Breastfeeding Support in the Pharmacy Lottie Charlotte Louise
Breastfeeding Support in the Pharmacy “Lottie” Charlotte Louise Ayres MPharm MRPharm. S GPh. C 2068942 “Tree of Life” by Pino Conte NGV, Melbourne, Australia
Hello… Industry (R&D) Community Hospital Final year of chemistry Ph. D Community Locum (Hartlepool) Equality Mental health Infant + Perinatal health
*IMPORTANT* Should NOT be controversial It’s NOT forcing someone to breastfeed It’s NOT telling everyone breastfeeding is best It’s NOT about causing guilt It is ensuring access to: • all the evidence-based INFORMATION • the right SUPPORT to enable parents to make their own informed decision. 3 of 23
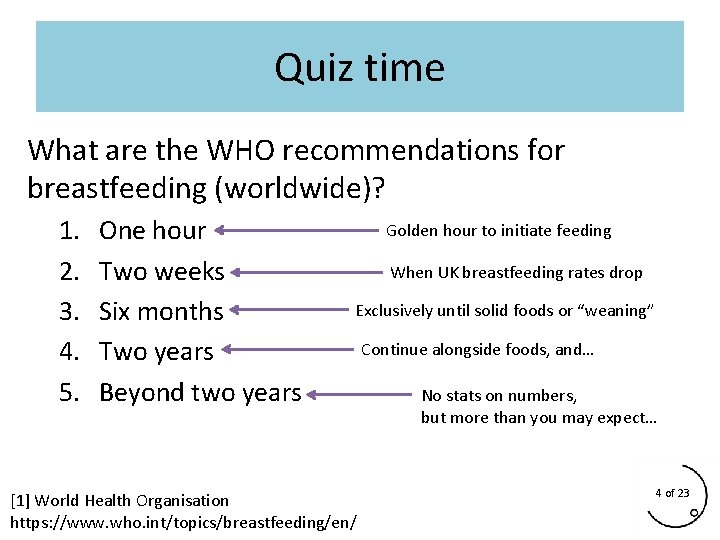
Quiz time What are the WHO recommendations for breastfeeding (worldwide)? 1. 2. 3. 4. 5. One hour Two weeks Six months Two years Beyond two years Golden hour to initiate feeding When UK breastfeeding rates drop Exclusively until solid foods or “weaning” [1] World Health Organisation https: //www. who. int/topics/breastfeeding/en/ Continue alongside foods, and… No stats on numbers, but more than you may expect… 4 of 23
The stats: % of mothers initiating feeding in England? England – 79% vs North East – 59% vs Hartlepool – 38% [2] % of mothers feeding 6 -8 weeks after birth? England – 42. 7% vs North East – 32. 1% vs Norway – 71% [3] “The overwhelming majority of mothers stop before they want to” [4] Why? • • lack of local support (public health cuts) social stigma lack of family support inconsistent messaging from healthcare professionals 5 of 23
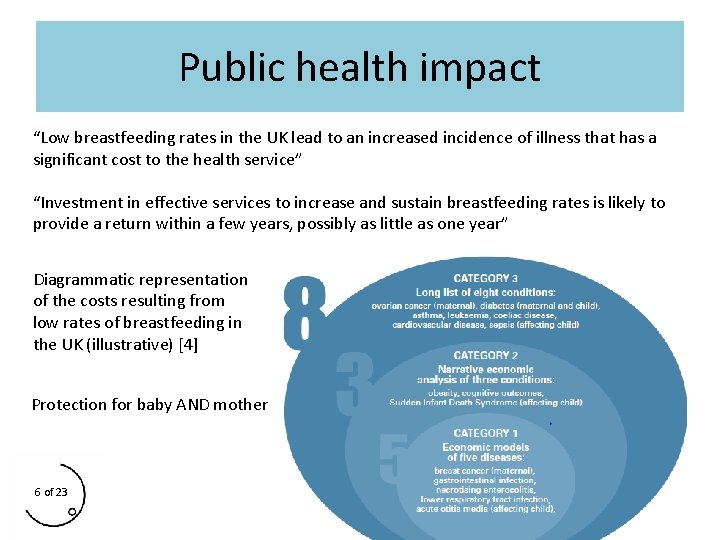
Public health impact “Low breastfeeding rates in the UK lead to an increased incidence of illness that has a significant cost to the health service” “Investment in effective services to increase and sustain breastfeeding rates is likely to provide a return within a few years, possibly as little as one year” Diagrammatic representation of the costs resulting from low rates of breastfeeding in the UK (illustrative) [4] Protection for baby AND mother 6 of 23
Breastfeeding Basics It should NOT hurt or damage nipples! Regulated by: • Prolactin • Oxytocin Milk production depends on removal of milk Accumulation of milk in breast due to restricted feeding or poor attachment or poor drainage results in decreased production by means of negative feedback (inhibition of lactation) Factory not a warehouse! 7 of 23
