BRACHIAL PLEXUS IMAGING BRACHIAL PLEXUS IMAGING Basic anatomy
BRACHIAL PLEXUS IMAGING
BRACHIAL PLEXUS IMAGING : • Basic anatomy • Pathologies affecting Brachial Plexus • Modalities of Imaging : v. Conventional methods. v. Ultrasound v. CT and CT Myelography v. MR
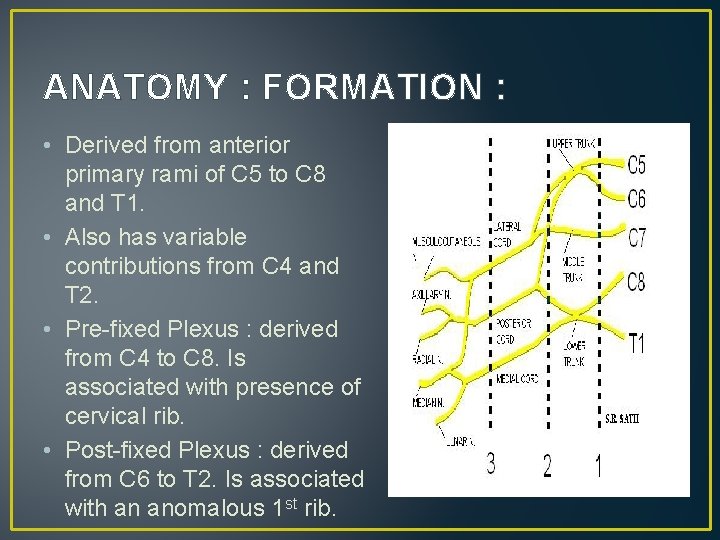
ANATOMY : FORMATION : • Derived from anterior primary rami of C 5 to C 8 and T 1. • Also has variable contributions from C 4 and T 2. • Pre-fixed Plexus : derived from C 4 to C 8. Is associated with presence of cervical rib. • Post-fixed Plexus : derived from C 6 to T 2. Is associated with an anomalous 1 st rib.
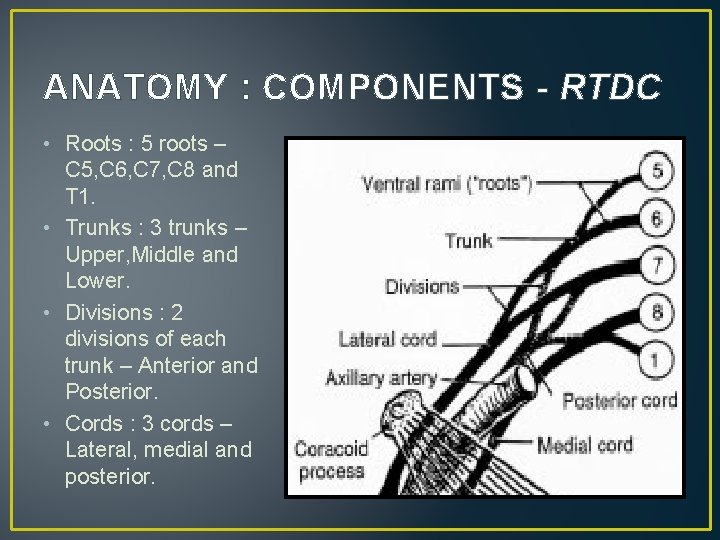
ANATOMY : COMPONENTS - RTDC • Roots : 5 roots – C 5, C 6, C 7, C 8 and T 1. • Trunks : 3 trunks – Upper, Middle and Lower. • Divisions : 2 divisions of each trunk – Anterior and Posterior. • Cords : 3 cords – Lateral, medial and posterior.
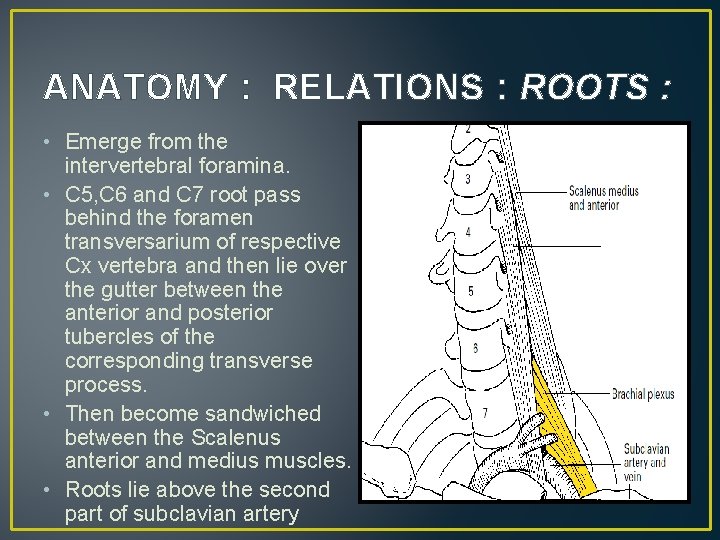
ANATOMY : RELATIONS : ROOTS : • Emerge from the intervertebral foramina. • C 5, C 6 and C 7 root pass behind the foramen transversarium of respective Cx vertebra and then lie over the gutter between the anterior and posterior tubercles of the corresponding transverse process. • Then become sandwiched between the Scalenus anterior and medius muscles. • Roots lie above the second part of subclavian artery
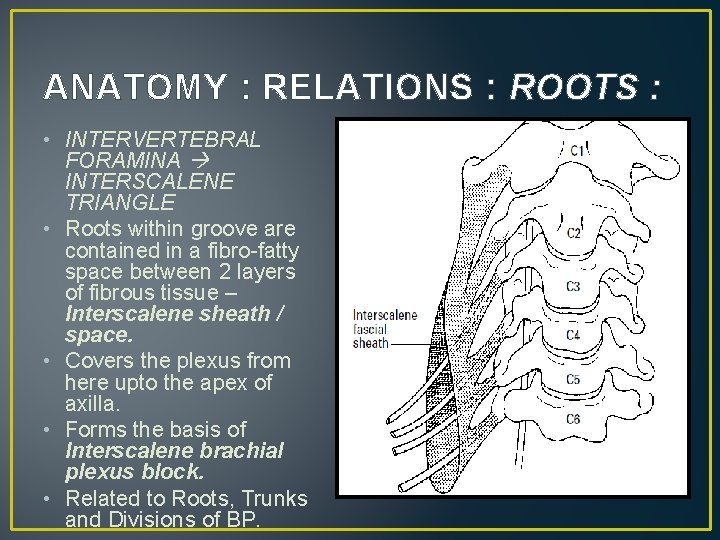
ANATOMY : RELATIONS : ROOTS : • INTERVERTEBRAL FORAMINA INTERSCALENE TRIANGLE • Roots within groove are contained in a fibro-fatty space between 2 layers of fibrous tissue – Interscalene sheath / space. • Covers the plexus from here upto the apex of axilla. • Forms the basis of Interscalene brachial plexus block. • Related to Roots, Trunks and Divisions of BP.
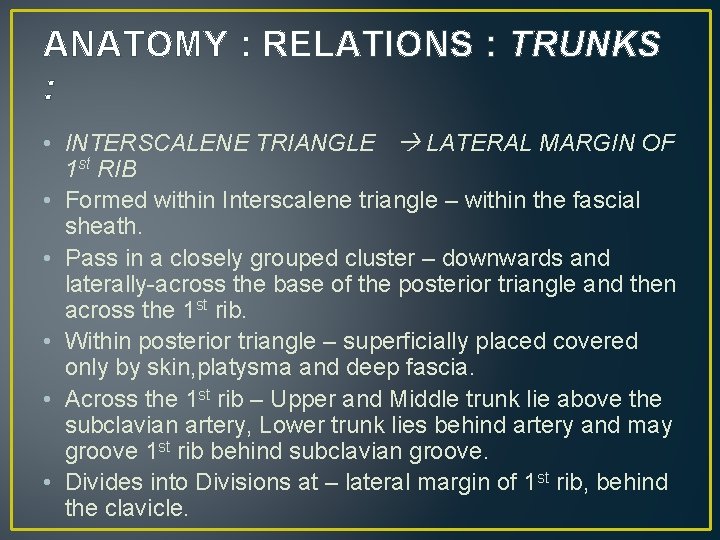
ANATOMY : RELATIONS : TRUNKS : • INTERSCALENE TRIANGLE LATERAL MARGIN OF 1 st RIB • Formed within Interscalene triangle – within the fascial sheath. • Pass in a closely grouped cluster – downwards and laterally-across the base of the posterior triangle and then across the 1 st rib. • Within posterior triangle – superficially placed covered only by skin, platysma and deep fascia. • Across the 1 st rib – Upper and Middle trunk lie above the subclavian artery, Lower trunk lies behind artery and may groove 1 st rib behind subclavian groove. • Divides into Divisions at – lateral margin of 1 st rib, behind the clavicle.
ANATOMY : RELATIONS : DIVISIONS : • LATERAL BORDER OF 1 st RIB APEX OF AXILLA. • Situated behind the Clavicle, Subclavius muscle and Suprascapular vessels. • Project into the axilla through its apex – then regroup to form the cords.
