Bone Tissue Part 2 Support Movement Function of
Bone Tissue Part 2: Support & Movement
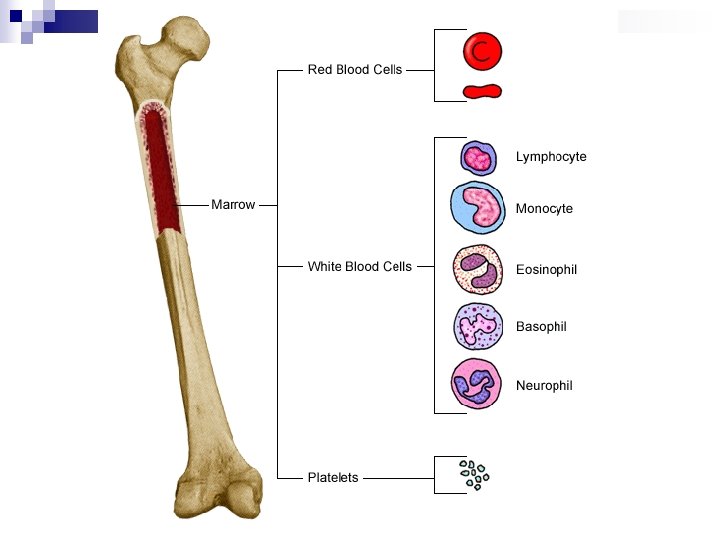
Function of the Human Skeleton n Provides support for the body Protection to the internal organs Provides & framework for the connection of skeletal muscles ¨ Allows n for movement Contains red bone marrow for blood formation and storage ¨ Produces n blood cells Primary storage site for minerals & fats ¨ Including calcium!
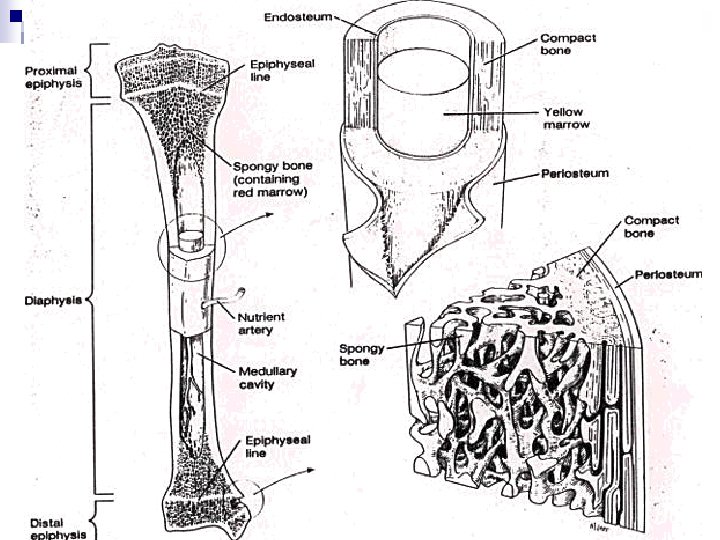
Bone Tissue n Osseous (Bone) Tissue: Dynamic (everchanging) living tissue that makes up the skeletal structure. ¨ Bone is a type of connective tissue with a matrix made of hydoxyapatite (a calcium salt). n Two types of bone: ¨ Compact Bone ¨ Spongy Bone
Bone Tissue n Osteon: The functional unit of compact bone. Contains many types of bone cells. ¨ Osteogenic Cells: “Stem Cells” that divide to provide a constant supply of the other bone cells. ¨ Osteoblasts: “Bone-building” cells that transport calcium from the bloodstream to the bone matrix. ¨ Osteoclasts: “Bone-chewing” cells that reabsorb bone & transport calcium from the bone to the blood.
