Brain edema Definition increased intracranial water content Associated
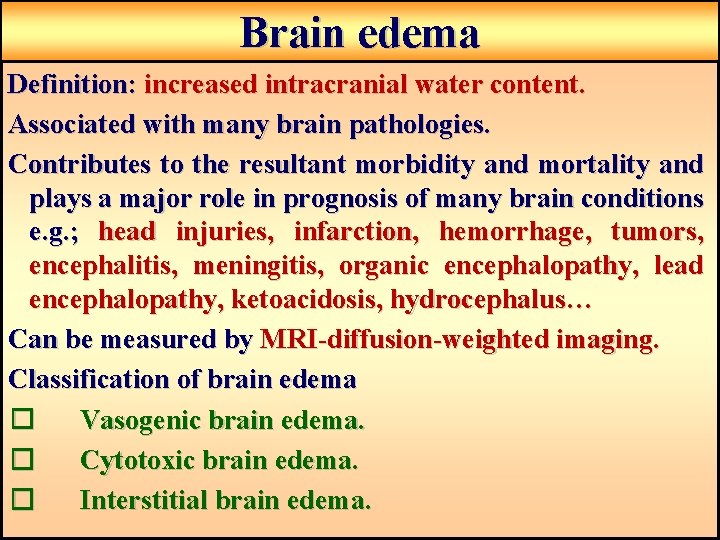
Brain edema Definition: increased intracranial water content. Associated with many brain pathologies. Contributes to the resultant morbidity and mortality and plays a major role in prognosis of many brain conditions e. g. ; head injuries, infarction, hemorrhage, tumors, encephalitis, meningitis, organic encephalopathy, lead encephalopathy, ketoacidosis, hydrocephalus… Can be measured by MRI-diffusion-weighted imaging. Classification of brain edema � Vasogenic brain edema. � Cytotoxic brain edema. � Interstitial brain edema.
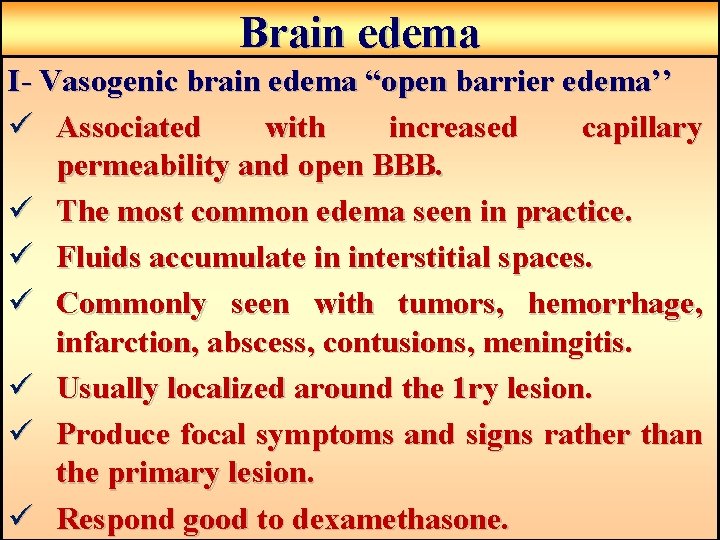
Brain edema I- Vasogenic brain edema “open barrier edema’’ ü Associated with increased capillary permeability and open BBB. ü The most common edema seen in practice. ü Fluids accumulate in interstitial spaces. ü Commonly seen with tumors, hemorrhage, infarction, abscess, contusions, meningitis. ü Usually localized around the 1 ry lesion. ü Produce focal symptoms and signs rather than the primary lesion. ü Respond good to dexamethasone.
