Brain Death Concept and Certification Yan Wing Wa
Brain Death Concept and Certification Yan Wing Wa Department of Intensive Care Pamela Youde Nethersole Eastern Hospital Spring 2007 1

2
The earliest brain death case n n n 1963 UK Potter case. Potter suffered from severe brain injury in an assault. After resuscitation, Potter was in brain death state. Hospital took out one kidney from Potter after family’s agreement. Potter died soon after. Hospital was alleged murder and the jury supported. 3
n n 1967 first heart transplant from a comatose patient was performed in Republic of Africa. 1968 similar heart transplant was performed in Japan. A lot of debate created 4
Pros n n Brain death is irreversible and death is inevitable. Modern heart lung support is so advanced that it might cause more suffering to patient, family and society in brain death case. A person with permanent loss of brain response is equivalent to “death”. Open a new era for organ transplantation. 5
Cons n n Brain death concept was built on organ transplantation. It is difficult to bury a person with a beating heart. It is difficult for the public to understand the brain death concept and they are not prepared to accept it. Infants are mentally incompetent, declaration of infant brain death should better be more careful. 6
If “Brain death exist” n n If cardiopulmonary death (cardiopulmonary cessation-potentially revertible by resuscitation) precedes brain death, it may wrongly classified a patient as dead according to modern standard. Those patients with drug overdose, near-drowning and hypothermia may prematurely be classified as death. 7
