BONY PELVIS OUTLINE l INTRODUCTION l PELVIC GIRDLE
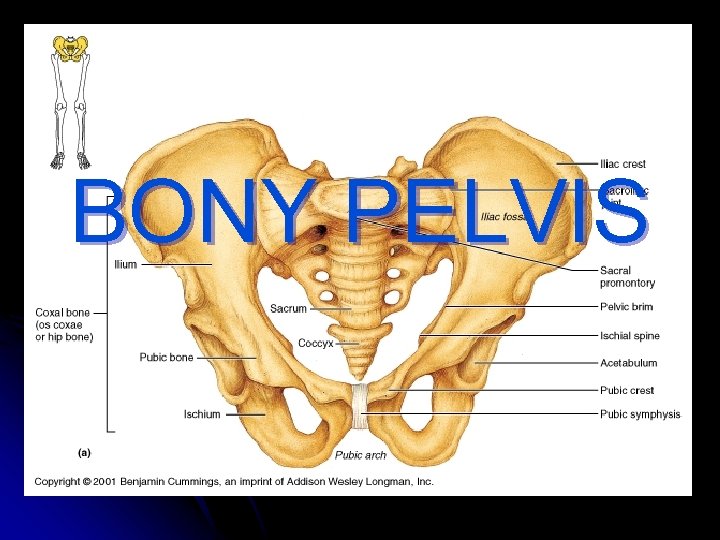
BONY PELVIS
OUTLINE l INTRODUCTION l PELVIC GIRDLE l BONES OF PELVIC GIRGLE l DIVISION OF THE PELVIS l JOINTS AND LIGAMENTS OF PELVIC GIRDLE l PELVIC CAVITY l WALLS AND FLOOR OF THE PELVIC CAVITY
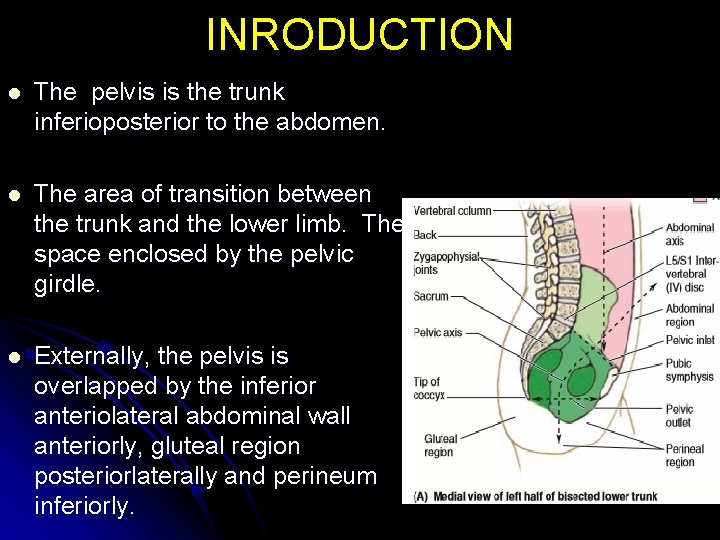
INRODUCTION l The pelvis is the trunk inferioposterior to the abdomen. l The area of transition between the trunk and the lower limb. The space enclosed by the pelvic girdle. l Externally, the pelvis is overlapped by the inferior anteriolateral abdominal wall anteriorly, gluteal region posteriorlaterally and perineum inferiorly.
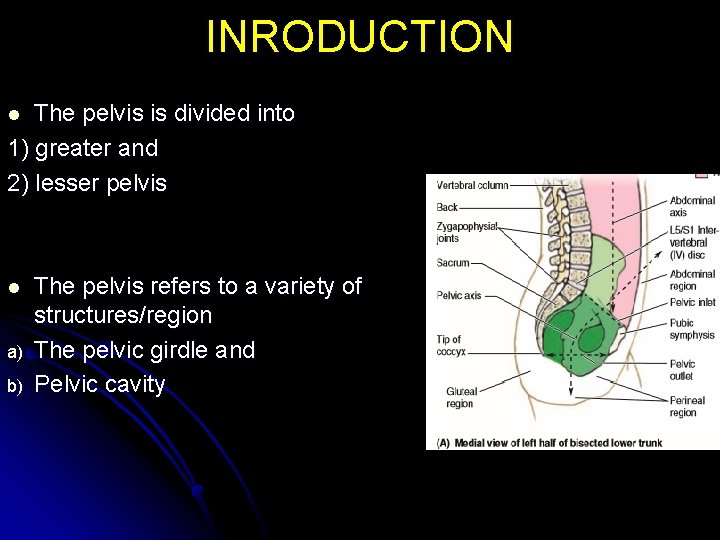
INRODUCTION The pelvis is divided into 1) greater and 2) lesser pelvis l l a) b) The pelvis refers to a variety of structures/region The pelvic girdle and Pelvic cavity
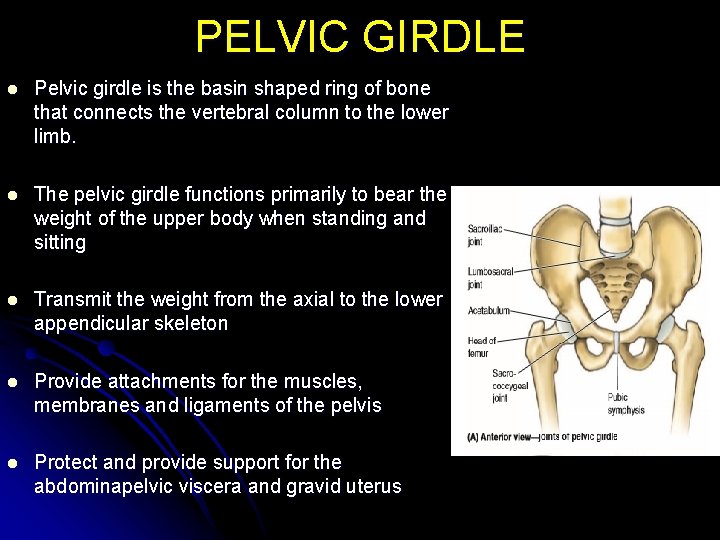