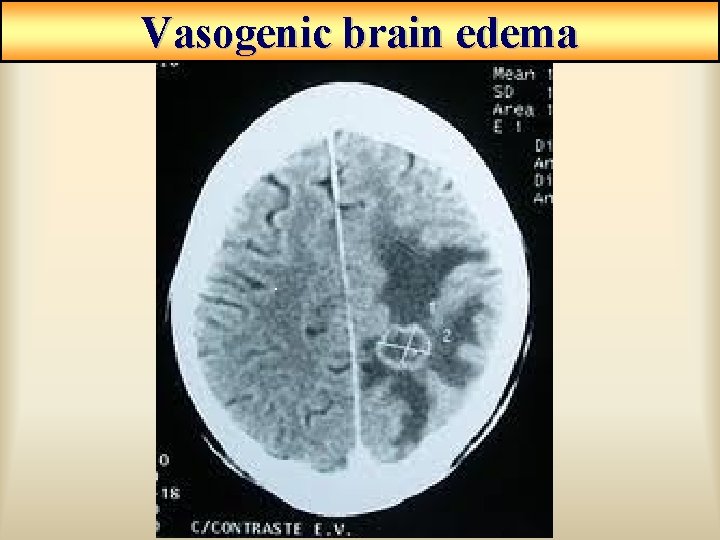
Vasogenic brain edema
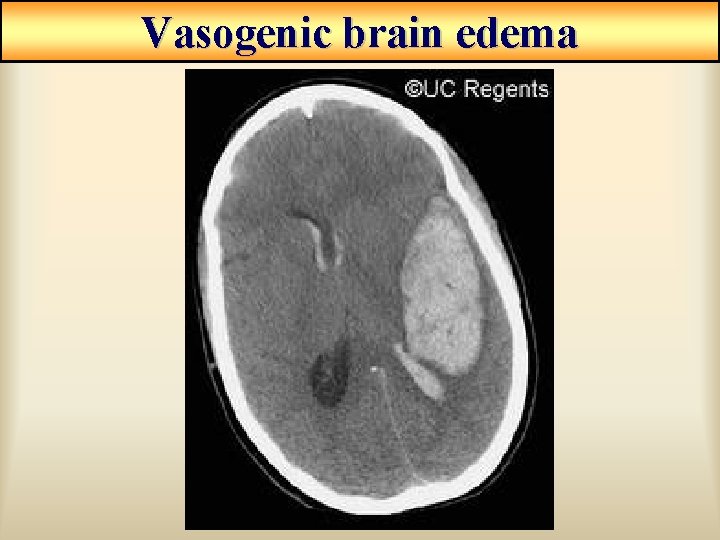
Vasogenic brain edema
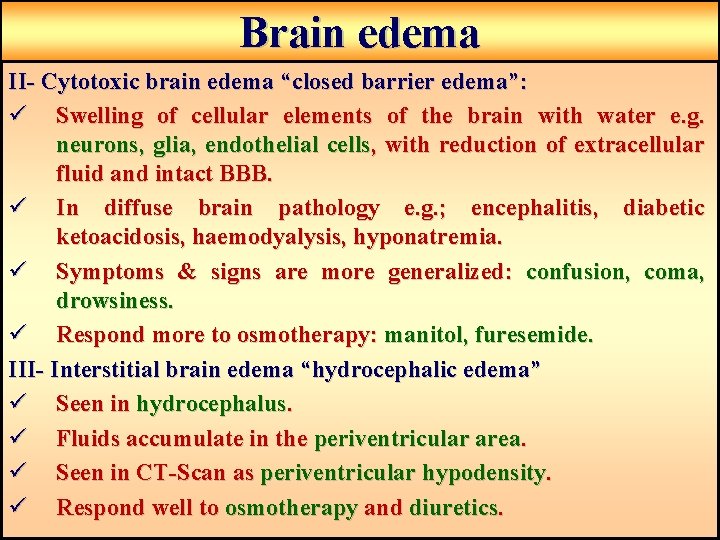
Brain edema II- Cytotoxic brain edema “closed barrier edema”: ü Swelling of cellular elements of the brain with water e. g. neurons, glia, endothelial cells, with reduction of extracellular fluid and intact BBB. ü In diffuse brain pathology e. g. ; encephalitis, diabetic ketoacidosis, haemodyalysis, hyponatremia. ü Symptoms & signs are more generalized: confusion, coma, drowsiness. ü Respond more to osmotherapy: manitol, furesemide. III- Interstitial brain edema “hydrocephalic edema” ü Seen in hydrocephalus. ü Fluids accumulate in the periventricular area. ü Seen in CT-Scan as periventricular hypodensity. ü Respond well to osmotherapy and diuretics.
