Breast Cancer Katherine Mac Gillivray Melissa Poirier Objectives
Breast Cancer Katherine Mac. Gillivray & Melissa Poirier
Objectives Discuss breast cancer statistics in Canada and Nova Scotia. Overview of the breasts anatomy and physiology. Discuss risk factors for breast cancer and how to minimize those risks. Discuss differences between benign, non-invasive and invasive breast disease. Brief overview of breast cancer in men. Discuss types of lymph node involvement. Discuss screening options for breast cancer. Discuss diagnostic tests used for breast cancer. Discuss grading & staging of breast cancer. What are the treatment options for breast cancer? Discuss complications and prognosis of breast cancer. Discuss pre/postoperative nursing diagnosis and interventions.
Canadian Statistics for 2012 In Canada, 200 men & 23, 000 women will be diagnosed with breast cancer in 2012. Of that, 50 men & 5100 women will succumb to the disease. Breast cancer accounts for 26% of new cancer cases in Canadian women. Approximately 62 Canadian women are diagnosed with breast cancer daily. Approximately 14 Canadian women die daily of breast cancer. 1 in 9 women will develop breast cancer in their lifetime and 1 in 29 will die from it.
Statistics in Nova Scotia for 2012 An estimated 740 women will be diagnosed with breast cancer. An estimated 160 women will die of breast cancer. 100 out of every 100, 000 women of NS will be diagnosed with breast cancer. Of 100, 000 deaths, 20 women will die as the result of breast cancer. In Nova Scotia, there is limited data available for breast cancer in men. Men succumb to prostate, colorectal and lung cancers.
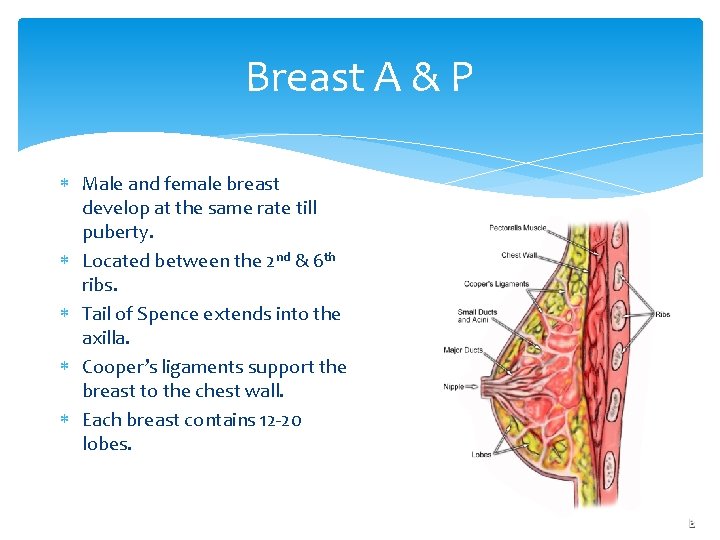
Breast A & P Male and female breast develop at the same rate till puberty. Located between the 2 nd & 6 th ribs. Tail of Spence extends into the axilla. Cooper’s ligaments support the breast to the chest wall. Each breast contains 12 -20 lobes.

Risk Factors Personal Health History Family Health History Certain Genome Changes Radiation Therapy to the Chest Reproductive and Menstruation History Race Being Overweight or Obese after Menopause Lack of Physical Activity Alcohol Use Smoking Age
Minimizing Your Risk Lose excess weight. Be physically active. Limit your intake of alcohol. Breastfeed your baby. Quit smoking. Talk to your doctor about the risks and benefits of hormone replacement therapy (HRT). Reduce exposure to chemicals
Benign Proliferative Breast Disease Atypical Hyperplasia Benign Abnormal proliferation of cells Increased risk of breast cancer Lobular Carcinoma in Situ Benign Proliferation of cells in the lobules Unable to be diagnosed with a Mammogram Increased risk of breast cancer
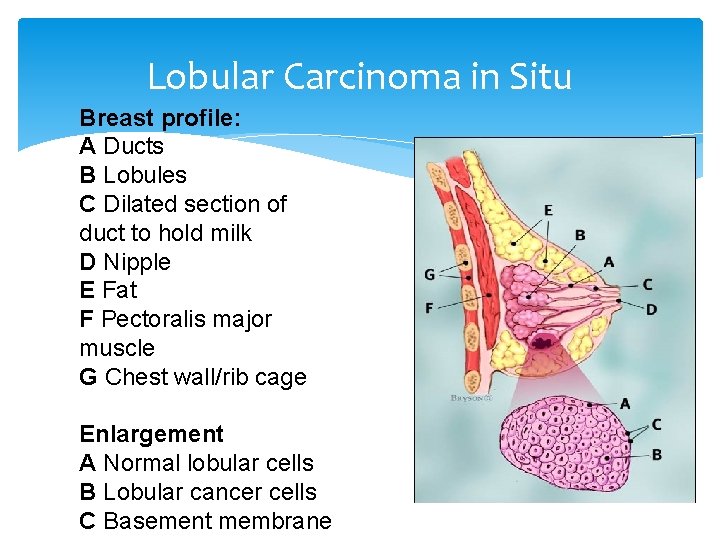
Lobular Carcinoma in Situ Breast profile: A Ducts B Lobules C Dilated section of duct to hold milk D Nipple E Fat F Pectoralis major muscle G Chest wall/rib cage Enlargement A Normal lobular cells B Lobular cancer cells C Basement membrane
Types of Breast Cancer: Non-Invasive vs. Invasive Non-Invasive Cancer Ductal Carcinoma in Situ Invasive Cancer Infiltrating Ductal Carcinoma Infiltrating Lobular Carcinoma Medullary Carcinoma Mucinous Carcinoma Tubular Ductal Carcinoma Inflammatory Carcinoma Paget’s Disease