PELVIC GIRDLE l Pelvic girdle is the basin shaped ring of bone that connects the vertebral column to the lower limb. l The pelvic girdle functions primarily to bear the weight of the upper body when standing and sitting l Transmit the weight from the axial to the lower appendicular skeleton l Provide attachments for the muscles, membranes and ligaments of the pelvis l Protect and provide support for the abdominapelvic viscera and gravid uterus
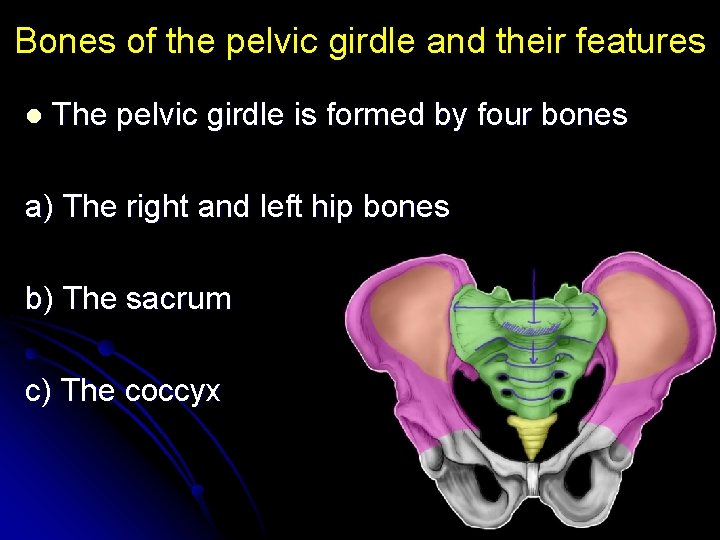
Bones of the pelvic girdle and their features l The pelvic girdle is formed by four bones a) The right and left hip bones b) The sacrum c) The coccyx
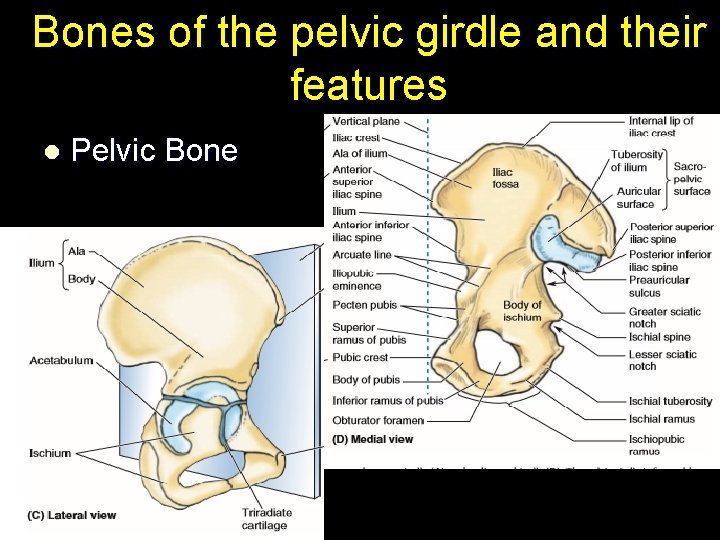
Bones of the pelvic girdle and their features l Pelvic Bone
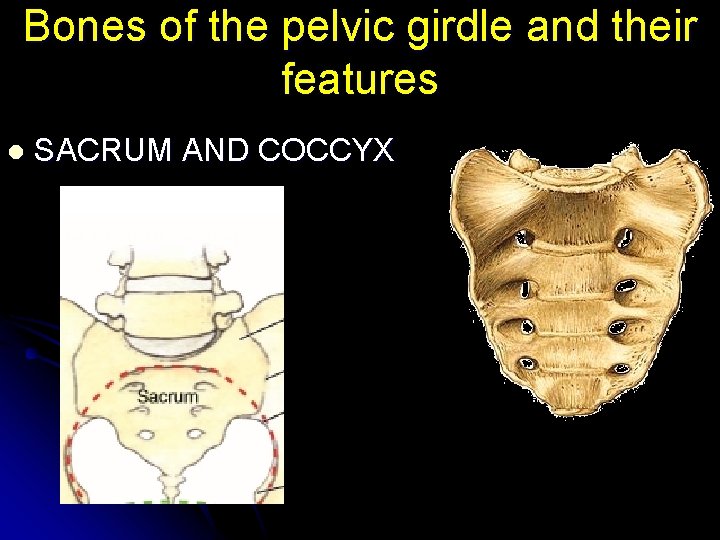
Bones of the pelvic girdle and their features l SACRUM AND COCCYX
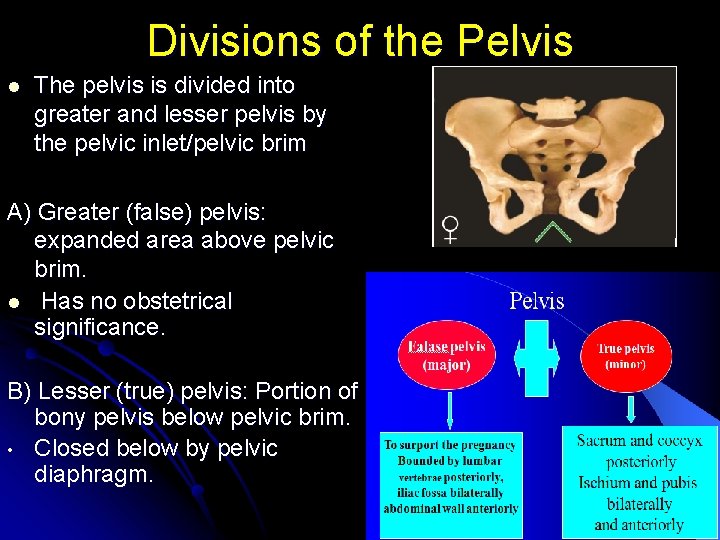
Divisions of the Pelvis l The pelvis is divided into greater and lesser pelvis by the pelvic inlet/pelvic brim A) Greater (false) pelvis: expanded area above pelvic brim. l Has no obstetrical significance. B) Lesser (true) pelvis: Portion of bony pelvis below pelvic brim. • Closed below by pelvic diaphragm.
