 3
Impact on clinicians • Clinicians spend around a quarter of their time collecting information rather than treating patients. 4 • e. Prescription systems in Sweden, the US and Denmark increased health provider productivity per prescription by over 50%. 5 • e. Referrals in Europe reduced average time spent on referrals by 97%. 6
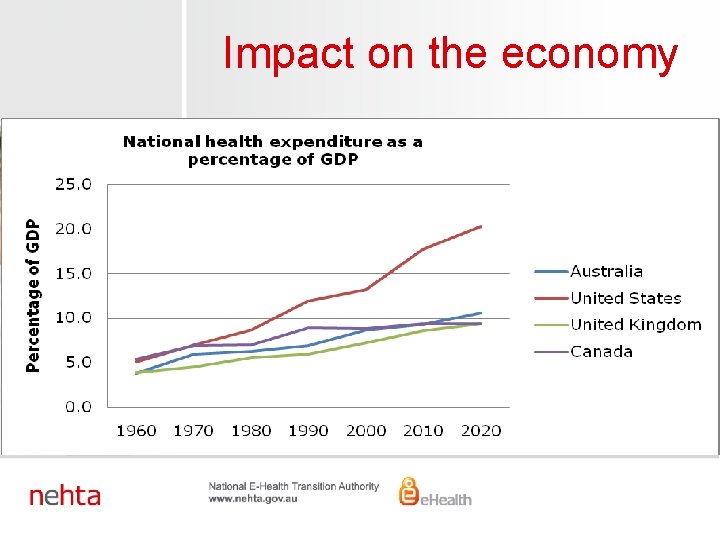
Impact on the economy
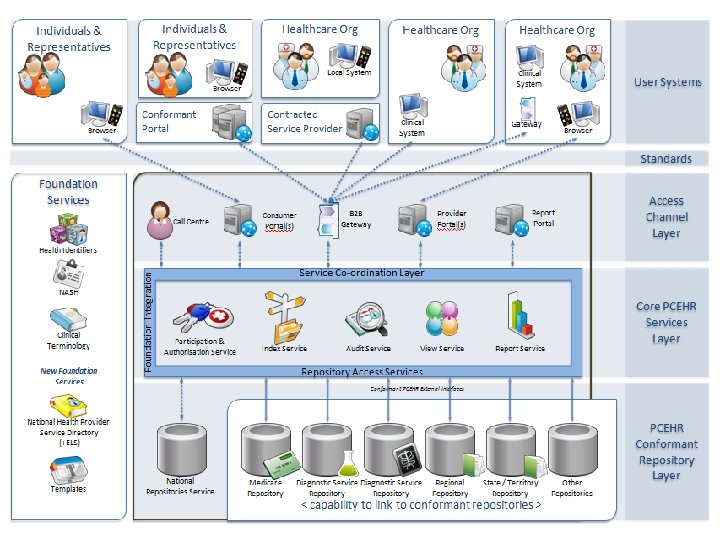
The role of the public and private systems in healthcare provision • The system and processes are managed by a mix of government and private sector organisations • Our Architecture is designed to link-up healthcare information – with standards based information sharing • It represents a “middle-road” approach, creating common technical goals with underpinning standards
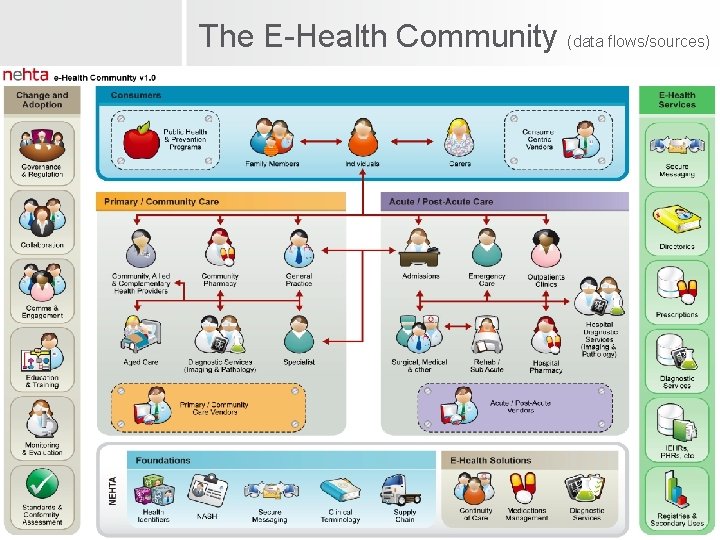
The E-Health Community (data flows/sources)
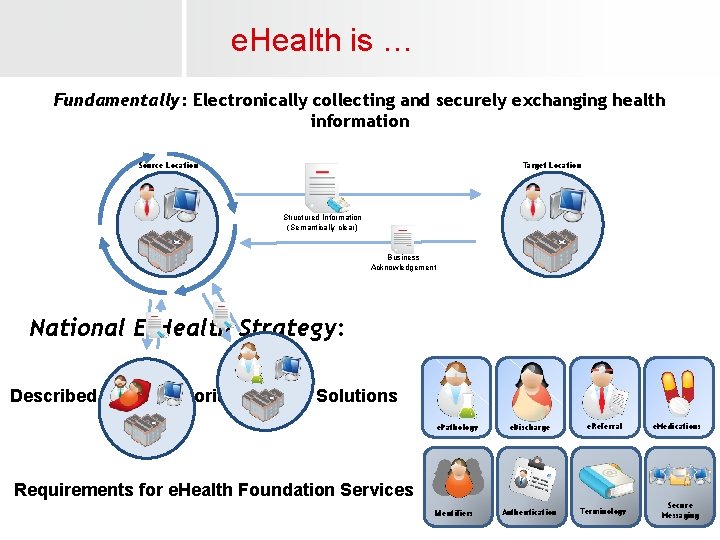
e. Health is … Fundamentally: Electronically collecting and securely exchanging health information Source Location Target Location Structured Information (Semantically clear) Business Acknowledgement National E-Health Strategy: Described a set of Priority E-Health Solutions e. Pathology e. Discharge e. Referral Authentication Terminology e. Medications Requirements for e. Health Foundation Services Identifiers Secure Messaging
