Bordetella pertussis 1 Bordetella pertussis General characteristics q
Bordetella pertussis 1
Bordetella pertussis General characteristics q Gram-negative coccobacillus or bacillus arranged singly, in pairs or in small groups q They are obligate respiratory tract pathogens, therefore, they are unable to survive outside their hosts q Aerobic and encapsulated. q Reservoir is humans (Specific to Humans) 2
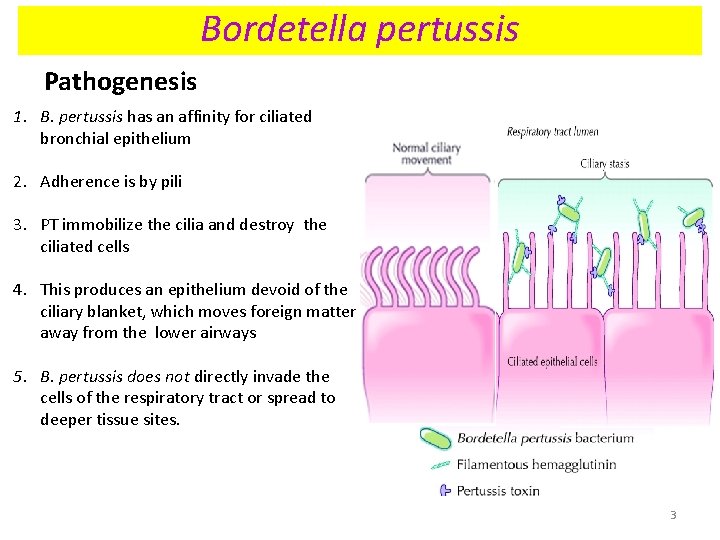
Bordetella pertussis Pathogenesis 1. B. pertussis has an affinity for ciliated bronchial epithelium 2. Adherence is by pili 3. PT immobilize the cilia and destroy the ciliated cells 4. This produces an epithelium devoid of the ciliary blanket, which moves foreign matter away from the lower airways 5. B. pertussis does not directly invade the cells of the respiratory tract or spread to deeper tissue sites. 3
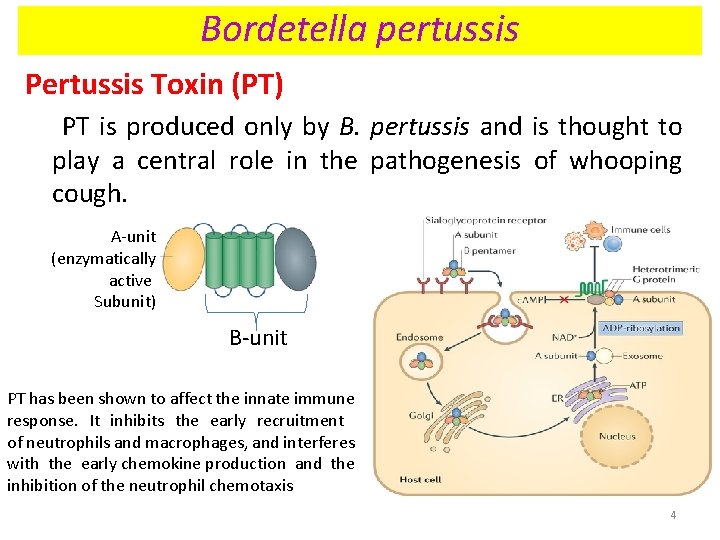
Bordetella pertussis Pertussis Toxin (PT) PT is produced only by B. pertussis and is thought to play a central role in the pathogenesis of whooping cough. A-unit (enzymatically active Subunit) B-unit PT has been shown to affect the innate immune response. It inhibits the early recruitment of neutrophils and macrophages, and interferes with the early chemokine production and the inhibition of the neutrophil chemotaxis 4
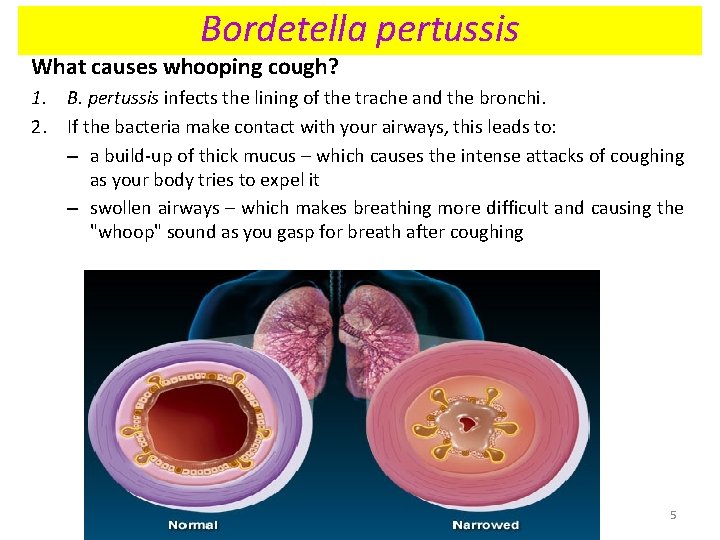