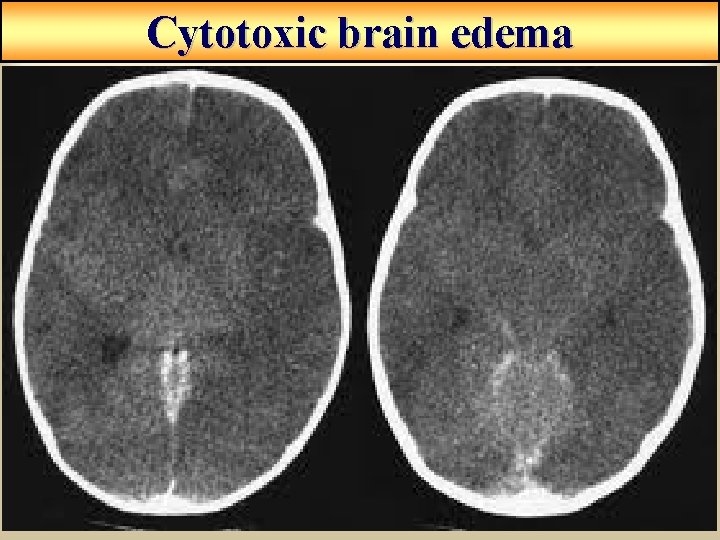
Cytotoxic brain edema
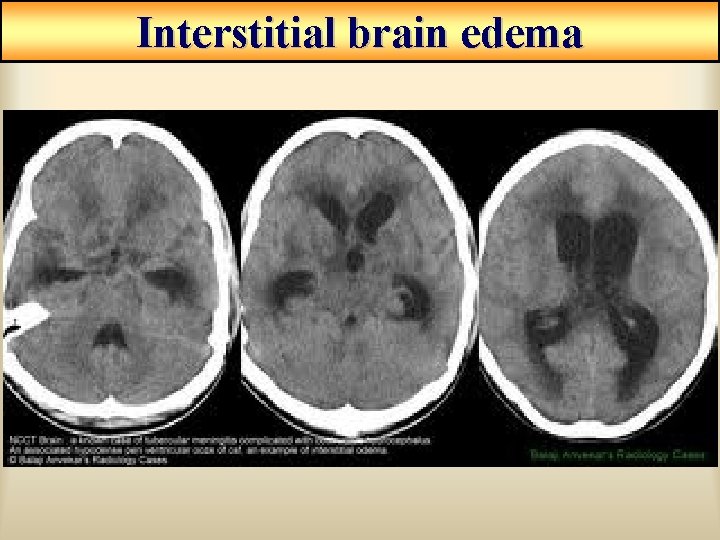
Interstitial brain edema
CNS Infections Include: • Meningitis. • Encephalitis. • Local suppurations. Usually one syndrome predominant, but two of them may coexist in the same patient. Common shared clinical features: • Pyrexia. • Headache. • Disturbed conscious level. • Focal neurological deficits. • Features of increased intracranial tension.
Meningitis Definition: inflammation of the meningeal coverings of the brain and/or spinal cord. May be: -Acute – Subacute - Chronic Causes: Inflammatory Infective: Bacterial “septic meningitis” >>> polymorphnuclear cells in CSF. Viral “aseptic meningitis” >>> lymphocytes cells in CSF Fungal, parasitic, TB, … Inflammatory Non infective: toxic, demyelinating. Route of infection: Blood stream >>> blood born organisms cross BBB. Direct spread of infection From local para-meningeal suppurations. Direct introduction; neurosurgery or trauma.
Clinical Feature of meningitis Age incidence: Children►young adult► elderly and immune suppressed. 1) General features: Fever, malaise, vomiting, headache, photophobia, neck stiffness, … Absence of fever, neck stiffness (children, elderly, immunosuppresed and severe infection). Headache is more common with viral meningitis. Disturbances in consciousness is more common with bacterial meningitis. TB, fungal and parasitic >>>> chronic presentation. Viral and bacterial >>>> acute presentation.
Clinical Feature of meningitis 2) • • • Seizure: Occurs in up to 40% of children, also in old pts. Early evoked by fever and infection. If prolonged, CSF must be examined for encephalitis. 3) Systemic infection, search for: • Chest infection. • Septic arthritis. • Endocarditis. • Skin rashes.
