Borrelia Epidemiology of Borrelia Infections Borrelia recurrentis Borrelia
Borrelia
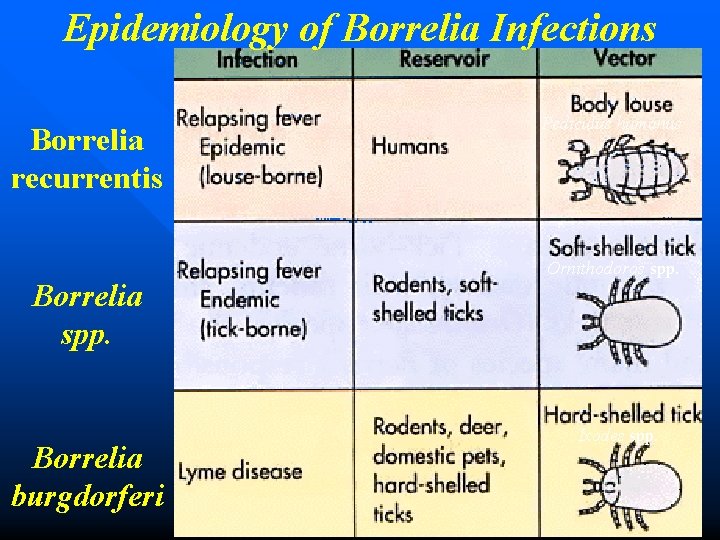
Epidemiology of Borrelia Infections Borrelia recurrentis Borrelia spp. Borrelia burgdorferi Pediculus humanus Ornithodoros spp. Ixodes spp.

Borrelia recurrentis other Borrelia spp. RELAPSING FEVER

Epidemiology of Relapsing Fever Ø Associated with poverty, crowding, warfare Ø Arthropod vectors • Louse-borne borreliosis = Epidemic Relapsing Fever ü Person-to-person transmission by human body lice (vectors), Infected human reservoir ü Caused by B. recurrentis ü Host infected: by scratching (crushing of louse) ü Lice leave host that develops a fever and seek normal temp host

– Tick-borne borreliosis = Endemic Relapsing Fever üSporadic cases üCaused by Borrelia spps üTransmitted by soft body ticks (vectors) from small mammal reservoir üTicks can multiply and infect new human hosts
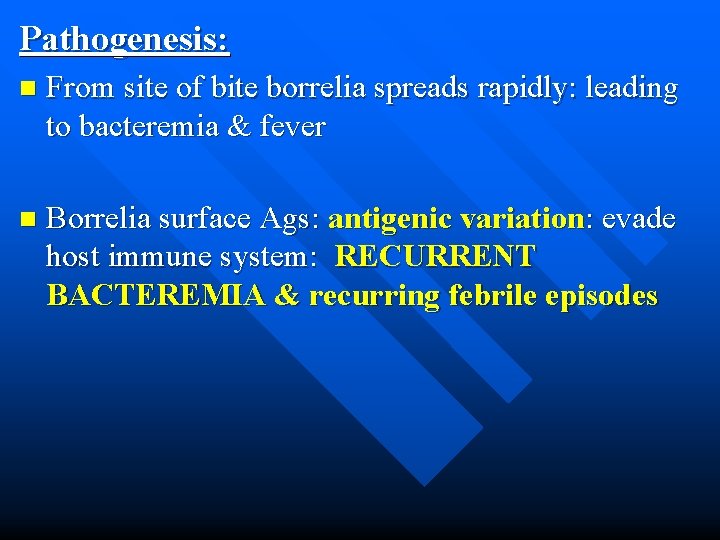
Pathogenesis: n From site of bite borrelia spreads rapidly: leading to bacteremia & fever n Borrelia surface Ags: antigenic variation: evade host immune system: RECURRENT BACTEREMIA & recurring febrile episodes
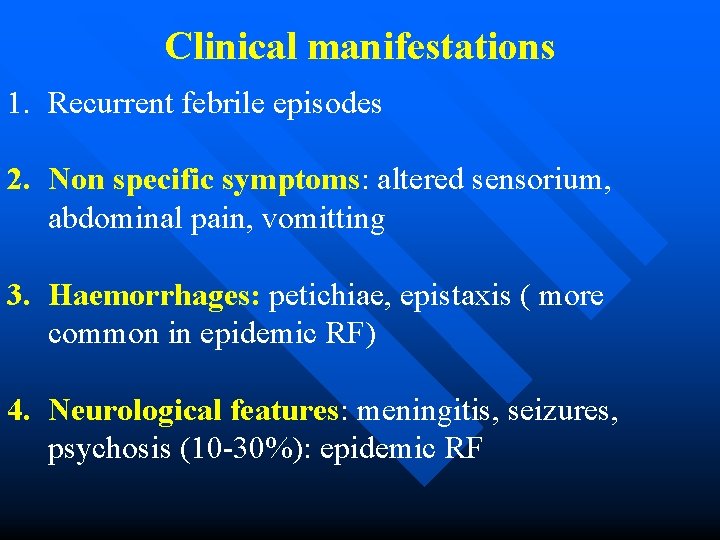