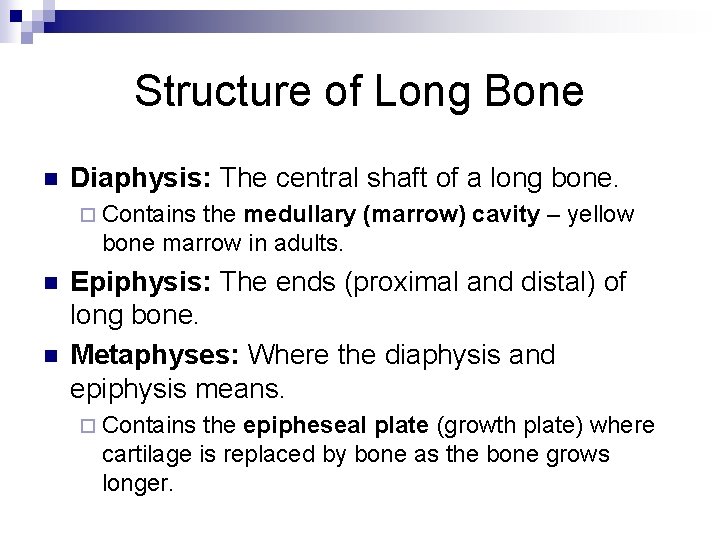
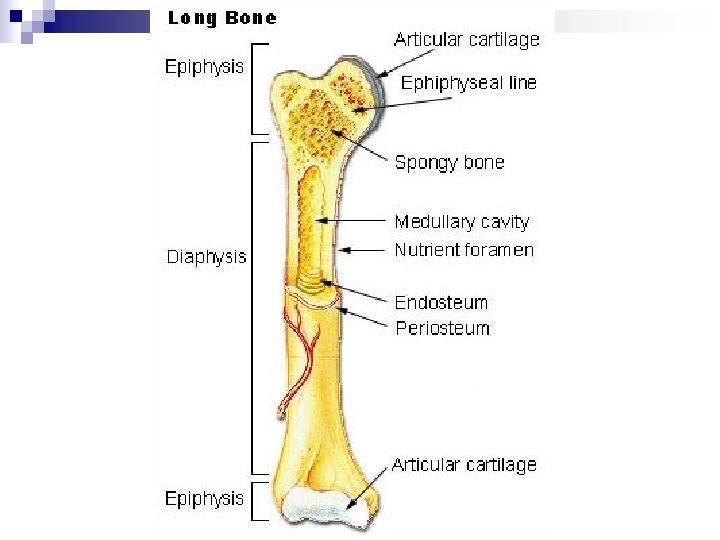
Structure of Long Bone n Diaphysis: The central shaft of a long bone. ¨ Contains the medullary (marrow) cavity – yellow bone marrow in adults. n n Epiphysis: The ends (proximal and distal) of long bone. Metaphyses: Where the diaphysis and epiphysis means. ¨ Contains the epipheseal plate (growth plate) where cartilage is replaced by bone as the bone grows longer.
Structure of Long Bone Articular Cartilage: The layer of hyaline cartilage surrounding the epiphysis where bones connect at joints. n Periosteum: The tough covering on the outside of the surface of bone, composed primarily of dense irregular connective tissue. n Endosteum: Thin membrane lining medullary cavity. n ¨ Contains a single layer of bone-forming cells.