Bordetella pertussis What causes whooping cough? 1. B. pertussis infects the lining of the trache and the bronchi. 2. If the bacteria make contact with your airways, this leads to: – a build-up of thick mucus – which causes the intense attacks of coughing as your body tries to expel it – swollen airways – which makes breathing more difficult and causing the "whoop" sound as you gasp for breath after coughing 5
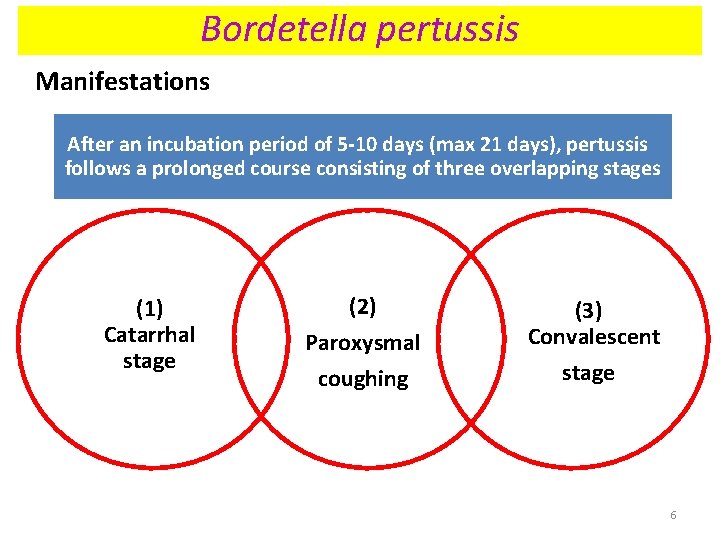
Bordetella pertussis Manifestations After an incubation period of 5 -10 days (max 21 days), pertussis follows a prolonged course consisting of three overlapping stages (1) Catarrhal stage (2) Paroxysmal (3) Convalescent coughing stage 6
Bordetella pertussis Manifestations 1 - Catarrhal stage • Catarrh: inflammation of a mucous membrane, especially of the respiratory tract, accompanied by excessive secretions. • After an incubation period of 5 -10 days (max 21 days), generalised symptoms of an upper respiratory tract infection occur which are collectively called as catarrhal stage and include sneezing, running nose and coughing. • The first stage or prodrome lasts 1 -2 weeks. 7
Bordetella pertussis Manifestations 2. Paroxysmal Stage • From Greek: paroxysmos, irritation; cough • The second stage progresses into episodes of uncontrollable cough. • Each paroxysm consists of 5 -20 rapid coughs with the patient unable to breathe between the coughs. • During a spasm, there may be impressive neck-vein distension, bulging eyes, tongue protrusion, and cyanosis. • Such prolonged coughing may lead to anoxia, expelling of mucus and vomiting. • Weight loss is common as a result of the illness’s interference with eating • This stage may continue for 1 -6 weeks. 8