Clinical manifestations 1. Recurrent febrile episodes 2. Non specific symptoms: altered sensorium, abdominal pain, vomitting 3. Haemorrhages: petichiae, epistaxis ( more common in epidemic RF) 4. Neurological features: meningitis, seizures, psychosis (10 -30%): epidemic RF
LAB DIAGNOSIS: 1. Microscopy: » Peripheral blood smears: Giemsa stain » QBC » DFAb test » Dark ground microscopy 2. Culture: isolation from blood 3. Serology: ELISA, IFA to detect serum Abs 4. Glp. Q assay: Glycero-phospho-diesterase assay to detect Ab against Glp. Q ag 5. Molecular methods: PCR for Glp. Q genes
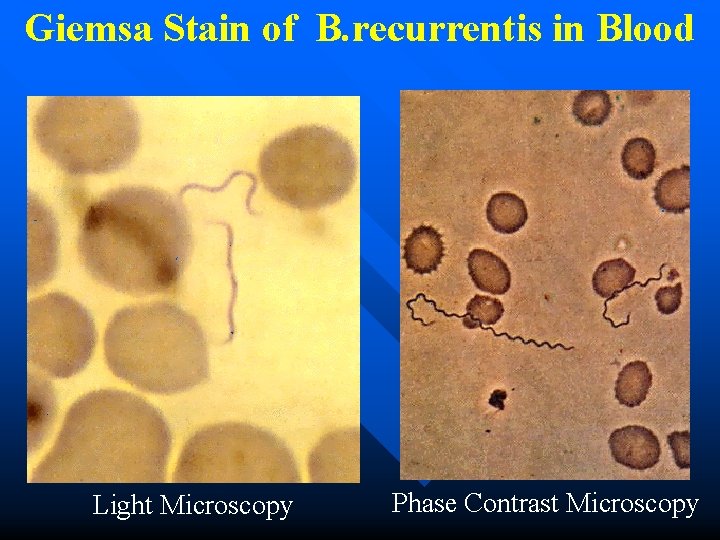
Giemsa Stain of B. recurrentis in Blood Light Microscopy Phase Contrast Microscopy
Treatment: n Doxycycline or erythromycin n
Lyme’s Disease
Introduction n Lyme disease was named in 1977 when arthritis was observed in a cluster of children in and around Lyme, USA n Causative agent: B. burgdorferi & related spps. – B. garinii – B. afzelii
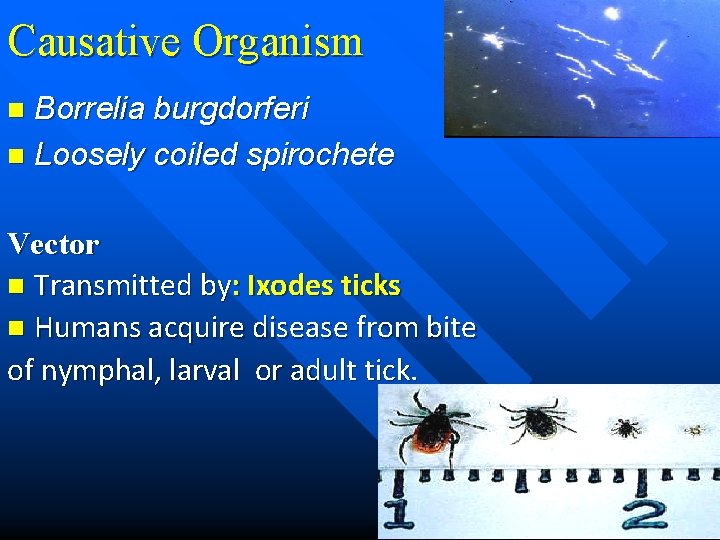
Causative Organism Borrelia burgdorferi n Loosely coiled spirochete n Vector n Transmitted by: Ixodes ticks n Humans acquire disease from bite of nymphal, larval or adult tick.