Clinical Feature of meningitis 4) Focal signs: (in >15% of bacterial meningitis) Arteritis of intracranial arteries >>> infarction. Cerebral venous thrombosis >>> focal signs, seizures. Inflammation of basal meninges >>> cranial nerve palsies. Abscess formation. 5) Electrolyte disturbances: More in children. The syndrome of inappropriate secretion of ADH >>> hyponateraemia.
Viral Meningitis o o o Forms > 70% of acute aseptic meningitis More in children and young adults More in summer & autumn Usually benign and self limiting Commonest causative viurses; Enterovirus (echo. . , polio. . ), Arbovirus, H. simplex, Varicella zoster, Mumps and HIV Clinical Features: � Is Common to all viruses � Common to find signs of specific infections eg; mumps, parotitis… � Sudden onset of fever, headache, neck stiffness � URTI, nausea, irritability, myalgia, drowsiness � Appearance of focal neurological deficit→ suggest Encephalitis. � Prognosis & outcome : – May recover spontaneously in few days, rarely weeks – Recovery is complete in most cases NB * Headache is common *Consciousness is not impaired
Bacterial Meningitis Common in children < 5 ys. Boys > girls Transmission: Personal contact Inhalation of airborne infected droplets Common organisms in children: E. coli Streptococci H. Influenza Common organisms in adults: Meningococci (commonest) Pneumococci Common organisms in elderly: G –ve bacilli Clinical picture: Common in closed communities (schools, military camps, …) Incubation Period < 10 days Suggestive features of meningococcal meningitis: – Typical rash appears on the trunk, legs, palms, soles, and mucous membrane ranging from purpura to bullous lesions. – DIC (in severe cases). – Adrenal Hemorrhage may result & cause cardiovascular collapse. – Myocarditis, pericarditis and arthritis.
