Borderline Resectable Pancreatic Cancer Fung Man Him Matrix

Borderline Resectable Pancreatic Cancer Fung Man Him Matrix QMH Joint Hospital Surgical Grand Round
Content 1. Epidemiology 2. Definitions 3. Evaluation 4. Surgical Considerations 5. Neoadjuvant chemotherapy
Cancer of the Pancreas • Rank 6 th in cancer mortality in Hong Kong • Rank 4 th in the US • Overall 5 year survival: 5% • 80% Unresectable • 50 -55% metastatic • 20 -25% locally advanced • 20% resectable at presentation • Post resection and adjuvant treatment 5 year survival: 20% Stathis A et al. Nat Rev Clin Oncol. 2010
Unresectable • Metastatic • Locally Advanced • R 2 resection: no improvement in survival • R 1 resection: reduced survival J Gastrointest Surg. 2000 • Median survival < 1 year Loehrer et al. J Clin Oncol 2011
Borderline resectable • Surgery is the only cure for CA pancreas • R 0 resection is crucial to long term survival • Historically, vascular involvement renders resection with negative margin problematic and increases morbidities • Increasing evidence to show vascular resection in selected cases does not compromise margin and hence the term “Borderline resectable pancreatic cancer”

Borderline resectable pancreatic cancer • Involvement by tumor that exceeds one-half circumference of the vessel is highly specific for unresectable tumor Lu et al. AJR Am J Roentgenol. 1997 • Abutment: • Contact ≤ 180 degrees of circumference of blood vessel • Encasement: • Contact >180 degree of circumference of blood vessel
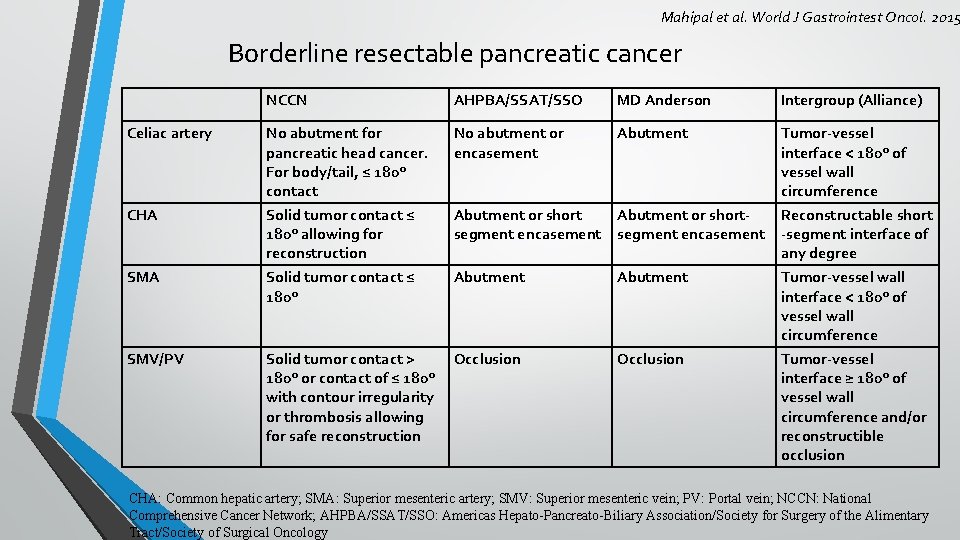