Ductal Carcinoma in Situ Breast profile: A Ducts B Lobules C Dilated section of duct to hold milk D Nipple E Fat F Pectoralis major muscle G Chest wall/rib cage Enlargement A Normal duct cells B Ductal cancer cells C Basement membrane D Lumen (center of duct)

Non-Invasive (In Situ) Cell Growth Subtypes Non-invasive cancer is grouped into four subcategories, based on how the cancer cells grow relative to each other, within the center of the milk duct: Solid Cribriform Papillary Comedo

Solid: There is wall-to wall cell growth A - Cancer cells B - Basement membrane

Cribriform: There are holes between groups of cancer cells, making it look like Swiss cheese. A - Cancer Cells B - Basement membrane C - Lumen (center of duct)
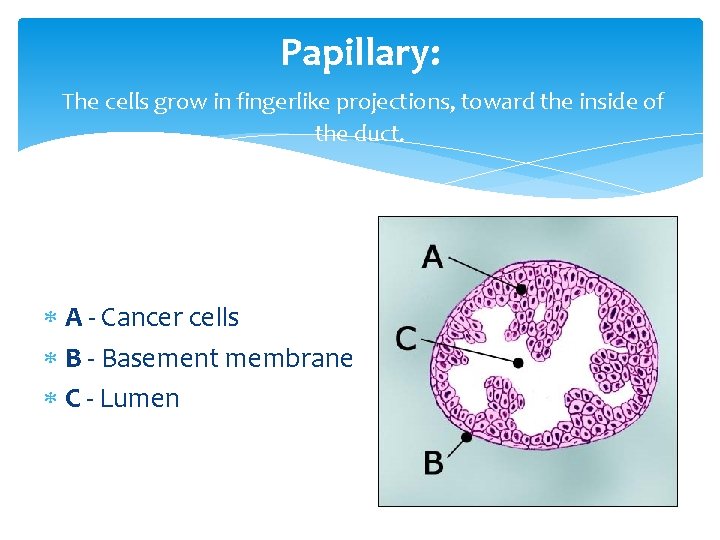
Papillary: The cells grow in fingerlike projections, toward the inside of the duct. A - Cancer cells B - Basement membrane C - Lumen
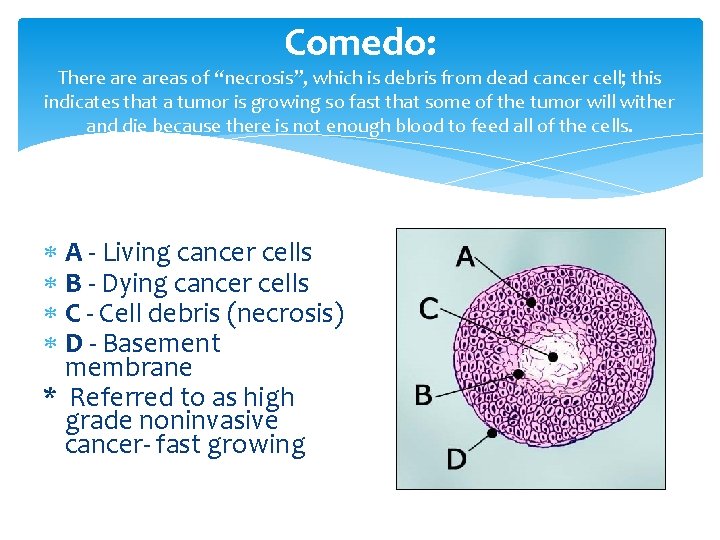
Comedo: There areas of “necrosis”, which is debris from dead cancer cell; this indicates that a tumor is growing so fast that some of the tumor will wither and die because there is not enough blood to feed all of the cells. A - Living cancer cells B - Dying cancer cells C - Cell debris (necrosis) D - Basement membrane * Referred to as high grade noninvasive cancer- fast growing

