Breathe Well Live Well An Asthma Management Program
Breathe Well, Live Well An Asthma Management Program for Adults. Chris Draft, Buffalo Bills Larry English, San Diego Chargers Larry Grant, St. Louis Rams Leonard Little, St. Louis Rams Adam Carriker, St. Louis Rams Gary Gibson, St. Louis Rams Ellis Lankster, Buffalo Bills Corey Chavous, St. Louis Rams Haruki Nakamura, Baltimore Ravens

Justine Henin Four-time French Open champ Jerome Bettis This bullish running back—aptly nicknamed “The Bus”— Jackie Joyner-Kersee Track-and-field star, four-time Olympian, and three-time gold medalist Paula Radcliffe The marathon Dennis Rodman Amy Van Dyken
� � � 23 million Americans suffer from asthma One of the most common chronic conditions among children. Third-ranking cause of hospitalization among children, Leading cause of school absenteeism, accounting for more than 14 million total missed days of school. Every DAY in America: � 78, 000 people miss school or work due to asthma � 35, 000 people have an asthma attack � 4, 600 people visit the emergency room due to asthma � 1, 200 people are admitted to the hospital due to asthma � 10 people die from asthma
No. 10: Greensboro, N. C. No. 9: St. Louis, Mo. High pollen levels and poor air quality contribute to big asthma issues No. 8: Greenville, S. C. Poor air quality and an above average use of controller medications No. 7: Charlotte, N. C. No. 6: Allentown, Pa. high prevalence of asthma and a low number of asthma specialists No. 5: Memphis, Tenn. high poverty rates and poor air quality; less access to health care and medications No. 4: Atlanta, Ga. No. 3: Milwaukee, Wis. air quality and is worse than the national average for the use of "rescue" asthma medications. No. 2: Tulsa, Okla. high prevalence of asthma and a low number of asthma specialists, according to data compiled by the AAFA. . No. 1: Knoxville, Tenn. High pollen counts, poor air quality, the lack of a smoking ban in all public places, and the above average usage of asthma medications all contribute to this distinction.
� Affects one in every 15 children. � New cases and hospitalization increased 30% over the past 20 years. � Asthma deaths among young people have more than DOUBLED.
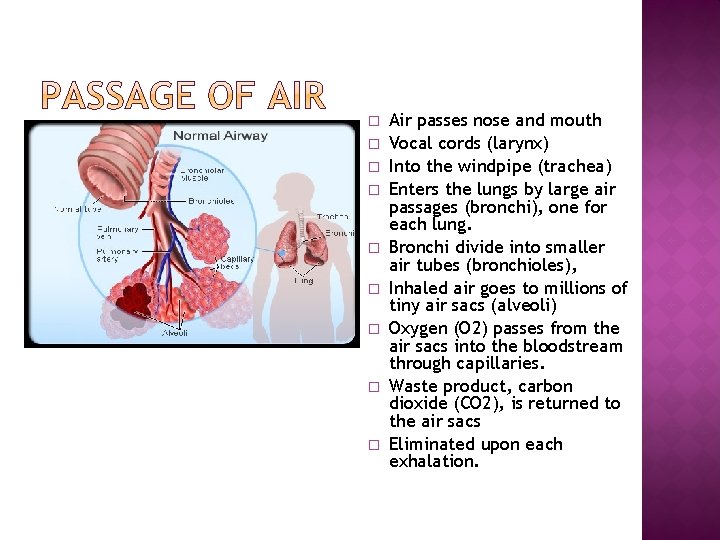
� � � � � Air passes nose and mouth Vocal cords (larynx) Into the windpipe (trachea) Enters the lungs by large air passages (bronchi), one for each lung. Bronchi divide into smaller air tubes (bronchioles), Inhaled air goes to millions of tiny air sacs (alveoli) Oxygen (O 2) passes from the air sacs into the bloodstream through capillaries. Waste product, carbon dioxide (CO 2), is returned to the air sacs Eliminated upon each exhalation.
http: //video. about. com/? bcpid=42795866 001&bclid=0&bctid=1711771025 • Narrowing of ONLY the bronchial tubes • Does not affect alveoli (air sacs) or the lung tissue.