ANATOMY : RELATIONS : CORDS : • WITHIN AXILLA • Lateral, Medial and Posterior : Named after their relation with the axillary artery. • Initially the medial cord lies posterior to axillary artery and lateral and posterior cord lie lateral to axillary artery. • Later they assume the positions as per their name.
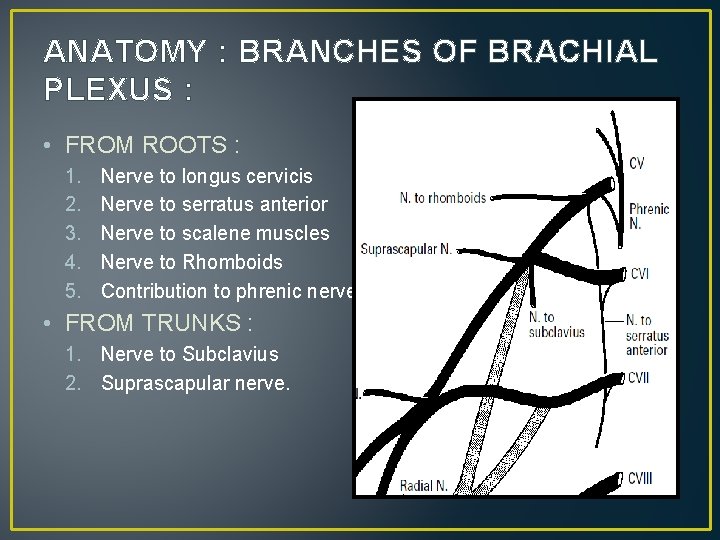
ANATOMY : BRANCHES OF BRACHIAL PLEXUS : • FROM ROOTS : 1. 2. 3. 4. 5. Nerve to longus cervicis Nerve to serratus anterior Nerve to scalene muscles Nerve to Rhomboids Contribution to phrenic nerve. • FROM TRUNKS : 1. Nerve to Subclavius 2. Suprascapular nerve.
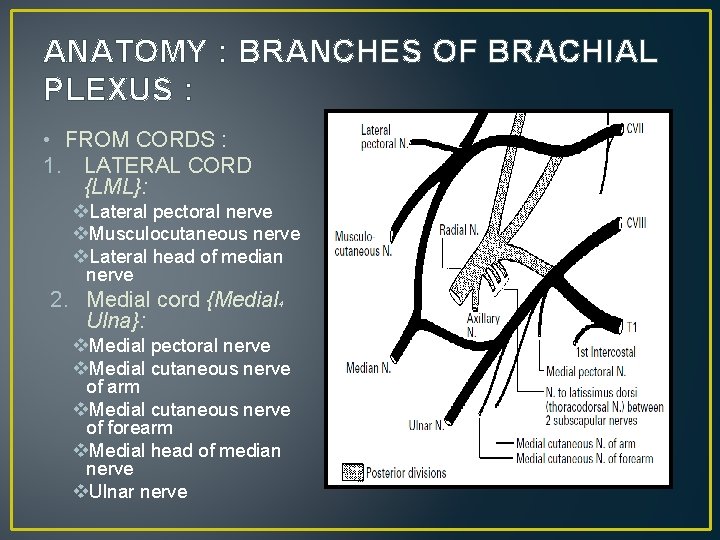
ANATOMY : BRANCHES OF BRACHIAL PLEXUS : • FROM CORDS : 1. LATERAL CORD {LML}: v. Lateral pectoral nerve v. Musculocutaneous nerve v. Lateral head of median nerve 2. Medial cord {Medial Ulna}: 4 v. Medial pectoral nerve v. Medial cutaneous nerve of arm v. Medial cutaneous nerve of forearm v. Medial head of median nerve v. Ulnar nerve
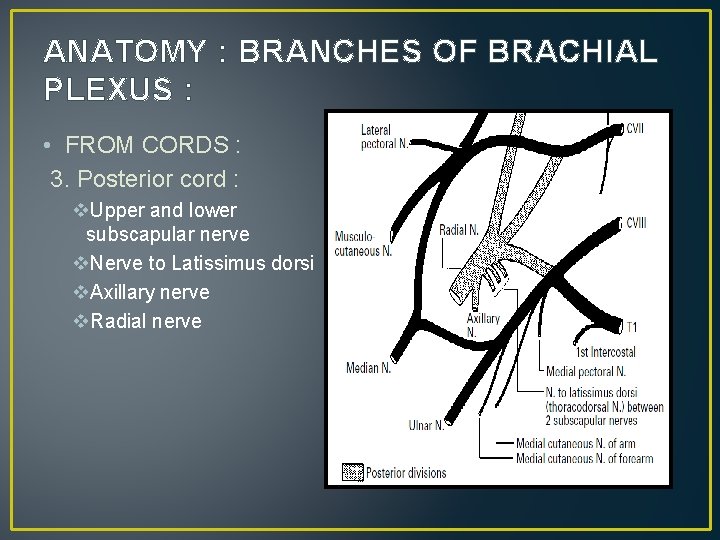
ANATOMY : BRANCHES OF BRACHIAL PLEXUS : • FROM CORDS : 3. Posterior cord : v. Upper and lower subscapular nerve v. Nerve to Latissimus dorsi v. Axillary nerve v. Radial nerve
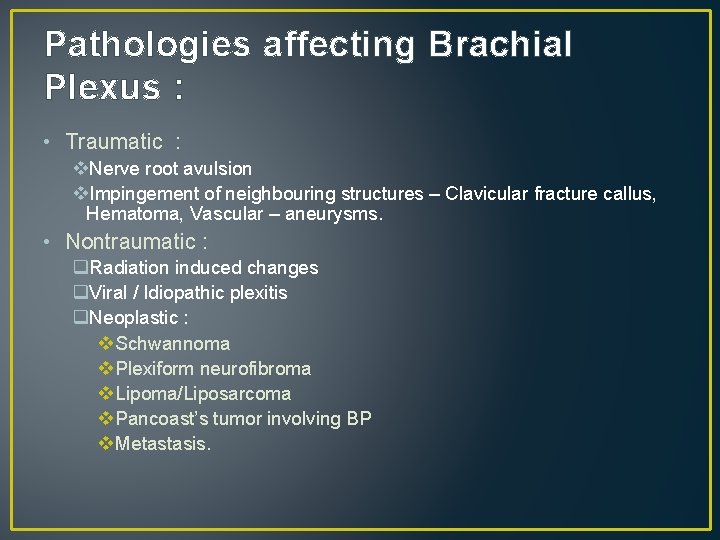
Pathologies affecting Brachial Plexus : • Traumatic : v. Nerve root avulsion v. Impingement of neighbouring structures – Clavicular fracture callus, Hematoma, Vascular – aneurysms. • Nontraumatic : q. Radiation induced changes q. Viral / Idiopathic plexitis q. Neoplastic : v Schwannoma v Plexiform neurofibroma v Lipoma/Liposarcoma v Pancoast’s tumor involving BP v Metastasis.
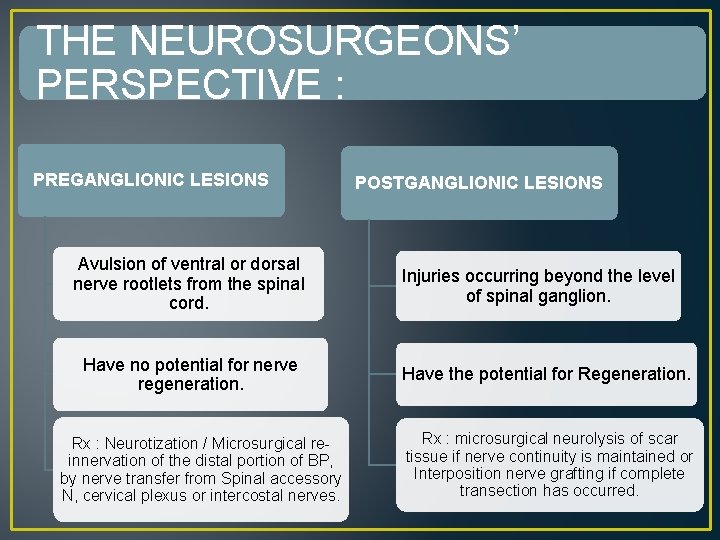
THE NEUROSURGEONS’ PERSPECTIVE : PREGANGLIONIC LESIONS Avulsion of ventral or dorsal nerve rootlets from the spinal cord. Have no potential for nerve regeneration. Rx : Neurotization / Microsurgical reinnervation of the distal portion of BP, by nerve transfer from Spinal accessory N, cervical plexus or intercostal nerves. POSTGANGLIONIC LESIONS Injuries occurring beyond the level of spinal ganglion. Have the potential for Regeneration. Rx : microsurgical neurolysis of scar tissue if nerve continuity is maintained or Interposition nerve grafting if complete transection has occurred.