Invasive Cancers Most Common: Infiltrating Ductal Carcinoma Infiltrating Lobular Carcinoma
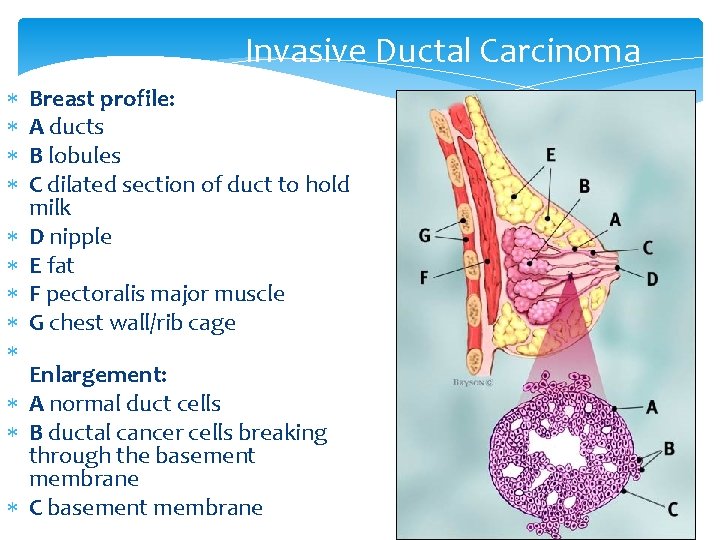
Invasive Ductal Carcinoma Breast profile: A ducts B lobules C dilated section of duct to hold milk D nipple E fat F pectoralis major muscle G chest wall/rib cage Enlargement: A normal duct cells B ductal cancer cells breaking through the basement membrane C basement membrane
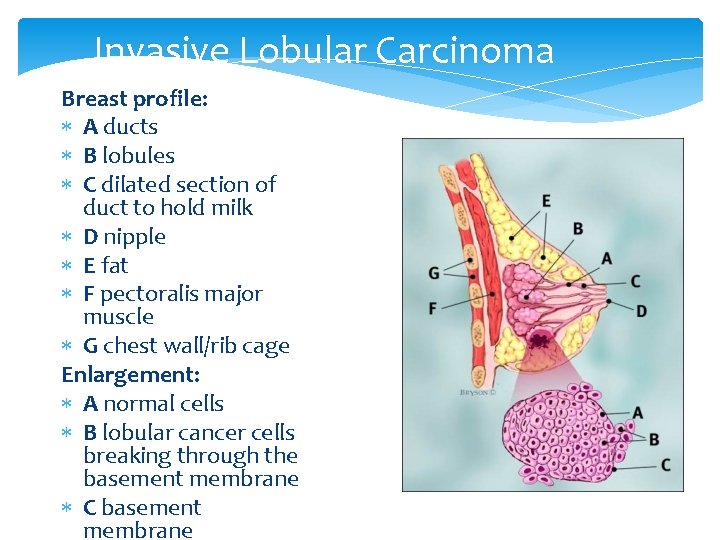
Invasive Lobular Carcinoma Breast profile: A ducts B lobules C dilated section of duct to hold milk D nipple E fat F pectoralis major muscle G chest wall/rib cage Enlargement: A normal cells B lobular cancer cells breaking through the basement membrane C basement membrane
Other Invasive Carcinomas Medullary Carcinoma Mucinous Carcinoma Tubular Ductal Carcinoma Inflammatory Carcinoma Paget’s Disease