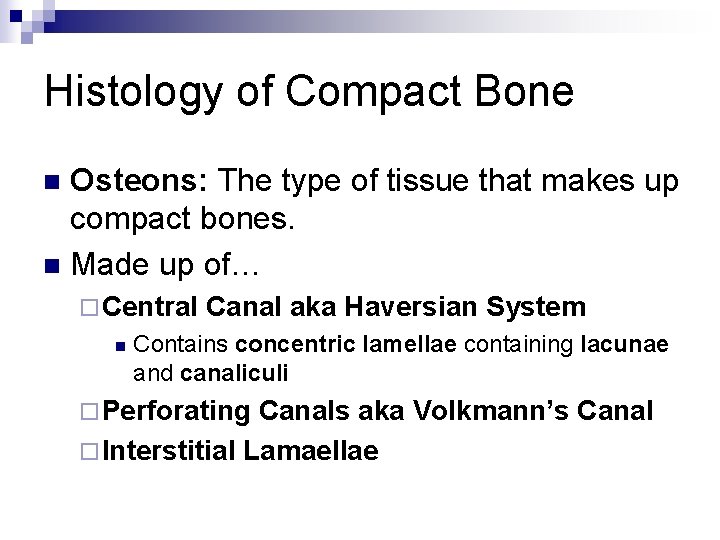
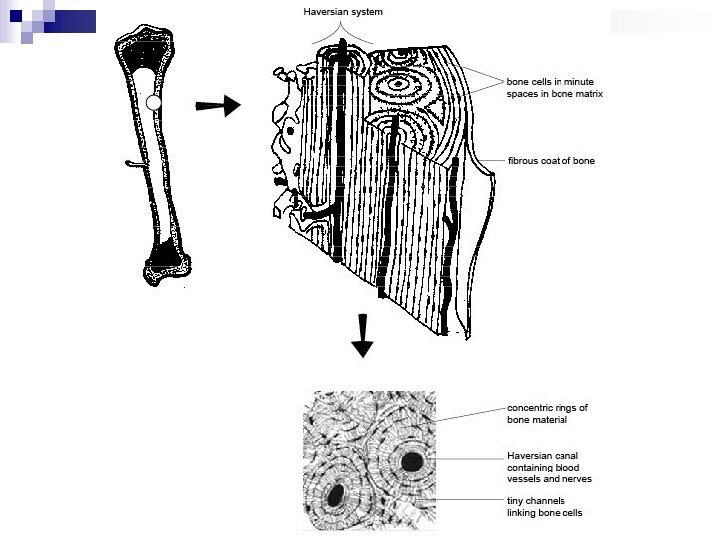
Histology of Compact Bone Osteons: The type of tissue that makes up compact bones. n Made up of… n ¨ Central n Canal aka Haversian System Contains concentric lamellae containing lacunae and canaliculi ¨ Perforating Canals aka Volkmann’s Canal ¨ Interstitial Lamaellae
Components of Osteons n Central Canal aka Haversian Systems: The functional unit of compact bone. Located in the center of the osteon. ¨ Provides a passageway for blood vessels and nerves through the length of the bone. ¨ Surrounded by calcified rings called concentric lamellae Lacunae: Spaces in the concentric lamellae containing osteocytes. n Canaliculi: Tiny canals between the lamellae. n
Components of Osteons n Perforating Canal aka Volkmann’s Canal: Passageways with blood & lymph vessels and nerves running at a right angle to the Haversian canals. ¨ Connects blood vessels from Periosteum to Haversian canals. n Interstitial Lamellae: The area between the osteons ¨ Consists of fragments of old, partially destroyed osteons

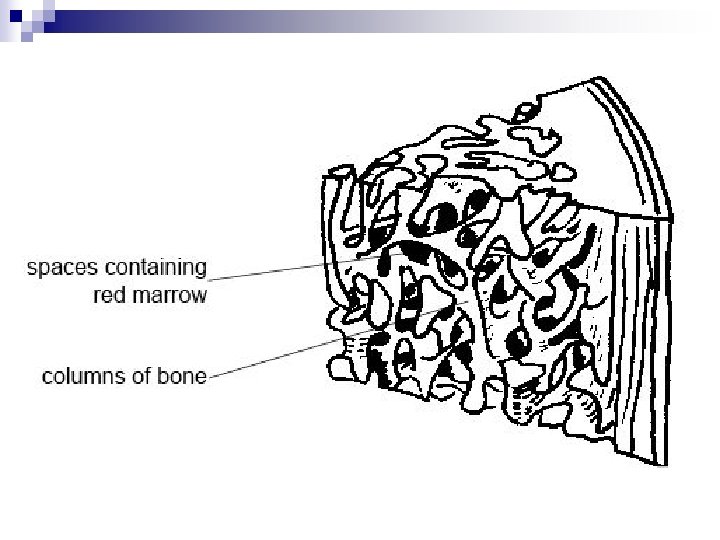
