Bringing Trauma Informed Practice to Palliative and Hospice
Bringing Trauma Informed Practice to Palliative and Hospice Care KAREN WILLOW, LCSW PARTNERS IN CARE HOME HEALTH AND HOSPICE BEND OREGON
Objectives 1. Outline Sources of Trauma 2. Discuss Principles of Healing 3. Review Emerging Research in Palliative Care

What is “Trauma-Informed? ” An approach, program, organization, or system that is trauma-informed: Realizes the widespread impact of trauma and understands potential paths for recovery. Recognizes the signs and symptoms of trauma in clients, families, staff, and others involved with the system. Responds by fully integrating knowledge about trauma into policies, procedures, and practices; . Seeks to actively prevent additional trauma.
Emerging Research and Practice Shifts � Barbara Ganzel, Ph. D. , LMSW Ithaca College, Director of Gerontology • • • Palliative care goal = alleviate pain and suffering Mental Health Parity (psychological trauma is often not included) Standard Precautions (dementia/shower/holocaust survivors) EMDR - integrate short term EMDR protocol as a primary intervention for trauma, “one shot EMDR”. � David Feldman, Ph. D. Stepwise Psychosocial Palliative Care Model � Research on trauma with Veterans Now let’s consider how trauma may be present for all those we serve.
Trauma Across the Care Continuum Diagnosis - Serious Illness – Palliative Care – Hospice – Death - Bereavement
https: //www. pinterest. com/pin/520939881875093980/