TB Meningitis The incidence is decreasing. In the developing countries, the incidence is still high. Usually occurs secondary to TB infections else where, commonly pulmonary TB. Infection is more severe in & around: 1 - Basal meninges 3 - Meningeal arteries 2 - Foraminae of the 4 th ventricle 4 - Cerebral arteries >>> complications of TB meningitis as hydrocephalus, ↑ICT, CN palsies, focal deficit. Clinical Features : � Appears slowly over 3 -4 weeks in adults and shorter in children � Symptoms and signs are nonspecific: 1 - Nausea and vomiting 2 - Malaise and apathy 3 - Anorexia, irritability, depression, confusion, disturbed behavior � Headache & fever…. . not common � Signs of meningeal irritation, epileptic seziure, focal neurological deficits, Cranial nerve palsies, hydrocephalus, cerebeller tuberculoma, spinal TB.
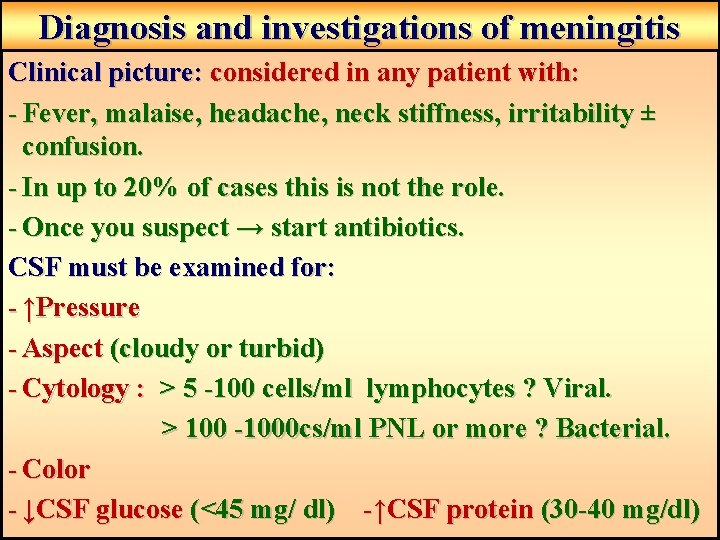
Diagnosis and investigations of meningitis Clinical picture: considered in any patient with: - Fever, malaise, headache, neck stiffness, irritability ± confusion. - In up to 20% of cases this is not the role. - Once you suspect → start antibiotics. CSF must be examined for: - ↑Pressure - Aspect (cloudy or turbid) - Cytology : > 5 -100 cells/ml lymphocytes ? Viral. > 100 -1000 cs/ml PNL or more ? Bacterial. - Color - ↓CSF glucose (<45 mg/ dl) -↑CSF protein (30 -40 mg/dl)
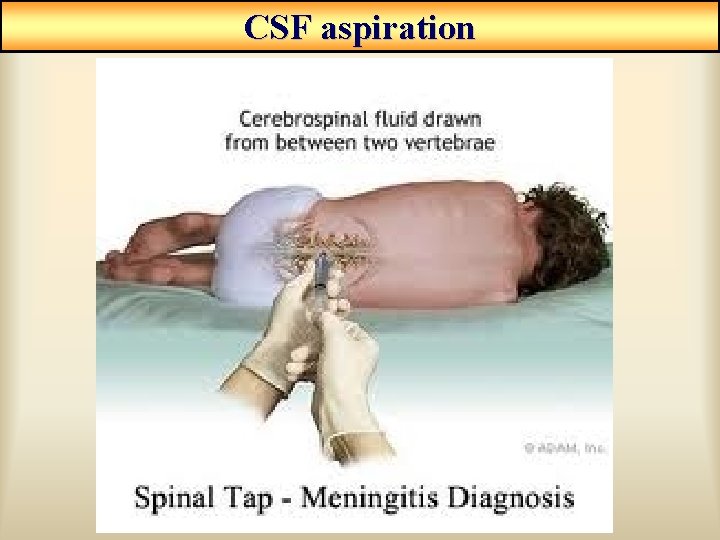
CSF aspiration
Diagnosis and investigations of meningitis Blood culture and blood tests: - In > 50% of cases, organism can be detected. - Increased ESR, blood electrolytes, CBC. Brain imaging MRI is better than CT. Differential Diagnosis: 1 - Infective causes: Encephalitis, Brain abscess, Septicemia & Subdural empyema 2 - Non-infective causes: SAH, Drugs, Chemical irritation, Brain tumor, Collagen diseases eg; SLE
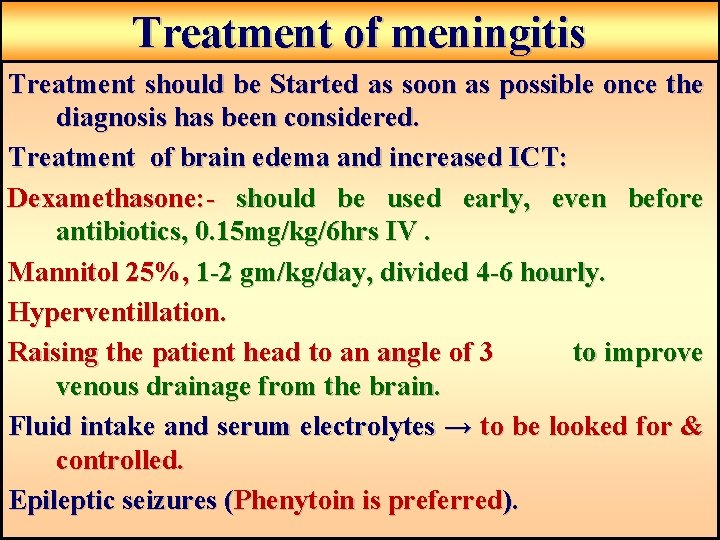
Treatment of meningitis Treatment should be Started as soon as possible once the diagnosis has been considered. Treatment of brain edema and increased ICT: Dexamethasone: - should be used early, even before antibiotics, 0. 15 mg/kg/6 hrs IV. Mannitol 25%, 1 -2 gm/kg/day, divided 4 -6 hourly. Hyperventillation. Raising the patient head to an angle of 3 to improve venous drainage from the brain. Fluid intake and serum electrolytes → to be looked for & controlled. Epileptic seizures (Phenytoin is preferred).