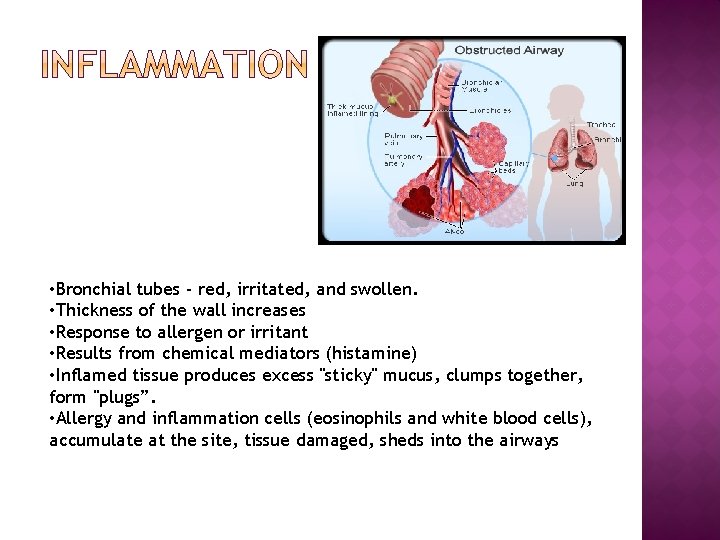
• Bronchial tubes - red, irritated, and swollen. • Thickness of the wall increases • Response to allergen or irritant • Results from chemical mediators (histamine) • Inflamed tissue produces excess "sticky" mucus, clumps together, form "plugs”. • Allergy and inflammation cells (eosinophils and white blood cells), accumulate at the site, tissue damaged, sheds into the airways
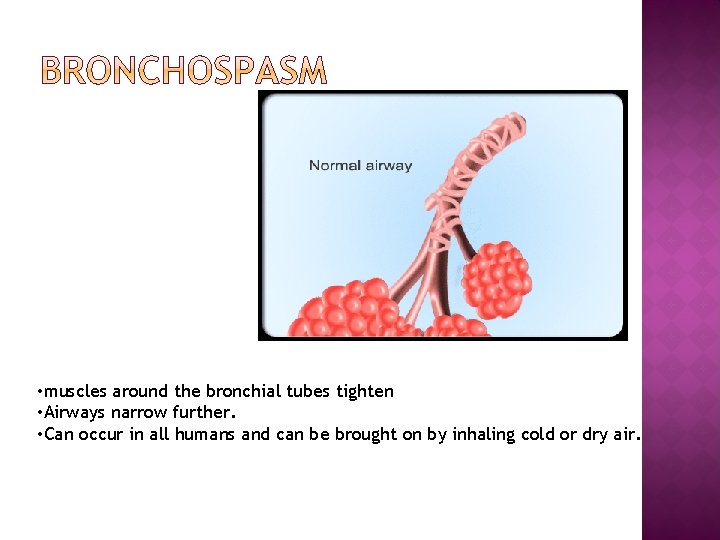
• muscles around the bronchial tubes tighten • Airways narrow further. • Can occur in all humans and can be brought on by inhaling cold or dry air.
• Chronically inflamed and constricted airways become highly sensitive, or reactive, to triggers. • allergens, • irritants, • and infections. • Exposure to these triggers may result in progressively more inflammation and narrowing.
• Not all asthmatics react to the same triggers. • Effect on the lungs varies from one individual to another. • Severity depends on 1. # agents activate your symptoms. 2. How sensitive your lungs are to them. • Triggers worsen nasal or eye symptoms.