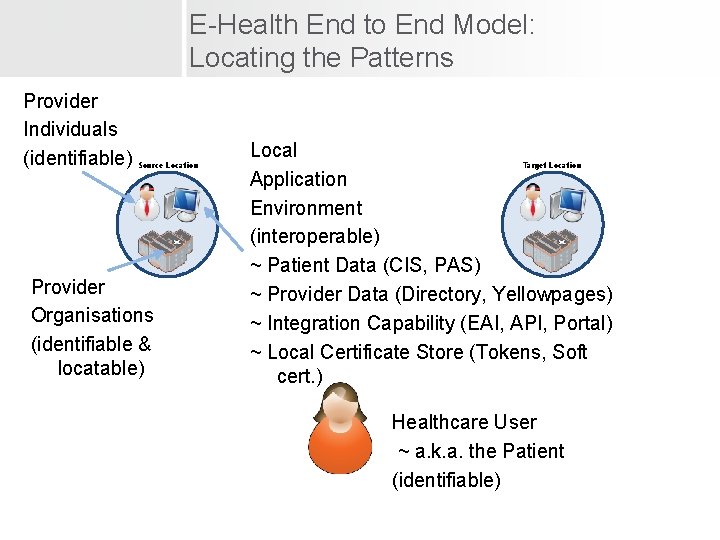
E-Health End to End Model: Locating the Patterns Provider Individuals (identifiable) Source Location Provider Organisations (identifiable & locatable) Local Application Environment (interoperable) ~ Patient Data (CIS, PAS) ~ Provider Data (Directory, Yellowpages) ~ Integration Capability (EAI, API, Portal) ~ Local Certificate Store (Tokens, Soft cert. ) Target Location Healthcare User ~ a. k. a. the Patient (identifiable)
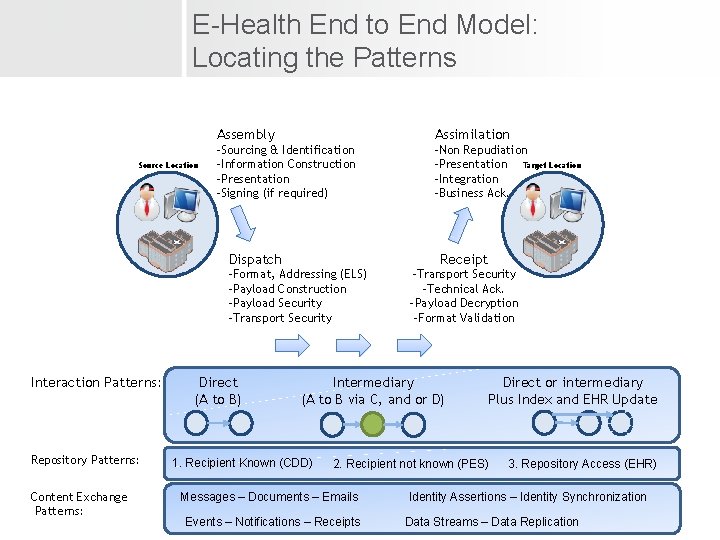
E-Health End to End Model: Locating the Patterns Source Location Assembly Assimilation -Sourcing & Identification -Information Construction -Presentation -Signing (if required) -Non Repudiation -Presentation Target Location -Integration -Business Ack. Dispatch Receipt -Format, Addressing (ELS) -Payload Construction -Payload Security -Transport Security Interaction Patterns: Repository Patterns: Content Exchange Patterns: Direct (A to B) -Transport Security -Technical Ack. -Payload Decryption -Format Validation Intermediary (A to B via C, and or D) 1. Recipient