Breast Cancer in Pregnancy Tricia Merrigan MD FACS
Breast Cancer in Pregnancy Tricia Merrigan, MD, FACS Avera Medical Group Comprehensive Breast Care September
Outline Introduction Epidemiology and risk factors Diagnostic work up Treatment of breast cancer in pregnancy • Staging • Treatment options • Special considerations in pregnancy • Obstetric follow-up during treatment • •
Introduction • Breast cancer is the most common cancer among women both in the US and in the world • About 1 in 8 women (12%) will be diagnosed with an invasive breast cancer during their lifetime • In 2015, an estimated 231, 840 new cases of invasive breast cancer are expected to be diagnosed in women in the U. S. , along with 60, 290 new cases of non-invasive (in situ) breast cancer
Introduction • About 2, 350 new cases of invasive breast cancer are expected to be diagnosed in men in 2015 • A man’s lifetime risk of breast cancer is about 1 in 1, 000 • In 2015, there are more than 3 million breast cancer survivors in the US
Breast Cancer in Pregnancy • Pregnancy-related breast cancer is defined as breast cancer diagnosed during pregnancy or within 1 year after delivery • Breast cancer occurs about once in every 3, 000 pregnancies • 3. 9 million births in U. S. in 2014 • 1300 cases of breast cancer estimated in pregnancy

Breast Cancer in Pregnancy • Typically presents as a painless lump palpated by the woman • Often diagnosed at a later stage • Women who are pregnant or nursing often have swollen and tender breasts making it more difficult to identify masses • This leads to poorer outcomes than breast cancer in non-pregnant women • Clinical breast exams should be part of prenatal and postnatal care
Risk Factors for Breast Cancer • • General population– Established Risks: • being female and growing older • Family history • Women with a mother or sister with breast cancer are at about a 2 -fold risk • 85% of women diagnosed WILL NOT have a family history • 5 -10% are truly hereditary (i. e. BRCA mutation, PTEN, P 53) • Reproductive factors • Age at menarche, parity, age at first pregnancy, age at menopause, breastfeeding history, exogenous hormones