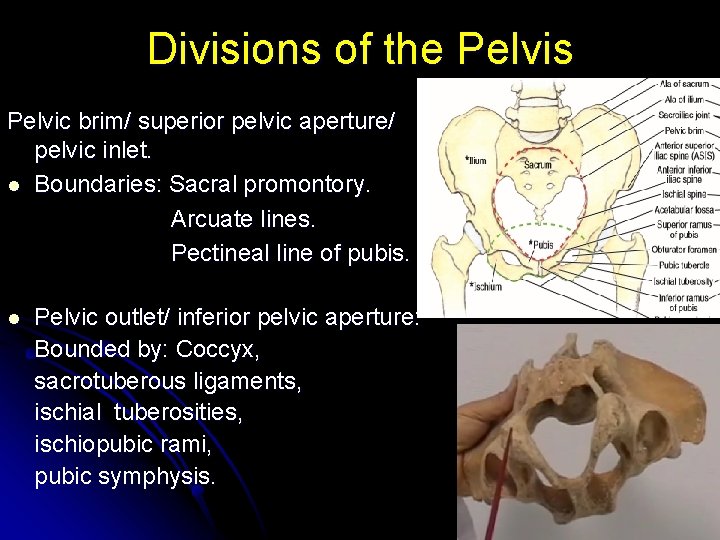
Divisions of the Pelvis Pelvic brim/ superior pelvic aperture/ pelvic inlet. l Boundaries: Sacral promontory. Arcuate lines. Pectineal line of pubis. l Pelvic outlet/ inferior pelvic aperture: Bounded by: Coccyx, sacrotuberous ligaments, ischial tuberosities, ischiopubic rami, pubic symphysis.
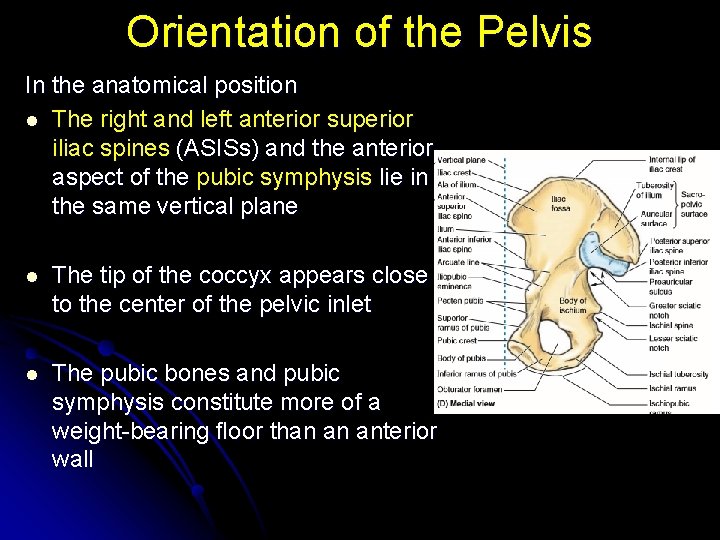
Orientation of the Pelvis In the anatomical position l The right and left anterior superior iliac spines (ASISs) and the anterior aspect of the pubic symphysis lie in the same vertical plane l The tip of the coccyx appears close to the center of the pelvic inlet l The pubic bones and pubic symphysis constitute more of a weight-bearing floor than an anterior wall
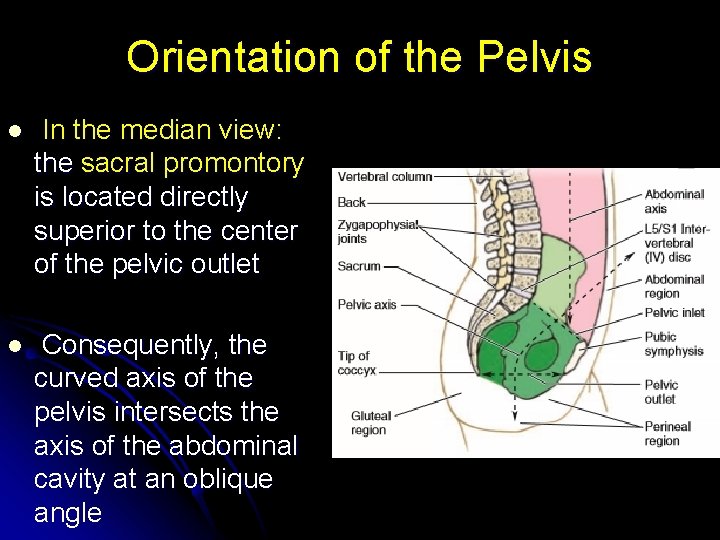
Orientation of the Pelvis l In the median view: the sacral promontory is located directly superior to the center of the pelvic outlet l Consequently, the curved axis of the pelvis intersects the axis of the abdominal cavity at an oblique angle
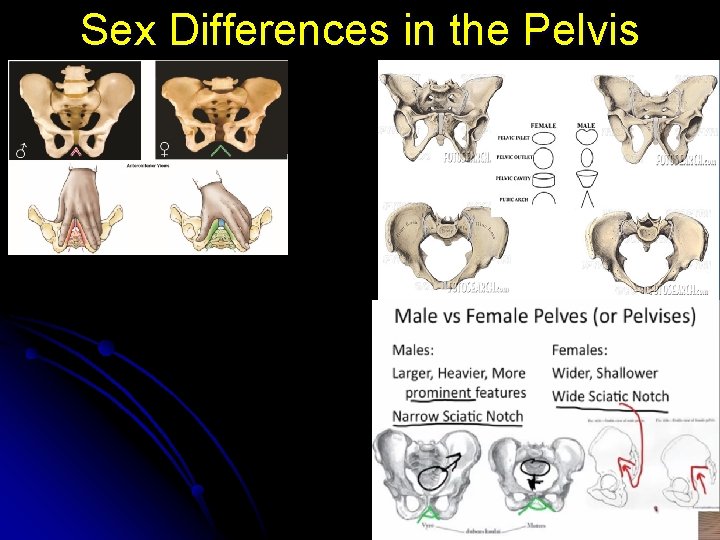
Sex Differences in the Pelvis
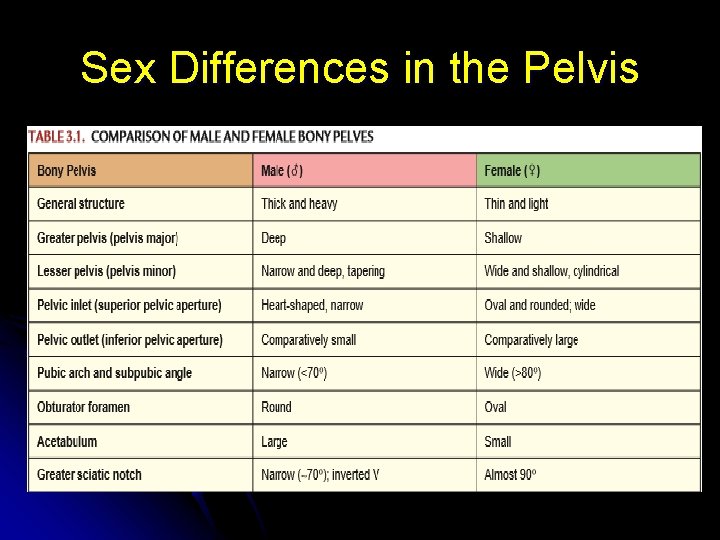
Sex Differences in the Pelvis