IMAGING : CONVENTIONAL METHODS • Are of limited use. • Provide indirect evidence of BP pathology rather than its actual demonstration. • X-RAYS : • Specific sites of involvement may raise suspicion about possibility of brachial plexus involvement. • Chest Xray : S/o Pancoasts tumour may raise doubts about BP involvement. • Clavicular fractures : May be associated with BP injury
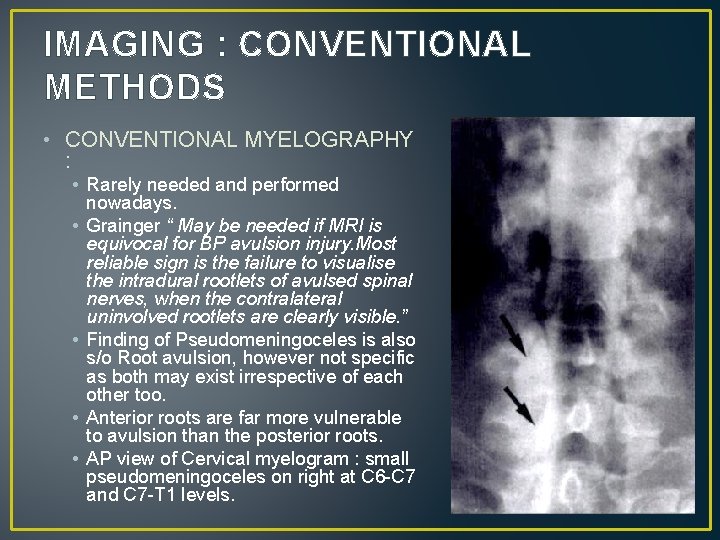
IMAGING : CONVENTIONAL METHODS • CONVENTIONAL MYELOGRAPHY : • Rarely needed and performed nowadays. • Grainger “ May be needed if MRI is equivocal for BP avulsion injury. Most reliable sign is the failure to visualise the intradural rootlets of avulsed spinal nerves, when the contralateral uninvolved rootlets are clearly visible. ” • Finding of Pseudomeningoceles is also s/o Root avulsion, however not specific as both may exist irrespective of each other too. • Anterior roots are far more vulnerable to avulsion than the posterior roots. • AP view of Cervical myelogram : small pseudomeningoceles on right at C 6 -C 7 and C 7 -T 1 levels.
IMAGING : HIGH RESOLUTION ULTRASOUND • HRU refers to use of high frequency probes (7 – 15 Mhz). • Based on identification of “Typical characteristics of peripheral nerves : ” v. More echogenic than muscles but less echogenic than tendons. v. Honeycomb appearance v. Less mobile than tendons. • Characteristics of diseased nerves : v. Nerve enlargement v. Hypoechoic signal resulting from nerve edema. v. Discontinuity of nerve fascilcles- Complete or Partial.
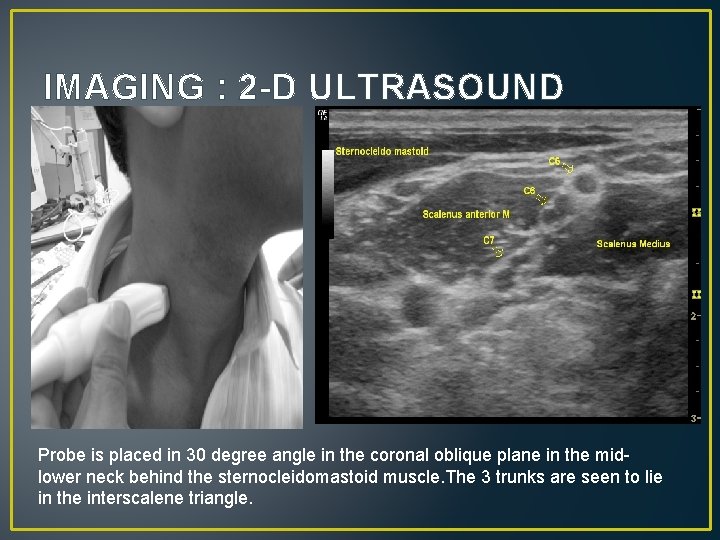
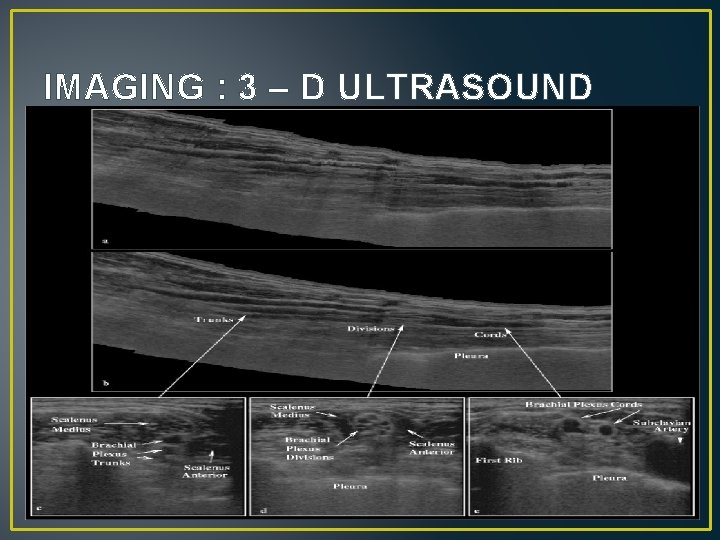
IMAGING : 2 -D ULTRASOUND Probe is placed in 30 degree angle in the coronal oblique plane in the midlower neck behind the sternocleidomastoid muscle. The 3 trunks are seen to lie in the interscalene triangle.
IMAGING - 2 -D ULTRASOUND • Start with 30 degree angle in the oblique coronal plane identifying trunks in the interscalene triangle and then trace them proximally and distally. • Patient position : Sitting position with head neutral or turned to opposite side by 10 – 20 degrees. • Roots C 8 -T 1 are most difficult to visualise due to greater penetration required.
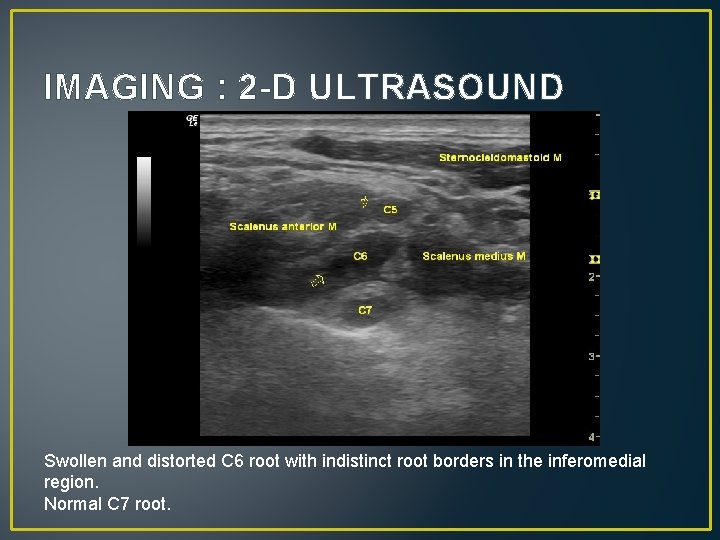
IMAGING : 2 -D ULTRASOUND Swollen and distorted C 6 root with indistinct root borders in the inferomedial region. Normal C 7 root.
IMAGING : 3 – D ULTRASOUND • HR Freehand Stradix – 3 D ultrasound system – Cambridge University Engineering Department. • Preserves much of the 2 D data resulting in a highly accurate 3 D data set with a point location accuracy of within 0. 5 mm. • Basic technique remains the same with patient seated, head rotated 30 degrees to contralateral side and arms by the side.
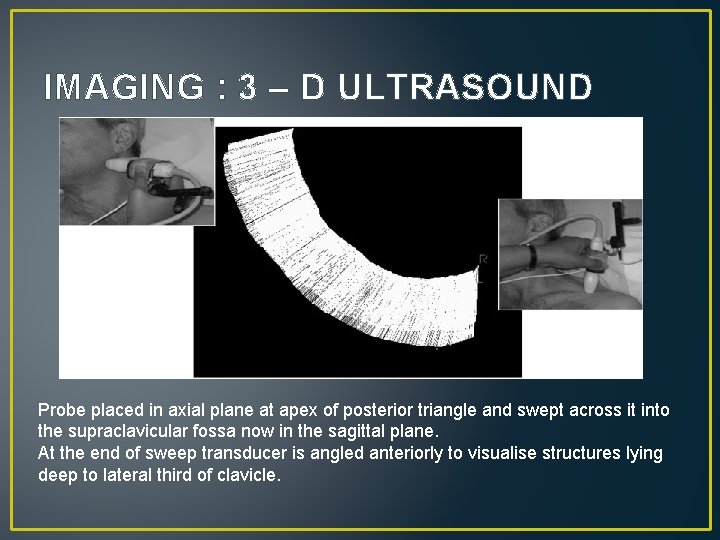
IMAGING : 3 – D ULTRASOUND Probe placed in axial plane at apex of posterior triangle and swept across it into the supraclavicular fossa now in the sagittal plane. At the end of sweep transducer is angled anteriorly to visualise structures lying deep to lateral third of clavicle.