Clinical manifestations: Three Stages of Disease n Stage 1: Early localised infection: IP: 3 -32 days, maculo-papular rash at site of tick bite: erythema migrans n Stage 2: Early disseminated infection: hematological spread to multiple organs: » 20 skin lesions, arthralgia, malaise, fatigue, » Neurological abnormalities (15%): meningitis, encephelitis, meningoradiculitis (Bannwarth’s syndrome)
n Stage 3: Late persistent infection: (Lyme arthritis): 60% in untreated patients, Large joints (knee) n Post lyme syndrome: chronic fatigue & neurocognitive manifestations Spirochete expresses: Osp. A in midgut of tick n Expresses Osp. C in salivary gland of the tick n

Localized Rash
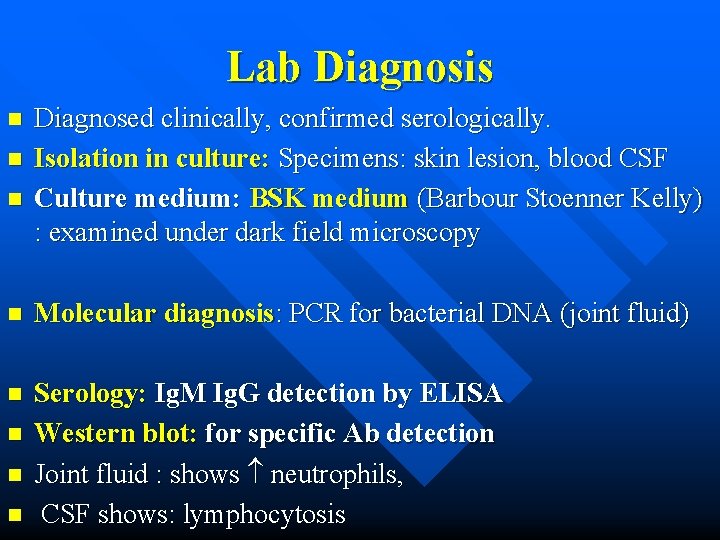
Lab Diagnosis n n n Diagnosed clinically, confirmed serologically. Isolation in culture: Specimens: skin lesion, blood CSF Culture medium: BSK medium (Barbour Stoenner Kelly) : examined under dark field microscopy n Molecular diagnosis: PCR for bacterial DNA (joint fluid) n Serology: Ig. M Ig. G detection by ELISA Western blot: for specific Ab detection Joint fluid : shows neutrophils, CSF shows: lymphocytosis n n n
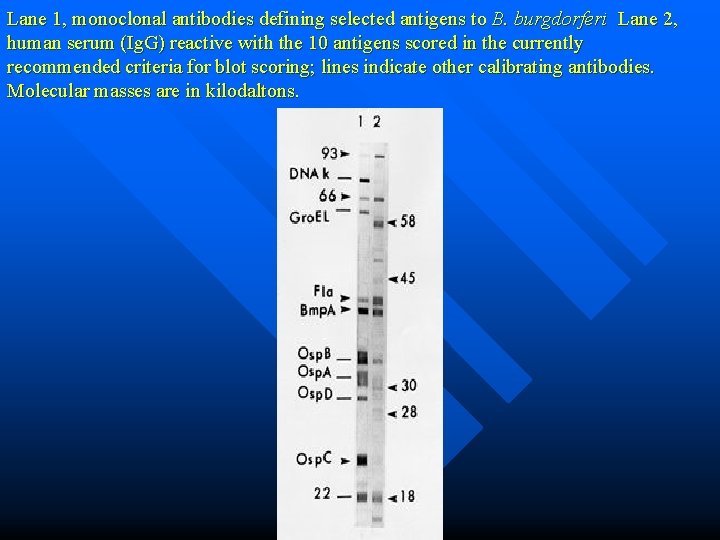
Lane 1, monoclonal antibodies defining selected antigens to B. burgdorferi Lane 2, human serum (Ig. G) reactive with the 10 antigens scored in the currently recommended criteria for blot scoring; lines indicate other calibrating antibodies. Molecular masses are in kilodaltons.