n n Traditional heart lung definition of death is objective and transparent. Brain death certification is very much dependent on doctors’ subjection. Brain death definition is a “western” culture. It may cause cultural conflict if it is introduced by force into the oriental countries. 8
Brain Death in CHINA n n First brain death case in China was certified dead on 10 April 2003 in 武汉同济医院 for a patient with brain stem hemorrhage. Brain death legislation in China is still ongoing. 9
Brain Death = Death (in Hong Kong) under Common Law = ? Well accepted by people and the medical community in Hong Kong 10
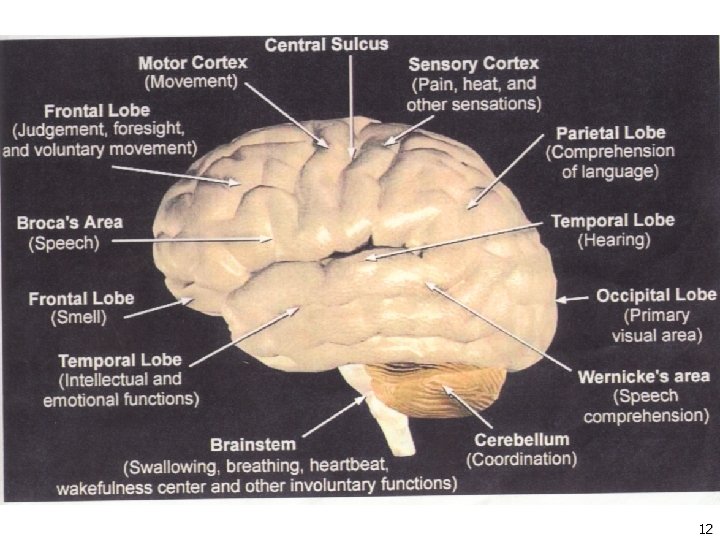
Brain Death n n Irreversible loss of function of the brain and brain stem – United States. Irreversible loss of function of the brain stem – United Kingdom, Australia, Hong Kong SAR. 11
12
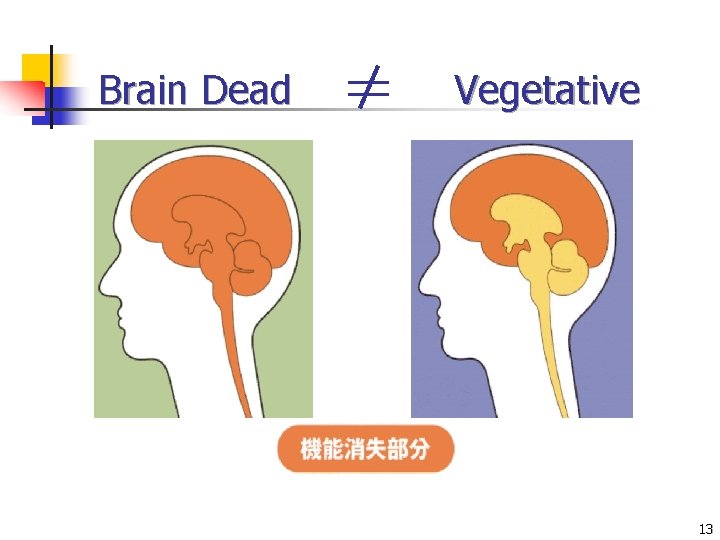
Brain Dead Vegetative 13

Brain Dead Patients n n n Lost vasomotor, temperature & breathing control irreversible. Rely on ventilator completely. Develop hypotension & cardiac arrest inevitably after a period of time (within a few hours to a few days). 14
Vegetative Patients n n Impaired cerebral functions: cognitive function, memory, motor power or speech. Brain stem still function: brain stem reflex responses +ve, spontaneous breathing & heart beating. 15

Brain Death Certification n Permit NO errors in classifying a living individual as dead n n Allow as few errors as possible in classifying a dead person as alive n n i. e. 100% specificity i. e. high sensivity, otherwise loss of potential donor organs Allow for determination to be made without unreasonable delay. n Be adaptable to a variety of clinical situations. n Be explicit and verifiable. 16
