Bringing EMS Into Care Coordination Mobile Healthcare Access
Bringing EMS Into Care Coordination: Mobile Healthcare Access & Integration Pilot Study Nita Ham, Director Officer State Office of Rural Health Programs & Joycelyn Yates, Chief Quality Albany Area Primary Health Care, Inc.

87 Rural Hospital Closures: January 2010 – Present 1
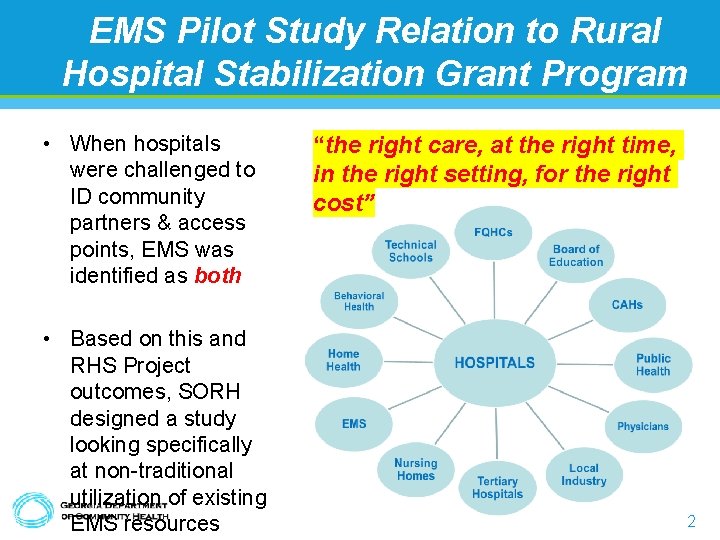
EMS Pilot Study Relation to Rural Hospital Stabilization Grant Program • When hospitals were challenged to ID community partners & access points, EMS was identified as both • Based on this and RHS Project outcomes, SORH designed a study looking specifically at non-traditional utilization of existing EMS resources “the right care, at the right time, in the right setting, for the right cost” 2
The Changing Role of EMS… 3
EMS…Originally Designed for Emergencies • Identified, designed, and defined through the ‘ 60 s, ‘ 70 s, ‘ 80 s, ‘ 90 s • National curriculum updates in 1985, 1998, & 2009 have driven the industry toward standardization, accountability, and accreditation of educational programs • Initial education focuses on managing emergencies – Serves as an extension of the ED/ED physician – Prepared for, and good at that • However, not much about the response system has changed – Dial “ 9 -1 -1”; resources are dispatched – EMS arrives, conducts assessment, provides interventions – Transports patient to ED (or no transport at all) • Not prepared for how EMS is often used today 4
Where Does EMS Belong? • Emergency Medical Services – By appearance • Considered “Public Safety” – By performance • Medical Provider – Provides medical care – Significant skill-set & broad scope of practice – Designed for emergencies • Bills for “services” – Currently only gets 5
“ 9 -1 -1”; Too Easy/Too Often “Don’t Guess…Call EMS” The Results… • It worked • EMS is obligated to respond to 9 -1 -1 calls • EMS = Medical Care • Co-Dependent Relationship – Often calls are for primary care needs (“unscheduled” medical care) – Patient can request or refuse transport – Traditionally, only option was to transport to ED • Often recognized that ED is not appropriate place for patient’s needs • Bill for transport – Patients need medical care • Emergent or not; call 9 -1 -1 – EMS needs to transport patients to get paid • Emergent or not; transport to ED • Often taxes available resources – Not there for “real” emergencies • This cycle resulted in a need to re-examine the “big 6