Mahipal et al. World J Gastrointest Oncol. 2015 Borderline resectable pancreatic cancer NCCN AHPBA/SSAT/SSO MD Anderson Intergroup (Alliance) Celiac artery No abutment for pancreatic head cancer. For body/tail, ≤ 180° contact No abutment or encasement Abutment Tumor-vessel interface < 180° of vessel wall circumference CHA Solid tumor contact ≤ 180° allowing for reconstruction Abutment or short. Reconstructable short segment encasement -segment interface of any degree SMA Solid tumor contact ≤ 180° Abutment Tumor-vessel wall interface < 180° of vessel wall circumference SMV/PV Solid tumor contact > 180° or contact of ≤ 180° with contour irregularity or thrombosis allowing for safe reconstruction Occlusion Tumor-vessel interface ≥ 180° of vessel wall circumference and/or reconstructible occlusion CHA: Common hepatic artery; SMA: Superior mesenteric artery; SMV: Superior mesenteric vein; PV: Portal vein; NCCN: National Comprehensive Cancer Network; AHPBA/SSAT/SSO: Americas Hepato-Pancreato-Biliary Association/Society for Surgery of the Alimentary Tract/Society of Surgical Oncology
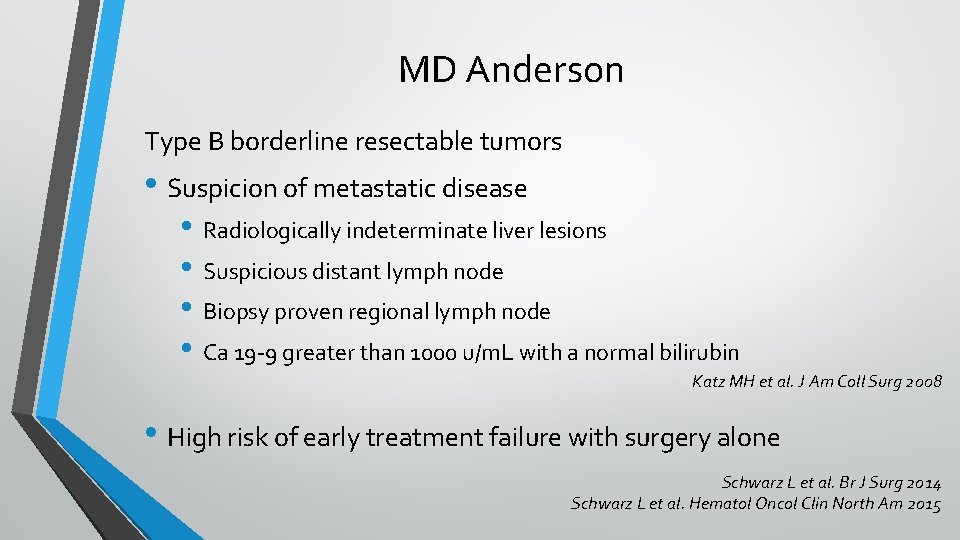
MD Anderson Type B borderline resectable tumors • Suspicion of metastatic disease • Radiologically indeterminate liver lesions • Suspicious distant lymph node • Biopsy proven regional lymph node • Ca 19 -9 greater than 1000 u/m. L with a normal bilirubin Katz MH et al. J Am Coll Surg 2008 • High risk of early treatment failure with surgery alone Schwarz L et al. Br J Surg 2014 Schwarz L et al. Hematol Oncol Clin North Am 2015
MD Anderson Type C borderline resectable tumors • marginal performance status • severe pre-existing comorbidity profile (including advanced age) that put patient at high risk for a major surgical procedure
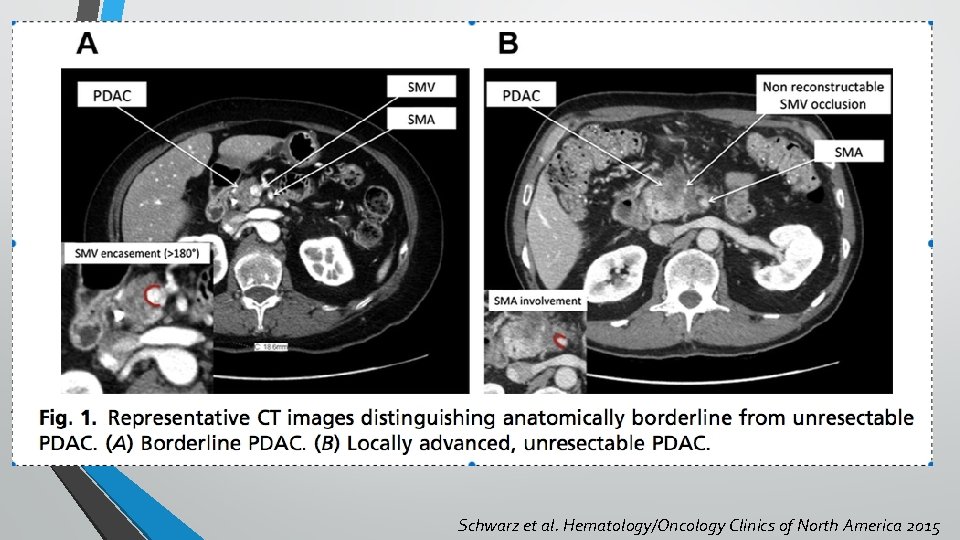
Schwarz et al. Hematology/Oncology Clinics of North America 2015