Guidelines on Diagnosis of Brain Death n Hospital Authority Head Office Operation Circular No. 7/95 17

Guidelines on Diagnosis of Brain Death n Adopted by Hospital Authority (COC in Intensive Care) Operations Circular 15/2003 20 November 2003 18

Guidelines on Diagnosis of Brain Death n n was drafted by the Hong Kong Society of Critical Care Medicine (HKSCCM) Brain Death Guidelines Working Group n n Dr Yan Wing Wa Dr Thomas Buckley Dr Wong Kwan Keung Dr So Hing Yu 19
n Input from all members in the HKSCCM Council Dr Chan Wai Ming, YCH Dr Claudia Cheng, PWH Dr Cheung Po Wa, NDH Dr Charles Gomersall, PWH Mr Stephen Ha Prof Gavin Joynt, PWH Dr Koo Chi Kwan, QEH Dr Lai Kang Yiu, QEH Dr Dr Anne Leung, PYNEH Phil Nelson, QMH Ian Tan, PYNEH Peggy Tan, TMH Tong Chak Kwan, PMH Florence Yap, PWH Karl Young, QMH 20
Comments were also invited from n 15 Colleges of HKAM n Hong Kong Transplantation Society n Nephrology Society n Neurology Society 21
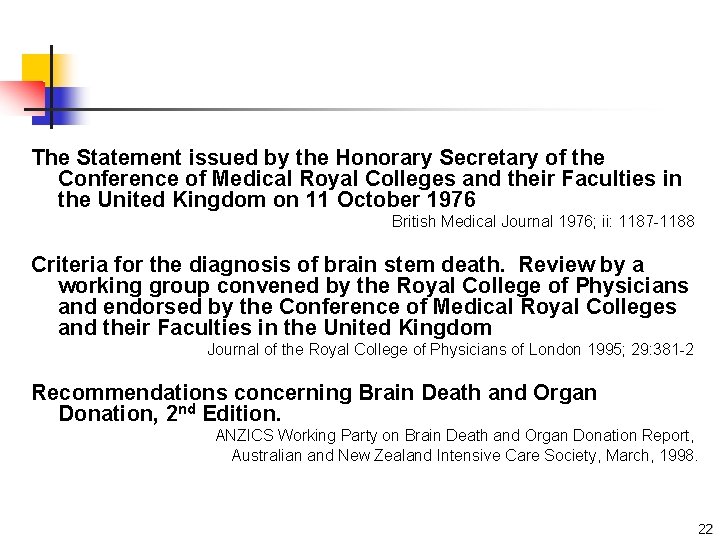
The Statement issued by the Honorary Secretary of the Conference of Medical Royal Colleges and their Faculties in the United Kingdom on 11 October 1976 British Medical Journal 1976; ii: 1187 -1188 Criteria for the diagnosis of brain stem death. Review by a working group convened by the Royal College of Physicians and endorsed by the Conference of Medical Royal Colleges and their Faculties in the United Kingdom Journal of the Royal College of Physicians of London 1995; 29: 381 -2 Recommendations concerning Brain Death and Organ Donation, 2 nd Edition. ANZICS Working Party on Brain Death and Organ Donation Report, Australian and New Zealand Intensive Care Society, March, 1998. 22
