BRAIN INJURY 101 Acquired Brain Injury Stroke or
BRAIN INJURY 101
Acquired Brain Injury Stroke or Cerebral Vascular Accident (CVA): a disruption of blood flow (thrombi emboli) in the brain; aneurysms; arteriovenous malformations; and intracerebral hemorrhage. Anoxic Injury: damage to the brain due to lack of oxygen or reduced flow of oxygen. Other Encephalopathies: damage to the brain caused by infections (e. g. , meningitis, encephalitis), tumors, and metabolic disorders.
Traumatic Brain Injury Incidence Every 21 seconds, one person in the US sustains a TBI 1. 5 million Americans will sustain an TBI this year 80, 000 -90, 000 people annually experience the onset of long-term disabilities following TBI An estimated 5. 3 million Americans-a little more than 2% of the US population-currently live with disabilities resulting from TBI
Traumatic Brain Injury Incidence Each year 500, 000 Americans are hospitalized and over 200, 000 will demonstrate persistent cognitive, physical and/or emotional deficits that will prevent functioning at pre-injury levels Males aged 15 -24 and persons older than 75 years of age have the highest incidence of TBI
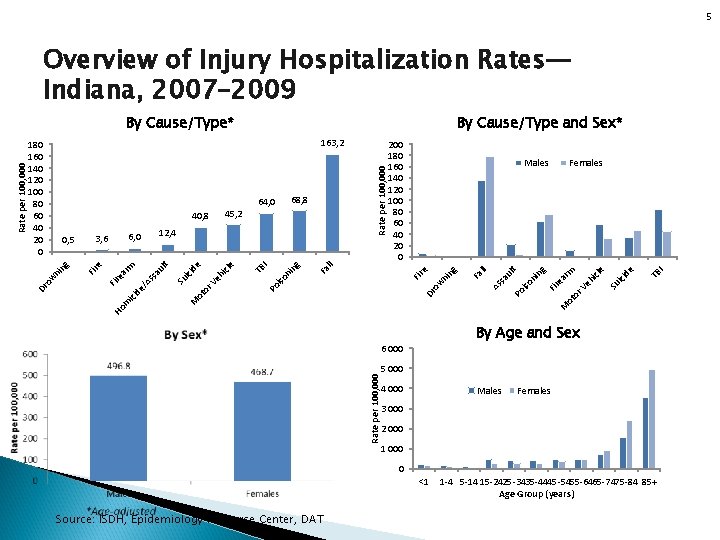
5 Overview of Injury Hospitalization Rates— Indiana, 2007– 2009 By Cause/Type and Sex* TB I e cid Su i ot or Fir Ve hi rm cle Females ea ni ng t iso ul Po sa As Fa ll ng ow ni Fir e Fa ll ng ni iso Po hi Ve ot or TB I cle e cid Su i M ss ici de /A Fir m M lt au rm ea e Fir 12, 4 6, 0 3, 6 Males Ho By Age and Sex 6 000 Rate per 100, 000 ow ni ng 0, 5 68, 8 64, 0 200 180 160 140 120 100 80 60 40 20 0 Dr 45, 2 40, 8 Rate per 100, 000 163, 2 180 160 140 120 100 80 60 40 20 0 Dr Rate per 100, 000 By Cause/Type* 5 000 4 000 Males Females 3 000 2 000 1 000 0 <1 Source: ISDH, Epidemiology Resource Center, DAT 1 -4 5 -14 15 -2425 -3435 -4445 -5455 -6465 -7475 -84 85+ Age Group (years)
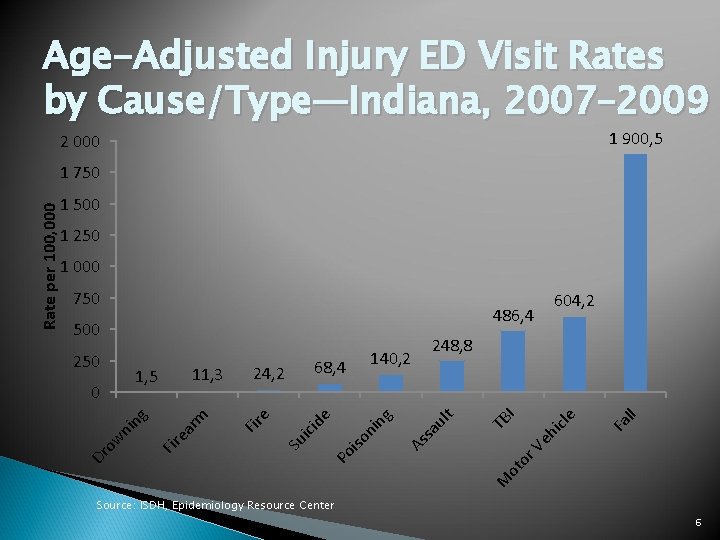