Men & Breast Cancer Less than 1% of breast cancers happen to men in Canada; however the number is increasing Men over the age of 60 are most often diagnosed with breast cancer Risk factors, diagnosis, staging and treatment are the same as in women Risk factors include: mumps, radiation exposure & decreased testosterone levels. Most common is ductal carcinoma – found in breast ducts Symptoms include a small painless lump, discharge from nipple, inverted nipple and skin ulceration Adverse feelings related to “manhood” and sexuality, having a “women’s disease”
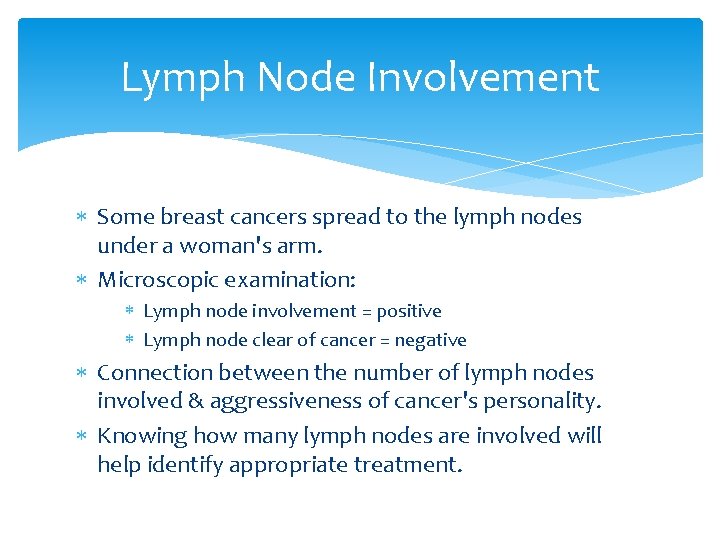
Lymph Node Involvement Some breast cancers spread to the lymph nodes under a woman's arm. Microscopic examination: Lymph node involvement = positive Lymph node clear of cancer = negative Connection between the number of lymph nodes involved & aggressiveness of cancer's personality. Knowing how many lymph nodes are involved will help identify appropriate treatment.
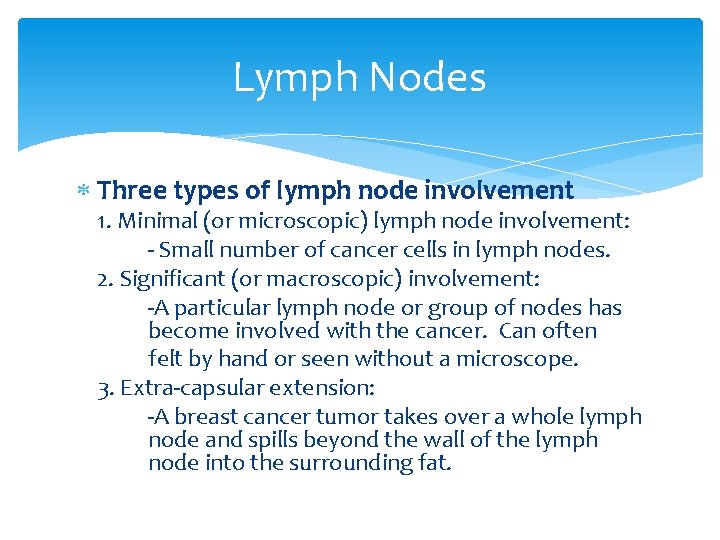
Lymph Nodes Three types of lymph node involvement 1. Minimal (or microscopic) lymph node involvement: - Small number of cancer cells in lymph nodes. 2. Significant (or macroscopic) involvement: -A particular lymph node or group of nodes has become involved with the cancer. Can often felt by hand or seen without a microscope. 3. Extra-capsular extension: -A breast cancer tumor takes over a whole lymph node and spills beyond the wall of the lymph node into the surrounding fat.
Lymph Nodes In most cases, the more extensive the lymph node involvement, the more aggressive the cancer. But the extent of disease within a particular lymph node is less important than the total number of lymph nodes affected. The more lymph nodes that are involved, the more threatening the cancer may be. Doctors use the following categories to describe the overall level of lymph node involvement: No lymph nodes involved 1– 3 nodes involved 4– 9 nodes involved 10 or more nodes involved.

Has Cancer Invaded Lymph or Blood Vessels? A blood vessels B lymphatic channels Enlargement A Normal duct cell B Cancer cells C Basement membrane D Lymphatic channel E Blood vessel F Breast tissue