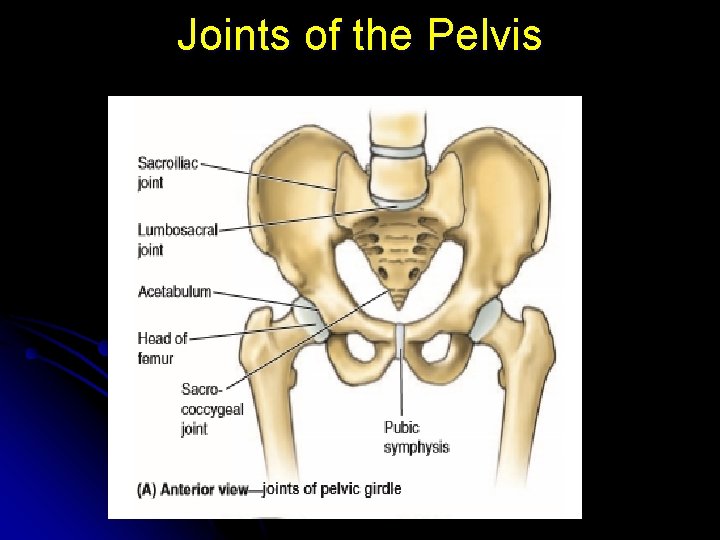
Joints of the Pelvis
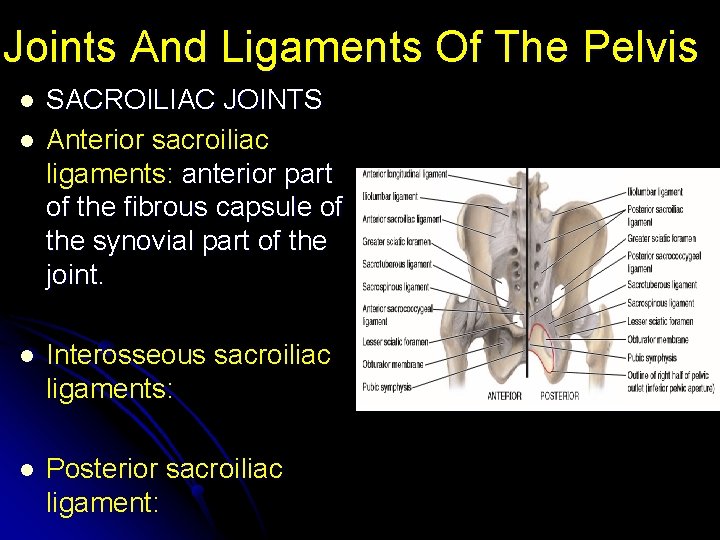
Joints And Ligaments Of The Pelvis l l SACROILIAC JOINTS Anterior sacroiliac ligaments: anterior part of the fibrous capsule of the synovial part of the joint. l Interosseous sacroiliac ligaments: l Posterior sacroiliac ligament:
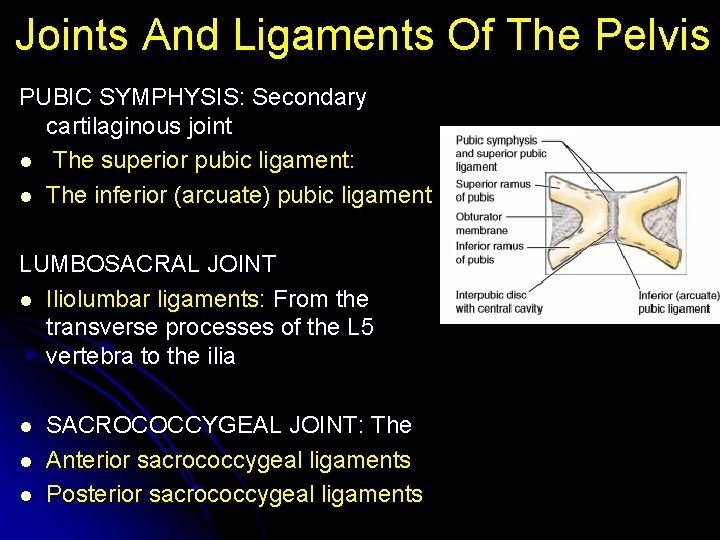
Joints And Ligaments Of The Pelvis PUBIC SYMPHYSIS: Secondary cartilaginous joint l The superior pubic ligament: l The inferior (arcuate) pubic ligament LUMBOSACRAL JOINT l Iliolumbar ligaments: From the transverse processes of the L 5 vertebra to the ilia l l l SACROCOCCYGEAL JOINT: The Anterior sacrococcygeal ligaments Posterior sacrococcygeal ligaments
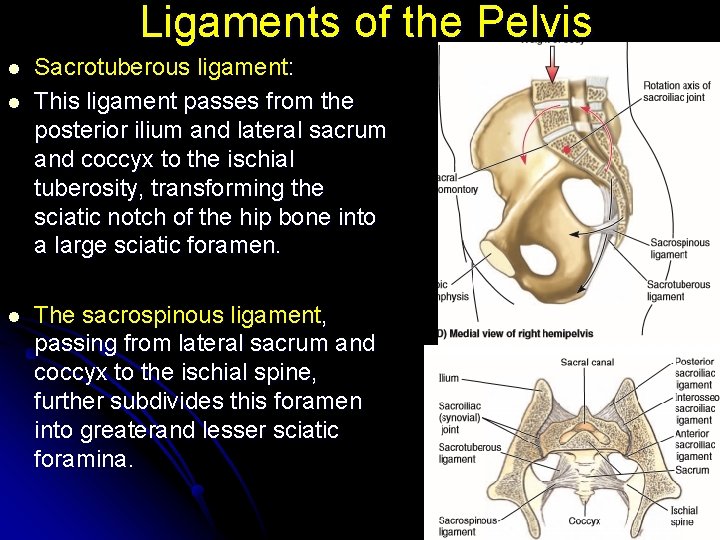
Ligaments of the Pelvis l l l Sacrotuberous ligament: This ligament passes from the posterior ilium and lateral sacrum and coccyx to the ischial tuberosity, transforming the sciatic notch of the hip bone into a large sciatic foramen. The sacrospinous ligament, passing from lateral sacrum and coccyx to the ischial spine, further subdivides this foramen into greaterand lesser sciatic foramina.