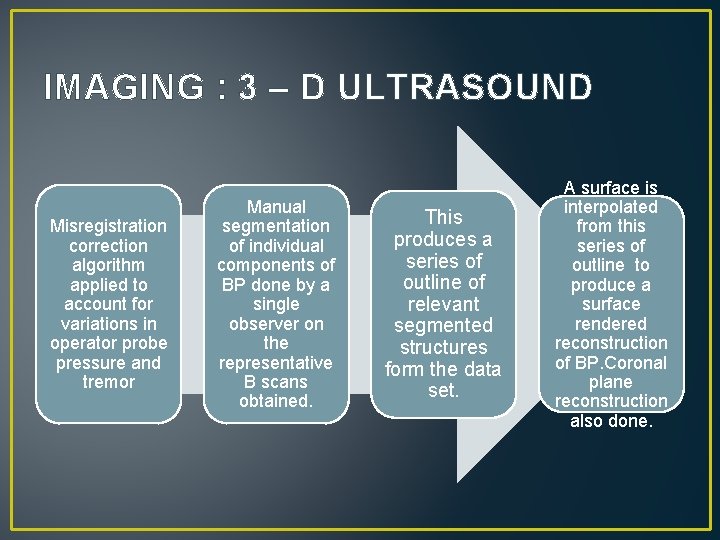
IMAGING : 3 – D ULTRASOUND Misregistration correction algorithm applied to account for variations in operator probe pressure and tremor Manual segmentation of individual components of BP done by a single observer on the representative B scans obtained. This produces a series of outline of relevant segmented structures form the data set. A surface is interpolated from this series of outline to produce a surface rendered reconstruction of BP. Coronal plane reconstruction also done.
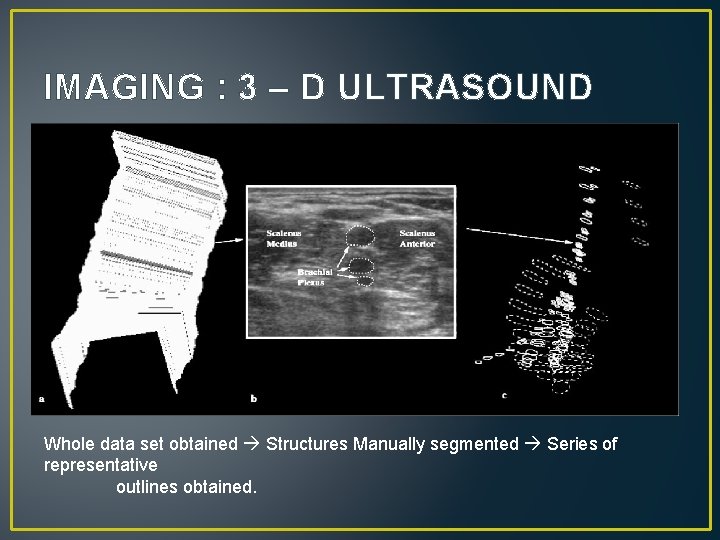
IMAGING : 3 – D ULTRASOUND Whole data set obtained Structures Manually segmented Series of representative outlines obtained.
IMAGING : 3 – D ULTRASOUND
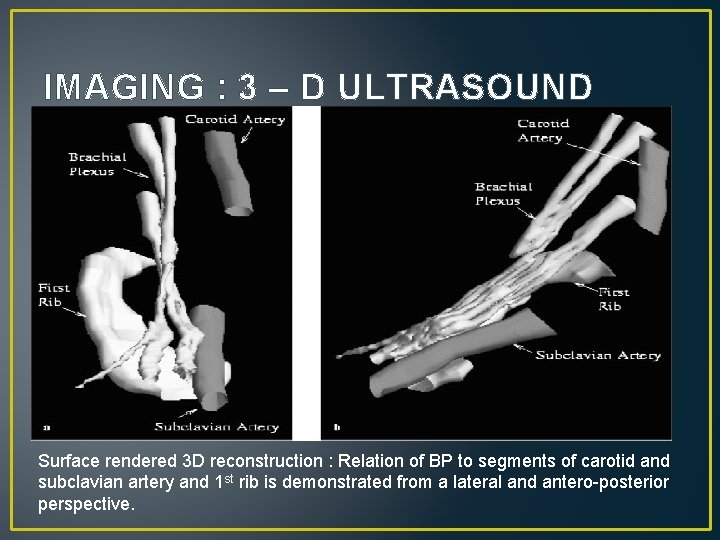
IMAGING : 3 – D ULTRASOUND Surface rendered 3 D reconstruction : Relation of BP to segments of carotid and subclavian artery and 1 st rib is demonstrated from a lateral and antero-posterior perspective.
IMAGING : 3 – D ULTRASOUND • Advantages of 3 D ultrasound : v. Allows frame by frame analysis of anatomy – better deliniation and better idetification of anatomical variations. v. Spatial reconstruction can be used in radiotherapy planning. With the advent of 3 D conformal radiotherapy and intensity-modulated radiotherapy (IMRT) , a spatial map of the brachial plexus could be imported into the planning system and the dose to the plexus adjusted accordingly. v. Better resolution by elimination of operator dependant factors such as probe pressure and tremors.
IMAGING : CT STUDIES • CT scans were used for BP imaging but : • Limited to the axial plane imaging. May be overcomed by recent softwares enabling reconstruction along Cor and Sag planes. • Dense shoulder bones and contrast within the Subclavian/Axillary vessels cause severe beam hardening artefacts and degrade the image quality. • Poorly timed bolus of contrast may make the identification of neighboring vessels difficult. These vessels need to be identified for correct evaluation of the BP. • Axial CT views are, in some centers, still considered as the Standard Reference in the pre-op assessment of Cx nerve root involvement in trauma cases. • Due to greater soft tissue resolution and multiplanar imaging MRI has gradually replaced CT in evaluation of pathologies of BP.
IMAGING : AXIAL CT MYELOGRAPHY • TECHNIQUE AND RESULTS : • Contiguous axial images were obtained from C 3 vertebra to upper part of T 2 vertebra. • For Infants : 1 mm thick sections at 1 mm intervals. • For Adults : 3 mm thick sections at 3 mm intervals. • High resolution reconstruction algorithm used. • Results : For complete nerve root avulsions : v. Sensitivity and Specificity of 95 % and 98 % resp. v. Positive and Negative Predictive value of 95 % and 98 %. • Partial nerve root avulsions are difficult to evaluate.
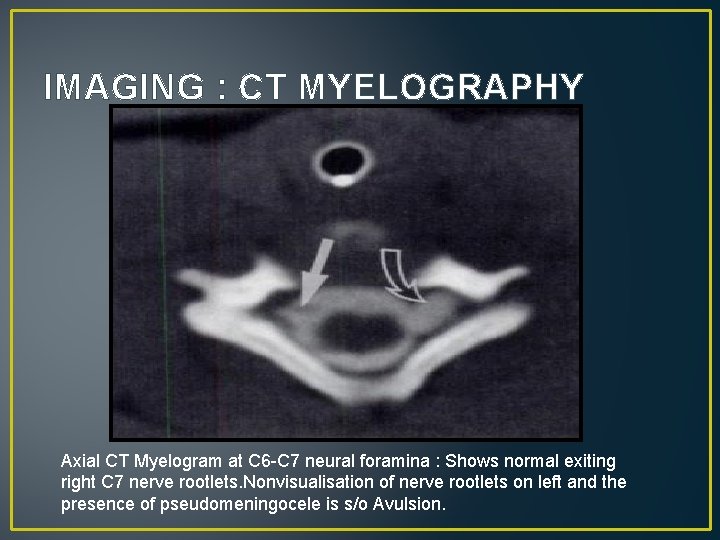
IMAGING : CT MYELOGRAPHY Axial CT Myelogram at C 6 -C 7 neural foramina : Shows normal exiting right C 7 nerve rootlets. Nonvisualisation of nerve rootlets on left and the presence of pseudomeningocele is s/o Avulsion.
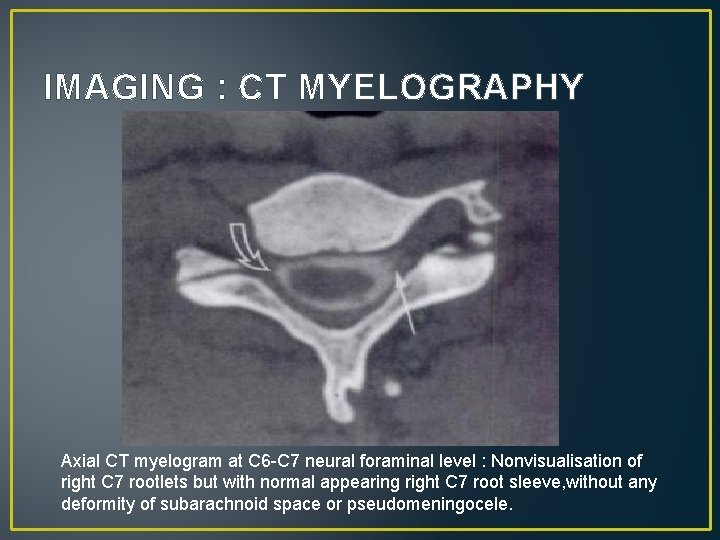
IMAGING : CT MYELOGRAPHY Axial CT myelogram at C 6 -C 7 neural foraminal level : Nonvisualisation of right C 7 rootlets but with normal appearing right C 7 root sleeve, without any deformity of subarachnoid space or pseudomeningocele.