The Foundations of Trauma Informed Care Commitment to trauma awareness Create safe context: Physical safety Emotional safety Trustworthiness Clear and consistent boundaries Transparency Predictability Understanding the impact of historical trauma and oppression Recognize and honor the individual: Relationship Respect Compassion Acceptance and non-judgment Coordination Mutuality Restore power: Strength focus Empowerment Choice Skill building https: //traumainformedoregon. org/resources/trauma-informed-care-principles/
The Ubuntu Ethic “Sawa Bona” – “I see you” – instead of hello “Sikkona”– “I am here” A Zulu folk saying: “A person is a person because of other people. ” *Until you see me I am not here! *When you see me you bring me into existence. *We invoke each other’s potential by our willingness to see the essence of each other. T Ondra L. Berry. Heartset Mindset Skillset Toolset From Inspiration to Mastery. http: //slideplayer. com/slide/7032054
Skillful Use of Self How we prepare for visit Self as healing agent Personal awareness/healing
Who Might Experience Trauma? • • Patient/family/friends Primary care medical team Hospice or palliative care team Office staff, administrators and board members • Facility staff • Community agency providers • Anyone else who interacts with the person with serious illness
Adverse Childhood Experiences Study (ACES) Adverse childhood experiences are the most basic and long lasting cause of health risk behaviors, mental illness, social malfunction, disease, disability, death and healthcare costs. Adverse Childhood Experiences and their Relationship to Adult Well-being and Disease: Turning gold into lead. Anda, R and Fellitti, V. , August 27, 2012, Retrieved from thenationalcouncil. org
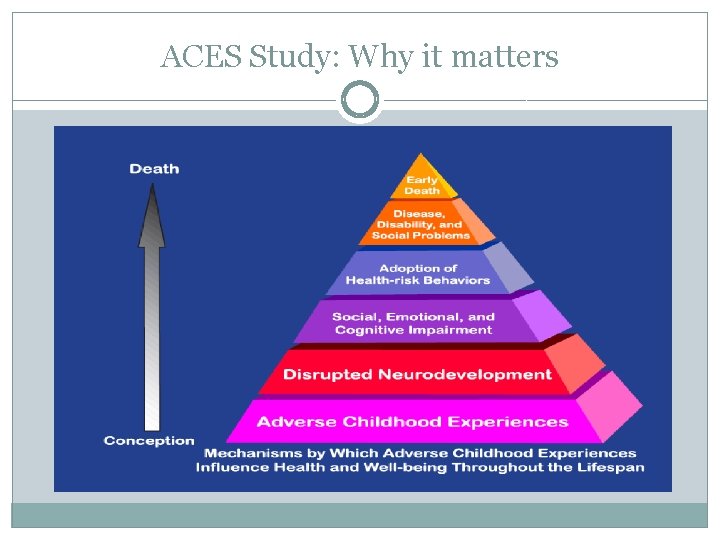
ACES Study: Why it matters
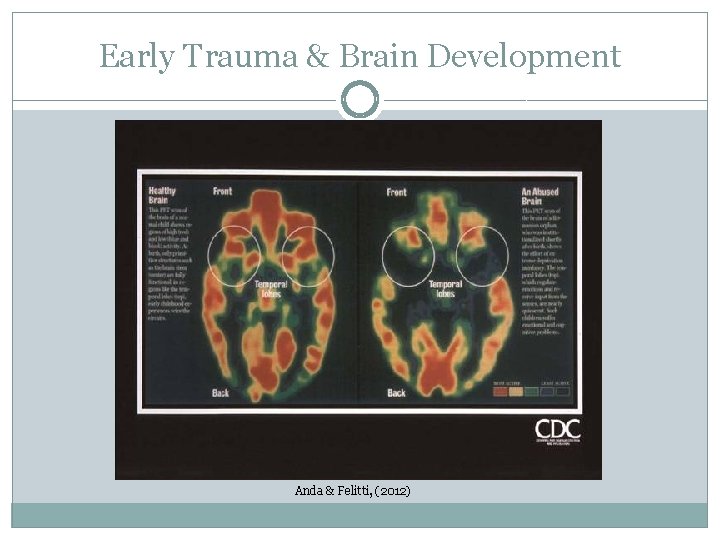
Early Trauma & Brain Development Anda & Felitti, (2012)
Attachment is critical for brain development
Why attachment matters… Secure =flexible Avoidant =restricted Ambivalent=anxious/insecure Disorganized =impaired ability to relate & regulate emotions
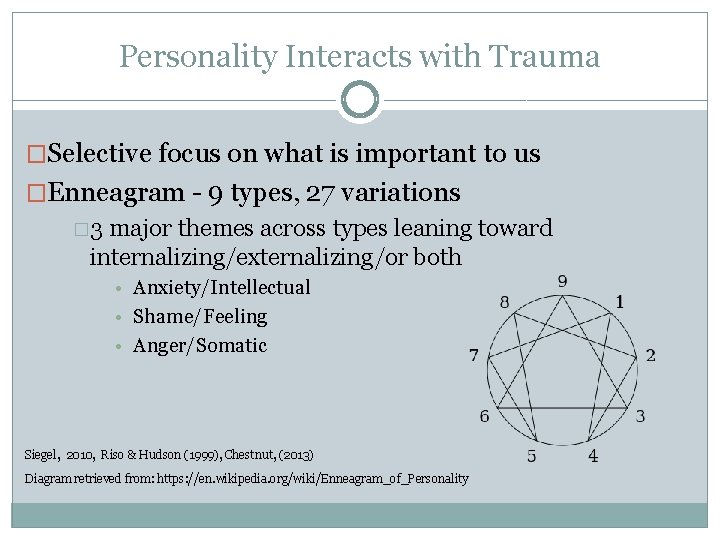
Personality Interacts with Trauma �Selective focus on what is important to us �Enneagram - 9 types, 27 variations � 3 major themes across types leaning toward internalizing/externalizing/or both • Anxiety/Intellectual • Shame/Feeling • Anger/Somatic Siegel, 2010, Riso & Hudson (1999), Chestnut, (2013) Diagram retrieved from: https: //en. wikipedia. org/wiki/Enneagram_of_Personality
Trauma During or From Health Care