Risk Factors for Breast Cancer Lifestyle and dietary factors • Obesity, alcohol use, smoking, lack of exercise • Breast factors • Dense breasts • Previous biopsies with moderate to high risk pathology • Enviromental • Prior thoracic radiation • Risk highest if before 20 and lowest if after 40 •
Risk Factors • No specific risk factors for breast cancer in pregnancy are known • BRCA 1 or BRCA 2 mutations may be at increased risk, but they do not have an increased incidence of breast cancer in pregnancy • As women defer childbearing and the incidence of malignancies rises with age, this situation is expected to become more common
Diagnostic Work Up • History and physical • Clinical breast exam • Any suspicious breast lump or inflamed breast needs evaluation • Presumed mastitis that does not resolve with initial treatment should prompt evaluation • Ultrasound preferred first • Bilateral Mammography (shielded)
Diagnostic Work Up • If diagnostics are negative consider referral to specialist • If positive, then continue with biopsy (core biopsy preferred) • **A percutaneous biopsy of any lesion that does not meet all the criteria for a simple cyst is strongly recommended** • Also recommend that you communicated with pathology that the patient is pregnant which can avoid over-interpretation of pathology
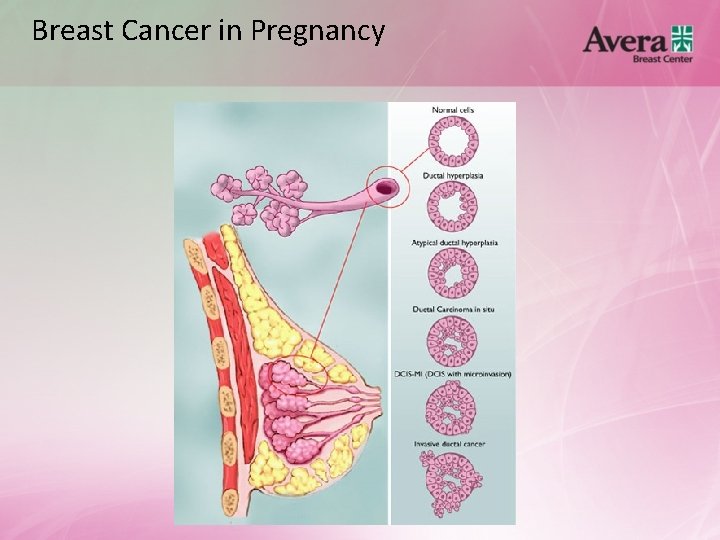
Breast Cancer in Pregnancy
Breast Cancer in Pregnancy • Two main types of breast cancer • Invasive ductal- 80% of breast cancer cases • Invasive lobular- 10% of breast cancer cases • Inflammatory breast cancer is a clinical diagnosis when the breast cancer blocks the lymphatics and causes a red, swollen, “inflamed” breast • Very aggressive and progresses rapidly • Accounts for 1 -6% of all breast cancers in the US
Breast Cancer in Pregnancy • Most pregnant patients are diagnosed with invasive ductal carcinomas which are often associated with aggressive behavior • Grade 3 tumors • Lymphovascular invasion • High rate of estrogen receptor negativity • About 42% HER 2 positive
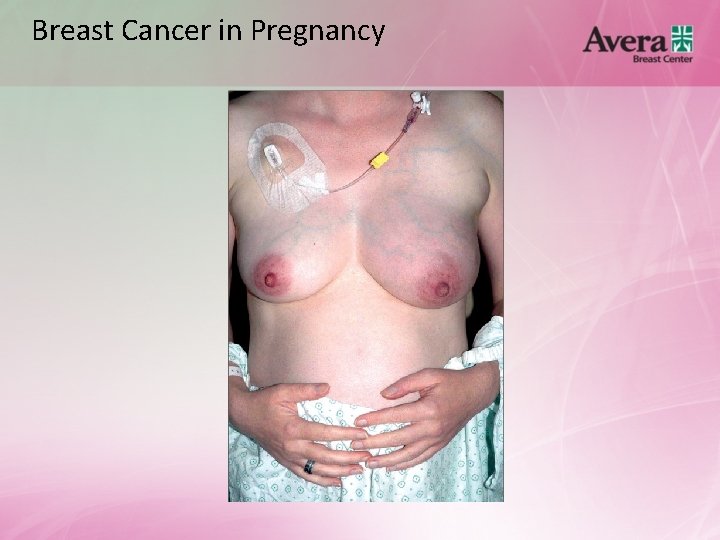
Breast Cancer in Pregnancy
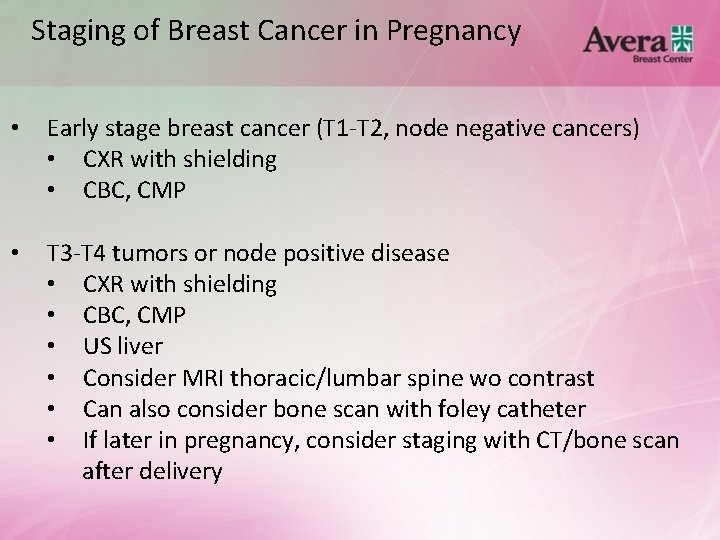