IMAGING : CT MYELOGRAPHY • LIMITATIONS OF AXIAL CT MYELOGRAPHY : • Spinal nerve rootlets run in an oblique direction, so in axial plane entire visualisation from cord to exit foramina not possible. • As seen previously results though good for complete avulsion injury, are poor for partial injuries. • These shortcomings can be overcome by using Coronal and Oblique coronal reconstruction images of the Axial CT Myelogram.
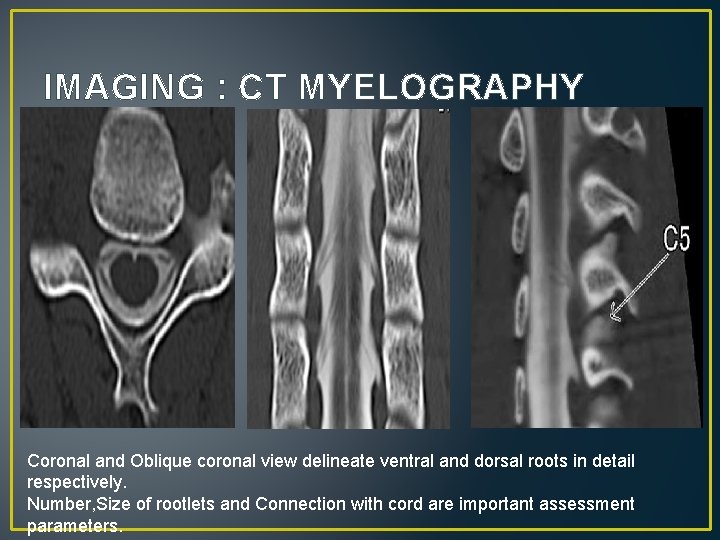
IMAGING : CT MYELOGRAPHY Coronal and Oblique coronal view delineate ventral and dorsal roots in detail respectively. Number, Size of rootlets and Connection with cord are important assessment parameters.
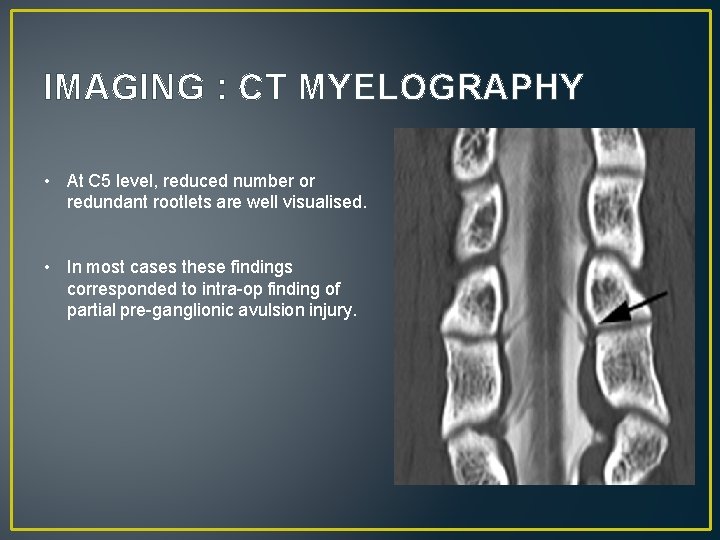
IMAGING : CT MYELOGRAPHY • At C 5 level, reduced number or redundant rootlets are well visualised. • In most cases these findings corresponded to intra-op finding of partial pre-ganglionic avulsion injury.
IMAGING : MRI • WHY MR i. S THE BEST FOR BP IMAGING ? v. Conventional radiography is far less sensitive. v. CT has improved sensitivity but has poor soft tissue resolution to identify nerves. v. With MRI detailed evaluation of all the components of brachial plexus – Roots, Trunks, Divisions and Cords – is possible. v. Has excellent soft tissue contrast. v. Has advantage of Multiplanar imaging.
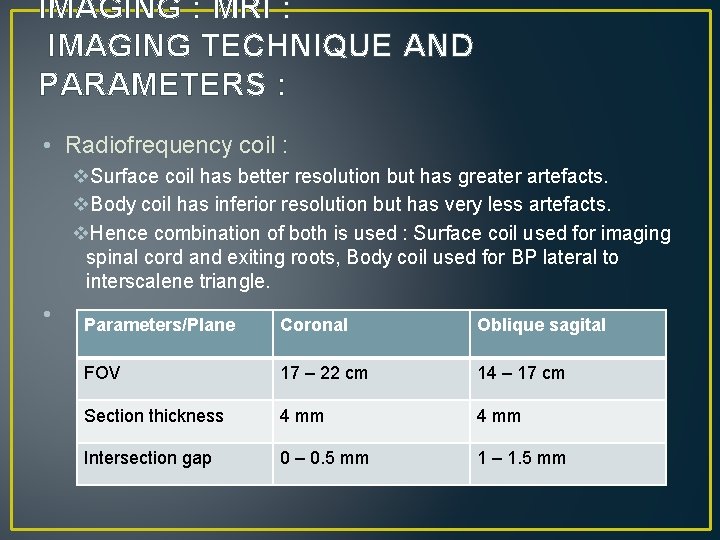
IMAGING : MRI : IMAGING TECHNIQUE AND PARAMETERS : • Radiofrequency coil : v. Surface coil has better resolution but has greater artefacts. v. Body coil has inferior resolution but has very less artefacts. v. Hence combination of both is used : Surface coil used for imaging spinal cord and exiting roots, Body coil used for BP lateral to interscalene triangle. • Parameters/Plane Coronal Oblique sagital FOV 17 – 22 cm 14 – 17 cm Section thickness 4 mm Intersection gap 0 – 0. 5 mm 1 – 1. 5 mm
IMAGING : MRI : IMAGING TECHNIQUE AND PARAMETERS : • Orientation : • Direct coronal plane imaging and Oblique sagital plane imaging is preferred as BP runs in a coronal plane from medial-superior to lateral-inferior direction. The individual nerve roots can be visualised in Axial plane alongwith sagital views of the exiting nerve roots. • Sequences : • • Coronal T 1 and STIR. Sag T 1 Axial T 1 and T 2 fat sat or STIR images. Post contrast T 1 fat sat if required
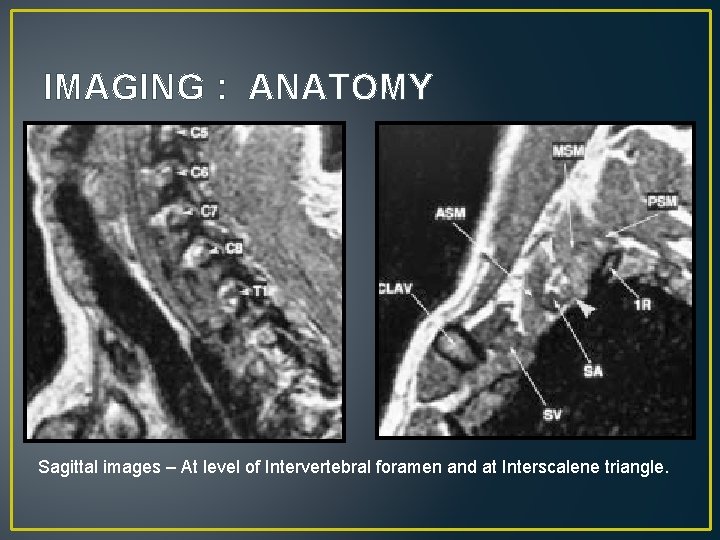
IMAGING : ANATOMY Sagittal images – At level of Intervertebral foramen and at Interscalene triangle.
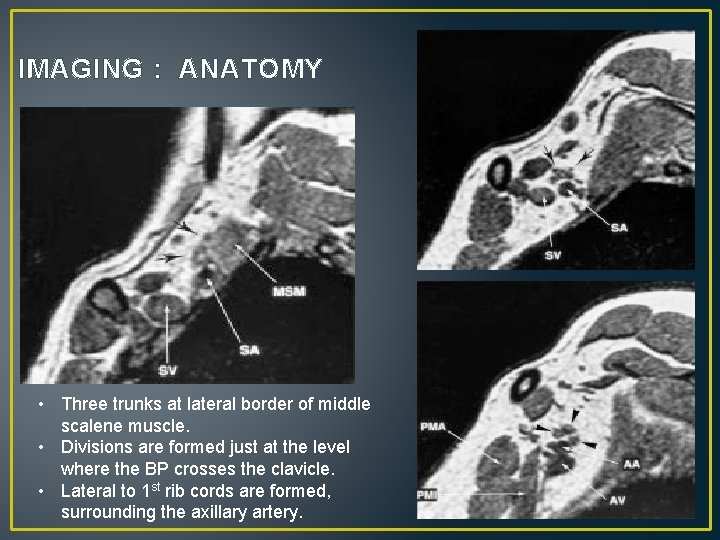
IMAGING : ANATOMY • Three trunks at lateral border of middle scalene muscle. • Divisions are formed just at the level where the BP crosses the clavicle. • Lateral to 1 st rib cords are formed, surrounding the axillary artery.