Critical Care Trauma • 80% of vented patients experience delirium • Cognitive decline • 6 month mortality rate post ICU care • Post Intensive Care Syndrome (PICS) Barr et al 2013, Needham, et al 2012, Dayvdow 2008 Sorocco, et a
Person in Situation Vulnerability and risk History of trauma Life circumstances Age Education/Income
Unique Issues for Older Adults

Arriving at the Point of Hospice Care • 80% population is over 65 • 40% over 85 • Serious/life threatening illness/dying • Intense medical intervention history • Multiple Losses (Grief/Trauma) • Functional, practical and age-related relational losses • Lack of curative options • Possible feelings of abandonment due to loss of prior treatment team Ganzel – Trauma Informed Hospice and Palliative Care – NHPCO 2012
Bereavement and Trauma • Loss of primary attachment figure • Complete life changes: companionship purpose/meaning identity • Traumatic grief/complicated grief (share characteristics with PTSD)

Trauma Assessment � Who is traumatized? Assess trauma narrative � Is trauma occurring now? � Is history being activated? � How much dysregulation is present? � What are the coping strategies? ● ● ● Early development attachment personality Adverse experiences Understanding the health care journey
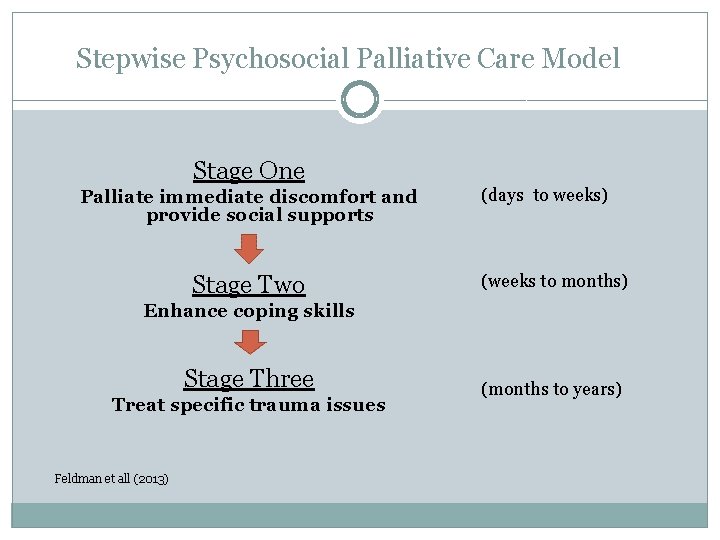
Stepwise Psychosocial Palliative Care Model Stage One Palliate immediate discomfort and provide social supports Stage Two (days to weeks) (weeks to months) Enhance coping skills Stage Three Treat specific trauma issues Feldman et all (2013) (months to years)

Trauma Interventions

Trauma Interventions Approaches Where is the intervention directed? � Medical � Patient/client � Environmental � Caregiver � Spiritual � Spouse � Natural Supports � Family Member(s)/Friends � Mental Health/Substance Use � Support groups � Somatic Approaches � Creative Approaches � Support for Grief, Loss, & Bereavement � Blended Families � Community Providers � Staff � Self
Mindful care
Relational Healing Reparative Restorative experiences Internalization of working with another
Emotional Regulation
Integration