Staging of Breast Cancer in Pregnancy • Early stage breast cancer (T 1 -T 2, node negative cancers) • CXR with shielding • CBC, CMP • T 3 -T 4 tumors or node positive disease • CXR with shielding • CBC, CMP • US liver • Consider MRI thoracic/lumbar spine wo contrast • Can also consider bone scan with foley catheter • If later in pregnancy, consider staging with CT/bone scan after delivery
Treatment of Breast Cancer in Pregnancy • Treatment should involve a multidisciplinary care team including organ system specialists, oncologists, obstetricians, perinatologists, pediatricians, and psychologists • Every patient with cancer during pregnancy should be recorded in a registry to provide information about medical management
Treatment of Breast Cancer in Pregnancy • The goal is to provide accurate information and define when and how far to push back usual treatment limits to satisfy the patient’s wishes while thinking about oncologic risks
Treatment of Breast Cancer in Pregnancy • Breast • Lumpectomy + radiation • Timing depends on biology of tumor, gestational age, need for chemotherapy (either Neo or adjuvant) • Mastectomy w/wo reconstruction w/wo radiation • Sentinel lymph node biopsy is safe in pregnancy • Use sulfur colloid technetium 99 or Lymphoseek • No lymphazurin or methylene blue
Treatment of Breast Cancer in Pregnancy • Body • Chemotherapy- Can be given in 2 nd and 3 rd trimester with approved drugs • Often given in neoadjuvant (before surgery) • Especially in triple negative, Her 2 positive, or locally advanced (lymph node metastasis) • If Er+(node neg), often Oncotype DX or Mammaprint gene assays used to determine chemotherapy benefit • Endocrine therapy- Antiestrogen therapy is delayed until after delivery
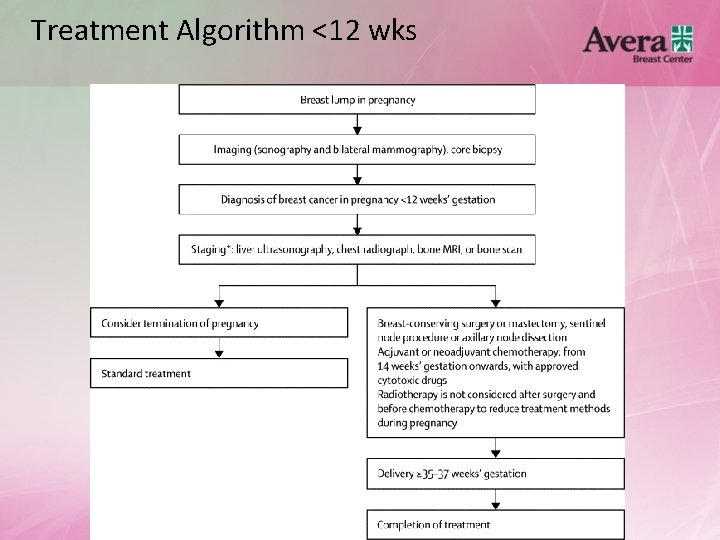
Treatment Algorithm <12 wks
Treatment of Breast Cancer in Pregnancy <12 weeks • Special considerations • Prefer delaying surgery if possible until 2 nd trimester • Chemotherapy is contraindicated in 1 st trimester, but considered relatively safe in 2 nd and 3 rd • Her 2 based therapy contraindicated during pregnancy • Maximum timeframe from surgery to radiation (if chemotherapy not recommended) that is considered safe is about 20 weeks
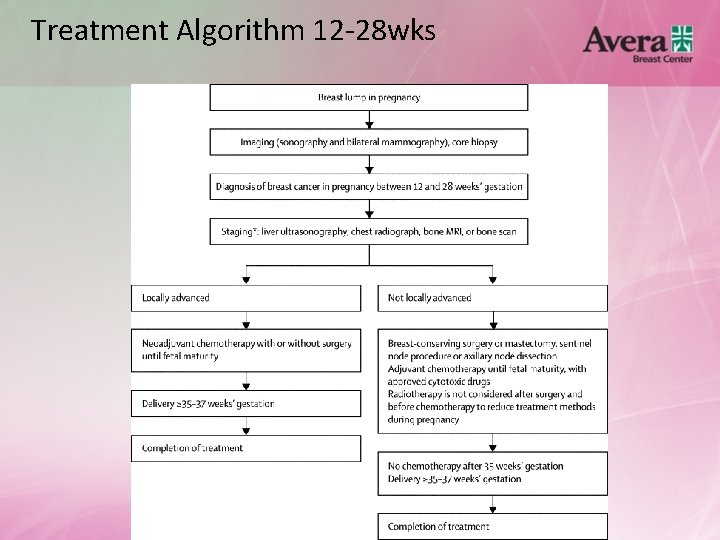
Treatment Algorithm 12 -28 wks
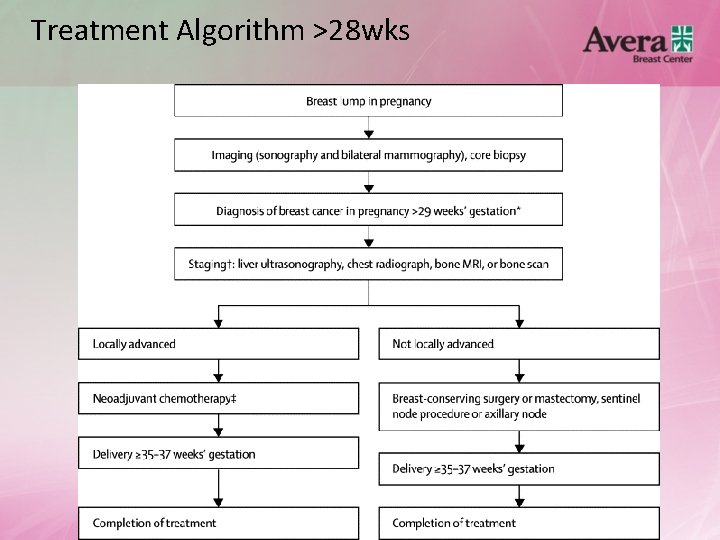