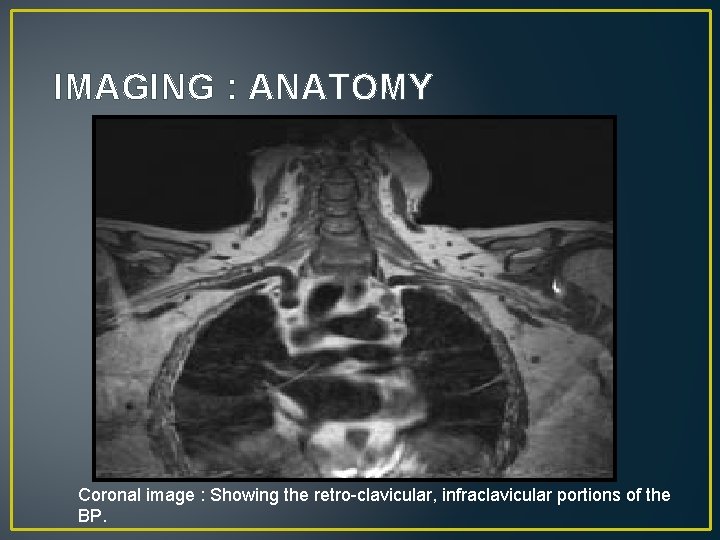
IMAGING : ANATOMY Coronal image : Showing the retro-clavicular, infraclavicular portions of the BP.
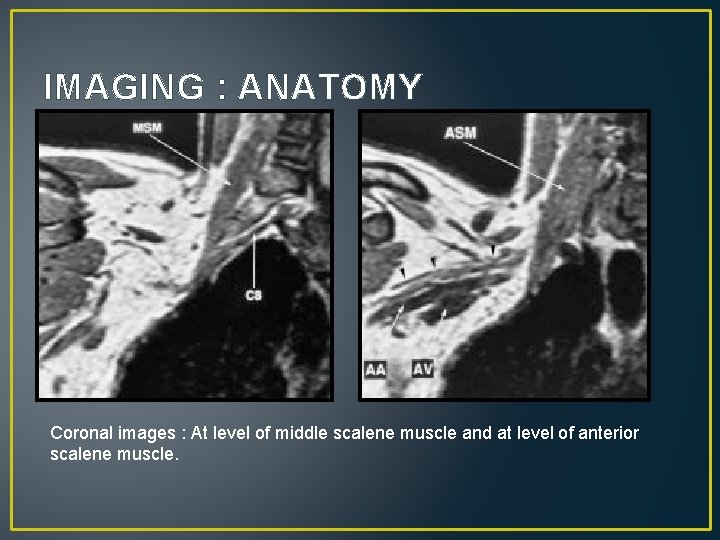
IMAGING : ANATOMY Coronal images : At level of middle scalene muscle and at level of anterior scalene muscle.
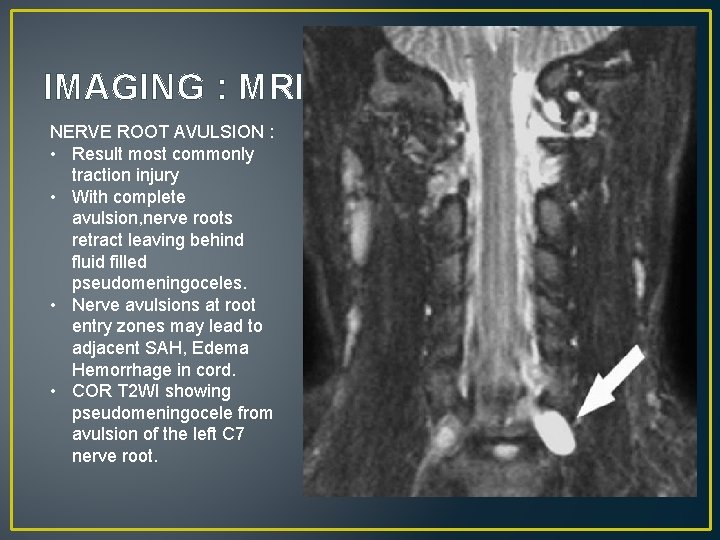
IMAGING : MRI NERVE ROOT AVULSION : • Result most commonly traction injury • With complete avulsion, nerve roots retract leaving behind fluid filled pseudomeningoceles. • Nerve avulsions at root entry zones may lead to adjacent SAH, Edema Hemorrhage in cord. • COR T 2 WI showing pseudomeningocele from avulsion of the left C 7 nerve root.
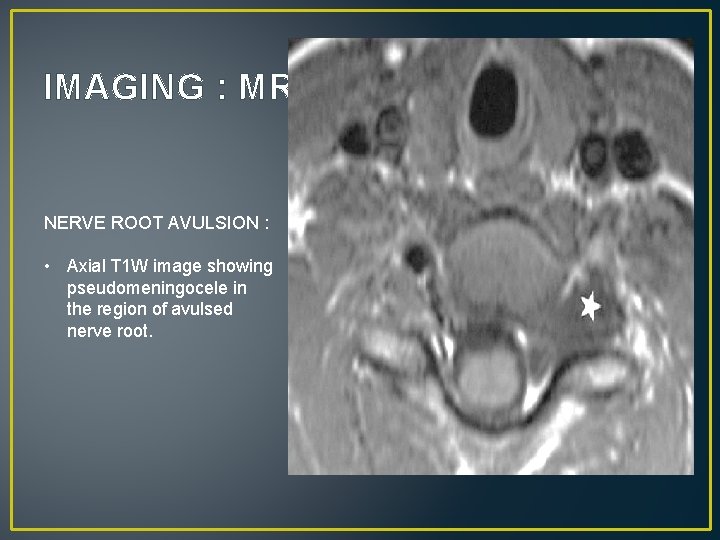
IMAGING : MRI NERVE ROOT AVULSION : • Axial T 1 W image showing pseudomeningocele in the region of avulsed nerve root.
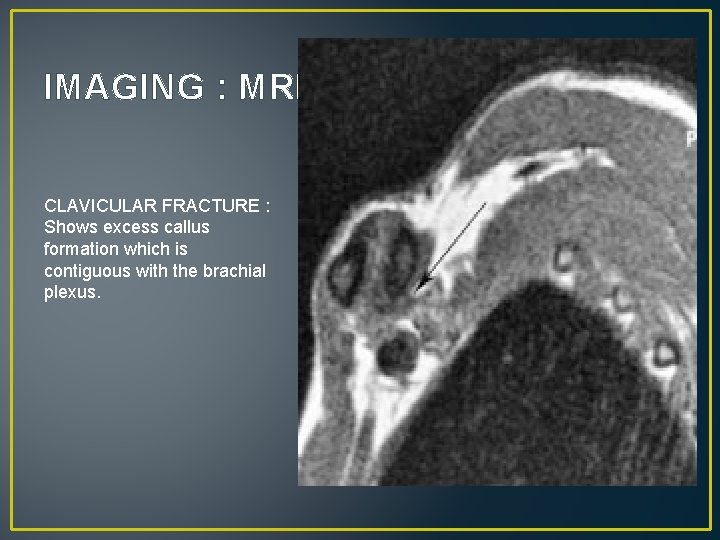
IMAGING : MRI CLAVICULAR FRACTURE : Shows excess callus formation which is contiguous with the brachial plexus.
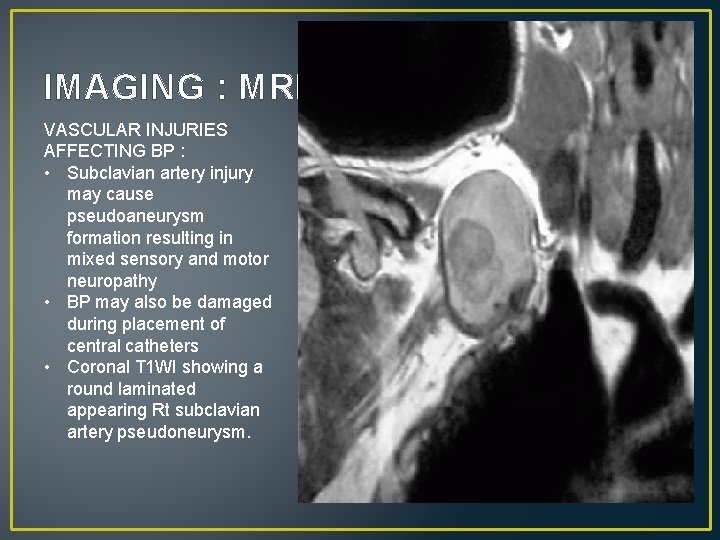
IMAGING : MRI VASCULAR INJURIES AFFECTING BP : • Subclavian artery injury may cause pseudoaneurysm formation resulting in mixed sensory and motor neuropathy • BP may also be damaged during placement of central catheters • Coronal T 1 WI showing a round laminated appearing Rt subclavian artery pseudoneurysm.