Pushback: EMS Providers Want to Manage Emergencies E M E R G E N C I E S E M E R G E N C I N O N - 7
Today… • EMS/EMS personnel are being used differently than original design…prepared or not – Accept the metamorphosis & prepare for the transition • “ 9 -1 -1” calls are not all emergencies; must have pathway for non-emergency callers • Calls will continue; not likely to change habits of entire populations – Accept their role on the health care team 8
Patient Centered Care “…care that is respectful of and responsive to individual patient preferences, needs and values, ensuring that patient values guide all clinical decisions” 9
The Care Coordination Model 10

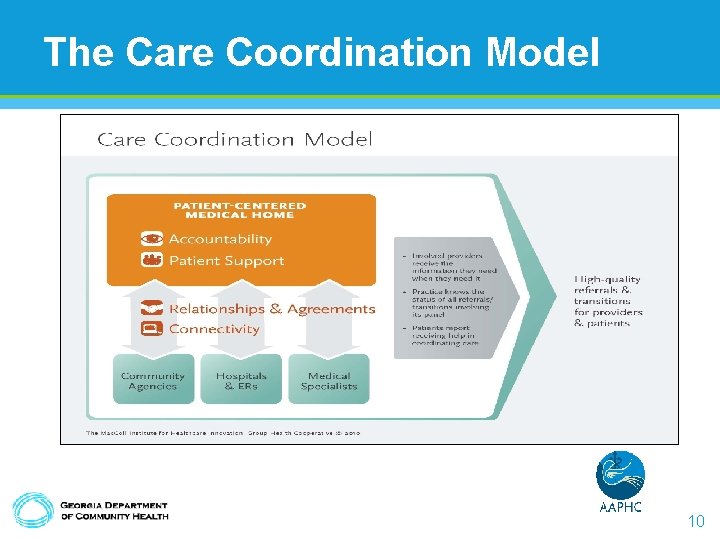
EMS & Care Coordination • Care coordination is “the deliberate organization of patientcare activities between two or more participants involved in a patient's care to facilitate the appropriate delivery of healthcare services. ” 11
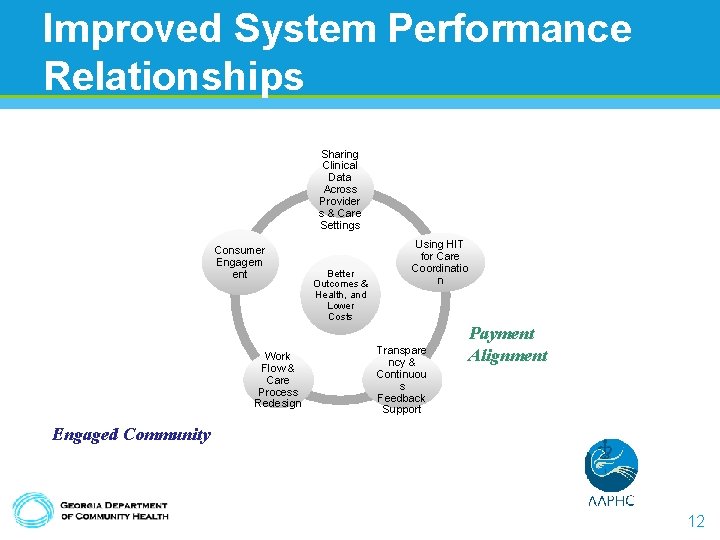
Improved System Performance Relationships Sharing Clinical Data Across Provider s & Care Settings Consumer Engagem ent Work Flow & Care Process Redesign Better Outcomes & Health, and Lower Costs Using HIT for Care Coordinatio n Transpare ncy & Continuou s Feedback Support Payment Alignment Engaged Community 12

Do Something New? Will I Get PAID? ? ? 13
Progress… 'The Moment We've Been Waiting For': Anthem to Compensate EMS Care Without Transport By John Erich Jan 02, 2018 Georgia Medicaid to Pay for Treatment on Scene, Alternative Destinations By G. Christopher Kelly Feb 26, 2018 14
Mobile Healthcare Access & Integration Pilot Study • Access: – verb • Approach or enter (a place). • Integrate: – verb • combine (one thing) with another so that they become a whole. 15
This is a WHOLISTIC Approach • Non-Emergency Component – Community Paramedicine Component of Program – Requires trained, dedicated CP staff – Requires coordination with hospital & others – Requires scheduling of appointments and home visits • Emergency Response Component – Additional options for those responding to “ 91 -1” calls – Requires addition of new protocols • Treat Without Transport • Transport to Alternate Destinations – Requires additional training for all EMS field staff 16