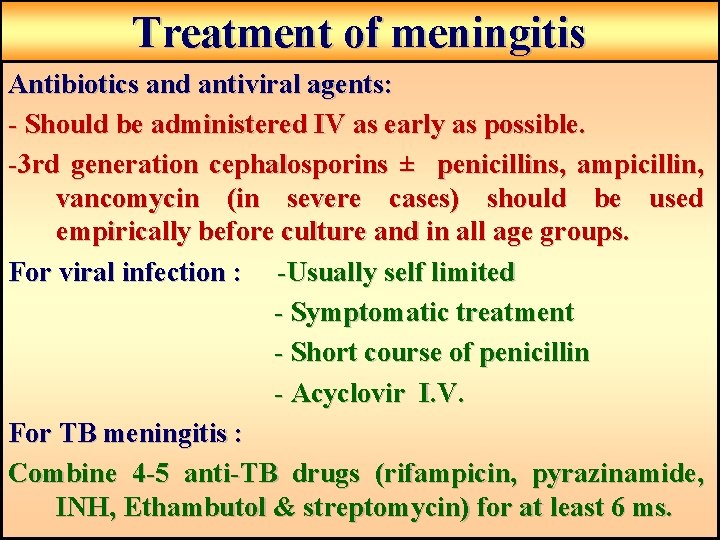
Treatment of meningitis Antibiotics and antiviral agents: - Should be administered IV as early as possible. -3 rd generation cephalosporins ± penicillins, ampicillin, vancomycin (in severe cases) should be used empirically before culture and in all age groups. For viral infection : -Usually self limited - Symptomatic treatment - Short course of penicillin - Acyclovir I. V. For TB meningitis : Combine 4 -5 anti-TB drugs (rifampicin, pyrazinamide, INH, Ethambutol & streptomycin) for at least 6 ms.
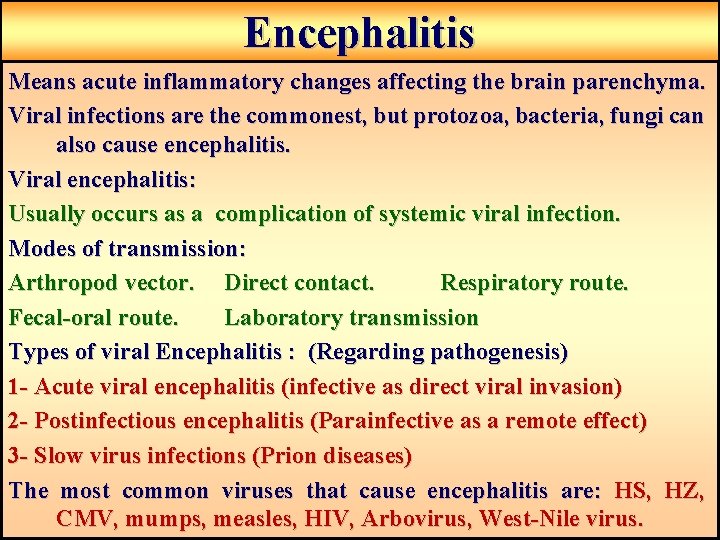
Encephalitis Means acute inflammatory changes affecting the brain parenchyma. Viral infections are the commonest, but protozoa, bacteria, fungi can also cause encephalitis. Viral encephalitis: Usually occurs as a complication of systemic viral infection. Modes of transmission: Arthropod vector. Direct contact. Respiratory route. Fecal-oral route. Laboratory transmission Types of viral Encephalitis : (Regarding pathogenesis) 1 - Acute viral encephalitis (infective as direct viral invasion) 2 - Postinfectious encephalitis (Parainfective as a remote effect) 3 - Slow virus infections (Prion diseases) The most common viruses that cause encephalitis are: HS, HZ, CMV, mumps, measles, HIV, Arbovirus, West-Nile virus.
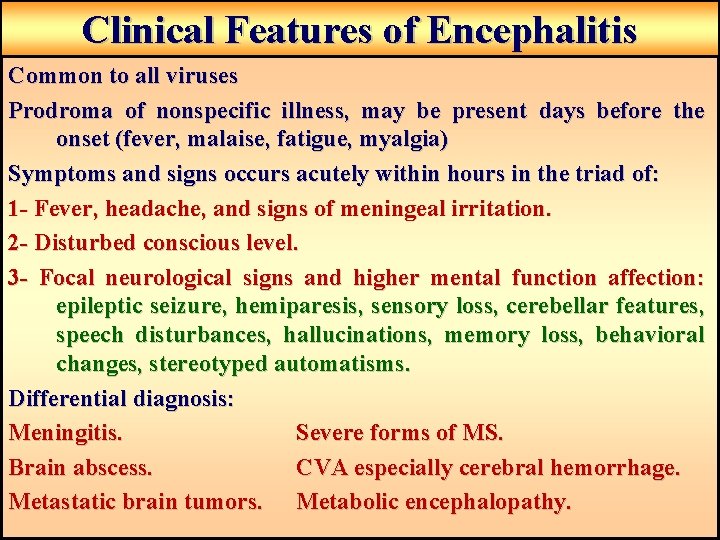
Clinical Features of Encephalitis Common to all viruses Prodroma of nonspecific illness, may be present days before the onset (fever, malaise, fatigue, myalgia) Symptoms and signs occurs acutely within hours in the triad of: 1 - Fever, headache, and signs of meningeal irritation. 2 - Disturbed conscious level. 3 - Focal neurological signs and higher mental function affection: epileptic seizure, hemiparesis, sensory loss, cerebellar features, speech disturbances, hallucinations, memory loss, behavioral changes, stereotyped automatisms. Differential diagnosis: Meningitis. Severe forms of MS. Brain abscess. CVA especially cerebral hemorrhage. Metastatic brain tumors. Metabolic encephalopathy.