Expanded Growth and Integration
Going Forward • Understand how trauma experiences impact all of us (patient, care team, family, others). • Acknowledge the presence of stress/trauma and considers what is needed to prevent harm and restore well -being. • Consider what needs to be added to our care systems to be sensitive to the effects of trauma. • Implement a trauma informed approach and educate others.
References 1 � Anda, R. , & Felitti, V. Adverse childhood experiences and their relationship to adult well-being and � � � � disease: Turning gold into lead. National Council Webn. R (August 27, 2012). Retrieved from: http: //www. thenationalcouncil. org/wp-content/uploads/2012/11/Natl-Council-Webinar-8 -2012. pdf Badenoch, B. The heart of trauma: Healing our embodied brains in the context of relationships. Presented in Bend, OR 2/19/16 and 2/20/16. Chestnut, B. (2013). The Complete Enneagram: 27 Paths to Self-Knowledge. USA: She Writes Press. Cook, J. (2011). Aging and PTSD. National Center for PTSD, Online Course. Retrieved from: http: //www. ptsd. va. gov/professional/continuing_ed/aging-ptsd. asp Davydow, D. (2008). Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. General Hospital Psychiatry, 30 (5) 421 -34 Feldman, D. et. al (2014). Treatment of posttraumatic stress disorder at the end of life: Application of the stepwise psychosocial palliative care model. Palliative and Supportive Care, 12 (3) 233 -43 Feldman, D. & Periyakoil, V. (2006). Posttraumatic stress disorder at the end of life. Journal of Palliative Medicine, 9 (1) 213 -18 Felliti, V. et al (1998). Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventative Medicine, 14 (4) 245 -58 Felliti, V. The Relation between adverse childhood experiences and adult health: Turning gold into lead. (2002) Retrieved from: http: //www. thepermanentejournal. org/files/Winter 2002/goldtolead. pdf
References 2 � Frueh, B. et al. (2004). Cognitive-behavioral treatment for PTSD among people with severe mental � � � � � illness: A proposed treatment model. Journal of Psychiatric Practice, 10, 26 -38 Ganzel, B. (2015) Trauma-informed hospice and palliative care. Presentation. Retrieved from: https: //www. youtube. com/watch? v=x. Ei. WJ 1 h. PWQM Kaiser, A. et al (undated) Post traumatic stress symptoms among older adults: A review. National Center for PTSD. Retrieved from: http: //www. ptsd. va. gov/professional/treatment/older/ptsd_symptoms_older_adults. asp Mc. Collum, D. (2010), The Coleva Project: Consequences of lifetime exposure to violence and abuse. Retrieved from: http: //www. coleva. net Mate, G. (2008). In the Realm of the Hungry Ghosts. Berkley, CA: North Atlantic Books Needham, D. et al (2012) Improving long-term outcomes after discharge from intensive care unit: Report from a stakeholder’s conference. Critical Care Medicine, 40 (2) 502 -9 Riso, R & Hudson, R (1999). The Wisdom of the Enneagram. New York: Banaam Books Romero, E. (2015). PTSD and end of life considerations. Retrieved from: http: //c. ymcdn. com/sites/www. hnmd. org/resource/remgr/2015_Annual_Conference/Erin. Romero_ PTSD_Presentation. pdf Siegel, D. (2011). Mindsight: The New Science of Personal Transformation. New York: Bantam Books Siegel, D. (2010). The Mindful Therapist. New York: WW Norton & Company Inc. Substance Abuse and Mental Health Services Administration. Trauma-informed approach and trauma -specific interventions. Retrieved from: http: //www. samhsa. gov/nctic/trauma-interventions
References 3 � Sorocco, K. (undated) Treating post traumatic stress disorder (PTSD) at end of life. OUHSU Online � � � Course. Retrieved from: http: //www. ouhsc. edu/okgec/documents/PTSD_Course. pdf Tatkin, S. (2011). Wired for Love. Oakland, CA: New Harbinger Publications Inc. The National Child Traumatic Stress Network. Secondary traumatic stress and related conditions: sorting one from another. Retrieved from: http: //www. nctsn. org/resources/topics/secondarytraumatic-stress Thomson, R. et al (2013) Palliative Care Principles Primary Care Physicians Should Know. ACH Media, Retrieved from: http: //www. ahcmedia. com/articles/64540 -palliative-care-principles-primary-carephysicians-should-know Van der Kolk, B. (2014). The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma. USA: Penguin Books Whyte, David (2009). The Three Marriages: Reimagining Work, Self and Relationship. USA; Penguin Books
- Slides: 37