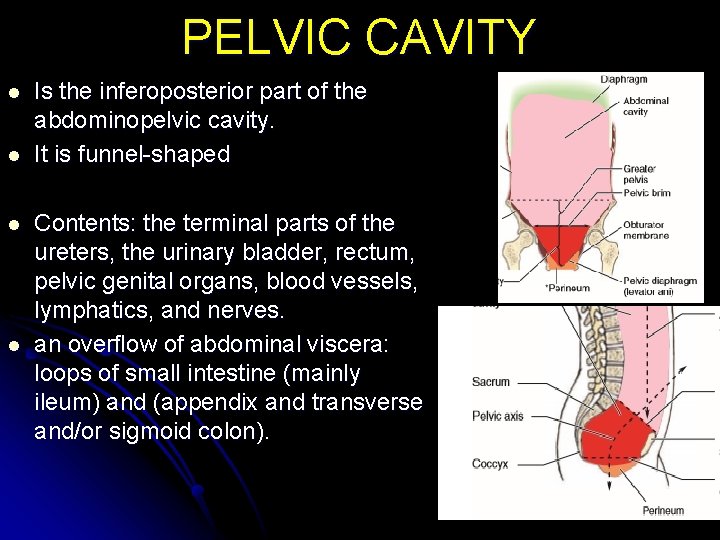
PELVIC CAVITY l l Is the inferoposterior part of the abdominopelvic cavity. It is funnel-shaped Contents: the terminal parts of the ureters, the urinary bladder, rectum, pelvic genital organs, blood vessels, lymphatics, and nerves. an overflow of abdominal viscera: loops of small intestine (mainly ileum) and (appendix and transverse and/or sigmoid colon).
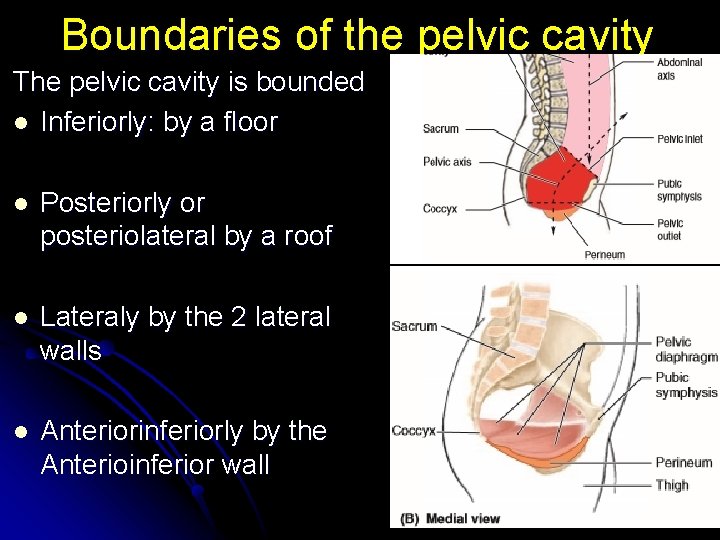
Boundaries of the pelvic cavity The pelvic cavity is bounded l Inferiorly: by a floor l Posteriorly or posteriolateral by a roof l Lateraly by the 2 lateral walls l Anteriorinferiorly by the Anterioinferior wall
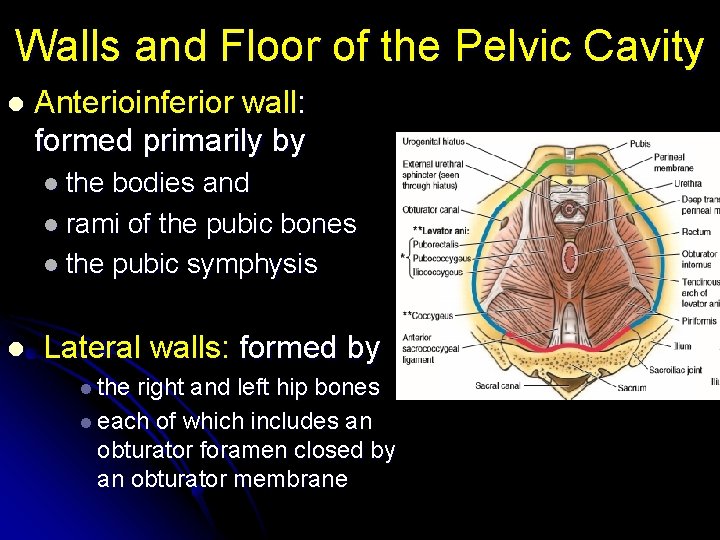
Walls and Floor of the Pelvic Cavity l Anterioinferior wall: formed primarily by l the bodies and l rami of the pubic bones l the pubic symphysis l Lateral walls: formed by l the right and left hip bones l each of which includes an obturator foramen closed by an obturator membrane
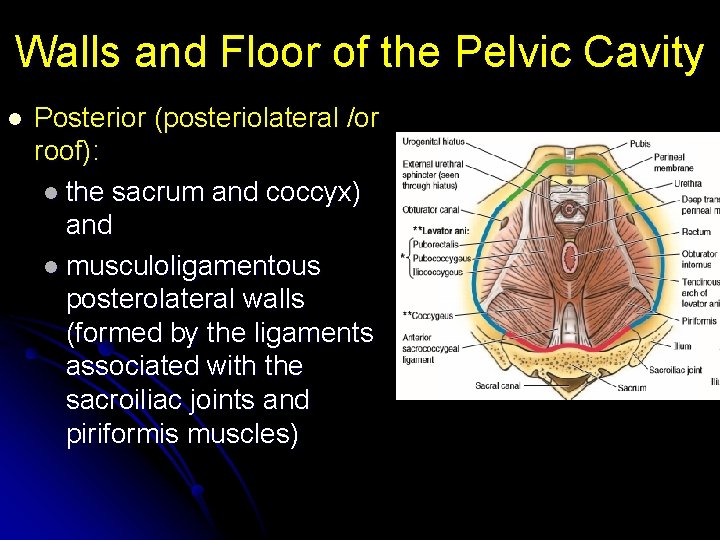
Walls and Floor of the Pelvic Cavity l Posterior (posteriolateral /or roof): l the sacrum and coccyx) and l musculoligamentous posterolateral walls (formed by the ligaments associated with the sacroiliac joints and piriformis muscles)
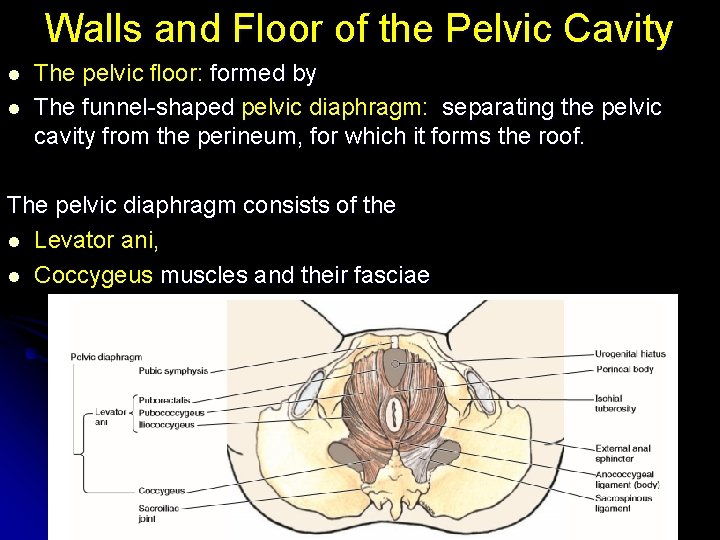