Breast Cancer Tissue

Report to Physician ASAP
Screening 1. 2. SBE (self-breast examination) Mammography
Self Breast Examination Self Breast Exams are an important way to find a breast cancer early. Not every cancer can be found this way, but it is critical to become familiar with your breasts in order to identify an abnormality SBE should be done once a month approximately 1 wk after your menstrual period
Self Breast Exam cont’d Lumps most women have lumps or lumpy areas in the breast that may be the result of Fibroadenomas or Cysts 8 out of 10 lumps removed from the breast are benign Upper/outer area(armpit) - most prominent lumps/bumps Lower half - sandy/pebbly beach Underneath nipple - collection of large grains Other parts - lumpy bowl of oatmeal
Studies show that regular breast self-exams, combined with an annual exam by a doctor, improves the chances of detecting cancer early.
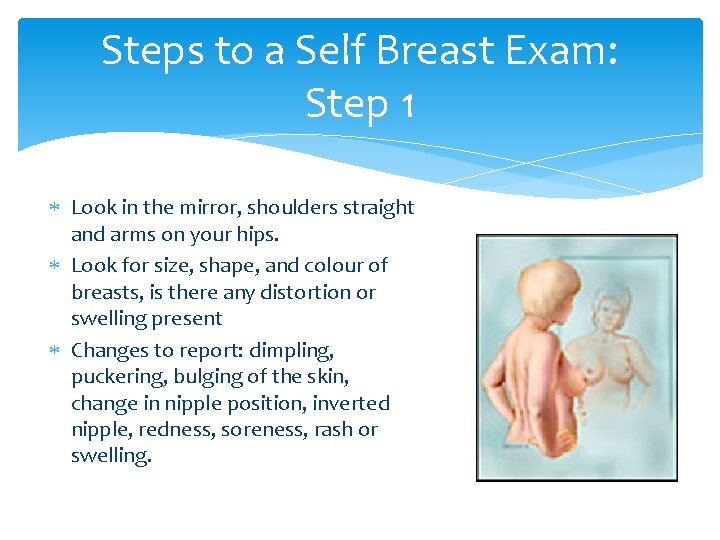
Steps to a Self Breast Exam: Step 1 Look in the mirror, shoulders straight and arms on your hips. Look for size, shape, and colour of breasts, is there any distortion or swelling present Changes to report: dimpling, puckering, bulging of the skin, change in nipple position, inverted nipple, redness, soreness, rash or swelling.
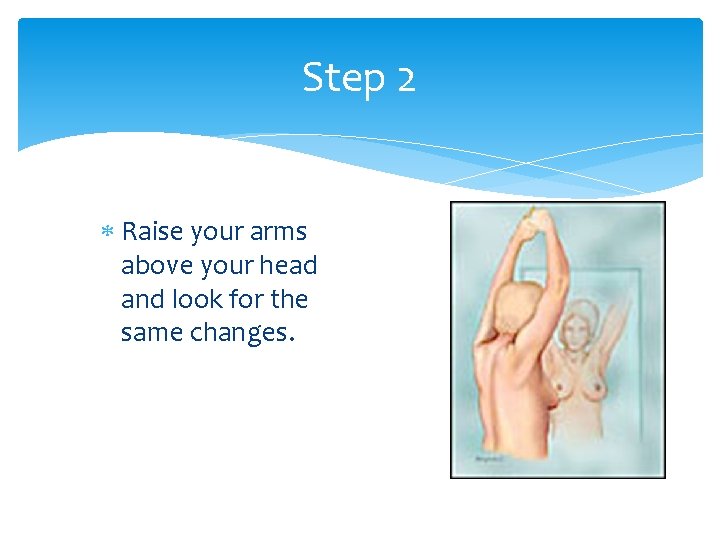
Step 2 Raise your arms above your head and look for the same changes.
Step 3 Still standing at the mirror, look for any discharge/fluid coming from your nipples. Changes to report: any fluid coming out of 1 or both nipples (unless you are lactating). Could be watery, milky, yellow or bloody.
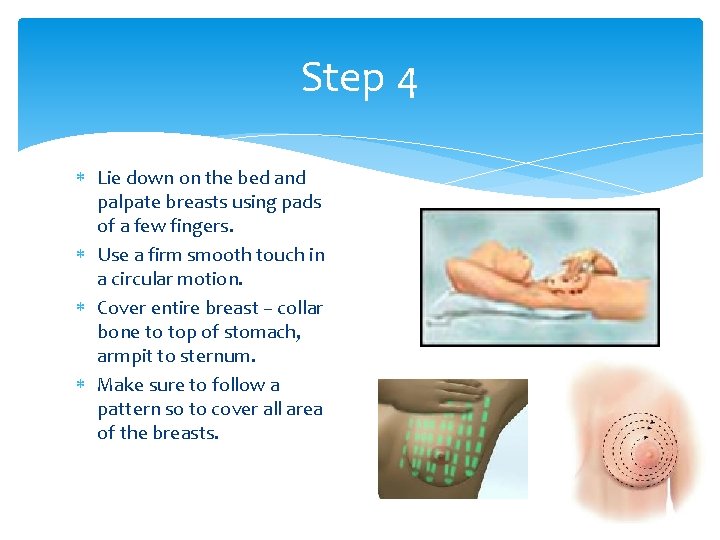
Step 4 Lie down on the bed and palpate breasts using pads of a few fingers. Use a firm smooth touch in a circular motion. Cover entire breast – collar bone to top of stomach, armpit to sternum. Make sure to follow a pattern so to cover all area of the breasts.

Step 5 Sit or stand palpate the breast in the same manner as step 4. Changes to report: lumps, bumps, irregularities

Mammography Breast imaging technique Identifies non-palpable masses and diagnoses palpable masses Procedure takes approximately 15 minutes Breast is compressed from top to bottom, and side to side New and old mammograms are compared Radiation exposure is equivalent to 1 hour in the sun Canadian Cancer Society recommends women to have a mammogram every 2 years between 50 & 69 years of age. Women at high risk and under 50 should speak with the HCP http: //www. youtube. com/watch? v=Y-Gm. Nm. Peq. HQ

EXPERT QUOTE "The biggest misconception about mammography is that it picks up every breast cancer. In fact, mammography misses at least 10 percent of breast cancer. So if you feel a lump that doesn't show up on a mammogram, bring it to your doctor's attention. Get it evaluated. " —Susan Orel, M. D.
Diagnosis for Breast Cancer Procedures for tissue analysis: Percutaneous Biopsy Fine-Needle Aspiration Core Needle Biopsy Guided Core Biopsy Surgical Biopsy Excisional Biopsy Incisional Biopsy