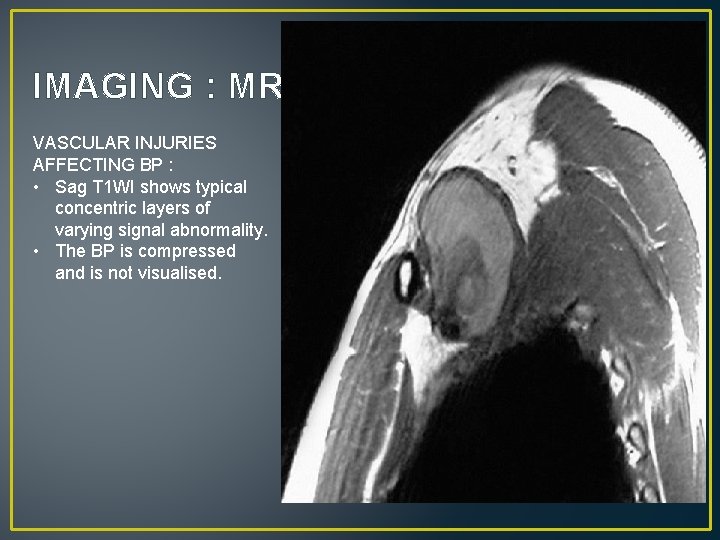
IMAGING : MRI VASCULAR INJURIES AFFECTING BP : • Sag T 1 WI shows typical concentric layers of varying signal abnormality. • The BP is compressed and is not visualised.
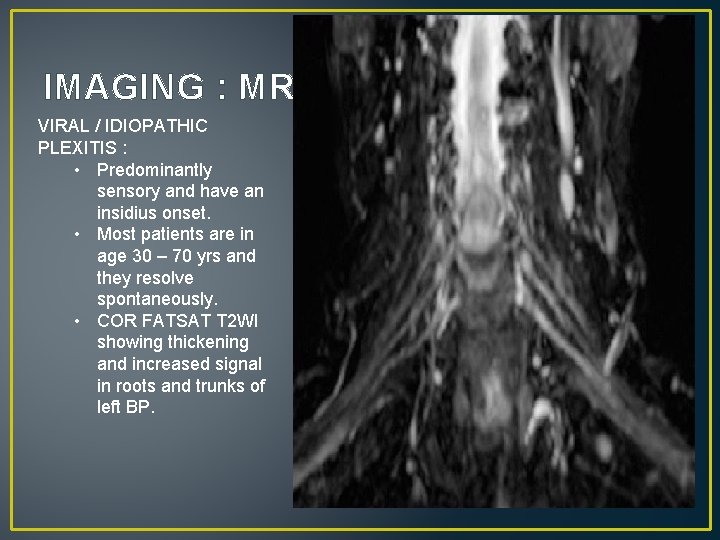
IMAGING : MRI VIRAL / IDIOPATHIC PLEXITIS : • Predominantly sensory and have an insidius onset. • Most patients are in age 30 – 70 yrs and they resolve spontaneously. • COR FATSAT T 2 WI showing thickening and increased signal in roots and trunks of left BP.
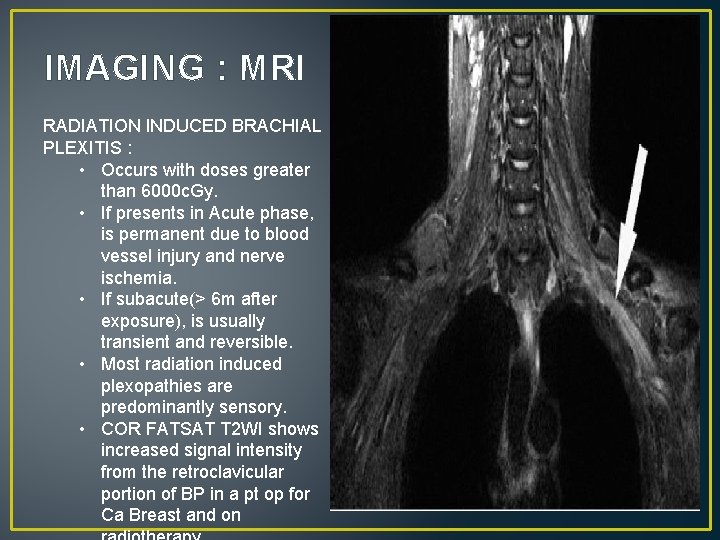
IMAGING : MRI RADIATION INDUCED BRACHIAL PLEXITIS : • Occurs with doses greater than 6000 c. Gy. • If presents in Acute phase, is permanent due to blood vessel injury and nerve ischemia. • If subacute(> 6 m after exposure), is usually transient and reversible. • Most radiation induced plexopathies are predominantly sensory. • COR FATSAT T 2 WI shows increased signal intensity from the retroclavicular portion of BP in a pt op for Ca Breast and on
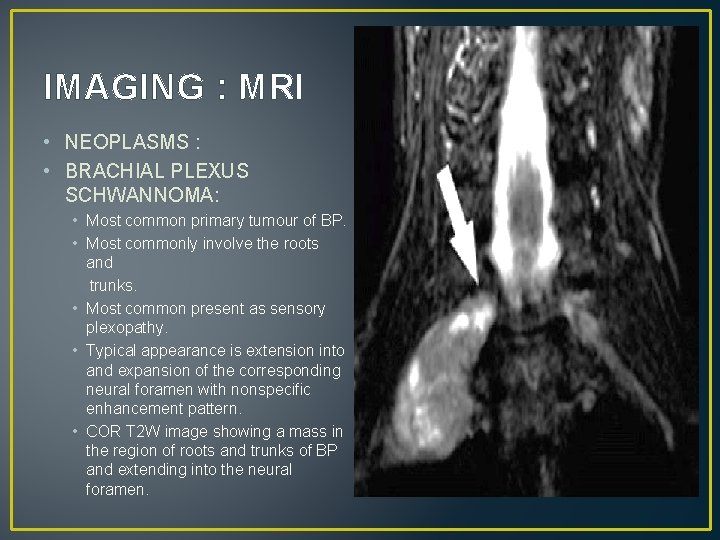
IMAGING : MRI • NEOPLASMS : • BRACHIAL PLEXUS SCHWANNOMA: • Most common primary tumour of BP. • Most commonly involve the roots and trunks. • Most common present as sensory plexopathy. • Typical appearance is extension into and expansion of the corresponding neural foramen with nonspecific enhancement pattern. • COR T 2 W image showing a mass in the region of roots and trunks of BP and extending into the neural foramen.
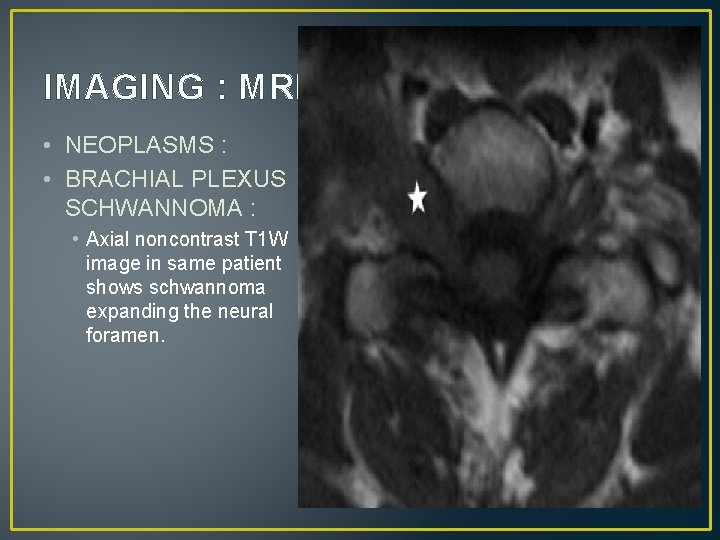
IMAGING : MRI • NEOPLASMS : • BRACHIAL PLEXUS SCHWANNOMA : • Axial noncontrast T 1 W image in same patient shows schwannoma expanding the neural foramen.