Overview of Pilot Study • This pilot study will evaluate the actual cost, benefit, and value of including EMS in care coordination for rural residents – Three Year Study Period • Fiscal Years 2018 (study designed), 2019, 2020 (implementation) – Program Divided into Two Phases • Phase One (FY 19) – Implementation of Mobile Integrated Healthcare/Community Paramedicine Program • Phase Two (FY 20) – Implementation of Transport to Alternate Destination and Treat Without Transport 17
Community Paramedicine/ Mobile Integrated Health Care What It Is… – Emerging healthcare profession allowing paramedics and EMTs to operate in expanded roles, providing routine health care services to underserved populations • What It Is Not… – Competition • Not intended to compete with Home Health Care or Hospice • Not intended to replace or reproduce services already available within any given community 18
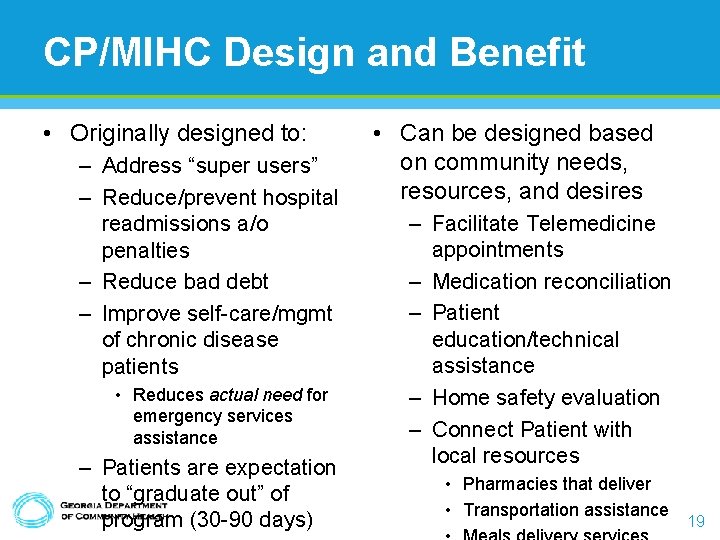
CP/MIHC Design and Benefit • Originally designed to: – Address “super users” – Reduce/prevent hospital readmissions a/o penalties – Reduce bad debt – Improve self-care/mgmt of chronic disease patients • Reduces actual need for emergency services assistance – Patients are expectation to “graduate out” of program (30 -90 days) • Can be designed based on community needs, resources, and desires – Facilitate Telemedicine appointments – Medication reconciliation – Patient education/technical assistance – Home safety evaluation – Connect Patient with local resources • Pharmacies that deliver • Transportation assistance 19
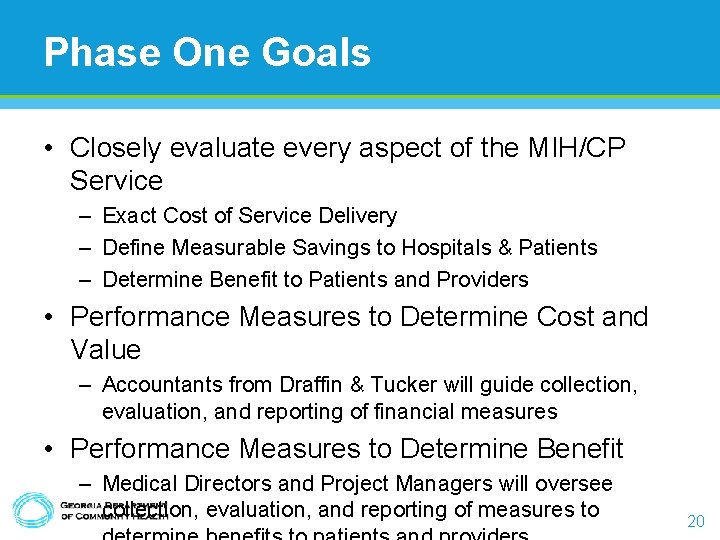
Phase One Goals • Closely evaluate every aspect of the MIH/CP Service – Exact Cost of Service Delivery – Define Measurable Savings to Hospitals & Patients – Determine Benefit to Patients and Providers • Performance Measures to Determine Cost and Value – Accountants from Draffin & Tucker will guide collection, evaluation, and reporting of financial measures • Performance Measures to Determine Benefit – Medical Directors and Project Managers will oversee collection, evaluation, and reporting of measures to 20
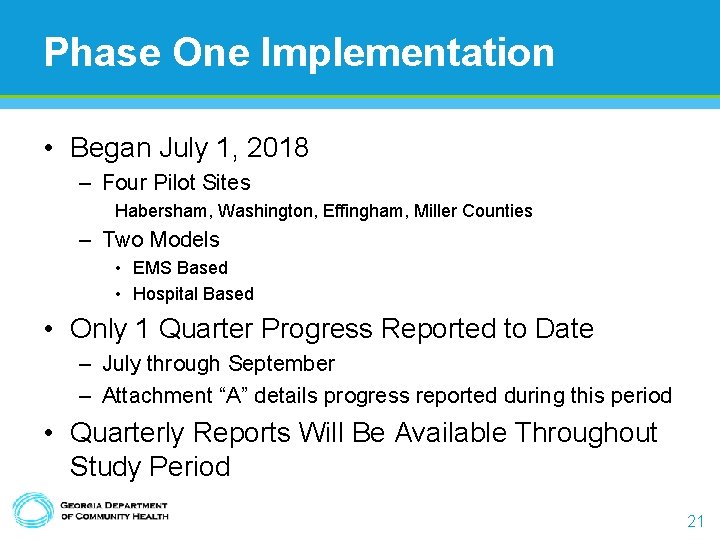