Needle Biopsy
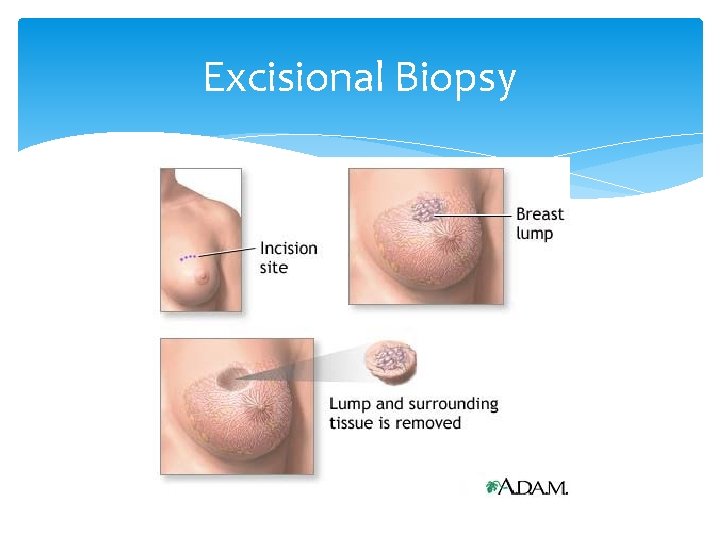
Excisional Biopsy

Grading
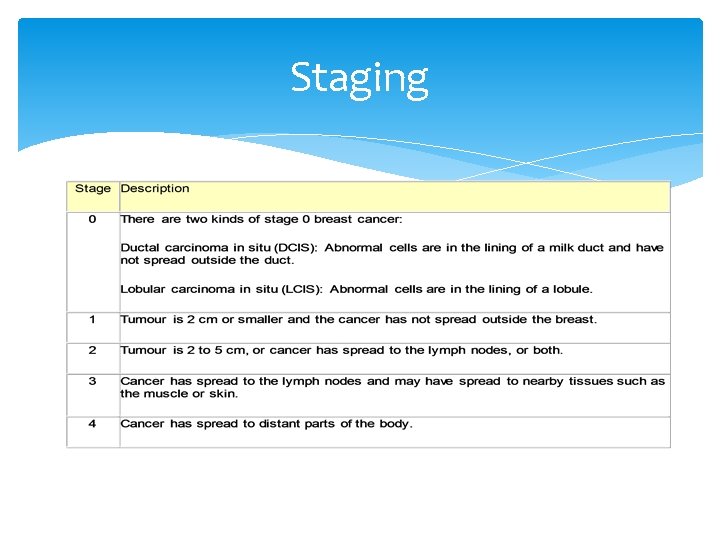
Staging

Treatment Surgery Chemotherapy Radiation Adjunctive Therapy Alternative Therapy
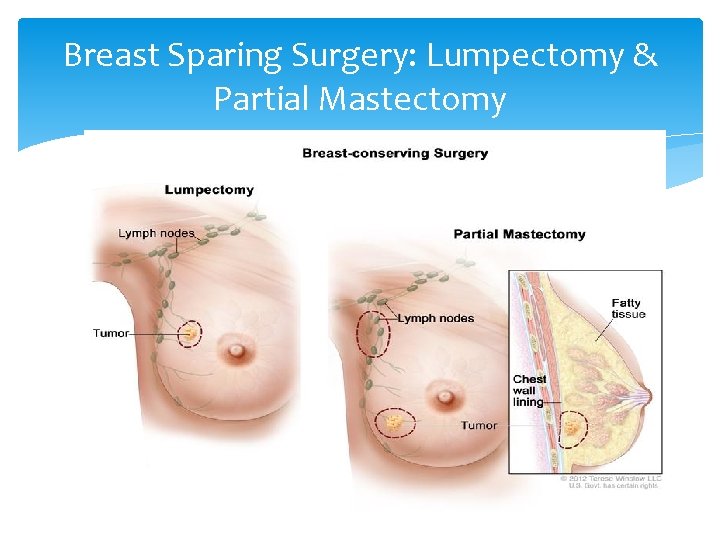