Treatment Algorithm >28 wks

Treatment of Breast Cancer in Pregnancy • Other considerations • Fertility- If undergoing chemotherapy, consider referral to fertility specialist for discussion about risks and options • Pregnancies after breast cancer treatment • New data suggests that it is safe for patients to become pregnant 2 years after completion of treatment for breast cancer
Obstetric Follow-up During Treatment • • • Fetal monitoring before and after surgery Chemotherapy • Check for fetal wellbeing and general development • Check for preterm contractions • Check for intrauterine growth restriction • No chemotherapy after 35 weeks Delivery • Mode of delivery determined by obstetric indications • Preferably after 35 -37 weeks gestation • At least three weeks after last cycle of chemotherapy • If preterm delivery is inevitable, fetal lung maturity if essential
Obstetric Follow-up During Treatment • • Post-partum • Examine placenta for metastatic disease • Oncological treatment can be continued immediately after vaginal delivery and a week after uncomplicated C-section Breastfeeding • Contraindicated during and after chemotherapy
Conclusions • • Breast cancer occurs in about 1 out of every 3000 pregnancies. Often diagnosed at a later stage with aggressive disease. Breast cancer treatment during pregnancy is possible and termination of pregnancy is not likely to improve prognosis. Multidisciplinary team is a must. Timing of pregnancy determines different treatment options. Chemotherapy can be administered in 2 nd and 3 rd trimesters. Registries are necessary to accrue numbers that allow more robust conclusions.
Sources NCCN Guidelines Version 2. 2015 - Breast Cancer- www. nccn. org http: //www. cancer. org/cancer/breastcancer/moreinformation/pregnancy-and-breastcancer http: //www. cancer. gov/cancertopics/pdq/treatment/breast-cancer-andpregnancy/Health. Professional Amant et al. Breast Cancer in Pregnancy. Lancet. 2012; 379(9815): 570 -579. Morice, P, Uzan C, et al. Lancet. 2012; 379(9815): 495 -496. Kuerer, H. M. (2010). Kuerer’s Breast Surgical Oncology. China: The Mcgraw-Hill Companies, Inc. Philippe Morice, Catherine Uzan, Serge Uzan
THANK YOU!! • Questions?
- Slides: 30