Age-Adjusted Injury ED Visit Rates by Cause/Type—Indiana, 2007– 2009 1 900, 5 2 000 1 500 1 250 1 000 750 486, 4 icl Ve h ll or Fa e I t M ot Po As sa ul ng iso ni de ici Su ea rm Fir ow ni ng 0 e 11, 3 1, 5 140, 2 68, 4 24, 2 Fir 250 604, 2 248, 8 TB 500 Dr Rate per 100, 000 1 750 Source: ISDH, Epidemiology Resource Center 6
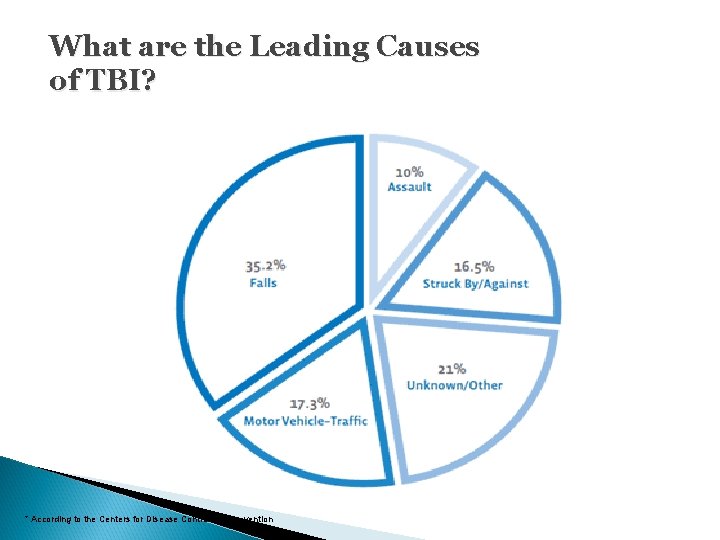
What are the Leading Causes of TBI? * According to the Centers for Disease Control and Prevention

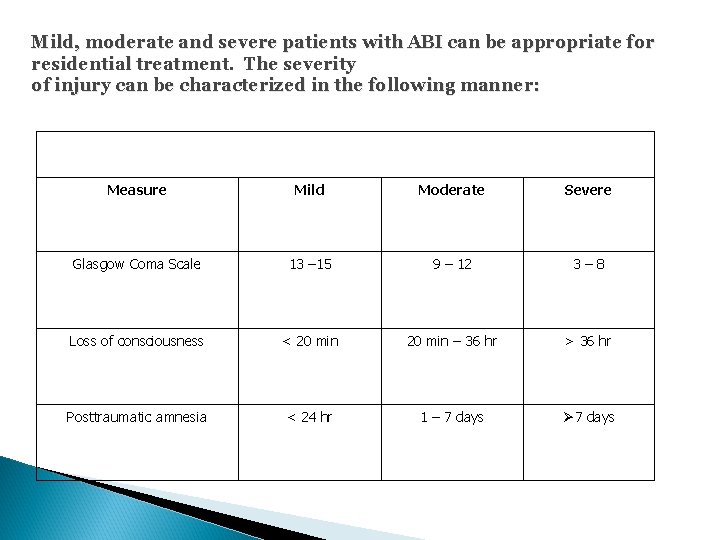
Mild, moderate and severe patients with ABI can be appropriate for residential treatment. The severity of injury can be characterized in the following manner: Measure Mild Moderate Severe Glasgow Coma Scale 13 – 15 9 – 12 3– 8 Loss of consciousness < 20 min – 36 hr > 36 hr Posttraumatic amnesia < 24 hr 1 – 7 days Ø 7 days
Mild Brain Injury An estimated 15% of persons who sustain a mild brain injury continue to experience negative consequences one year after injury Repeated mild brain injuries occurring over an extended period of time (i. e. , months, years) can result in cumulative neurological and cognitive deficits Repeated mild brain injuries occurring within a short period of time (i. e. , hours, day, or weeks) can be catastrophic or fatal
Concussion
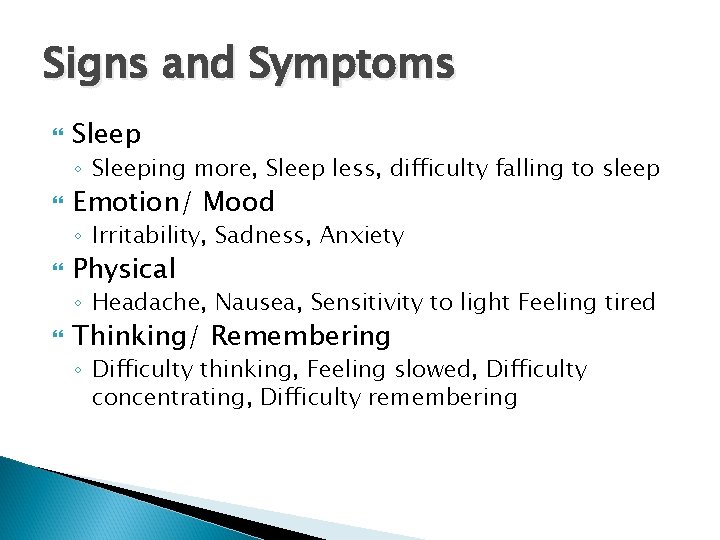
Signs and Symptoms Sleep ◦ Sleeping more, Sleep less, difficulty falling to sleep Emotion/ Mood ◦ Irritability, Sadness, Anxiety Physical ◦ Headache, Nausea, Sensitivity to light Feeling tired Thinking/ Remembering ◦ Difficulty thinking, Feeling slowed, Difficulty concentrating, Difficulty remembering


Domains of Functioning Mobility Cognition Communication Health Self-help skills Household management Community skills Leisure skills Vocational
Cognitive, Memory and Executive Functioning Consequences Short-term memory loss Long-term memory loss Slowed ability to process information Trouble concentrating or paying attention for periods of time Difficulty keeping up with a conversation; other communication difficulties such as word finding problems