• "Seasonal" pollens • Year-round dust mites, molds, pets, and insect parts • Foods: fish, egg, peanuts, cow's milk, and soy additives, such as sulfites • Latex
• Respiratory infections (viral "colds, " bronchitis, and sinusitis) • Aspirin, NSAIDs and beta blockers (used to treat blood pressure and other heart conditions) • Tobacco smoke • Outdoor factors: smog, weather changes, and diesel fumes • Indoor factors: paint, detergents, deodorants, chemicals, and perfumes • NIGHTTIME GERD (gastroesophageal reflux disorder) • Exercise, especially under cold dry conditions • Work-related factors: chemicals, dusts, gases, and metals • Emotional factors: laughing, crying, yelling, and distress • Hormonal factors: premenstrual syndrome
• Starts in early childhood (90% of all cases) from 2 -6 years of age, linked to exposure to allergens, • Allergic asthma , remission in early adulthood. • 75% of cases, asthma reappears later.
• Adult-onset asthma, 10% of all cases, occurs more often in middle-aged women, • frequently follows a respiratory tract infection. . • usually develops after the age of 30 and is not typically associated with allergies. • show up in your 50 s, 60 s, or even later. • chronic and year-round. • People with cat allergies are vulnerable
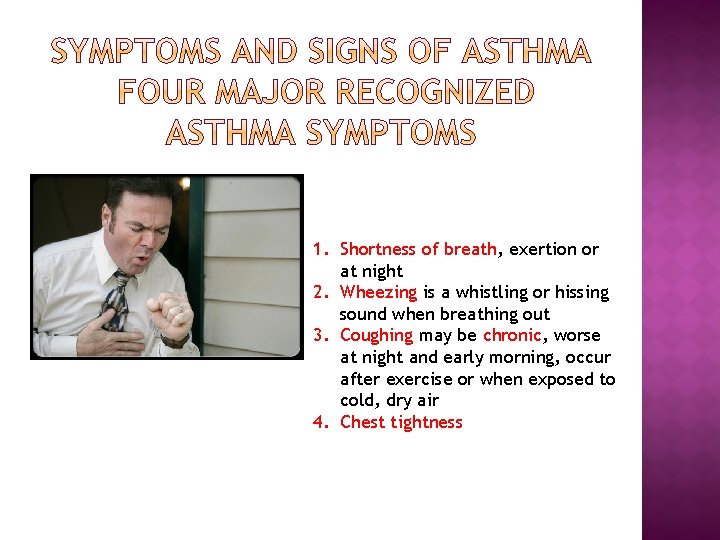
1. Shortness of breath, exertion or at night 2. Wheezing is a whistling or hissing sound when breathing out 3. Coughing may be chronic, worse at night and early morning, occur after exercise or when exposed to cold, dry air 4. Chest tightness
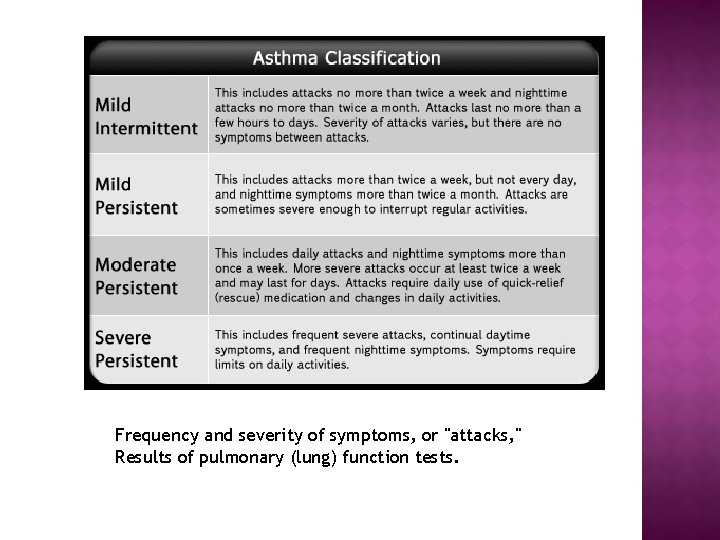
Frequency and severity of symptoms, or "attacks, " Results of pulmonary (lung) function tests.