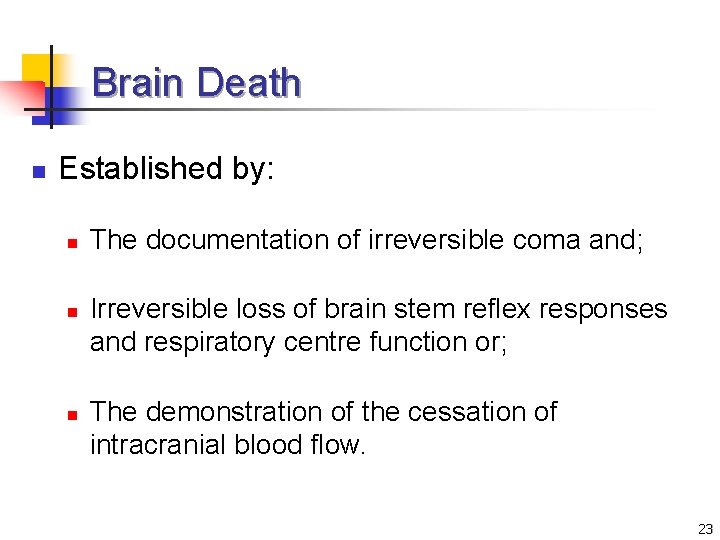
Brain Death n Established by: n n n The documentation of irreversible coma and; Irreversible loss of brain stem reflex responses and respiratory centre function or; The demonstration of the cessation of intracranial blood flow. 23
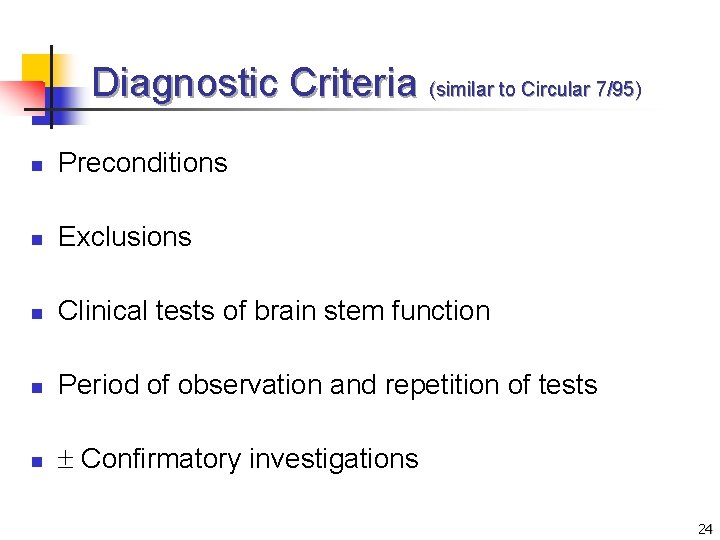
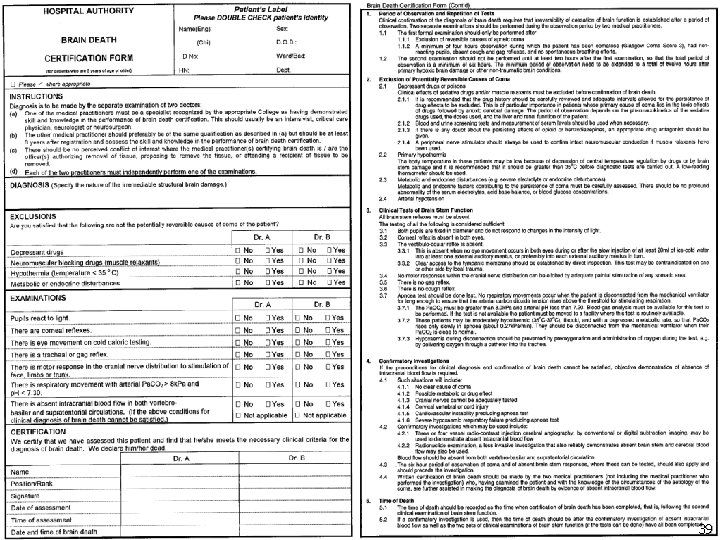
Diagnostic Criteria (similar to Circular 7/95) n Preconditions n Exclusions n Clinical tests of brain stem function n Period of observation and repetition of tests n Confirmatory investigations 24
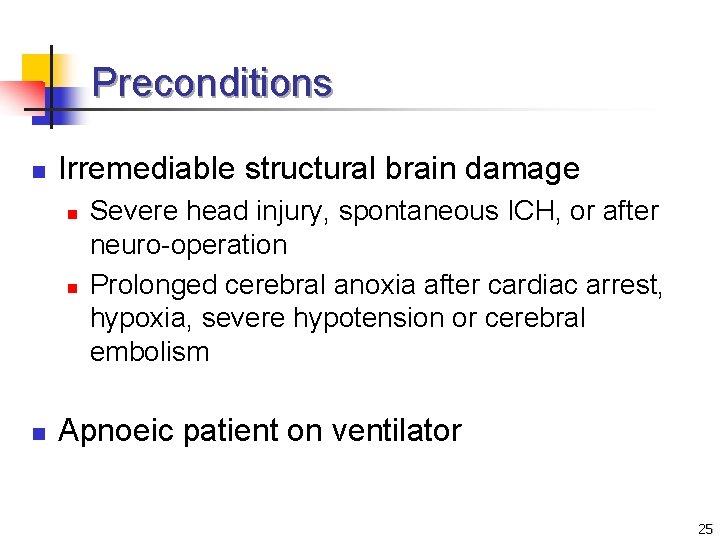
Preconditions n Irremediable structural brain damage n n n Severe head injury, spontaneous ICH, or after neuro-operation Prolonged cerebral anoxia after cardiac arrest, hypoxia, severe hypotension or cerebral embolism Apnoeic patient on ventilator 25
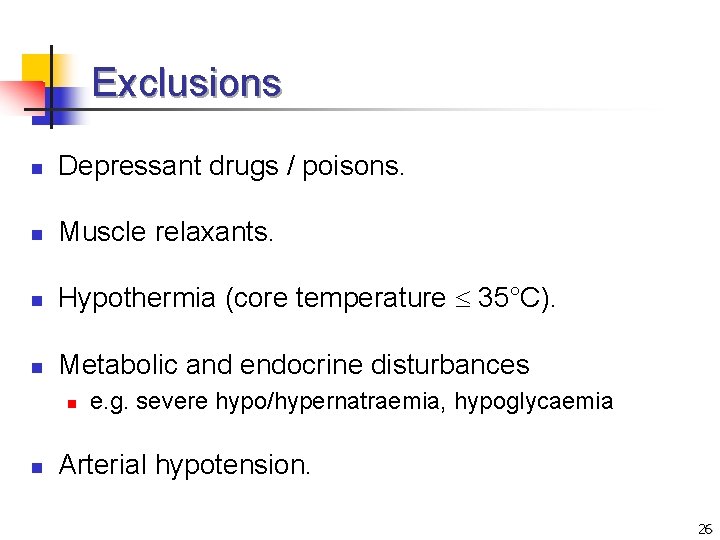
Exclusions n Depressant drugs / poisons. n Muscle relaxants. n Hypothermia (core temperature 35°C). n Metabolic and endocrine disturbances n n e. g. severe hypo/hypernatraemia, hypoglycaemia Arterial hypotension. 26

Clinical Tests of Brain Steam Function n Both pupils fixed and non-reactive to light. n Absent corneal reflex in both eyes. n Absent vestibulo-occular reflex (Caloric test) n n 20 ml ice-cold water into at least one external auditory meatus Absent motor responses within the cranial nerve. distribution by adequate painful stimulation in any somatic area. n Absent gag reflex. n Absent cough reflex. 27