Known (CDD) Direct or intermediary Plus Index and EHR Update 2. Recipient not known (PES) Messages – Documents – Emails Events – Notifications – Receipts 3. Repository Access (EHR) Identity Assertions – Identity Synchronization Data Streams – Data Replication
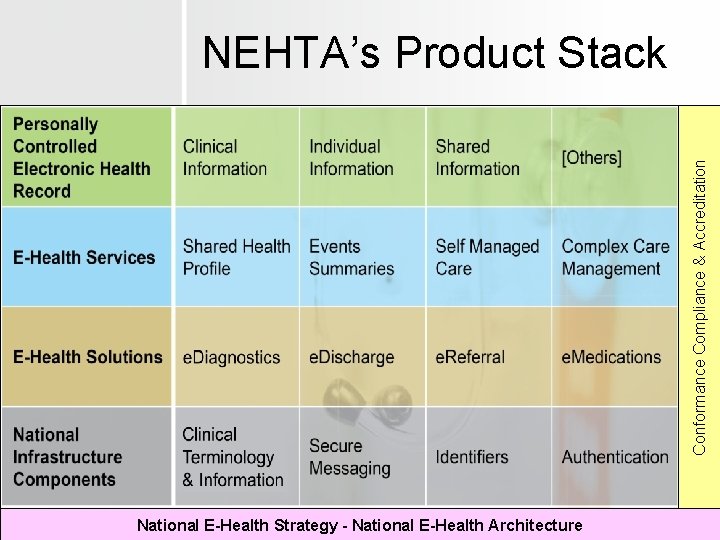
Conformance Compliance & Accreditation NEHTA’s Product Stack National E-Health Strategy - National E-Health Architecture
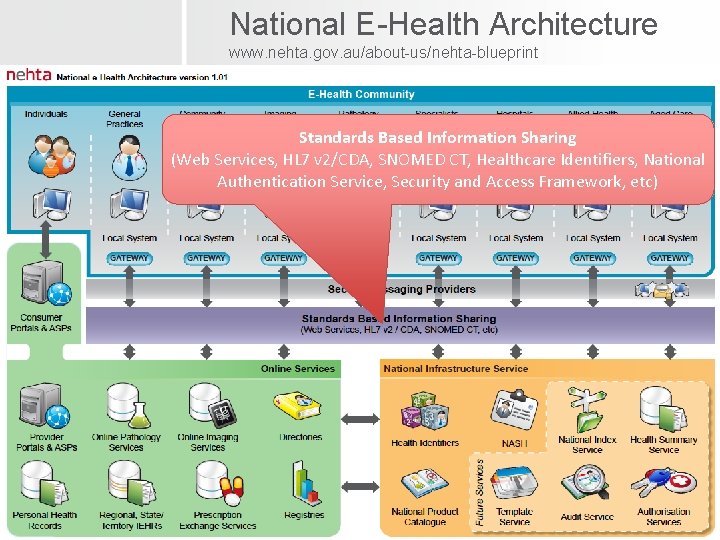
National E-Health Architecture www. nehta. gov. au/about-us/nehta-blueprint Standards Based Information Sharing (Web Services, HL 7 v 2/CDA, SNOMED CT, Healthcare Identifiers, National Authentication Service, Security and Access Framework, etc)
What is the PCEHR System? • The PCEHR System is a secure system which enables individuals to store and share clinical documents important to their ongoing care • Participation is voluntary and individuals will have a range of controls over the record • The PCEHR System will be underpinned by • Rigorous governance and oversight to maintain privacy; • National standards and core national infrastructure; • The PCEHR systems complements (not replaces) existing records and clinical communications
How will it work?