Walls and Floor of the Pelvic Cavity l l The pelvic floor: formed by The funnel-shaped pelvic diaphragm: separating the pelvic cavity from the perineum, for which it forms the roof. The pelvic diaphragm consists of the l Levator ani, l Coccygeus muscles and their fasciae
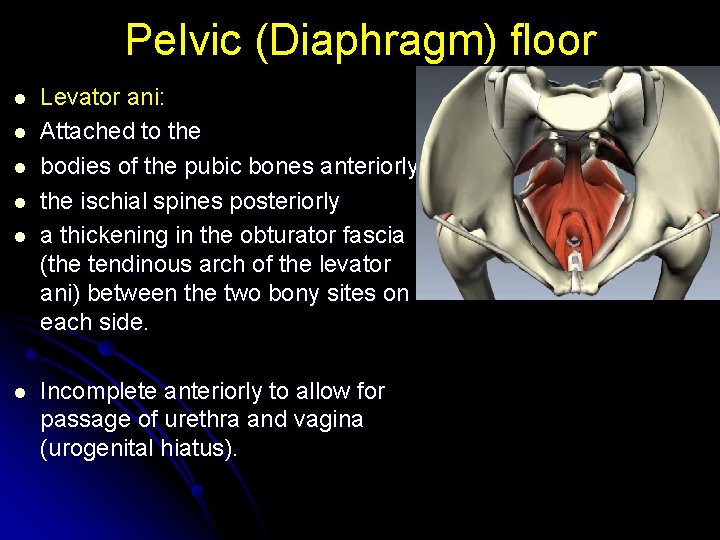
Pelvic (Diaphragm) floor l l l Levator ani: Attached to the bodies of the pubic bones anteriorly the ischial spines posteriorly a thickening in the obturator fascia (the tendinous arch of the levator ani) between the two bony sites on each side. Incomplete anteriorly to allow for passage of urethra and vagina (urogenital hiatus).
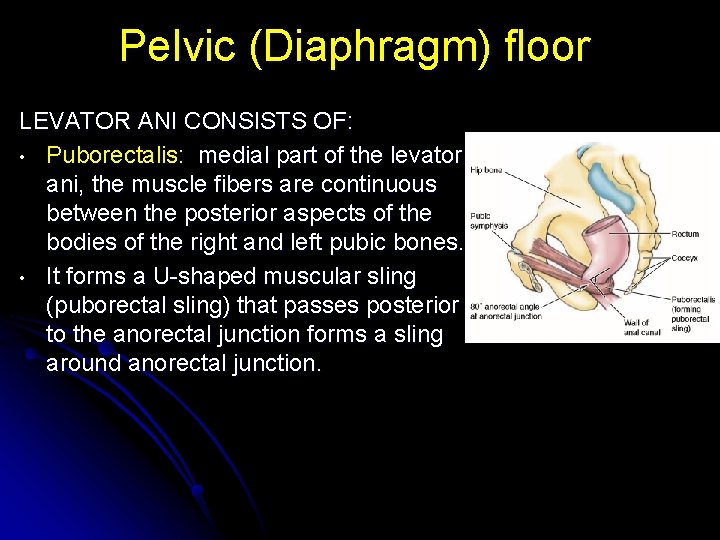
Pelvic (Diaphragm) floor LEVATOR ANI CONSISTS OF: • Puborectalis: medial part of the levator ani, the muscle fibers are continuous between the posterior aspects of the bodies of the right and left pubic bones. • It forms a U-shaped muscular sling (puborectal sling) that passes posterior to the anorectal junction forms a sling around anorectal junction.
Pelvic (Diaphragm) floor • • • Pubococcygeus: intermediate part of the levator ani arises lateral to the puborectalis from the posterior aspect of the body of the pubis and anterior tendinous arch its lateral fibers attach to the coccyx and its medial fibers merge with those of the contralateral muscle to form a fibrous raphe or tendinous plate, part of the anococcygeal bodyor ligament between the anus and the coccyx (often referred to clinically as the “levator plate”).