• CT scan Evaluation • Good spatial resolution, most widely used, recommended • Less sensitive for small hepatic and peritoneal metastases Wong et al. Clin Gastroenterol Hepatol. 2008 • MRI • More sensitive for subcentimeter liver and peritoneal metastases • PET CT • Helps to detect metastases • More sensitive than CT scan for distant disease • Need more data to support routine use Farma et al. Ann Surg Oncol. 2008
Evaluation • EUS • • • Able to detect focal lesions as small as 2 -3 mm in size sensitivities and accuracy approaching 100% and specificity >95% even for lesions <2 cm Complementary to CT scan for vascular staging • • Glazer et al. Pancreatology 2017 62 patients with BRPC (NCCN) 97% R 0 resection 34 patients required venous resection 88% identified by EUS; 67% identified by CT EUS detected 11 (29%) patients that are not detected by CT CT detected 4 patients that are not detected by EUS Operator dependent
Evaluation • CA 19 -9 • preoperative CA 19 -9 correlate with pancreatic cancer staging Karachristos A et al. J Gastrointest Surg. 2005 • post-resection CA 19 -9 levels prior to initiation of adjuvant chemotherapy have independent prognostic value, can be followed to indicate response to therapy Hess V Lancet Oncol. 2008 • Should be checked • • • Before surgery After surgery before adjuvant During surveillance
Surgical considerations • Mesenterico-portal venous resection • Arterial resection
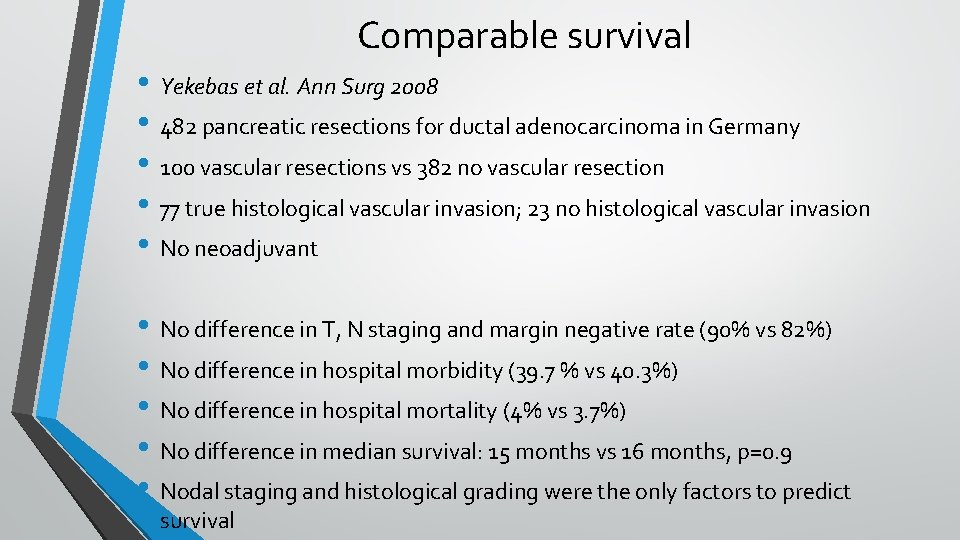
Comparable survival • Yekebas et al. Ann Surg 2008 • 482 pancreatic resections for ductal adenocarcinoma in Germany • 100 vascular resections vs 382 no vascular resection • 77 true histological vascular invasion; 23 no histological vascular invasion • No neoadjuvant • No difference in T, N staging and margin negative rate (90% vs 82%) • No difference in hospital morbidity (39. 7 % vs 40. 3%) • No difference in hospital mortality (4% vs 3. 7%) • No difference in median survival: 15 months vs 16 months, p=0. 9 • Nodal staging and histological grading were the only factors to predict survival