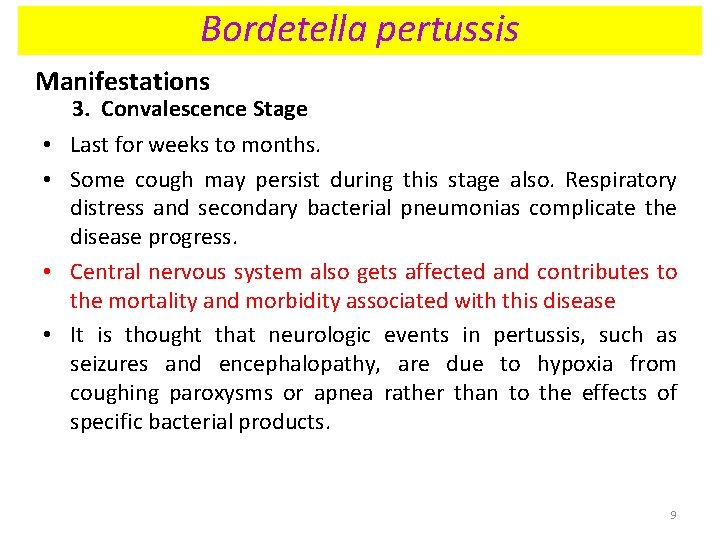
Bordetella pertussis Manifestations 3. Convalescence Stage • Last for weeks to months. • Some cough may persist during this stage also. Respiratory distress and secondary bacterial pneumonias complicate the disease progress. • Central nervous system also gets affected and contributes to the mortality and morbidity associated with this disease • It is thought that neurologic events in pertussis, such as seizures and encephalopathy, are due to hypoxia from coughing paroxysms or apnea rather than to the effects of specific bacterial products. 9
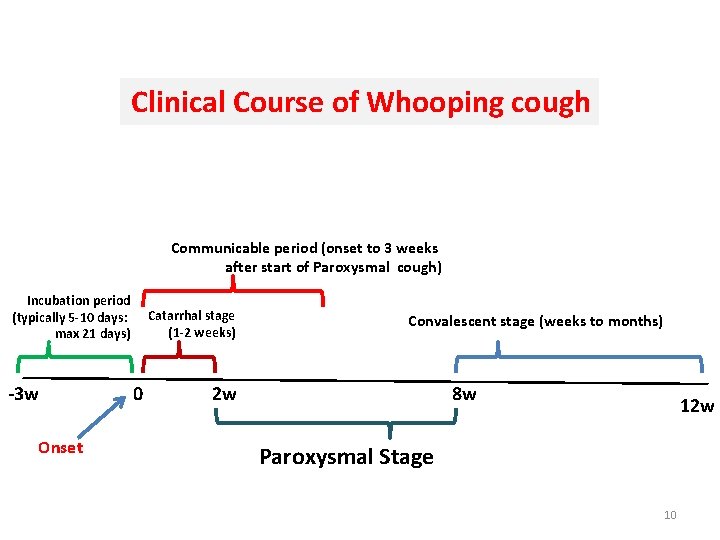
Clinical Course of Whooping cough Communicable period (onset to 3 weeks after start of Paroxysmal cough) Incubation period (typically 5 -10 days: max 21 days) -3 w Onset Catarrhal stage (1 -2 weeks) 0 Convalescent stage (weeks to months) 2 w 8 w 12 w Paroxysmal Stage 10
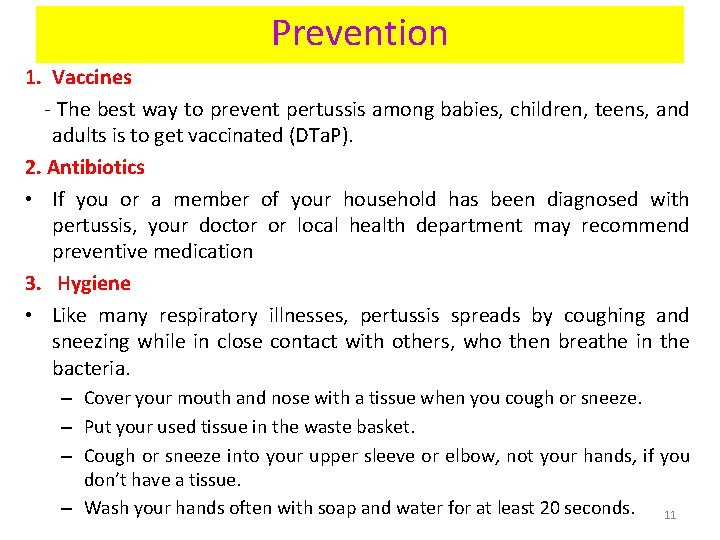
Prevention 1. Vaccines - The best way to prevent pertussis among babies, children, teens, and adults is to get vaccinated (DTa. P). 2. Antibiotics • If you or a member of your household has been diagnosed with pertussis, your doctor or local health department may recommend preventive medication 3. Hygiene • Like many respiratory illnesses, pertussis spreads by coughing and sneezing while in close contact with others, who then breathe in the