How do providers get access? • PCEHR System can be accessed by any Healthcare Organisation with a HPI-O and comply with the terms of access • Options for access include: • Enhanced versions of clinical systems • Provider Portal • Organisation choose which local users need access • Managed in local clinical system (or in HI PDS for provider portal) • The PCEHR System will only accept clinical documents from providers with a HPI-I
Participation by Individuals • Voluntary Participation based on an opt-in basis • Individual must have an IHI • Registration • Web Based Portal • Assisted Registration at Medicare or by some healthcare providers • A range of campaigns will be put in place to drive adoption • Can withdraw at any time • Can access their PCEHR via: • Consumer Portal • Third party conformant portals
Personal Control Individuals can: • Decide whether or not to have an active PCEHR • Access information in their PCEHR • Decide how healthcare provider access is obtained (e. g. is an access code required or can any provider involved in care have access) • Authorise and/or nominate representatives • Control access to documents in their PCEHR • View an activity history for their PCEHR • Make enquiries and complaints
Time Frame 2010 -11 • Consultation with various stakeholder groups 2011 -12 • Procure and Implement PCEHR System • Develop enabling legislation • Initiate lead sites 2012 + • Individuals able to register from July 2012 • Longer term sector wide change and adoption program underway ….
Who is Doing What? Ernst & Young PWC + Partners Reviewing Tenders Mc. Kinsey & Company + Partners
National e. Health Lead Sites • Deploy and test national e-Health infrastructure and standards; • Demonstrate tangible outcomes and benefits; • Build stakeholder support and momentum; and • Provide a meaningful foundation for further enhancement and roll-out of the national PCEHR system.
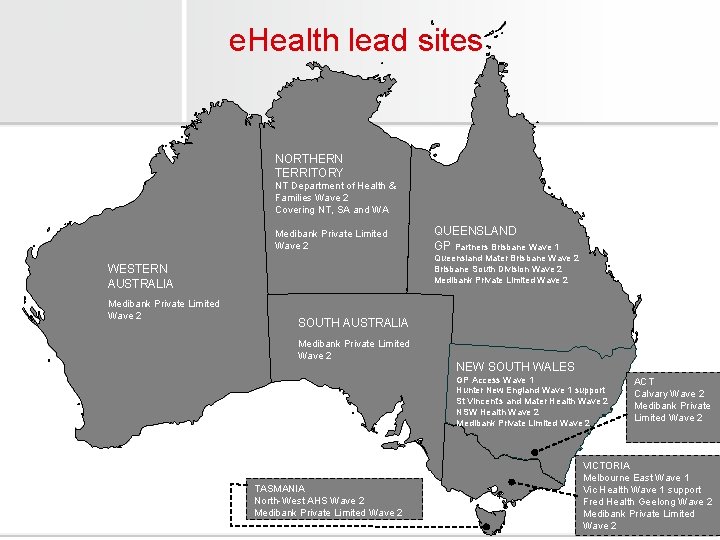
e. Health lead sites NORTHERN TERRITORY NT Department of Health & Families Wave 2 Covering NT, SA and WA Medibank Private Limited Wave 2 Queensland Mater Brisbane Wave 2 Brisbane South Division Wave 2 Medibank Private Limited Wave 2 WESTERN AUSTRALIA Medibank Private Limited Wave 2 QUEENSLAND GP Partners Brisbane Wave 1 SOUTH AUSTRALIA Medibank Private Limited Wave 2 NEW SOUTH WALES GP Access Wave 1 Hunter New England Wave 1 support St Vincent’s and Mater Health Wave 2 NSW Health Wave 2 Medibank Private Limited Wave 2 TASMANIA North-West AHS Wave 2 Medibank Private Limited Wave 2 ACT Calvary Wave 2 Medibank Private Limited Wave 2 VICTORIA Melbourne East Wave 1 Vic Health Wave 1 support Fred Health Geelong Wave 2 Medibank Private Limited Wave 2
Keeping it all together… How can we use an Architectural and Standards based approaches to support interoperability? • We have a highly complex environment, with development activities progressing on many fronts. Top down & bottom up. • We need a consistent mechanism to describe what we are working towards.