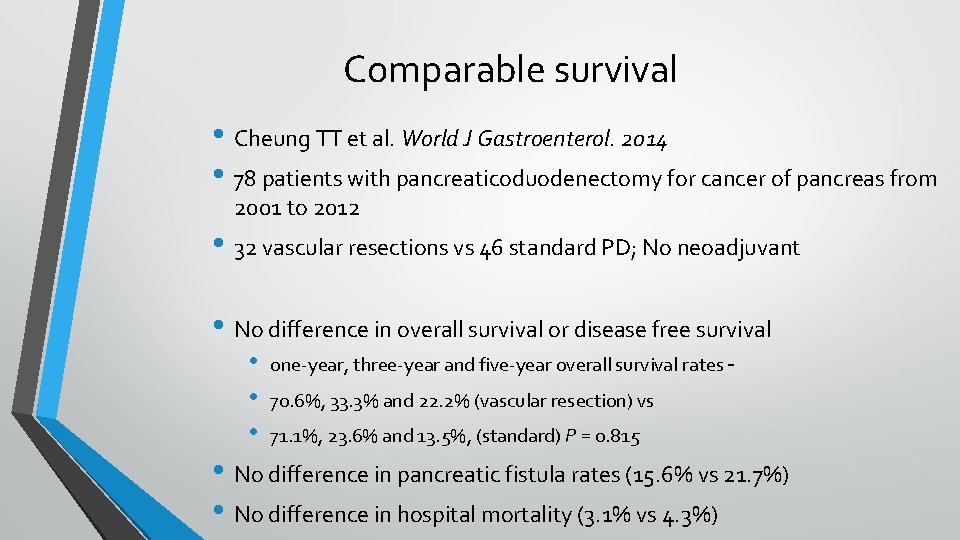
Comparable survival • Cheung TT et al. World J Gastroenterol. 2014 • 78 patients with pancreaticoduodenectomy for cancer of pancreas from 2001 to 2012 • 32 vascular resections vs 46 standard PD; No neoadjuvant • No difference in overall survival or disease free survival • • • one-year, three-year and five-year overall survival rates – 70. 6%, 33. 3% and 22. 2% (vascular resection) vs 71. 1%, 23. 6% and 13. 5%, (standard) P = 0. 815 • No difference in pancreatic fistula rates (15. 6% vs 21. 7%) • No difference in hospital mortality (3. 1% vs 4. 3%)
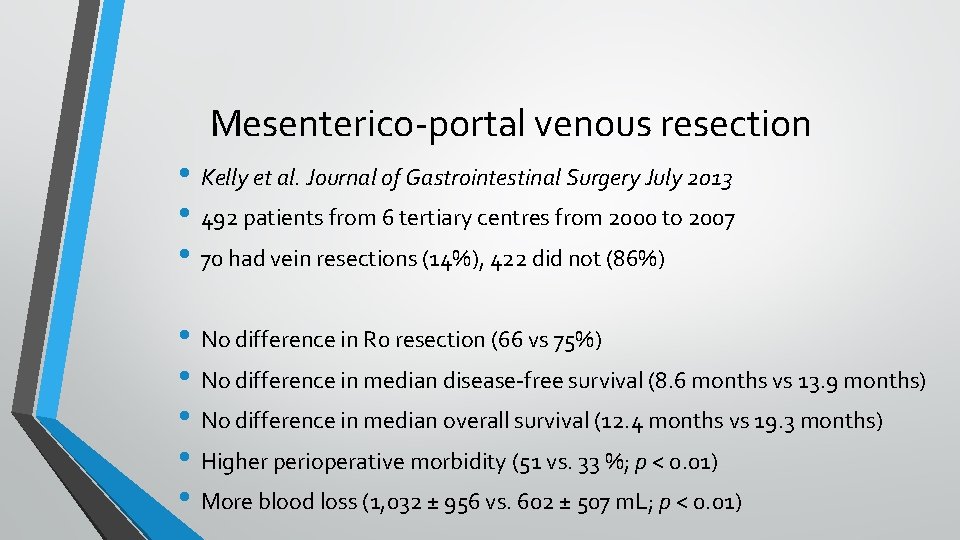
Mesenterico-portal venous resection • Kelly et al. Journal of Gastrointestinal Surgery July 2013 • 492 patients from 6 tertiary centres from 2000 to 2007 • 70 had vein resections (14%), 422 did not (86%) • No difference in R 0 resection (66 vs 75%) • No difference in median disease-free survival (8. 6 months vs 13. 9 months) • No difference in median overall survival (12. 4 months vs 19. 3 months) • Higher perioperative morbidity (51 vs. 33 %; p < 0. 01) • More blood loss (1, 032 ± 956 vs. 602 ± 507 m. L; p < 0. 01)
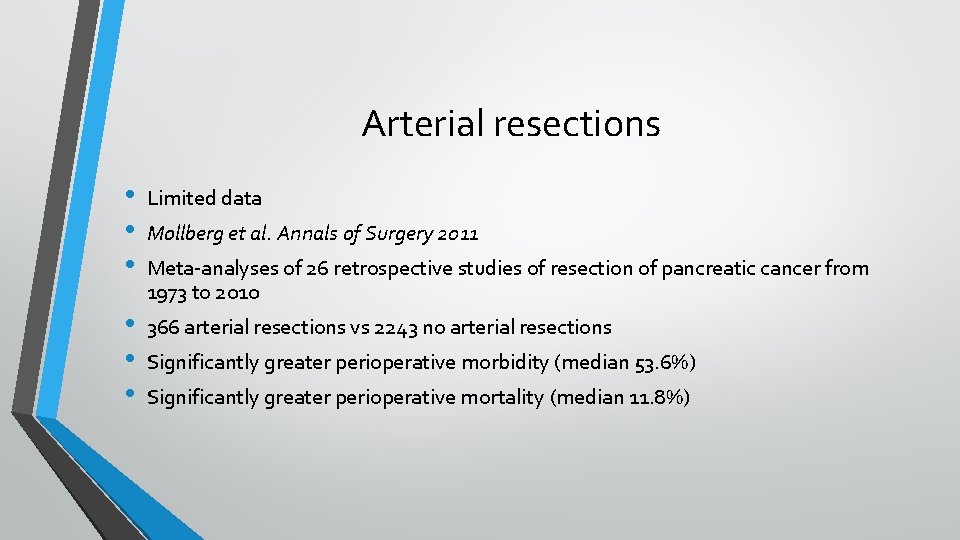
Arterial resections • • • Limited data • • • 366 arterial resections vs 2243 no arterial resections Mollberg et al. Annals of Surgery 2011 Meta-analyses of 26 retrospective studies of resection of pancreatic cancer from 1973 to 2010 Significantly greater perioperative morbidity (median 53. 6%) Significantly greater perioperative mortality (median 11. 8%)