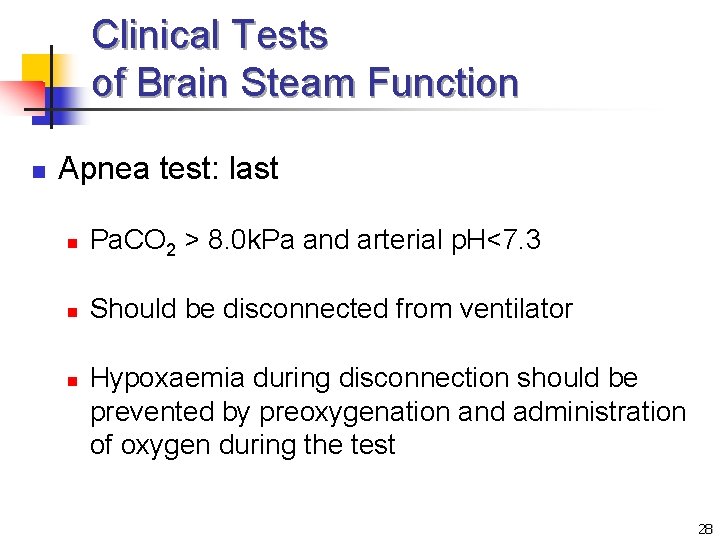
Clinical Tests of Brain Steam Function n Apnea test: last n Pa. CO 2 > 8. 0 k. Pa and arterial p. H<7. 3 n Should be disconnected from ventilator n Hypoxaemia during disconnection should be prevented by preoxygenation and administration of oxygen during the test 28
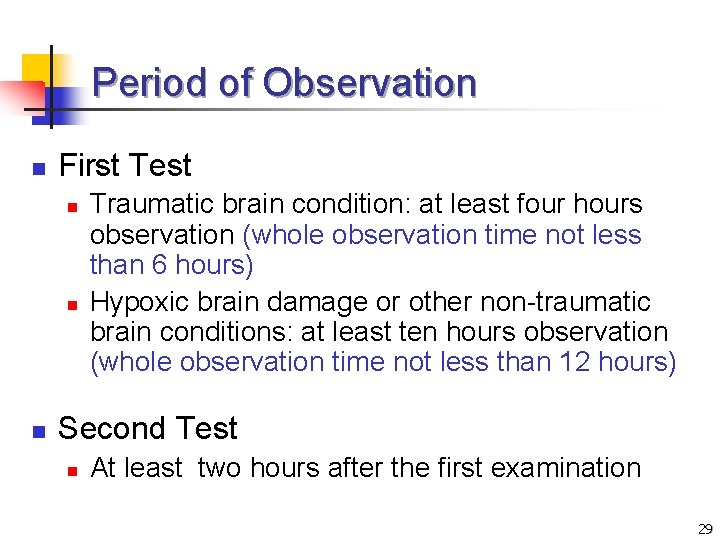
Period of Observation n First Test n n n Traumatic brain condition: at least four hours observation (whole observation time not less than 6 hours) Hypoxic brain damage or other non-traumatic brain conditions: at least ten hours observation (whole observation time not less than 12 hours) Second Test n At least two hours after the first examination 29
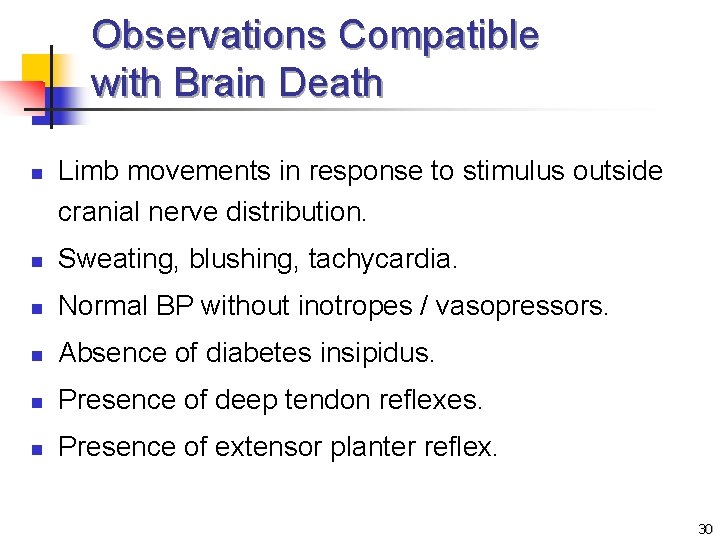
Observations Compatible with Brain Death n Limb movements in response to stimulus outside cranial nerve distribution. n Sweating, blushing, tachycardia. n Normal BP without inotropes / vasopressors. n Absence of diabetes insipidus. n Presence of deep tendon reflexes. n Presence of extensor planter reflex. 30
Confirmatory Investigations n Preconditions not satisfied e. g. n n n No clear cause of coma Possible metabolic or drug effect Cranial nerves not adequately tested Cervical cord injury Cardiovascular instability precluding apnoea test Severe hypoxaemic respiratory failure precluding apnoea test 31
Confirmatory Investigations n n Three or four vessel radio-contrast injection cerebral angiography (conventional / digital subtraction imaging) to demonstrate absence of intracranial blood flow. Radionuclide examination to demonstrate absence of brain stem and cerebral blood flow. 32