bacteria. – Cover your mouth and nose with a tissue when you cough or sneeze. – Put your used tissue in the waste basket. – Cough or sneeze into your upper sleeve or elbow, not your hands, if you don’t have a tissue. – Wash your hands often with soap and water for at least 20 seconds. 11
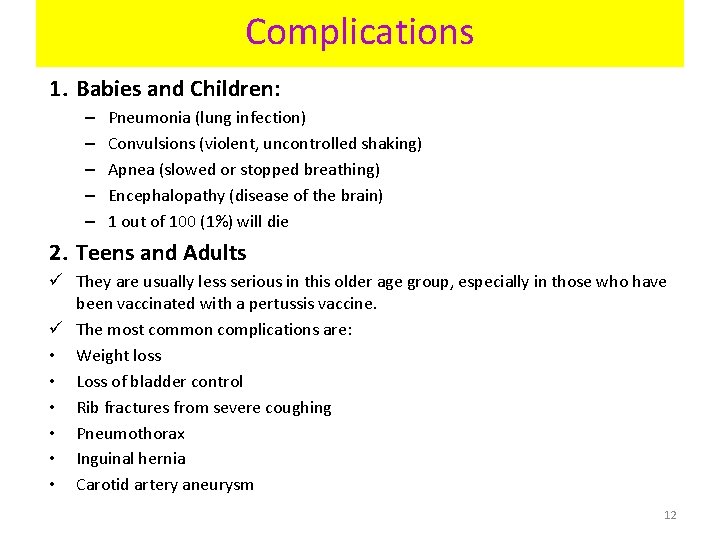
Complications 1. Babies and Children: – – – Pneumonia (lung infection) Convulsions (violent, uncontrolled shaking) Apnea (slowed or stopped breathing) Encephalopathy (disease of the brain) 1 out of 100 (1%) will die 2. Teens and Adults ü They are usually less serious in this older age group, especially in those who have been vaccinated with a pertussis vaccine. ü The most common complications are: • Weight loss • Loss of bladder control • Rib fractures from severe coughing • Pneumothorax • Inguinal hernia • Carotid artery aneurysm 12
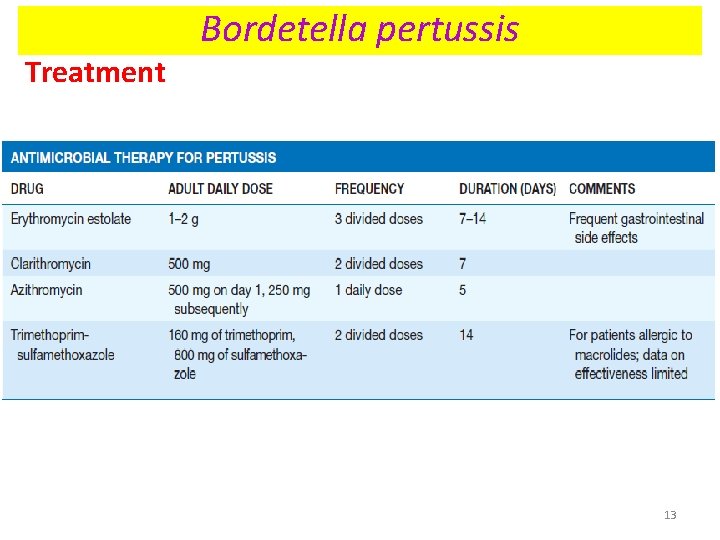
Treatment Bordetella pertussis 13
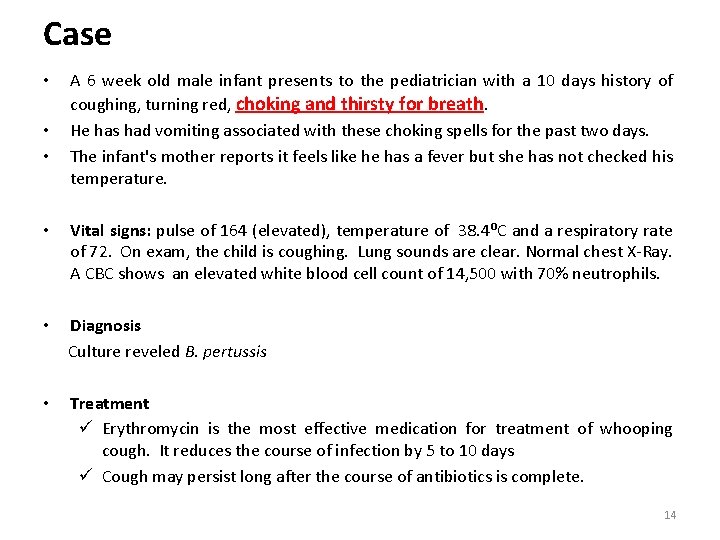
Case • • • A 6 week old male infant presents to the pediatrician with a 10 days history of coughing, turning red, choking and thirsty for breath. He has had vomiting associated with these choking spells for the past two days. The infant's mother reports it feels like he has a fever but she has not checked his temperature. • Vital signs: pulse of 164 (elevated), temperature of 38. 