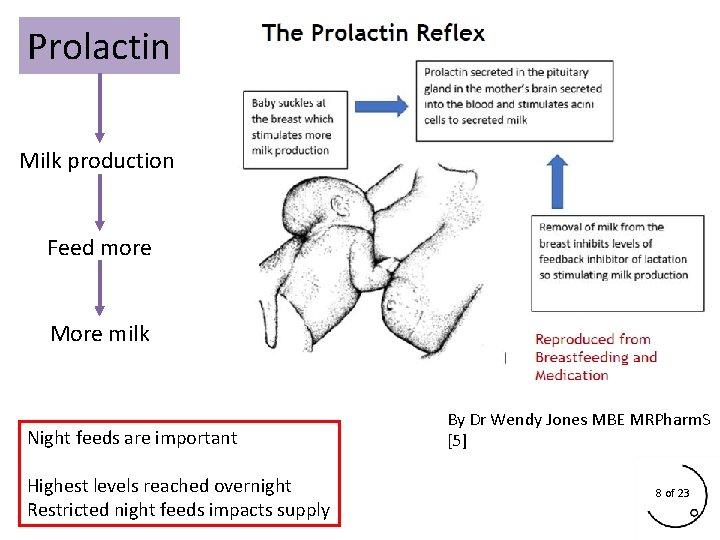
Prolactin Milk production Feed more More milk Night feeds are important Highest levels reached overnight Restricted night feeds impacts supply By Dr Wendy Jones MBE MRPharm. S [5] 8 of 23
![Oxytocin Milk ejection Skin-on-skin [6] Golden hour Infant too! By Dr Wendy Jones MBE Oxytocin Milk ejection Skin-on-skin [6] Golden hour Infant too! By Dr Wendy Jones MBE](http://slidetodoc.com/presentation_image_h/0b454f043a95f1816024688ddc9343aa/image-9.jpg)
Oxytocin Milk ejection Skin-on-skin [6] Golden hour Infant too! By Dr Wendy Jones MBE MRPharm. S [5] 9 of 23
Commonly seen problems • • Sore nipples* -> positioning & attachment, protect supply Engorgement -> protect supply, prevent mastitis Mastitis -> requires frequent effective drainage and ibuprofen Thrush -> may be incorrectly diagnosed, often a latch problem • Insufficient supply -> often perceived by mother but less frequently seen, check weight gain & dirty nappies, and remember that adding formula reduces supply in the long term! • Normal to feed every 2 -3 hours in the first three months • All require expert support -> SIGNPOSTING * Why most women give up! 10 of 23

What can we do in the Pharmacy? • • & • Evidence-based support: #dontsaystoplookitup Signposting to local breastfeeding experts Public health campaigns Local group info Safe place to feed (just a chair!) Equality Act 2010: A business cannot discriminate against mothers who are breastfeeding a child of any age 11 of 23
Alcohol risks • Chronic exposure • More than 2 units per day • May impact on baby’s development Context: 300 mg per 100 m. L maternal level = mild sedation in baby (80 mg / 100 m. L to fail police breath test in UK) • Binge drinking • More than 5 -6 units in one “session” • Two large (250 m. L) glasses of wine • “Essential that a sober adult cares for baby until mother is able to” More info: page 230 of Breastfeeding & Medication or BFN factsheet online 12 of 23