Time of Death n Recorded as the time when certification of brain death has been completed i. e. n Following the second brain stem examination or; n After confirmatory investigation, if required. 33
Medical Practitioners certifying brain death n NOT: n Designated officer authorising removal of tissue n Proposing to remove the tissue n Attending a recipient of tissue to be removed 34
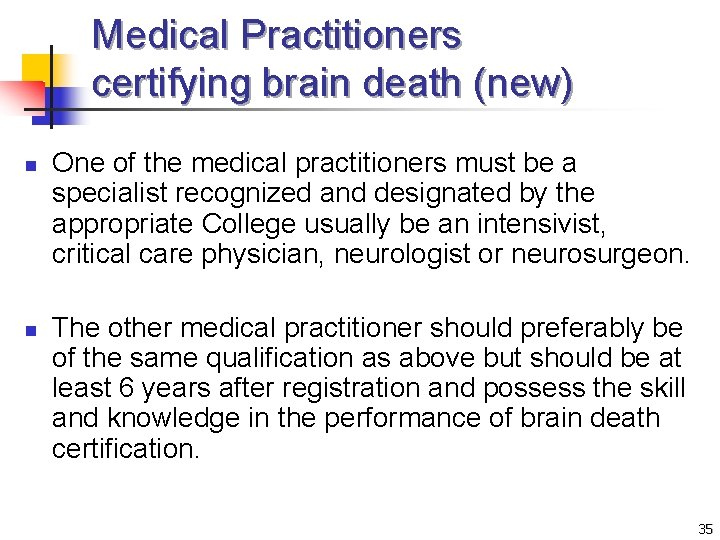
Medical Practitioners certifying brain death (new) n n One of the medical practitioners must be a specialist recognized and designated by the appropriate College usually be an intensivist, critical care physician, neurologist or neurosurgeon. The other medical practitioner should preferably be of the same qualification as above but should be at least 6 years after registration and possess the skill and knowledge in the performance of brain death certification. 35
Medical Practitioners certifying brain death Meticulous! n Falsely diagnosed a non-brain dead patient as brain dead is disastrous 36

13 May 2002 2 March 2003 37

26 Feb 2003 18 Feb 2003 38
39

Brain Death n For patients 5 year old n > 7 days: OK 40
Occulo-cephalic Reflex n Doll eyes sign n Not required n Trauma setting – not permitted 41
Keep Family Informed n Clinical team n n n Diagnosis and likely prognosis starting from the very beginning The transplant coordinators can be alerted on completion of the 1 st set of brain death test. Approach for organ donation should only start after completion of the whole brain death certification process, and is best done by transplant coordinators. 42
Questions / Comments 43

44
- Slides: 44