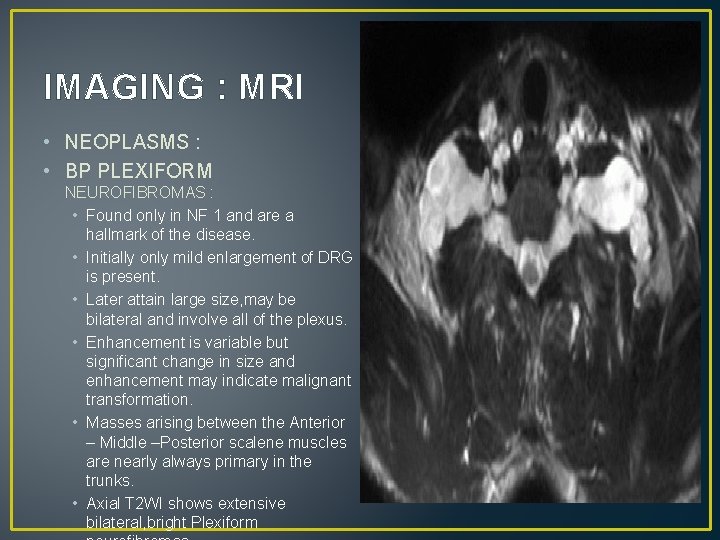
IMAGING : MRI • NEOPLASMS : • BP PLEXIFORM NEUROFIBROMAS : • Found only in NF 1 and are a hallmark of the disease. • Initially only mild enlargement of DRG is present. • Later attain large size, may be bilateral and involve all of the plexus. • Enhancement is variable but significant change in size and enhancement may indicate malignant transformation. • Masses arising between the Anterior – Middle –Posterior scalene muscles are nearly always primary in the trunks. • Axial T 2 WI shows extensive bilateral, bright Plexiform
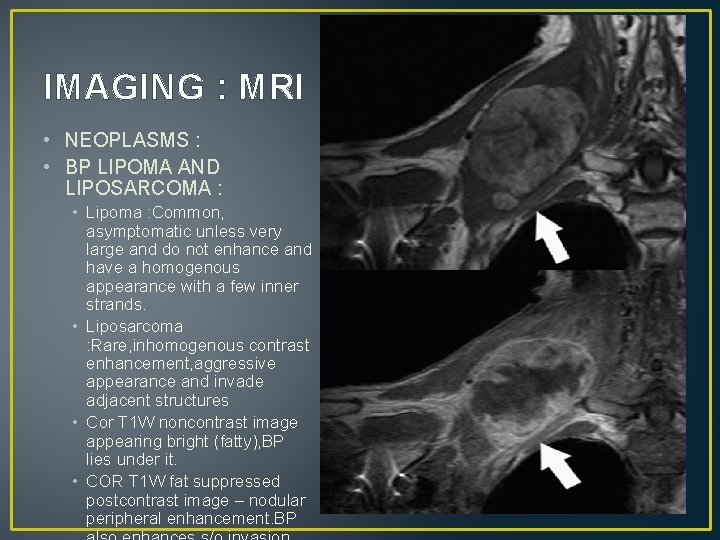
IMAGING : MRI • NEOPLASMS : • BP LIPOMA AND LIPOSARCOMA : • Lipoma : Common, asymptomatic unless very large and do not enhance and have a homogenous appearance with a few inner strands. • Liposarcoma : Rare, inhomogenous contrast enhancement, aggressive appearance and invade adjacent structures • Cor T 1 W noncontrast image appearing bright (fatty), BP lies under it. • COR T 1 W fat suppressed postcontrast image – nodular peripheral enhancement. BP
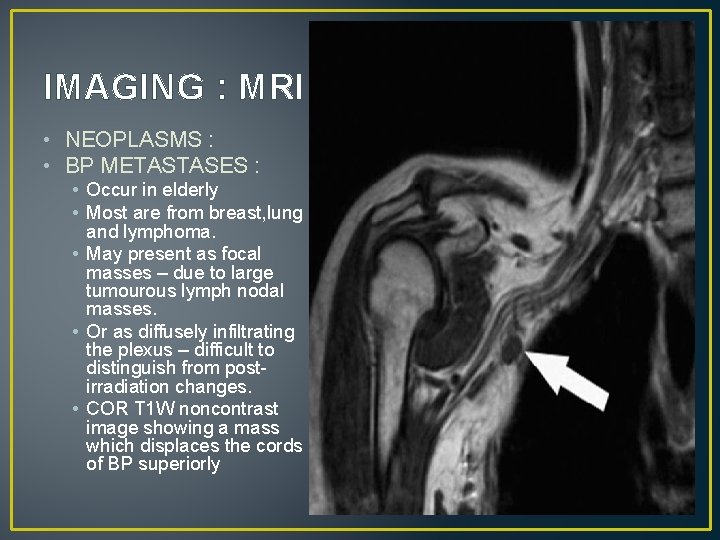
IMAGING : MRI • NEOPLASMS : • BP METASTASES : • Occur in elderly • Most are from breast, lung and lymphoma. • May present as focal masses – due to large tumourous lymph nodal masses. • Or as diffusely infiltrating the plexus – difficult to distinguish from postirradiation changes. • COR T 1 W noncontrast image showing a mass which displaces the cords of BP superiorly
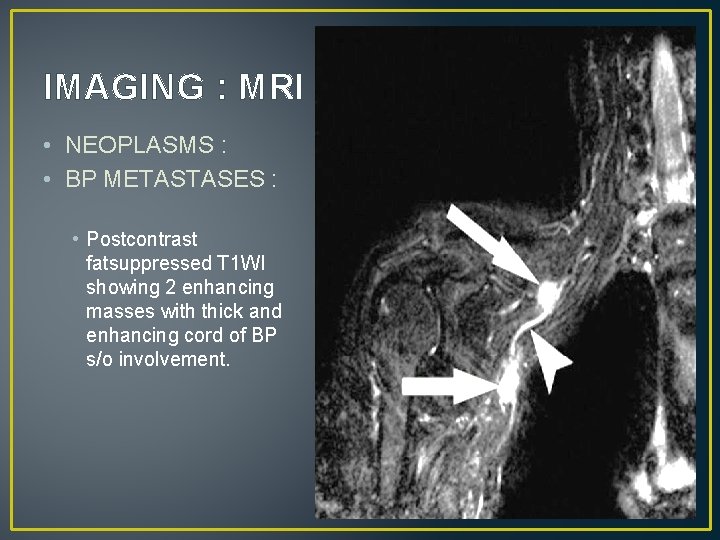
IMAGING : MRI • NEOPLASMS : • BP METASTASES : • Postcontrast fatsuppressed T 1 WI showing 2 enhancing masses with thick and enhancing cord of BP s/o involvement.
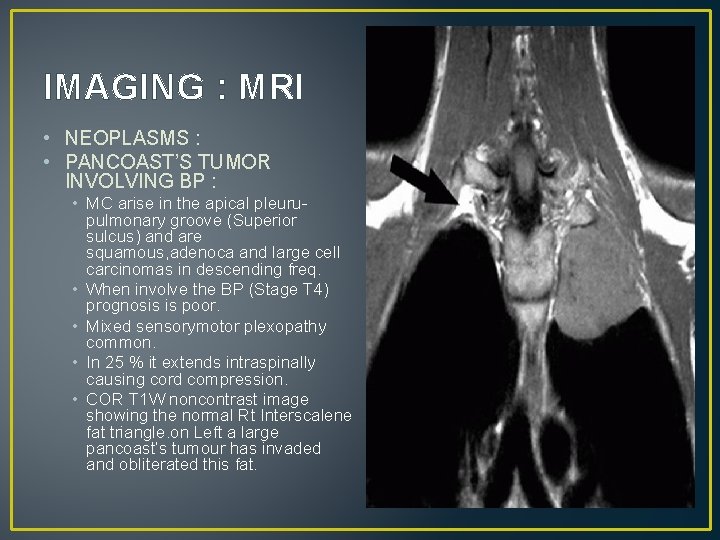
IMAGING : MRI • NEOPLASMS : • PANCOAST’S TUMOR INVOLVING BP : • MC arise in the apical pleurupulmonary groove (Superior sulcus) and are squamous, adenoca and large cell carcinomas in descending freq. • When involve the BP (Stage T 4) prognosis is poor. • Mixed sensorymotor plexopathy common. • In 25 % it extends intraspinally causing cord compression. • COR T 1 W noncontrast image showing the normal Rt Interscalene fat triangle. on Left a large pancoast’s tumour has invaded and obliterated this fat.
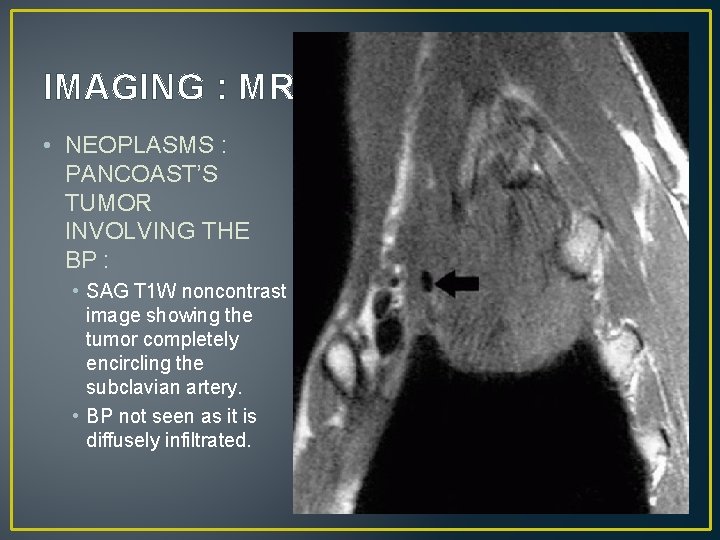
IMAGING : MRI • NEOPLASMS : PANCOAST’S TUMOR INVOLVING THE BP : • SAG T 1 W noncontrast image showing the tumor completely encircling the subclavian artery. • BP not seen as it is diffusely infiltrated.

THANK YOU. . !
- Slides: 57