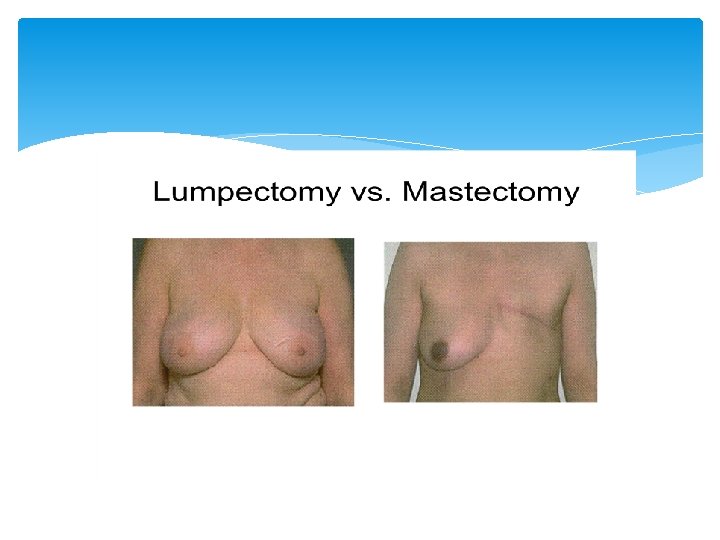
Breast Sparing Surgery: Lumpectomy & Partial Mastectomy
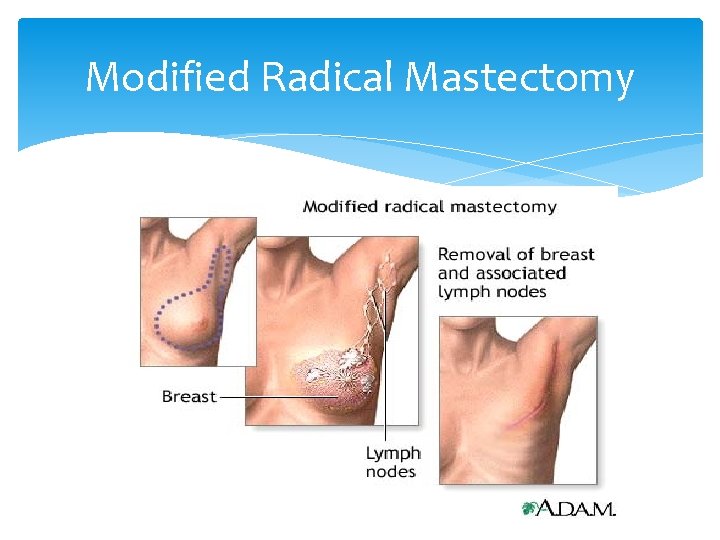
Modified Radical Mastectomy
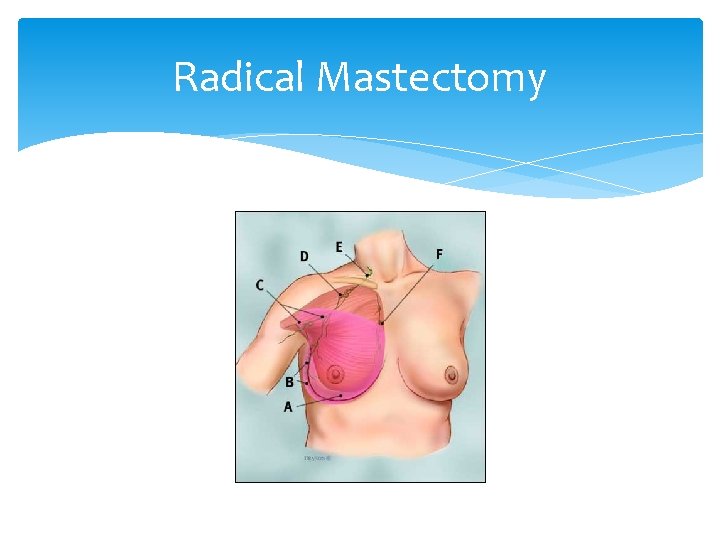
Radical Mastectomy
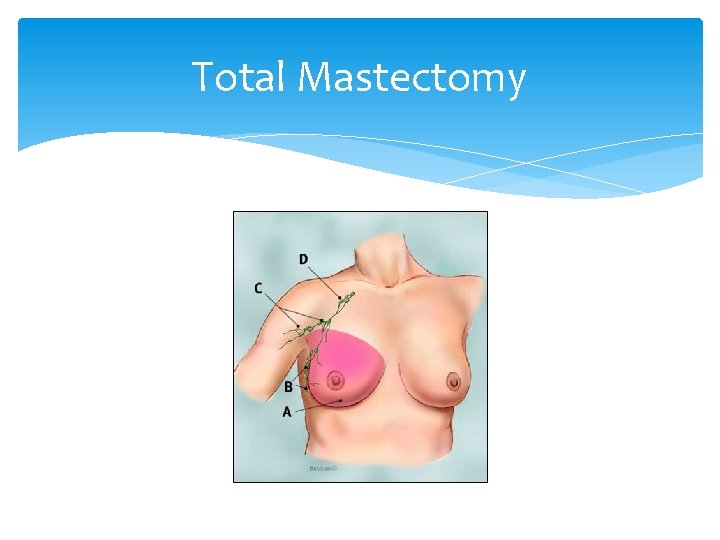
Total Mastectomy