• Potentially life-threatening • may continue despite the use of your usual quick-relief medications (inhaled bronchodilators). • unresponsive to treatment with an inhaler seek medical attention • Asthma attacks do not stop on their own. • If you ignore early warning signs, your at risk of developing a life-threatening asthma reaction called status asthmaticus.
1. Pulmonary function tests (spirometer, or peak flow meter) which measure lung function. 2. Allergy testing 3. Immunoglobulin E (Ig. E), a key antibody that's released during an allergic reaction. 4. X-ray exam to make sure nothing else is causing your asthma symptoms. 5. Look for coexisting conditions such as allergies, GERD, or sinusitis.
MEDICATIONS • Bronchodilators/ inhalers to relax bronchospasm • Corticosteroids reduce inflammation • Inhaled medications preferred over tablet or liquid medicines 1. act directly on the airway surface and airway muscles. 2. Absorption into body is minimal; side effects are fewer. 3. Oral medications include aminophylline.
People who have no triggers; do not experience asthma under any other circumstances. 1. More sensitive to changes in temperature and humidity. 2. Airways swell (bronchospasm) and secrete large amounts of mucus. 3. Partially block or obstruct the airways. Untreated and inflammation persists, permanent narrowing of the airways referred to as chronic obstructive pulmonary disease (COPD), like emphysema and chronic bronchitis. Rest breathe through your nose. Warms, humidifies, and cleanses the air. Exercising breathe through your mouth. Air that hits your lungs is colder and drier.
• Start, five to 20 minutes after beginning to exercise. • Peak , five to 10 minutes after stopping exercise then gradually diminish. • Gone within an hour. One or a combination of the following: 1. Coughing 2. Wheezing Chest tightness 3. Chest pain Prolonged shortness of breath 4. Extreme fatigue