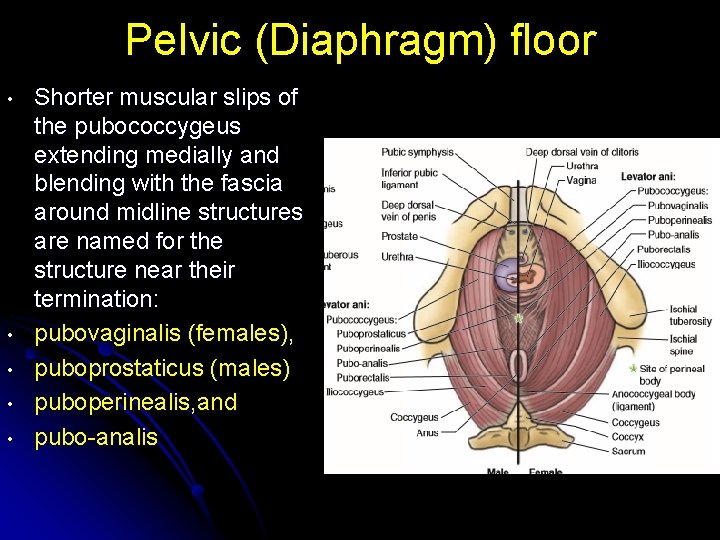
Pelvic (Diaphragm) floor • • • Shorter muscular slips of the pubococcygeus extending medially and blending with the fascia around midline structures are named for the structure near their termination: pubovaginalis (females), puboprostaticus (males) puboperinealis, and pubo-analis
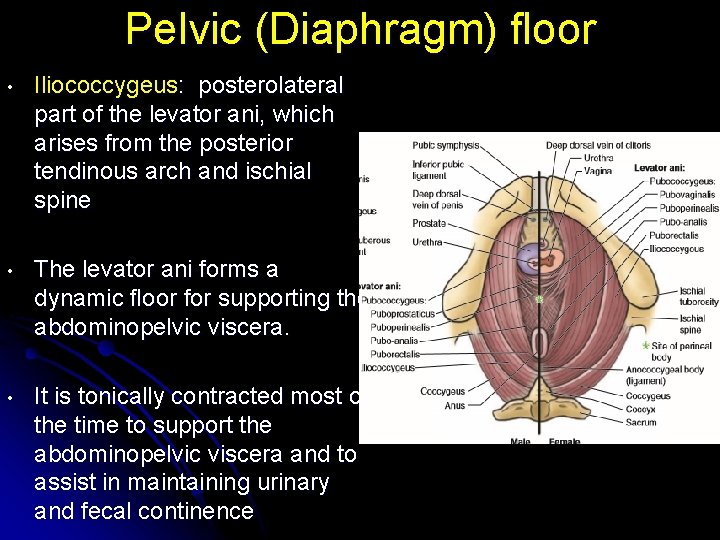
Pelvic (Diaphragm) floor • Iliococcygeus: posterolateral part of the levator ani, which arises from the posterior tendinous arch and ischial spine • The levator ani forms a dynamic floor for supporting the abdominopelvic viscera. • It is tonically contracted most of the time to support the abdominopelvic viscera and to assist in maintaining urinary and fecal continence
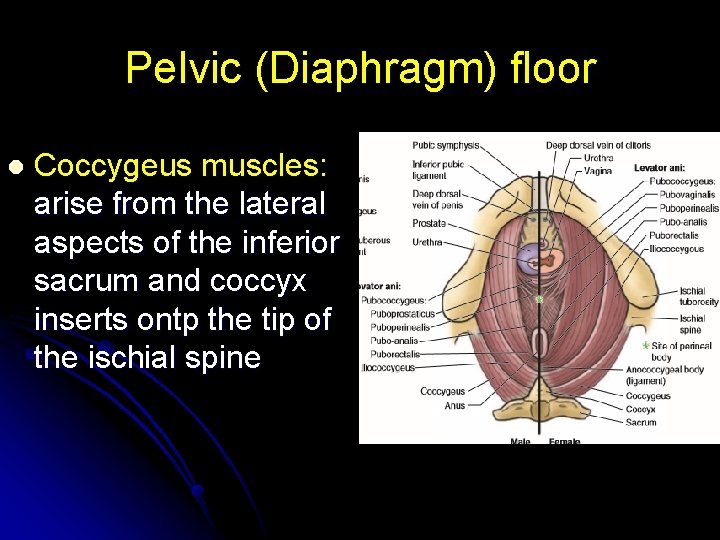
Pelvic (Diaphragm) floor l Coccygeus muscles: arise from the lateral aspects of the inferior sacrum and coccyx inserts ontp the tip of the ischial spine
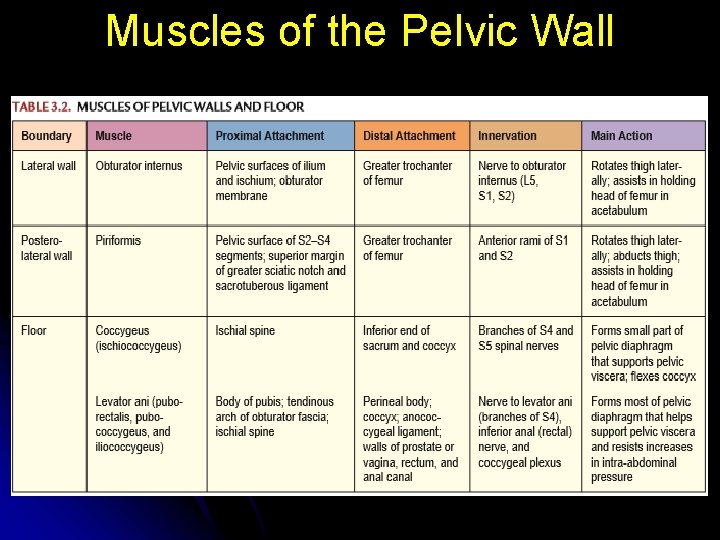
Muscles of the Pelvic Wall
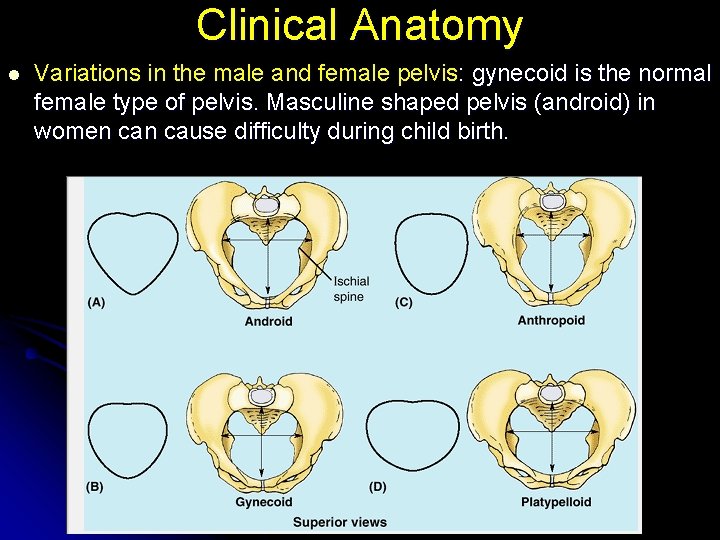
Clinical Anatomy l Variations in the male and female pelvis: gynecoid is the normal female type of pelvis. Masculine shaped pelvis (android) in women cause difficulty during child birth.