4⁰C and a respiratory rate of 72. On exam, the child is coughing. Lung sounds are clear. Normal chest X-Ray. A CBC shows an elevated white blood cell count of 14, 500 with 70% neutrophils. • Diagnosis Culture reveled B. pertussis • Treatment ü Erythromycin is the most effective medication for treatment of whooping cough. It reduces the course of infection by 5 to 10 days ü Cough may persist long after the course of antibiotics is complete. 14
Pulmonary Mycosis
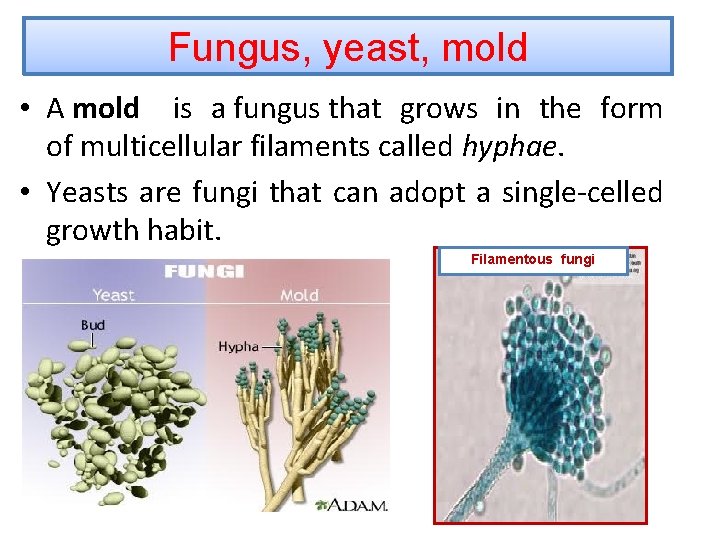
Fungus, yeast, mold • A mold is a fungus that grows in the form of multicellular filaments called hyphae. • Yeasts are fungi that can adopt a single-celled growth habit. Filamentous fungi
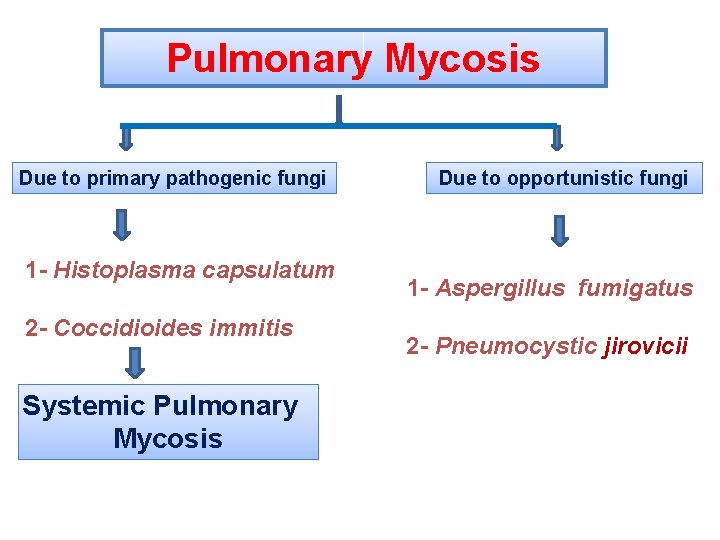
Pulmonary Mycosis Due to primary pathogenic fungi 1 - Histoplasma capsulatum 2 - Coccidioides immitis Systemic Pulmonary Mycosis Due to opportunistic fungi 1 - Aspergillus fumigatus 2 - Pneumocystic jirovicii
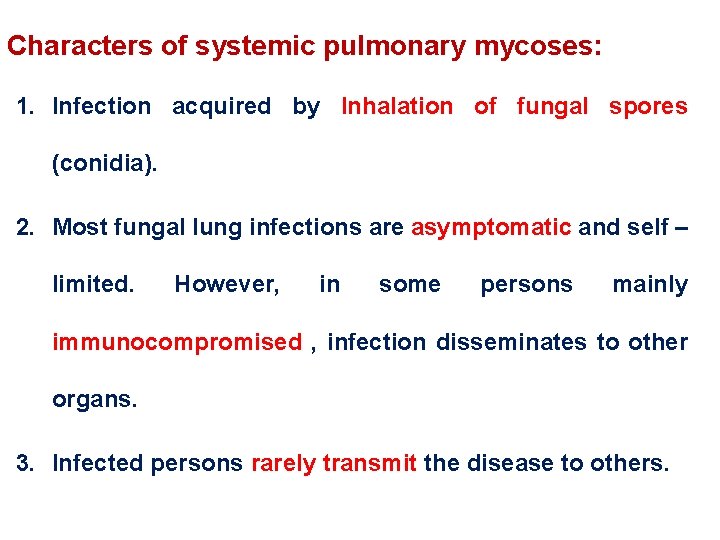
Characters of systemic pulmonary mycoses: 1. Infection acquired by Inhalation of fungal spores (conidia). 2. Most fungal lung infections are asymptomatic and self – limited. However, in some persons mainly immunocompromised , infection disseminates to other organs. 3. Infected persons rarely transmit the disease to others.
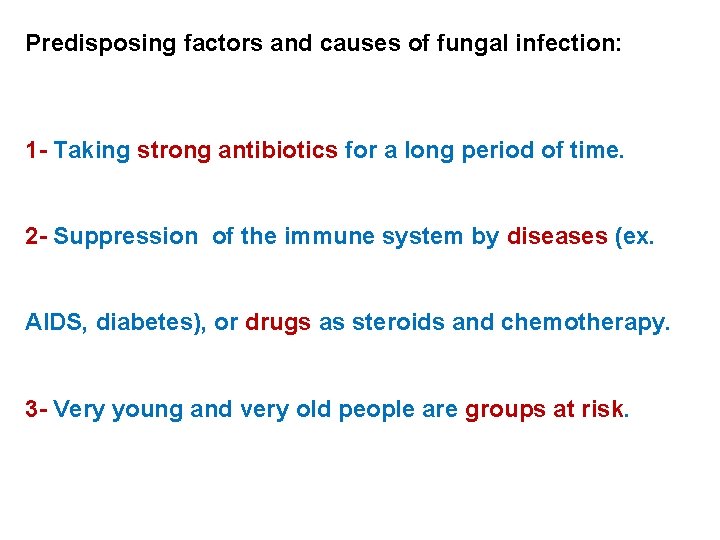
Predisposing factors and causes of fungal infection: 1 - Taking strong antibiotics for a long period of time. 2 - Suppression of the immune system by diseases (ex. AIDS, diabetes), or drugs as steroids and chemotherapy. 3 - Very young and very old people are groups at risk.