TRAM Flap Reconstruction
Complications Infection Lymphedema Hematoma/Seroma Formation Allergic Reaction
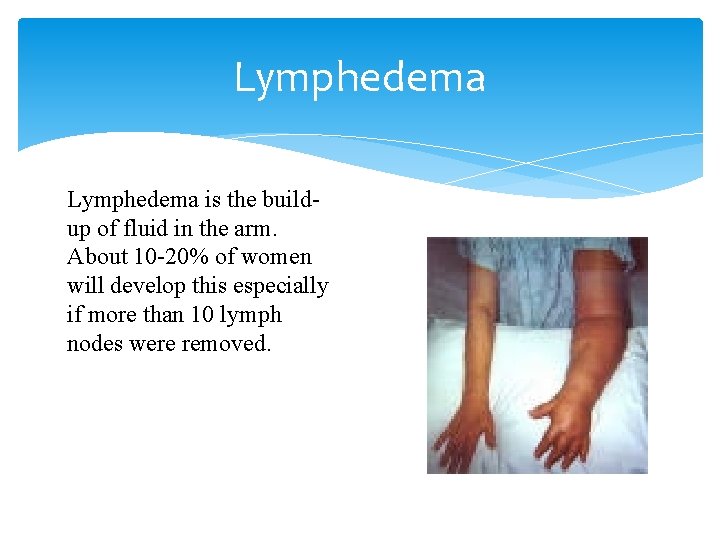
Lymphedema is the buildup of fluid in the arm. About 10 -20% of women will develop this especially if more than 10 lymph nodes were removed.
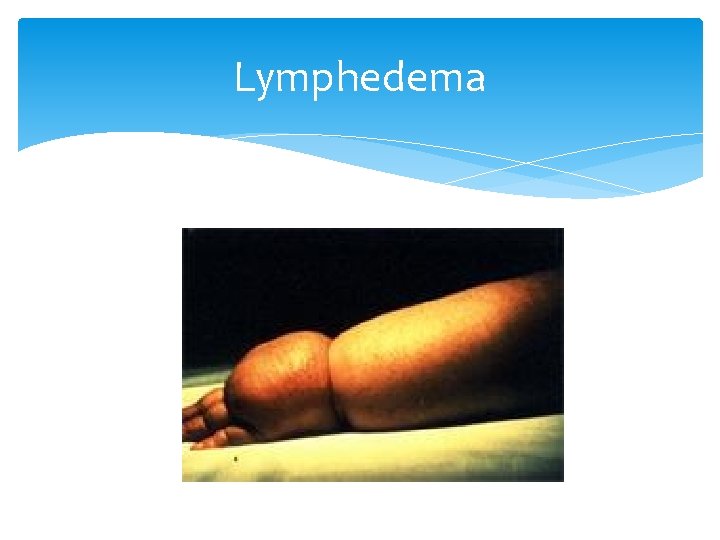
Lymphedema
How to Prevent Lymphedema Talk to HCP if experiencing symptoms of lymphedema Keep skin and nails clean Avoid blocking the flow of fluid through the body Keep blood from pooling in affected limb Exercise
Prognosis Two most important factors when determining the prognosis of breast cancer: Size of tumour Spread of tumour Excessive number of copies of certain genes Excessive amounts of the genes protein products

Preoperative Nursing Diagnosis Deficient knowledge Anxiety Fear Risk for ineffective coping Decisional conflict

Preoperative Nursing Interventions Provide education and preparation for surgical treatments Reduce fear and anxiety and improve coping ability Promote decision-making ability
Postoperative Nursing Diagnoses Acute pain Disturbed sensory perception Disturbed body image Risk for impaired adjustment Risk for ineffective coping for individual and family Deficient knowledge Risk for sexual dysfunction Risk for infection
Postoperative Nursing Interventions Relieving pain and discomfort Managing postoperative sensations Promoting a positive body image Promote positive adjustment and coping Improving sexual function Monitor for complications

Case Study Mrs. X, a 59 year old female with a family history of breast cancer recently found a small palpable mass in the upper outer quadrant of her left breast, she also noticed some slight dimpling upon a breast self exam. When she notified her doctor, he preformed a fine needle aspiration biopsy for tissue analysis. Mrs. X’s results showed she had an infiltrating ductal carcinoma, which is an invasive cancer. Mrs. X’s doctor staged her cancer as T 1 N 1 M 0. 1. 2. 3. How often and when should one perform a breast self exam? If Mrs. X’s breast cancer was genetically inherited, which gene(s)would most likely have a mutation? Interpret T 1 N 1 M 0
Case Study Cont’d Mrs. X was scheduled for a modified radical mastectomy (removal of entire breast tissue, nipple – areola complex and axillary lymph nodes). She met with a plastic surgeon to explore the option of breast reconstructive surgery but has decided to wait until after her surgery to decide. Mrs. X’s mother and sister both have undergone the same surgery and she has a very supportive husband. Mrs. X confides in you, the RN, that she is still anxious regarding her upcoming surgery. 1. 2. What are some preoperative nursing interventions you would do? What are some postoperative nursing interventions you would do?
References Day, R. A. , Paul, P. , Williams, B. , Smeltzer, S. C. , & Bare, B. G. (2010). Textbook of Canadian medical-surgical nursing (2 nd ed). Philadelphia, Pennsylvania: Wolters Kluwer Health/Lippincott Williams & Wilkins. www. breastcancer. org www. cancer. gov
- Slides: 62