Alcohol & breastfeeding • “Breastfeeding mothers can have occasional, small amounts of alcohol but should not drink regularly or heavily (e. g. binge drinking) without considering how to limit the baby’s exposure” [7] • Consider baby’s age & prematurity [8] • Levels are highest 30 -90 mins after drinking • Alcohol passes freely in and out of breastmilk so it isn’t necessary to express to clear it of alcohol A MOTHER SHOULD NEVER PUT YOURSELF INTO A SITUATION WHERE SHE COULD FALL ASLEEP WITH BABY AFTER DRINKING 13 of 23
![Smoking & breastfeeding • • • Exposure to smoke increases risk of SIDS [9] Smoking & breastfeeding • • • Exposure to smoke increases risk of SIDS [9]](http://slidetodoc.com/presentation_image_h/0b454f043a95f1816024688ddc9343aa/image-14.jpg)
Smoking & breastfeeding • • • Exposure to smoke increases risk of SIDS [9] Nicotine is found in breastmilk – may increase risk of colic [10] May reduce mother’s supply [10] Restrict to just after feeds to reduce amount in breastmilk It is NOT a reason to stop breastfeeding, still beneficial Considering giving up? • NRT (gum, patches, lozenges, nasal spray, inhalator) -> safe to use, good time to give up (free prescriptions) • Bupropion (Zyban) -> not a reason to stop breastfeeding (Lact. Med) • Varenicline (Champix) -> use alternative if possible (Lact. Med) • E-cigs and vaping –> safer than smoking Page 239 -242 of Breastfeeding & Medication or BFN factsheet online 14 of 23
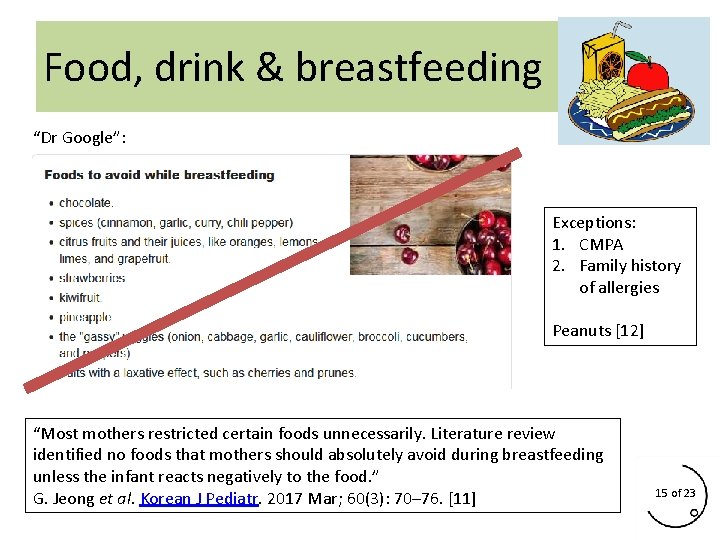
Food, drink & breastfeeding “Dr Google”: Exceptions: 1. CMPA 2. Family history of allergies Peanuts [12] “Most mothers restricted certain foods unnecessarily. Literature review identified no foods that mothers should absolutely avoid during breastfeeding unless the infant reacts negatively to the food. ” G. Jeong et al. Korean J Pediatr. 2017 Mar; 60(3): 70– 76. [11] 15 of 23
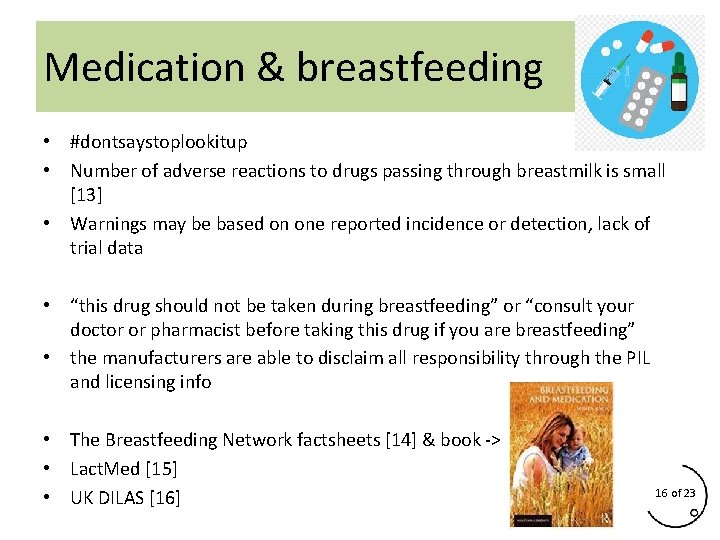
Medication & breastfeeding • #dontsaystoplookitup • Number of adverse reactions to drugs passing through breastmilk is small [13] • Warnings may be based on one reported incidence or detection, lack of trial data • “this drug should not be taken during breastfeeding” or “consult your doctor or pharmacist before taking this drug if you are breastfeeding” • the manufacturers are able to disclaim all responsibility through the PIL and licensing info • The Breastfeeding Network factsheets [14] & book -> • Lact. Med [15] • UK DILAS [16] 16 of 23