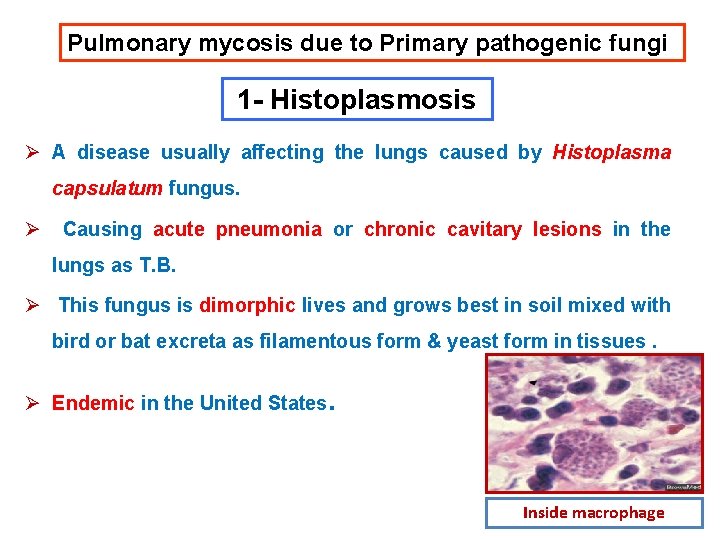
Pulmonary mycosis due to Primary pathogenic fungi 1 - Histoplasmosis Ø A disease usually affecting the lungs caused by Histoplasma capsulatum fungus. Ø Causing acute pneumonia or chronic cavitary lesions in the lungs as T. B. Ø This fungus is dimorphic lives and grows best in soil mixed with bird or bat excreta as filamentous form & yeast form in tissues. Ø Endemic in the United States. Inside macrophage
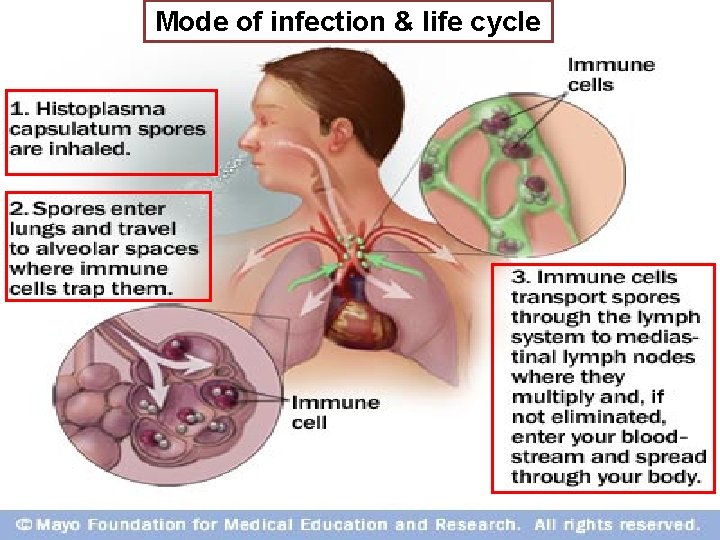
Mode of infection & life cycle
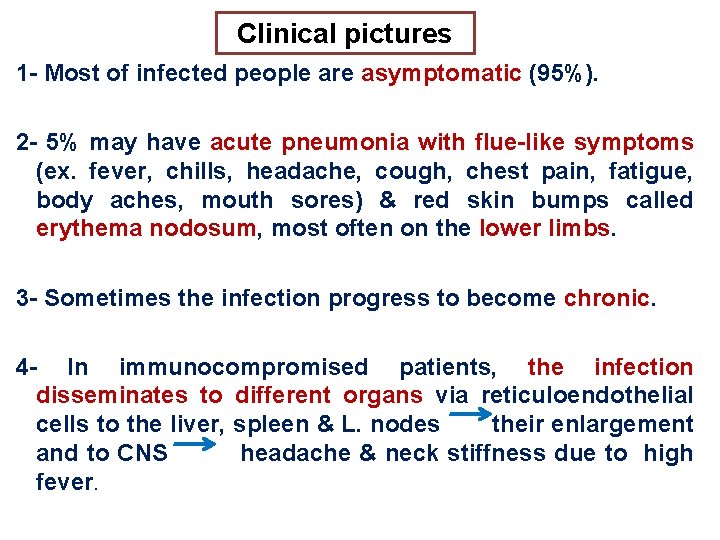
Clinical pictures 1 - Most of infected people are asymptomatic (95%). 2 - 5% may have acute pneumonia with flue-like symptoms (ex. fever, chills, headache, cough, chest pain, fatigue, body aches, mouth sores) & red skin bumps called erythema nodosum, most often on the lower limbs. 3 - Sometimes the infection progress to become chronic. 4 - In immunocompromised patients, the infection disseminates to different organs via reticuloendothelial cells to the liver, spleen & L. nodes their enlargement and to CNS headache & neck stiffness due to high fever.
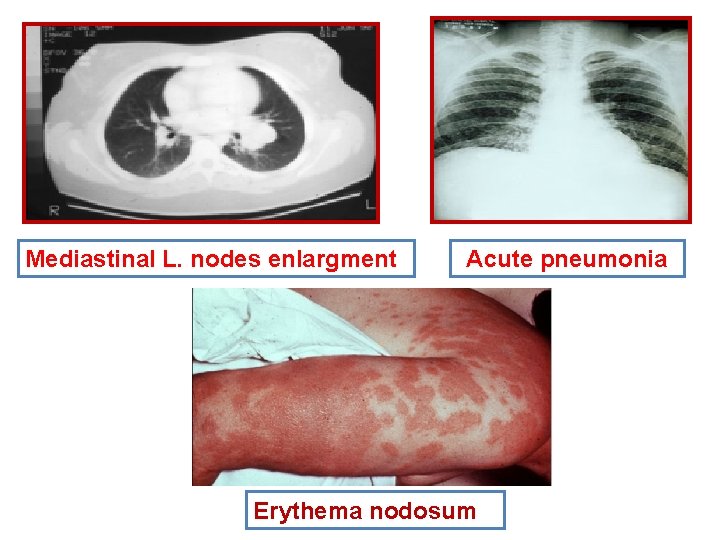
Mediastinal L. nodes enlargment Acute pneumonia Erythema nodosum
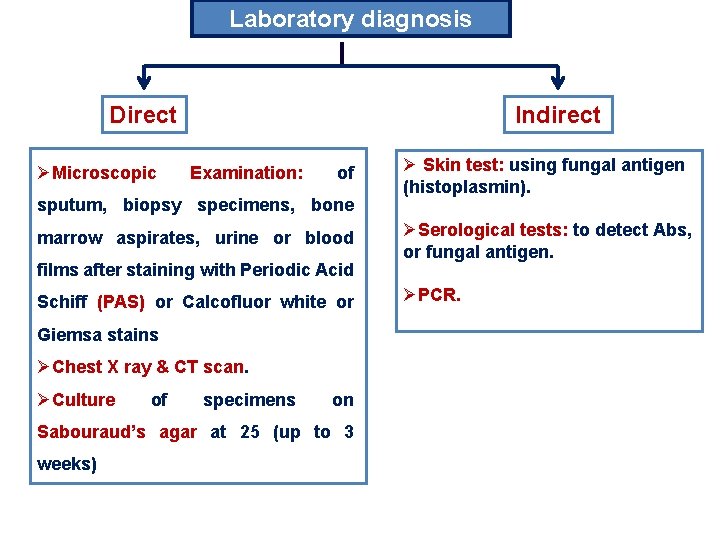
Laboratory diagnosis Direct ØMicroscopic Indirect Examination: of sputum, biopsy specimens, bone marrow aspirates, urine or blood films after staining with Periodic Acid Schiff (PAS) or Calcofluor white or Giemsa stains ØChest X ray & CT scan. ØCulture of specimens on Sabouraud’s agar at 25 (up to 3 weeks) Ø Skin test: using fungal antigen (histoplasmin). ØSerological tests: to detect Abs, or fungal antigen. ØPCR.