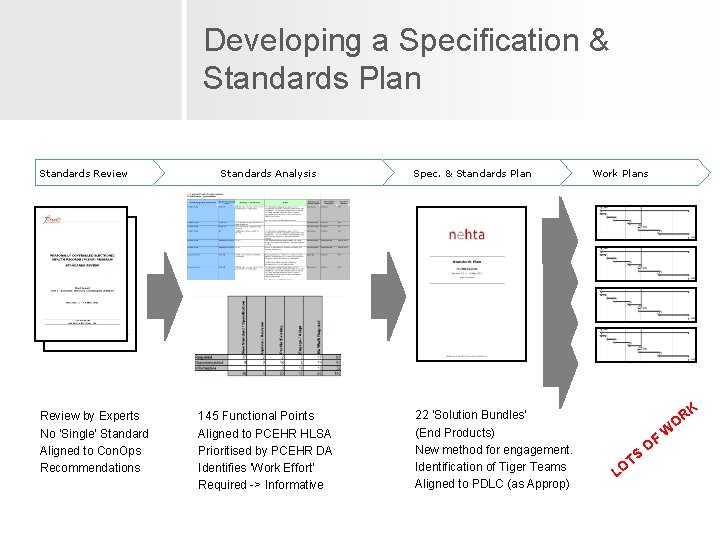
Developing a Specification & Standards Plan Standards Review by Experts No ‘Single’ Standard Aligned to Con. Ops Recommendations Standards Analysis 145 Functional Points Aligned to PCEHR HLSA Prioritised by PCEHR DA Identifies ‘Work Effort’ Required -> Informative Spec. & Standards Plan 22 ‘Solution Bundles’ (End Products) New method for engagement. Identification of Tiger Teams Aligned to PDLC (as Approp) Work Plans K R O S T LO OF W
Access by Healthcare Providers
How do healthcare providers get access to the system? • PCEHR System can be accessed by any Healthcare Organisation with a HPI-O and comply with the terms of access • Options for access include: Enhanced versions of clinical systems Provider Portal • Organisation choose which local users need access Any authorised user can view it (assuming they are involved in the individual’s care) The PCEHR System will only accept clinical documents from providers with a HPI-I
How do I …. Access an individual’s PCEHR? Access is granted to an organisation Only healthcare providers involved in an individual’s care should access an individual’s PCEHR, all access is audited Access only needs to be obtained once, but will expire after 3 years of non access Under basic access controls, if you are involved in the individual’s care you can access the individual’s PCEHR Under advanced access controls, the individual may Set up a PACC (PIN code) to access a PCEHR Apply “no access” and “limited access” access controls to clinical documents need Emergency access Can be used only when the individual is unable to provide consent and needs emergency care
How do I …. Find information in a PCEHR? Views Consolidated view – everything you need in one screen or a click away Index view – for sorting and filtering clinical documents Search Find clinical documents using keywords

When should I …. access a PCEHR? The PCEHR system is an information system Assume that most access will occur inside a consultation when you need access to additional information about the patient There is no requirement to access outside of a consultation, but you can if you want to You don’t necessarily need to look at a PCEHR to upload clinical documents E. g. Path labs You will need to look at a PCEHR when updating a shared health summary
When should I …. use which clinical document? The PCEHR takes copies of existing clinical documents, so you can use clinical documents as you do now If you discharge an admitted patient, use a discharge summary If you refer a patient, use a referral If you respond to a referral, use a specialist letter Want to make sure other providers can see a summary about your patient, use a shared health summary You need to have the individuals agreement to do it, be involved in an individual’s ongoing care and be either a medical practitioner, registered nurse or Aboriginal healthcare worker For everything else that is important for other providers to be able to see there is the event summary E. g. after hours care, sharing progress notes for a series of treatments, etc
Can I …. Correct a clinical document? The PCEHR System assumes that your system holds the “source of truth”. Steps: Fix the information in your local system first Send an amended version of the clinical document to the PCEHR What if I put a clinical document in the wrong PCEHR or I need it removed until I can put up a corrected version? You can ask for a clinical document to be “effectively removed” from a PCEHR.
Keeping up with the PCEHR program news National E-Health Strategy www. health. gov. au Public domain resources http: //www. youtube. com/user/Dept. Health. Ageing Email alerts – send and update your details via: ehealthsystems@health. gov. au General information www. yourhealth. gov. au NEHTA specific information www. nehta. gov. au
Thank you Questions … ?
- Slides: 36