Phase One Implementation • Began July 1, 2018 – Four Pilot Sites Habersham, Washington, Effingham, Miller Counties – Two Models • EMS Based • Hospital Based • Only 1 Quarter Progress Reported to Date – July through September – Attachment “A” details progress reported during this period • Quarterly Reports Will Be Available Throughout Study Period 21
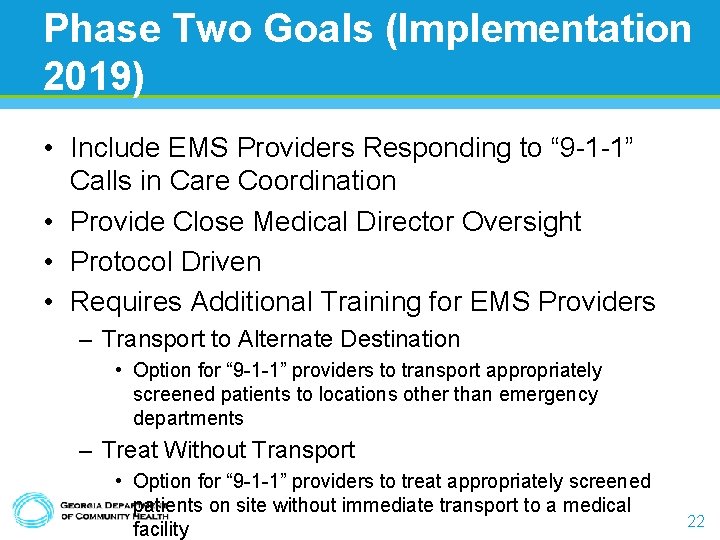
Phase Two Goals (Implementation 2019) • Include EMS Providers Responding to “ 9 -1 -1” Calls in Care Coordination • Provide Close Medical Director Oversight • Protocol Driven • Requires Additional Training for EMS Providers – Transport to Alternate Destination • Option for “ 9 -1 -1” providers to transport appropriately screened patients to locations other than emergency departments – Treat Without Transport • Option for “ 9 -1 -1” providers to treat appropriately screened patients on site without immediate transport to a medical facility 22
Transport… What they do now… • Assess patients and choose the most appropriate location for their continued care – “Closest appropriate facility” • Local ED • Trauma Centers • Cardiac/STEMI Centers • Stroke Centers • Burn Centers • Pediatric Emergency 23
Transport To Alternate Destinations What they need to do… • Assess patients and choose the most appropriate location for their continued care – “Closest appropriate facility” • Urgent Care Centers • Clinics • Doctor’s Offices • Behavioral Health Facilities • Dentist’s Offices – Stay local and use local 24
What is the Benefit of Alternate Destination? • Connects the patient with: – Appropriate site to address their needs – Possible permanent medical home – Less costly medical care • Keeps EMS resources in the county for emergencies • Utilizes/supports local resources • Reduce the burden to EDs • Reprograms patients from defaulting to “ 9 -1 -1” – Patient education opportunity 25
Treatment Without Transport • Some patients would benefit from treatment at scene without transport – Should be carefully supervised program • Decisions should be based on protocol • Could include MD consult via phone or telemedicine • Best if part of care coordination effort – Not intended to discourage transport of 26
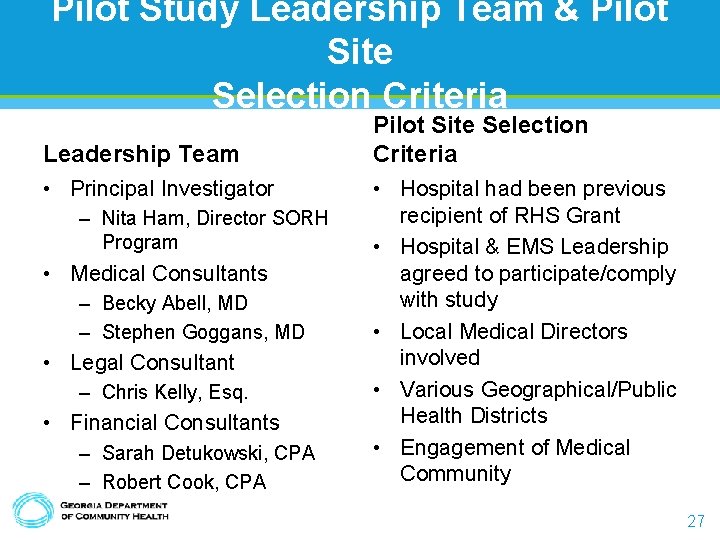