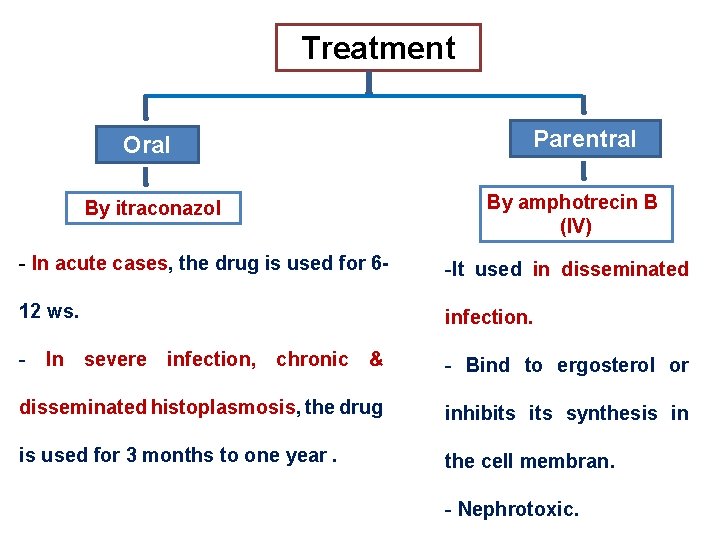
Treatment Oral By itraconazol Parentral By amphotrecin B (IV) - In acute cases, the drug is used for 6 - -It used in disseminated 12 ws. infection. - In severe infection, chronic & - Bind to ergosterol or disseminated histoplasmosis, the drug inhibits synthesis in is used for 3 months to one year. the cell membran. - Nephrotoxic.
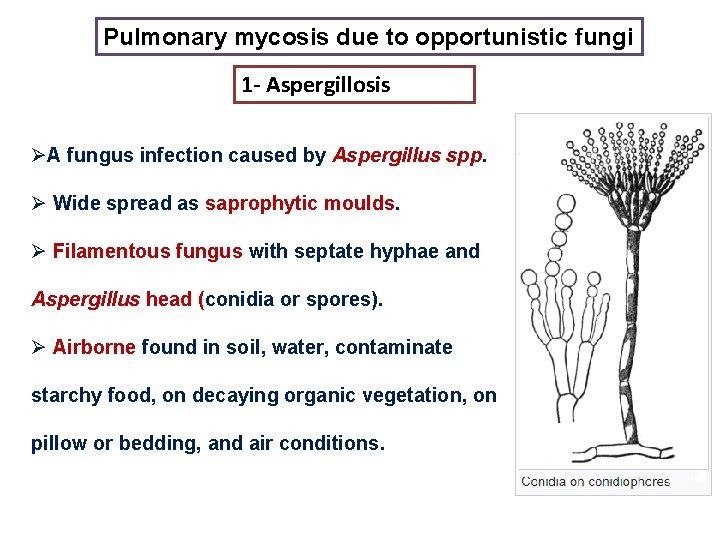
Pulmonary mycosis due to opportunistic fungi 1 - Aspergillosis ØA fungus infection caused by Aspergillus spp. Ø Wide spread as saprophytic moulds. Ø Filamentous fungus with septate hyphae and Aspergillus head (conidia or spores). Ø Airborne found in soil, water, contaminate starchy food, on decaying organic vegetation, on pillow or bedding, and air conditions.