Cognitive, Memory and Executive Functioning Consequences, Cont’d Spatial disorientation Organizational problems and impaired judgment Unable to do more than one thing at time (multitask) A lack of initiating activities, or once started, difficulty in competing tasks without reminders Safety-awareness deficits
Speech and Language Consequences Receptive - ability to understand others Expressive - ability to express one’s self to others
Physical Consequences Muscle spasticity or flacidity Mobility Contractures Coordination/Dexterity Fatigue/endurance Balance problems
Behavioral and Psychosocial Consequences Aggressive behavior/verbal outrages Increased Anxiety Depression and mood swings Impulsive behavior More easily agitated Egocentric behaviors; difficulty seeing how behaviors can affect others Withdrawal/lack of engagement Depression
Sensorimotor Consequences Motor functioning Vision & Hearing Taste & Smell Swallowing Endurance
Medical Consequences Urinary Disorders Seizures Disorders Sleep Disorders Headaches or migraines Pain Arthritis Aspiration pneumonia
Traumatic Brain Injury Rehabilitation “The development of the person to the fullest physical, psychological, social, vocational, avocational and educational potential consistent with his or her physiological or anatomical impairments and environmental limitations. ” Whyte & Rosenthal (1988)
Traumatic Brain Injury Outcome Factors The development of a means for measuring and predicting functional outcome post-brain injury is of critical importance if realistic goals are to be formulated to assist the person to resume independence to the maximum level possible. Outcome is defined as: “The adequacy with which a patient’s lifestyle is resumed including the efficiency with which he performs the activities of daily life” (Levin, Benton, & Grossman, 1982).