Pilot Study Leadership Team & Pilot Site Selection Criteria Leadership Team • Principal Investigator – Nita Ham, Director SORH Program • Medical Consultants – Becky Abell, MD – Stephen Goggans, MD • Legal Consultant – Chris Kelly, Esq. • Financial Consultants – Sarah Detukowski, CPA – Robert Cook, CPA Pilot Site Selection Criteria • Hospital had been previous recipient of RHS Grant • Hospital & EMS Leadership agreed to participate/comply with study • Local Medical Directors involved • Various Geographical/Public Health Districts • Engagement of Medical Community 27
What the Focus Should Be: Reduce Costs By Improving Care Patients REDUCING COSTS (WITHOUT RATIONING) Lower Costs 28
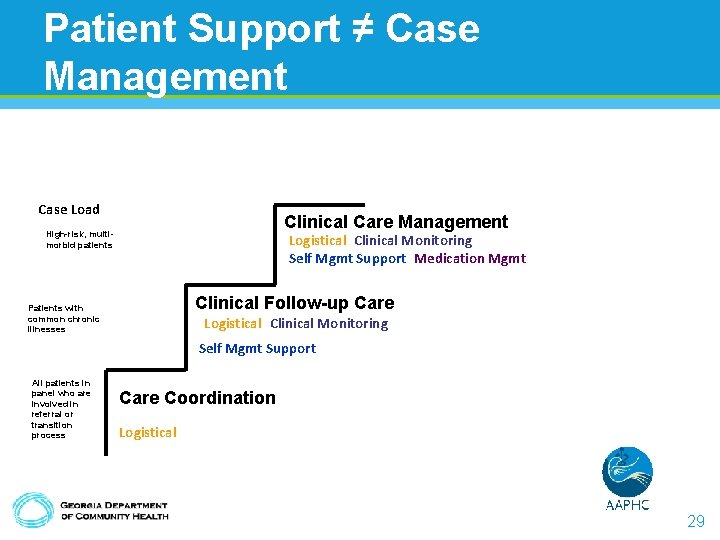
Patient Support ≠ Case Management Case Load Clinical Care Management High-risk, multimorbid patients Logistical Clinical Monitoring Self Mgmt Support Medication Mgmt Clinical Follow-up Care Patients with common chronic illnesses Logistical Clinical Monitoring Self Mgmt Support All patients in panel who are involved in referral or transition process Care Coordination Logistical 29
30
AAPHC Proposed Model Workflow v High risk patient identified by health centers based on 2+, 4+, 6+ chronic conditions, risk stratified by total expenditures v Patients loaded into “tiered queues” in Premedex System v Outreach for pre-education and verbal consent to care coordination * tasked to CC/CHW/interns/any staff member v Patient referred/tasked to appropriate CC based on tier v CC alerted for ”Initial Visit/Baseline enrollment” in Premedex or CCM System v CC contacts PCP/care team for pertinent information on patient v PCP/care team provides necessary info: recent med chart, updated med list, treatment plan * after enrollment/empanelment; patient should be placed on VIP status (ex. appt scheduling, communication/access to care team) v CC conducts initial visit-baseline enrollment/assessment(s) and educates on program/expectations for care coordination v CC is responsible in ensuring all patient referral loops are closed and monitored v CC conducts maintenance encounter based on agreed upon follow up plan * CCM billing: if health center is billing for CCM, care coordinator will utilize CCM module during maintenance encounters 31
Training A New Generation: Becoming A Team Member 32

Mission The mission of the Department of Community Health is to provide access to affordable, quality health care to Georgians through planning, purchasing and oversight We are dedicated to A Healthy Georgia. 33
- Slides: 34