Spongy Bone n Spongy Bone: Consists of a latticework of columns of bones called trabiculae. ¨ Named for the “sponge-like” appearance ¨ Permeated spaced filled with bone marrow, NOT osteons ¨ Trabeculae develop along lines of stress n Wolf’s Law: Bone mass & density will increase in areas of stress, so bone will be thickest where it is under the greatest stress. ¨ Much lighter than compact bone ¨ Found in irregularly shaped bones in places with less stress or stress from multiple directions ¨ Found at the epiphyses of long bones
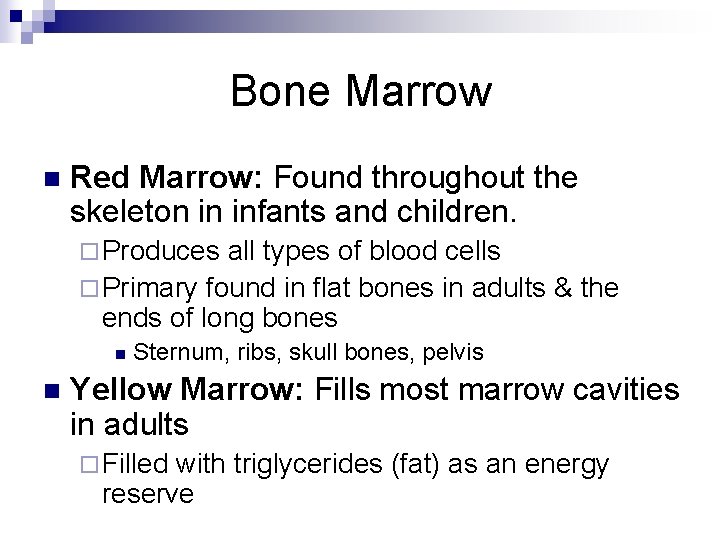
Bone Marrow n Red Marrow: Found throughout the skeleton in infants and children. ¨ Produces all types of blood cells ¨ Primary found in flat bones in adults & the ends of long bones n n Sternum, ribs, skull bones, pelvis Yellow Marrow: Fills most marrow cavities in adults ¨ Filled with triglycerides (fat) as an energy reserve
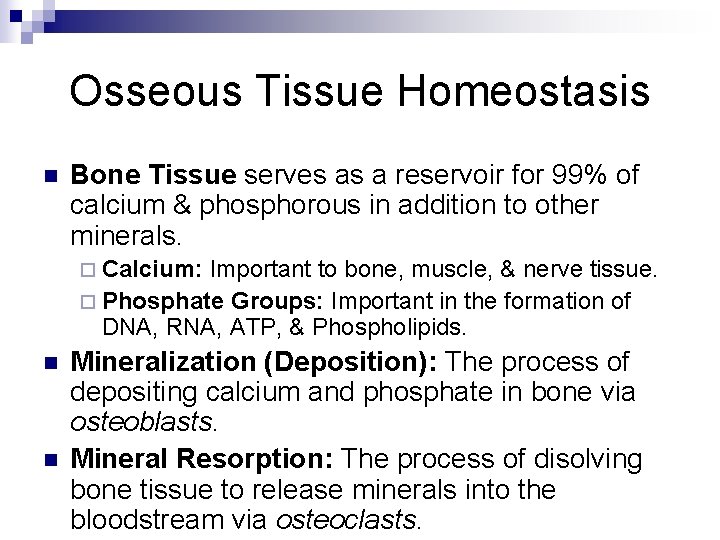
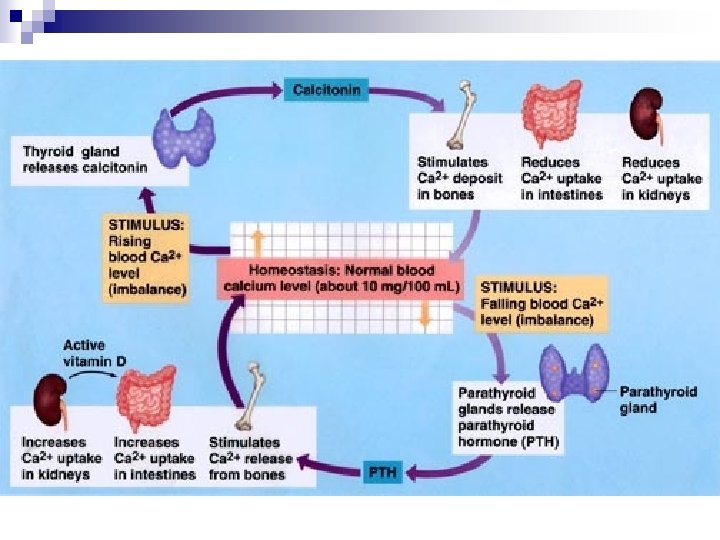
Osseous Tissue Homeostasis n Bone Tissue serves as a reservoir for 99% of calcium & phosphorous in addition to other minerals. ¨ Calcium: Important to bone, muscle, & nerve tissue. ¨ Phosphate Groups: Important in the formation of DNA, RNA, ATP, & Phospholipids. n n Mineralization (Deposition): The process of depositing calcium and phosphate in bone via osteoblasts. Mineral Resorption: The process of disolving bone tissue to release minerals into the bloodstream via osteoclasts.