Predicting Outcome After BI Pre-injury Factors: Pre-injury History General Health Prior history of brain injury Age at Time of Onset Psychosocial Issues Educational Level Employment History
Predicting Outcome After BI Injury Factors: Severity of Injury Etiology and Location Type of Injury Anoxic, Traumatic, Etc. Coma Depth and Duration Post-traumatic Amnesia Complicating Medical Factors Access to Acute Care
Predicting Outcome After BI Post-injury Factors: Time Elapsed Since Injury Socio-economic Status Nature and Extent of Financial Resources Motivation Level of Self Awareness, Self Control and Coping Skills Religious and Spiritual Beliefs Psychosocial Issues Access to a Continuum of Care
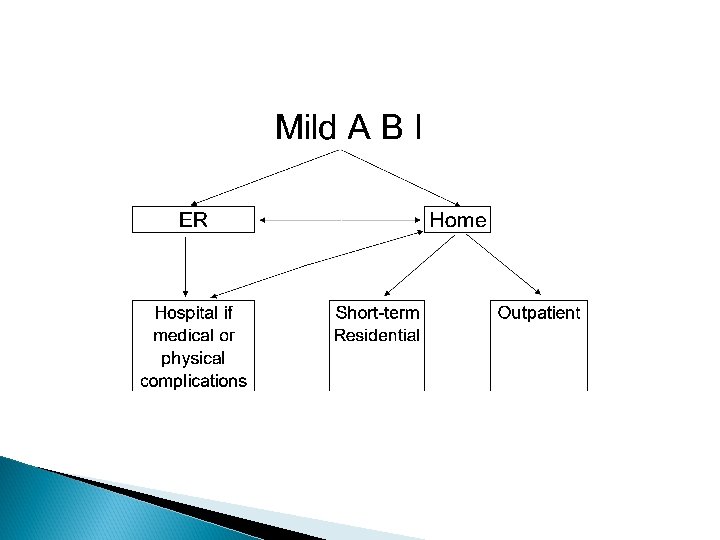
Traumatic Brain Injury Continuum of Care Examples of Services Available in the Continuum of Care Hospital-Based Services Trauma System/ER Acute Rehabilitation After-Hospital Services Skilled Nursing Facility (Sub-Acute) Post-Acute Treatment Transitional Treatment (Short Term) Long-Term Rehabilitation (6 -12 months) Outpatient Treatment Supported Living Programs
Functional Rehabilitation Occurs in naturalistic settings. Integrated into common daily routines. Offers a structure within which learning can occur and through which autonomy and self-reliance is fostered. Designed and carried out by trained staff Intended to empower the individual.
Effective Rehabilitation 1. Identify important skills individual can do independently, with assistance, and those that cannot be done. 2. Based on abilities and disabilities identified, assist individual to develop realistic long-term plan (include specification of discharge environment). 3. Determine abilities or outcomes individual will need to achieve the plan. 4. Identify long-term goals that must be met to acquire the necessary abilities. 5. Break long-range goals into specific short term objectives. 6. Design a plan for assisting individual to meet objectives. 7. Evaluate progress on basis of measurable outcome criteria. 8. Based on regular reviews, revise Steps 1 -7 as necessary.
General Guidelines Person-centered: individual should be included in identification and design of the treatment plan. Supportive: plan’s design should make it very likely that the individual will succeed (especially in the early stages). Simplicity: plan should be easy for staff and individual to understand. Consistency: plan must be implemented as consistently as possible. Flexibility: plan must be flexible enough to adapt to changes in the individual. Positive: staff should discuss the person’s successes.
Identification of Family Strengths 1. 2. 3. 4. 5. 6. Ability of the family to listen. Shared and common perceptions of reality within the family. Spirituality of the family. Ability of the family to realize the redemptive power of a seemingly tragic event. Ability of family members to take responsibility for disability-related problems. Ability of family members to use negotiation in family problem solving.
Identification of Family Strengths 7. Family members’ willingness to take good care of themselves. 8. Family’s ability to focus on present, rather than on past events. 9. Ability of family members to provide reinforcements for each other. 10. Ability of family members to discuss concerns. 11. Ability of family members to provide an atmosphere of belonging. 12. Family’s effective trans generational coping strategies
Resources Brain Injury Association of Indiana ◦ BIAI. ORG Defense and Veterans Center for Brain Injury DVBIC. GOV Contact your local VA VA. GOV
Robbie Schmidt, LCSW Program Director 317 -771 -1875
- Slides: 36