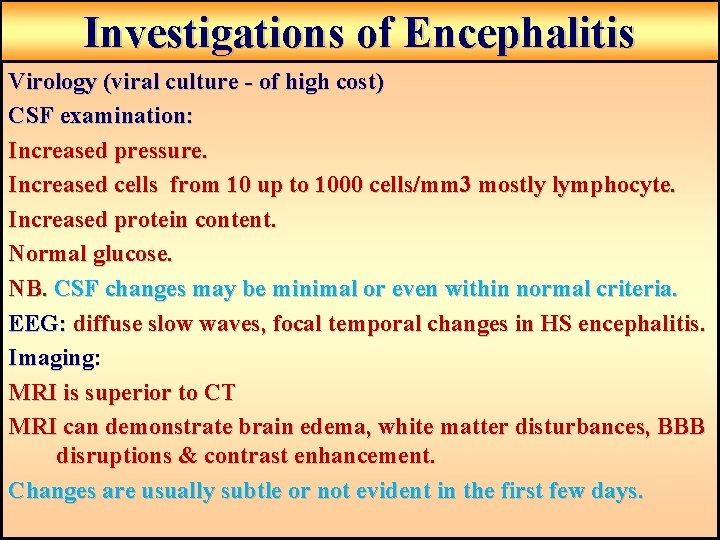
Investigations of Encephalitis Virology (viral culture - of high cost) CSF examination: Increased pressure. Increased cells from 10 up to 1000 cells/mm 3 mostly lymphocyte. Increased protein content. Normal glucose. NB. CSF changes may be minimal or even within normal criteria. EEG: diffuse slow waves, focal temporal changes in HS encephalitis. Imaging: MRI is superior to CT MRI can demonstrate brain edema, white matter disturbances, BBB disruptions & contrast enhancement. Changes are usually subtle or not evident in the first few days.