Hypocalcaemia n Hypocalcaemia: Low calcium concentration in the blood. ¨ Can result in adverse effects on the nervous and muscle systems.
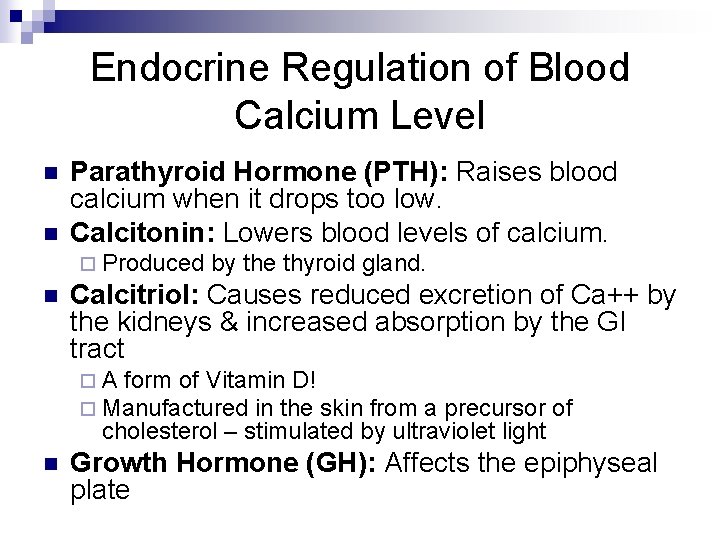
Endocrine Regulation of Blood Calcium Level n n Parathyroid Hormone (PTH): Raises blood calcium when it drops too low. Calcitonin: Lowers blood levels of calcium. ¨ Produced n by the thyroid gland. Calcitriol: Causes reduced excretion of Ca++ by the kidneys & increased absorption by the GI tract ¨ A form of Vitamin D! ¨ Manufactured in the skin from a precursor of cholesterol – stimulated by ultraviolet light n Growth Hormone (GH): Affects the epiphyseal plate
Bone Formation & Development Ossification: The process by which bones are formed. n TWO Methods of Ossification: n ¨ Intramembranous Ossification ¨ Endochondral Ossification
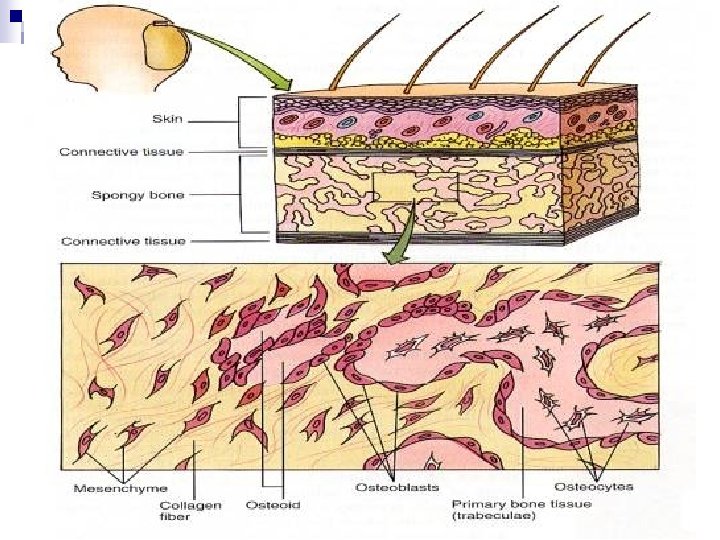
Intramembranous Ossification n Produces flat bones…. ¨ Replaces connective tissue membranes with bone in the skull, forms the mandible (the lower jaw) and the breastbone n n n