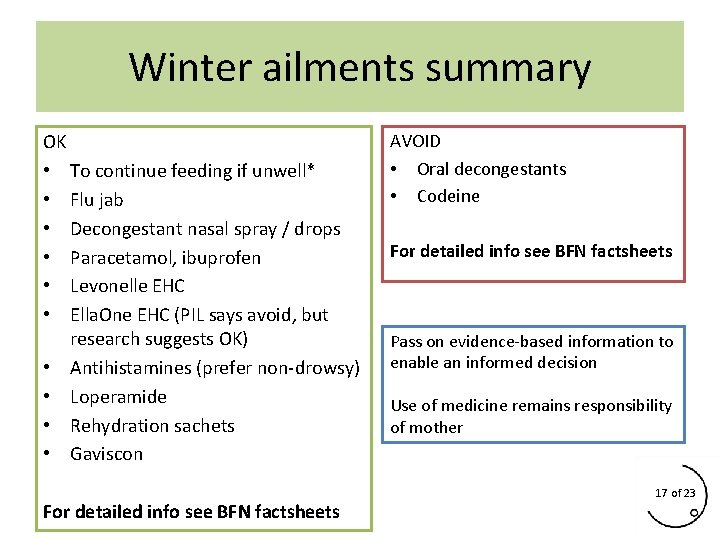
Winter ailments summary OK • To continue feeding if unwell* • Flu jab • Decongestant nasal spray / drops • Paracetamol, ibuprofen • Levonelle EHC • Ella. One EHC (PIL says avoid, but research suggests OK) • Antihistamines (prefer non-drowsy) • Loperamide • Rehydration sachets • Gaviscon For detailed info see BFN factsheets AVOID • Oral decongestants • Codeine For detailed info see BFN factsheets Pass on evidence-based information to enable an informed decision Use of medicine remains responsibility of mother 17 of 23
*If mother is unwell • Mother’s immune response to environment or illness provides rapid passive immunisation of child via breastmilk • Contains immunoglobulins (antibodies), leukocytes (mainly neutrophils and macrophages) and lactoferrin • Aids baby’s immune response in numerous ways and provides long lasting protection [17]
Printable leaflets from: 18 of 23
Dr Wendy Jones, MBE MRPharm. S 19 of 23
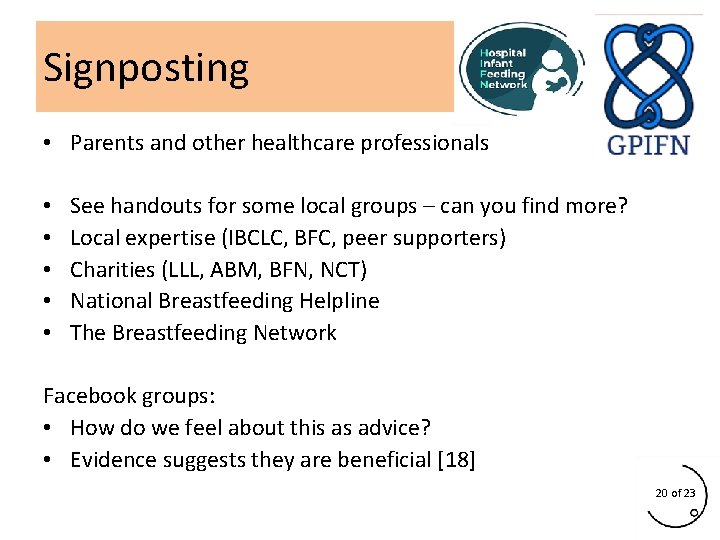
Signposting • Parents and other healthcare professionals • • • See handouts for some local groups – can you find more? Local expertise (IBCLC, BFC, peer supporters) Charities (LLL, ABM, BFN, NCT) National Breastfeeding Helpline The Breastfeeding Network Facebook groups: • How do we feel about this as advice? • Evidence suggests they are beneficial [18] 20 of 23
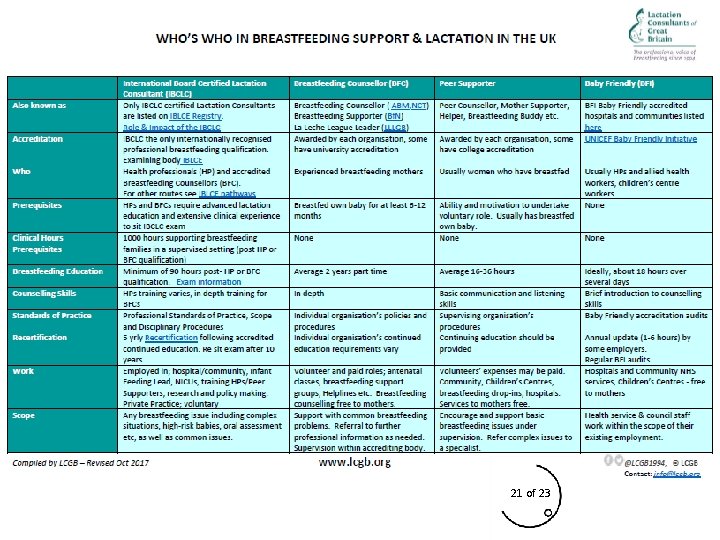
Who can help? 21 of 23

Where can I find out more? • Wendy’s online training for Pharmacists & books www. breastfeeding-and-medication. co. uk • Turas breastfeeding training (NHS Education for Scotland) • Train to volunteering with The Breastfeeding Network • Train to volunteering with The Association of Breastfeeding Mothers • CPPE training package online (Wendy’s) SIGNPOSTING HANDOUTS 22 of 23
Thank you for listening! “The success or failure of breastfeeding should not be seen solely as the responsibility of the woman” Dr Nigel Rollins, WHO 2016 “Verity” by Damien Hirst Ilfracombe, Devon The End
![• • • • • References from presentation: [1] World Health Organisation -> • • • • • References from presentation: [1] World Health Organisation ->](http://slidetodoc.com/presentation_image_h/0b454f043a95f1816024688ddc9343aa/image-25.jpg)