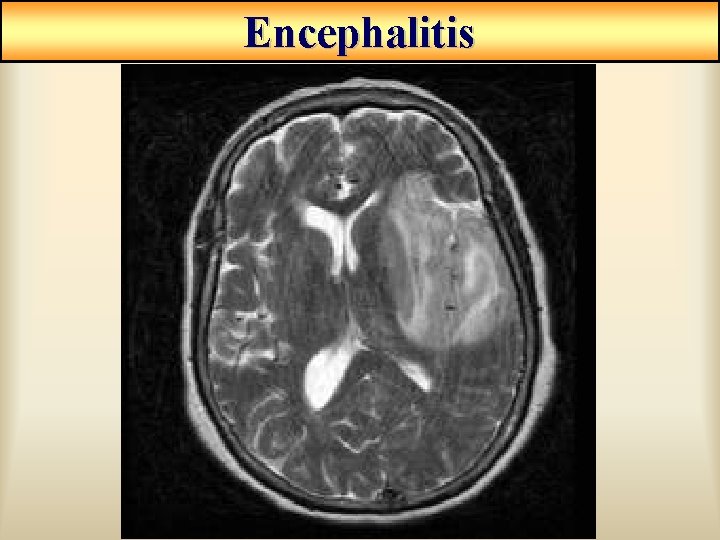
Encephalitis
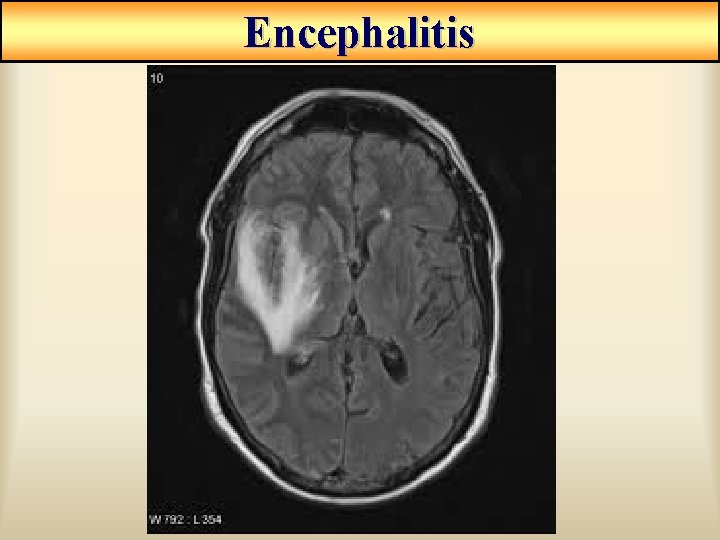
Encephalitis
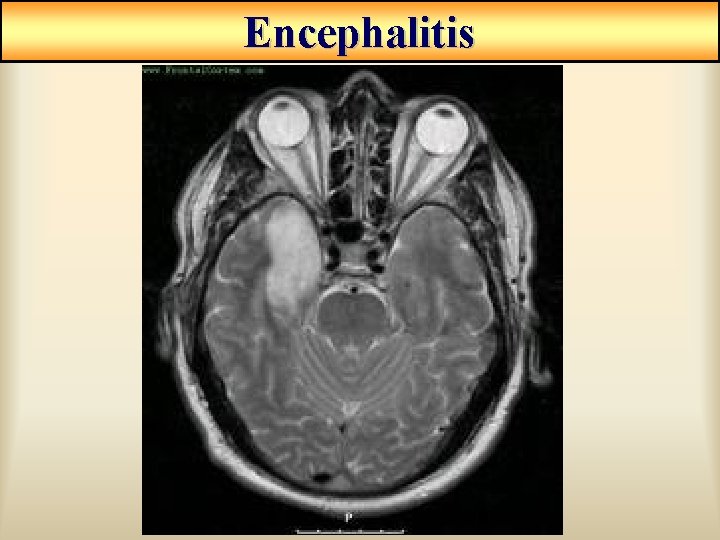
Encephalitis
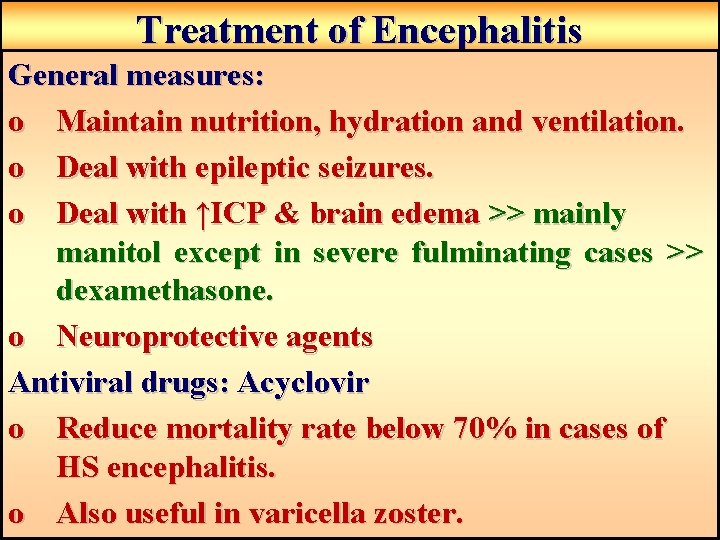
Treatment of Encephalitis General measures: o Maintain nutrition, hydration and ventilation. o Deal with epileptic seizures. o Deal with ↑ICP & brain edema >> mainly manitol except in severe fulminating cases >> dexamethasone. o Neuroprotective agents Antiviral drugs: Acyclovir o Reduce mortality rate below 70% in cases of HS encephalitis. o Also useful in varicella zoster.

- Slides: 30