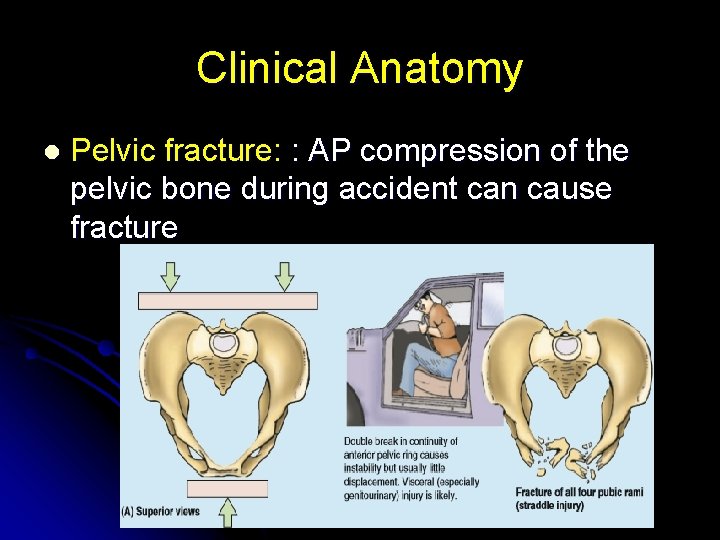
Clinical Anatomy l Pelvic fracture: : AP compression of the pelvic bone during accident can cause fracture
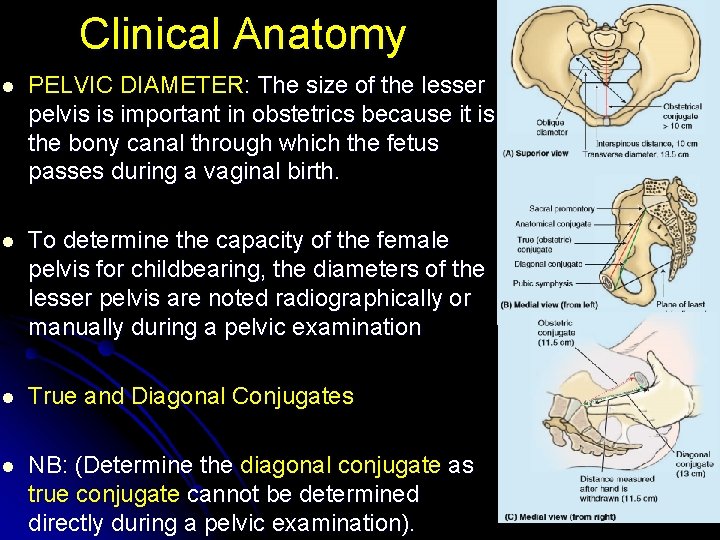
Clinical Anatomy l PELVIC DIAMETER: The size of the lesser pelvis is important in obstetrics because it is the bony canal through which the fetus passes during a vaginal birth. l To determine the capacity of the female pelvis for childbearing, the diameters of the lesser pelvis are noted radiographically or manually during a pelvic examination l True and Diagonal Conjugates l NB: (Determine the diagonal conjugate as true conjugate cannot be determined directly during a pelvic examination).
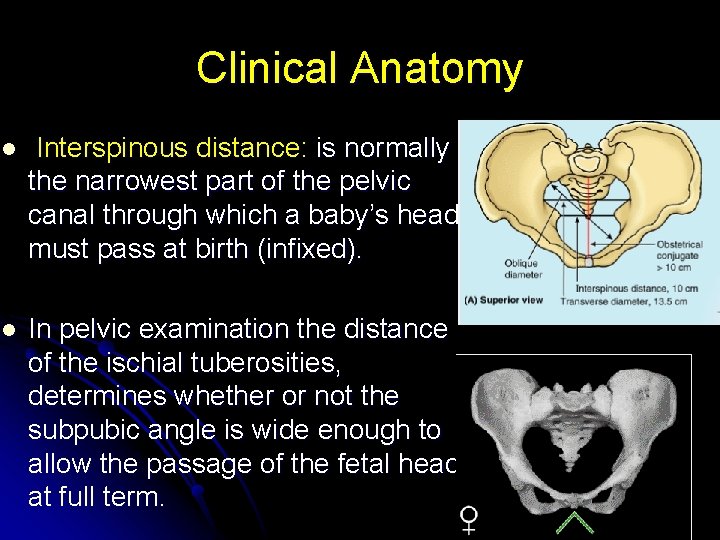
Clinical Anatomy l Interspinous distance: is normally the narrowest part of the pelvic canal through which a baby’s head must pass at birth (infixed). l In pelvic examination the distance of the ischial tuberosities, determines whether or not the subpubic angle is wide enough to allow the passage of the fetal head at full term.
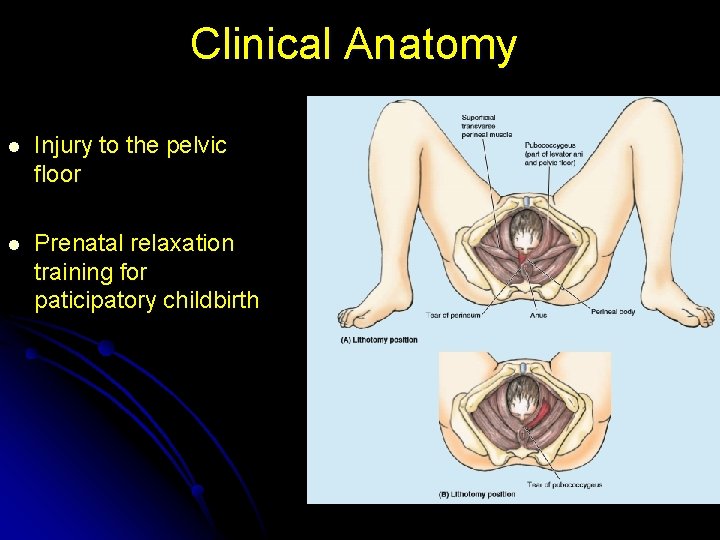
Clinical Anatomy l Injury to the pelvic floor l Prenatal relaxation training for paticipatory childbirth
THANK YOU
- Slides: 36