1. Warming up 2. Gradually cooling down after exertion Avoid exertion when you have a respiratory tract infection, such as a cold, flu, or bronchitis. Avoid exertion in extremely cold weather. 3. If you smoke, quit. 4. If you have allergies, avoid exertion when a reaction is likely to be triggered, as when the pollen count or pollution index is high.
1. Take before exercise. • Two to four puffs, five to 30 minutes before exercising. • Work rapidly (within minutes) to open the breathing passages. • Relax and dilate the muscles of the breathing passages, • Decrease resistance to exhaled air. • Last four to six hours. ALBUTEROL (PROVENTIL, VENTOLIN), SEREVENT Corticosteroids: Flovent, and Asmanex are taken a few hours before exercise With appropriate treatment, almost everyone with EIA can enjoy the mental and physical benefits of regular exercise.
SUPPORT GROUPS AND COUNSELING Allergy & Asthma Network Mothers of Asthmatics 2751 Prosperity Avenue, Suite 150 Fairfax, VA 22031 1 -800 -878 -4403 American Lung Association 61 Broadway, 6 th Floor New York, NY 10006 212 -315 -8700 Asthma and Allergy Foundation of America 1233 20 th St NW, Suite 402 Washington, DC 20636 202 -466 -7643
WEB LINKS Allergy & Asthma Network Mothers of Asthmatics American Academy of Allergy, Asthma & Immunology American Lung Association Asthma and Allergy Foundation of America National Asthma Education and Prevention Program, National Heart, Lung, and Blood Institute (NHLBI), National Institutes of Health, Lung Diseases Information National Institute of Allergy and Infectious Diseases National Institutes of Health
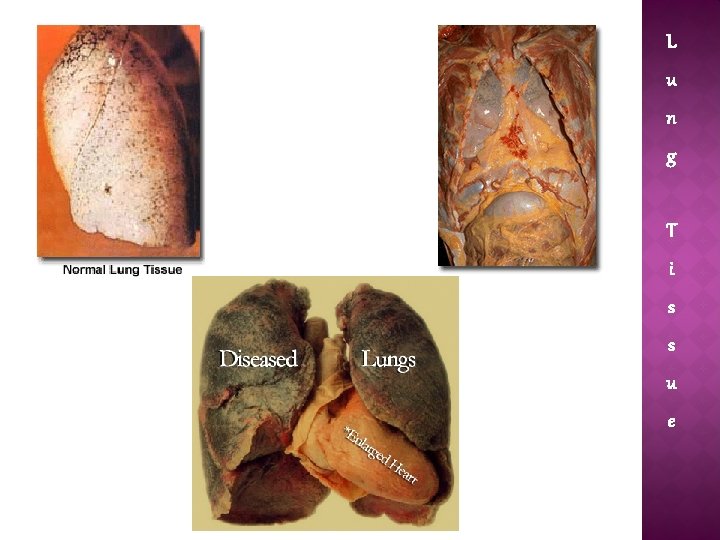
L u n g T i s s u e