Starts as embryonic connective tissue called mesenchyme Osteogenic (stem) cells develop into osteoblasts, which secrete bone matrix Calcification: Osteoblasts deposit osteoid tissue, then calcium phosphate is deposited. ¨ Osteoblasts then become osteocytes
Intramembranous Ossification Bone matrix develops into trabiculae to form spongy bone. n Compact bone tissue then forms around spongy bone as the mesenchyme condenses into periosteum n Spongy bone remains in the center, surrounded by a thin layer of compact bone. n
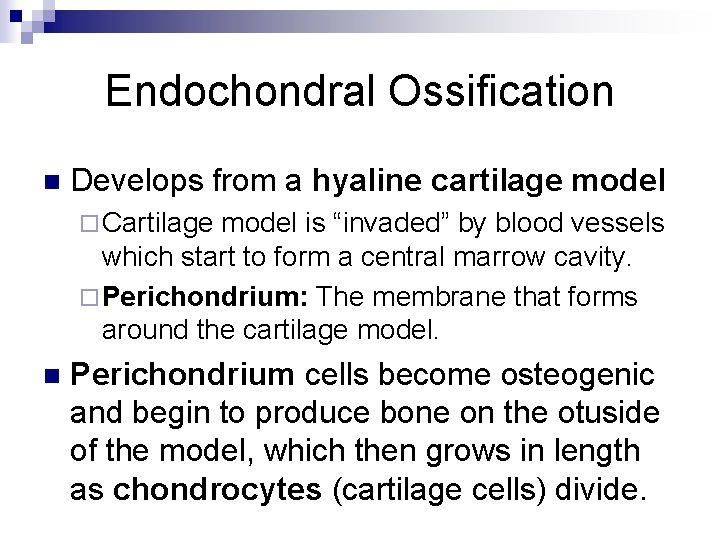
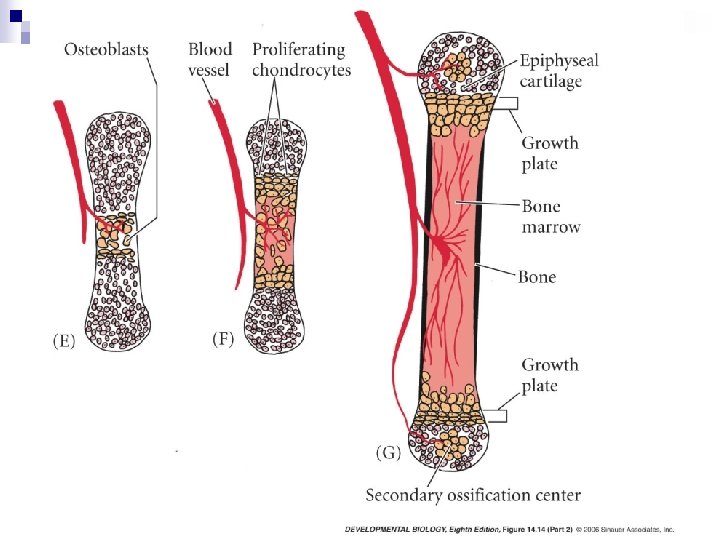
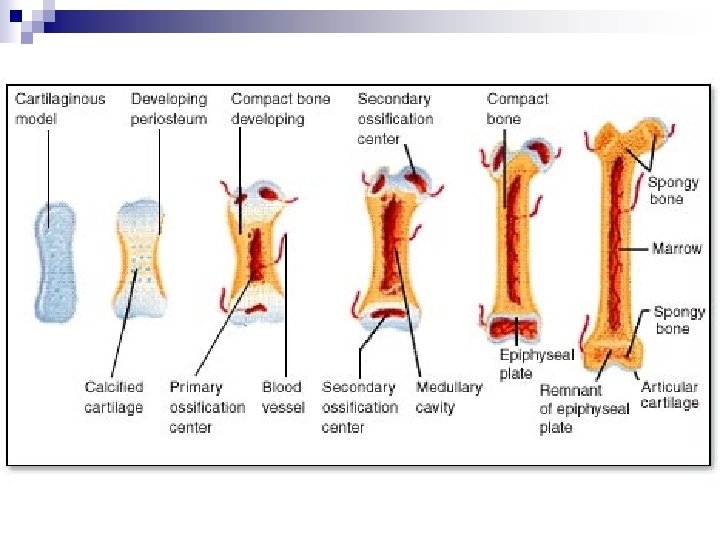
Endochondral Ossification n Develops from a hyaline cartilage model ¨ Cartilage model is “invaded” by blood vessels which start to form a central marrow cavity. ¨ Perichondrium: The membrane that forms around the cartilage model. n Perichondrium cells become osteogenic and begin to produce bone on the otuside of the model, which then grows in length as chondrocytes (cartilage cells) divide.