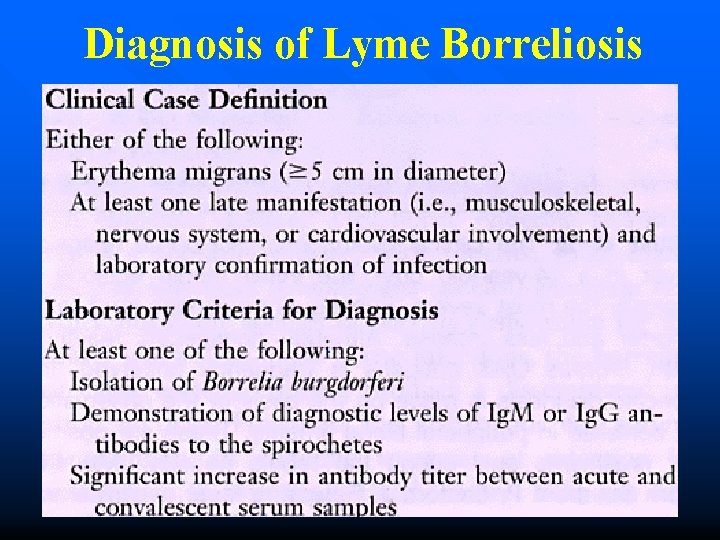
Diagnosis of Lyme Borreliosis
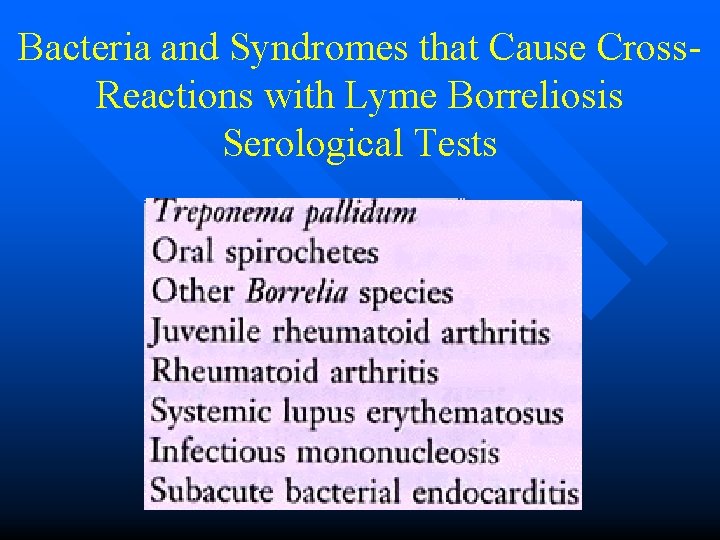
Bacteria and Syndromes that Cause Cross. Reactions with Lyme Borreliosis Serological Tests
Treatment n Oral doxycycline for all forms of the disease except CNS. n In children: amoxicillin n Neuro-borreliosis requires IV antibiotic therapy with ceftriaxone ( 14 -28 days).
Vincent’s angina n Trench mouth: acute ulcerative necrotizing gingivo -stomatitis n Caused by: » Borrelia vincentii & » Leptotrichia buccalis (anaerobic gram negative fuso bacterium) Normal flora: potential pathogens (malnutrition, viral disease)

n Inflamed gums, pharyngeal mucosa
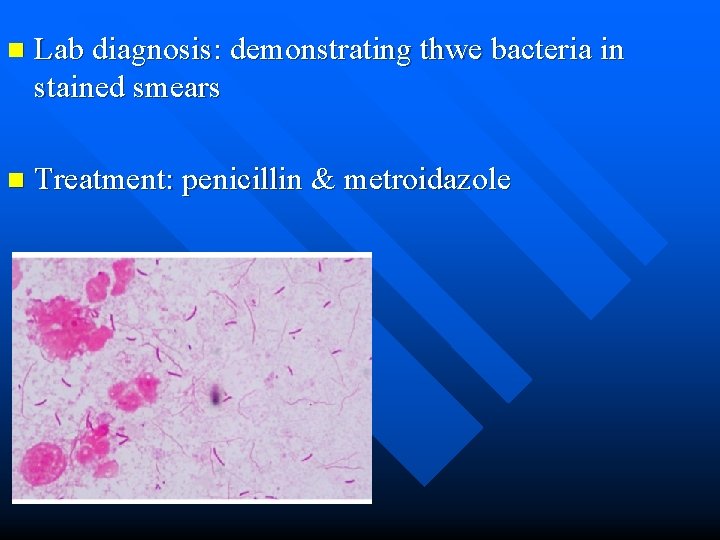
n Lab diagnosis: demonstrating thwe bacteria in stained smears n Treatment: penicillin & metroidazole
- Slides: 25