• • • • • References from presentation: [1] World Health Organisation -> https: //www. who. int/topics/breastfeeding/en/ [2] 2017/18 Director of Public Health Report for Hartlepool Borough Council -> https: //www. hartlepool. gov. uk/downloads/download/309/director_of_public_health_annual_report [3] 2017/18 Breastfeeding statistics -> https: //www. gov. uk/government/statistics/breastfeeding-at-6 -to-8 -weeksafter-birth-annual-data [4] Unicef resources -> https: //www. unicef. org. uk/babyfriendly/about/preventing-disease-and-saving-resources/ [5] Breastfeeding and medication book -> https: //www. breastfeeding-and-medication. co. uk/ [6] The Uvnäs Moberg K. , Prime D. K. Oxytocin effects in mothers and infants during breastfeeding. Infant 2013; 9(6): 201 -06. -> http: //www. infantjournal. co. uk/pdf/inf_054_ers. pdf [7] Breastfeeding Network factsheet on alcohol -> https: //www. breastfeedingnetwork. org. uk/alcohol/ [8] La Leche League info on alcohol -> https: //www. laleche. org. uk/alcohol-and-breastfeeding/ [9] Sudden Infant Death Syndrome and Smoking -> https: //www. who. int/tobacco/media/en/mitchell. pdf [10] Lact. Med info on nicotine -> https: //www. ncbi. nlm. nih. gov/books/NBK 501586/ [11] Foods to avoid during breastfeeding -> G. Jeong et al. Korean J Pediatr. 2017 Mar; 60(3): 70– 76. [12] Peanut allergies and breastfeeding -> Pitt TJ, Becker AB, Chan-Yeung M, Chan ES, Watson WTA, Chooniedass R, Azad MB (2017) J Allergy Clin Immunol. 2017 Aug. pii: S 0091 -6749(17)31104 -1. doi: 10. 1016/j. jaci. 2017. 06. 024. [13] Anderson PO, Pochop SL, Manoguerra AS. Adverse Drug Reactions in Breastfed Infants: Less Than Imagined. Clinical Pediatrics, 2003; 42(4): 325 -340). [14] the breastfeeding network factsheets -> https: //www. breastfeedingnetwork. org. uk/drugs-factsheets/ [15] Lact Med online -> https: //www. ncbi. nlm. nih. gov/books/NBK 501922/ [16] UKDILAS -> https: //www. sps. nhs. uk/articles/ukdilas-general-principles-for-medicine-use-during-breastfeeding/ [17] doi. org/10. 1371/journal. pone. 0156762 -> https: //journals. plos. org/plosone/article? id=10. 1371/journal. pone. 0156762 [18] online support -> https: //internationalbreastfeedingjournal. biomedcentral. com/articles/10. 1186/s 13006 -0180166 -9
- Slides: 25