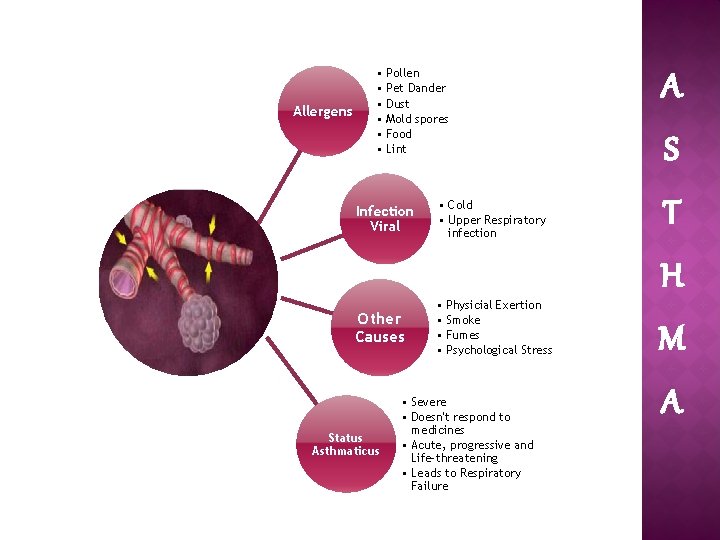
Allergens • Pollen • Pet Dander • Dust • Mold spores • Food • Lint Infection Viral Other Causes Status Asthmaticus • Cold • Upper Respiratory infection • Physicial Exertion • Smoke • Fumes • Psychological Stress • Severe • Doesn't respond to medicines • Acute, progressive and Life-threatening • Leads to Respiratory Failure A S T H M A
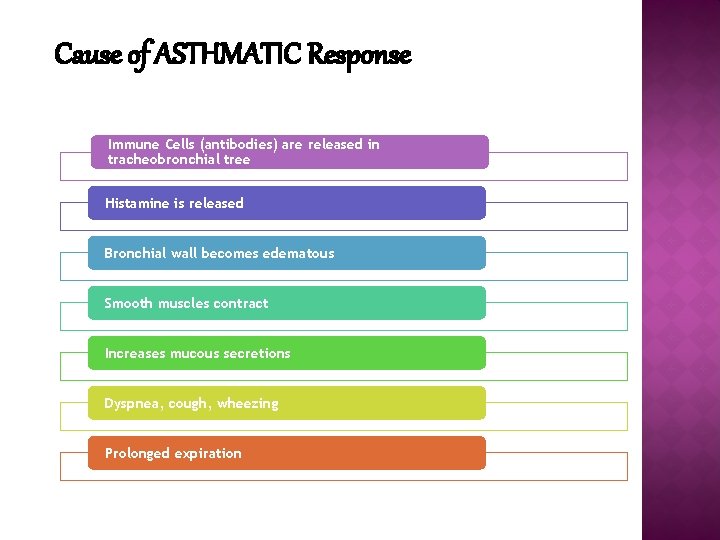
Cause of ASTHMATIC Response Immune Cells (antibodies) are released in tracheobronchial tree Histamine is released Bronchial wall becomes edematous Smooth muscles contract Increases mucous secretions Dyspnea, cough, wheezing Prolonged expiration
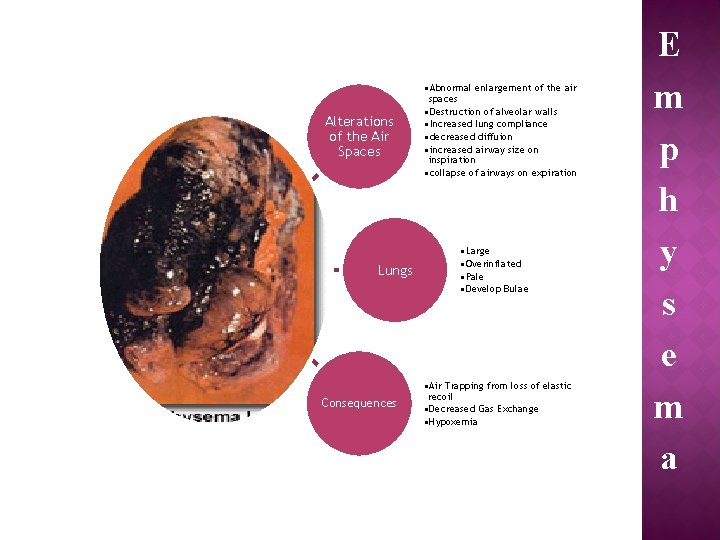
Alterations of the Air Spaces Lungs Consequences • Abnormal enlargement of the air spaces • Destruction of alveolar walls • Increased lung compliance • decreased diffuion • increased airway size on inspiration • collapse of airways on expiration • Large • Overinflated • Pale • Develop Bulae • Air Trapping from loss of elastic recoil • Decreased Gas Exchange • Hypoxemia E m p h y s e m a
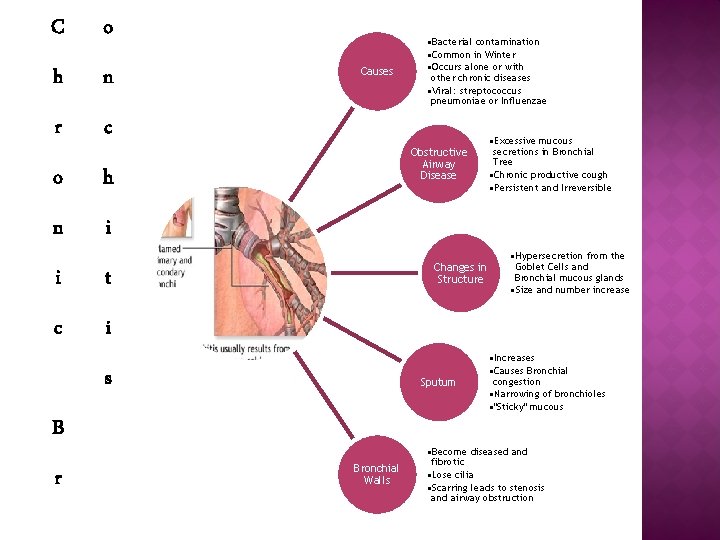
C o h n r c o h n i i t c i Causes Obstructive Airway Disease Changes in Structure s Sputum B r • Bacterial contamination • Common in Winter • Occurs alone or with other chronic diseases • Viral: streptococcus pneumoniae or Influenzae Bronchial Walls • Excessive mucous secretions in Bronchial Tree • Chronic productive cough • Persistent and Irreversible • Hypersecretion from the Goblet Cells and Bronchial mucous glands • Size and number increase • Increases • Causes Bronchial congestion • Narrowing of bronchioles • "Sticky" mucous • Become diseased and fibrotic • Lose cilia • Scarring leads to stenosis and airway obstruction
- Slides: 31