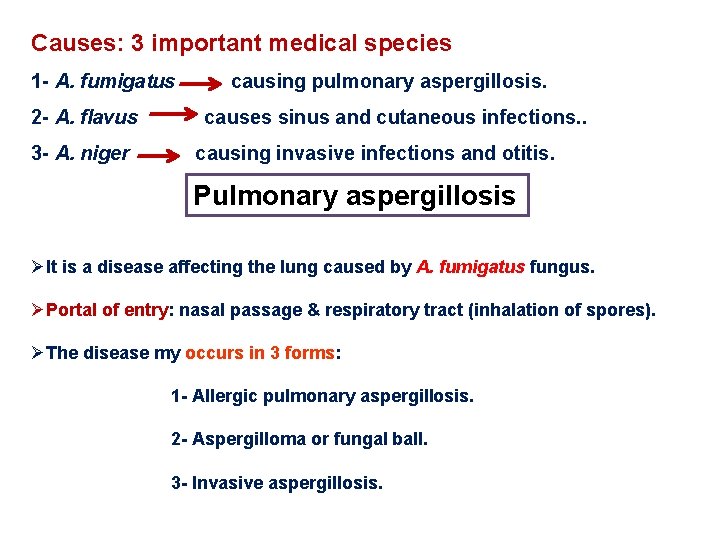
Causes: 3 important medical species 1 - A. fumigatus 2 - A. flavus 3 - A. niger causing pulmonary aspergillosis. causes sinus and cutaneous infections. . causing invasive infections and otitis. Pulmonary aspergillosis ØIt is a disease affecting the lung caused by A. fumigatus fungus. ØPortal of entry: nasal passage & respiratory tract (inhalation of spores). ØThe disease my occurs in 3 forms: 1 - Allergic pulmonary aspergillosis. 2 - Aspergilloma or fungal ball. 3 - Invasive aspergillosis.
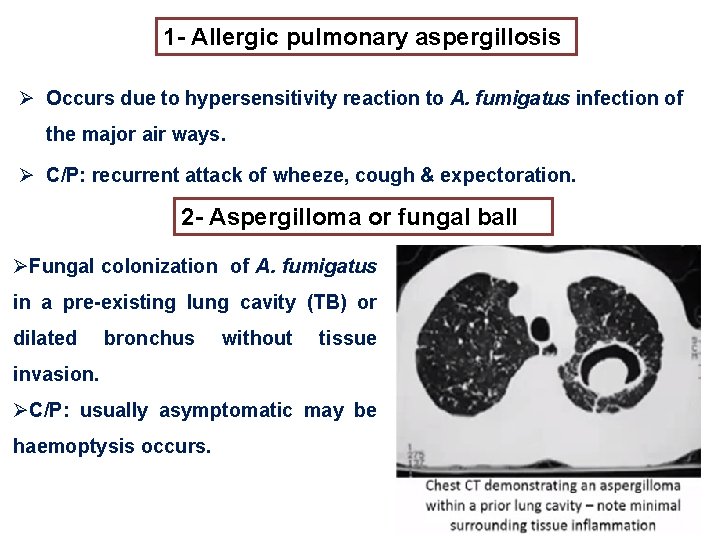
1 - Allergic pulmonary aspergillosis Ø Occurs due to hypersensitivity reaction to A. fumigatus infection of the major air ways. Ø C/P: recurrent attack of wheeze, cough & expectoration. 2 - Aspergilloma or fungal ball ØFungal colonization of A. fumigatus in a pre-existing lung cavity (TB) or dilated bronchus without tissue invasion. ØC/P: usually asymptomatic may be haemoptysis occurs.
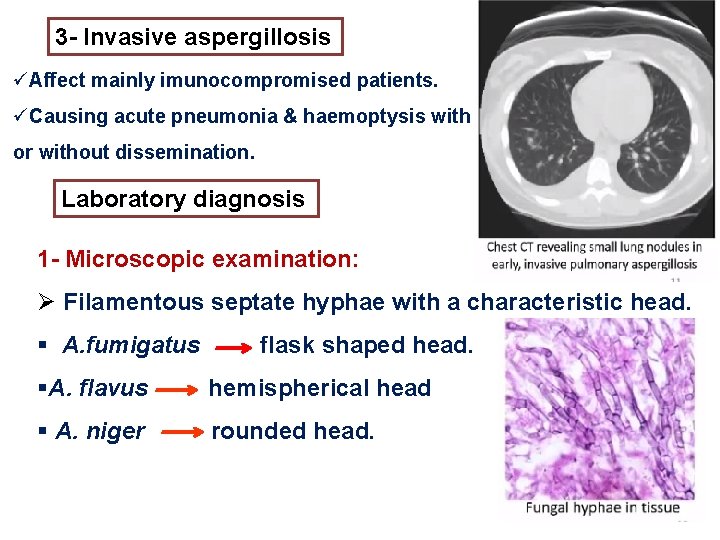
3 - Invasive aspergillosis üAffect mainly imunocompromised patients. üCausing acute pneumonia & haemoptysis with or without dissemination. Laboratory diagnosis 1 - Microscopic examination: Ø Filamentous septate hyphae with a characteristic head. § A. fumigatus flask shaped head. §A. flavus hemispherical head § A. niger rounded head.
2 - culture: § On sabouraud’s agar. § Aspergillus spp. can be identify by the pigmentation of their growth in the culture as follows: Ø A. fumigatus ØA. flavus Ø A. niger gives white filaments with green spores. gives white filaments with yellowish green spores. gives white filaments with blak spores. Treatment 1 - Antifungal drugs in invasive pulmonary aspergillosis and dissiminated disease: Ø Amphotricine B (IV) & oral itraconazole. 2 - Surgical removal of fungal ball in lung.
- Slides: 30