Morbidity and mortality • Worni et al JAMA Surg. 2013 • 10206 patients with pancreatic resection for malignant disease from 2000 to 2009 in the US • 412 patients (4%) with VR, increasing from 0. 7%(2000) to 6% (2009) • VR is associated with higher risk for intraoperative (8. 7% vs 5. 8%, p=0. 001) and postoperative (49% vs 43. 4%, p=0. 008) complications • Also higher mortality (6% vs 1. 9%, p<0. 001) • Bleeding / vascular complications / liver ischemia / venous congestion
Guideline and Consensus • Clear evidence supporting straightforward operative exploration and resection of mesenterico-portal axis • No good evidence that arterial resections during right-sided pancreatic resections are of benefit. Such resections may be harmful with increased morbidity and mortality and should not be recommended on a routine basis International Study Group of Pancreatic Surgery (ISGPS) Surgery, 2014
Neoadjuvant chemo-radiotherapy Theoretical benefits • Early treatment of micrometastases • Select patients with more favourable tumour biology for surgery • Achieve downstaging and/or increase the likelihood of R 0 resection • Ensures the use of chemotherapy Evans DB et al. Ann Surg oncol 2010 Katz MH et al. Arch Surg 2012 • FOLFIRINOX / m. FOLFIRNOX / Gemcitabine / combinations • Emerging evidence • Debatable especially for isolated, resectable venous involvement ISGPS. Surgery 2014
Summary • Definitions of borderline resectable cancer of pancreas • Venous resection should be considered if R 0 resection and reconstruction is possible in selected patients, noting possibly higher morbidity • Complementary role of EUS in the evaluation of vascular involvement to CT • Evidence on neoadjuvant chemo/chemo-irradiation emerging
- Slides: 22