Endochondral Ossification n Ossification moves inward from the external surface forming a primary ossification center. ¨ Cartilage is then “remodeled” into bone by osteoblasts with mineral deposits. ¨ Perichondrium becomes periosteum Secondary ossifaction proceeds outward from the center of the epiphyses n Hyaline cartilage remains in the growth plates n
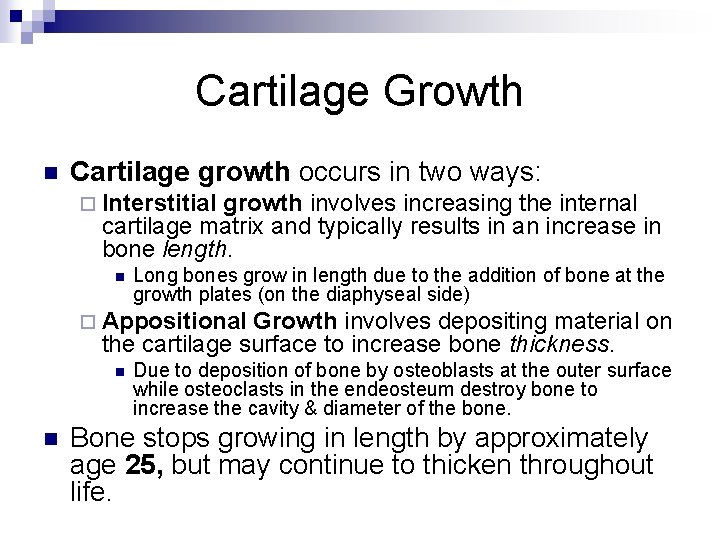
Cartilage Growth n Cartilage growth occurs in two ways: ¨ Interstitial growth involves increasing the internal cartilage matrix and typically results in an increase in bone length. n Long bones grow in length due to the addition of bone at the growth plates (on the diaphyseal side) ¨ Appositional Growth involves depositing material on the cartilage surface to increase bone thickness. n n Due to deposition of bone by osteoblasts at the outer surface while osteoclasts in the endeosteum destroy bone to increase the cavity & diameter of the bone. Bone stops growing in length by approximately age 25, but may continue to thicken throughout life.
Hormonal & Chemical Factors Influencing Bone Development n Homeostasis Factors: ¨ Parathyroid Hormone (PTH) ¨ Calcitonin n Bone Growth: ¨ Growth Hormone (GH) ¨ Thyroxine (Thyroid Hormone) n Sex Hormones ¨ Estrogen ¨ Testosterone
Hormonal & Chemical Factors Influencing Bone Development n Promotion of osteoclast activity ¨ n Vitamins: ¨ ¨ n Calcitriol C K B 12 A Minerals: ¨ ¨ ¨ Calcium Phosphorous Magnesium (Mg) Iron (Fe) Manganese (Mn) Fluorine (F)
Reminder: Cartilage n Types of Cartilage: ¨ Hyaline: Found in articular surfaces, growth plates in long bones ¨ Fibrocartilage: Absorbs shock, found in intervertebral discs ¨ Elastic: Found in the framework of the outer ear & the epiglottis n n Chondroblasts: Cells which actively produce cartilage Chondrocytes: Cells trapped in lacunae of cartilage
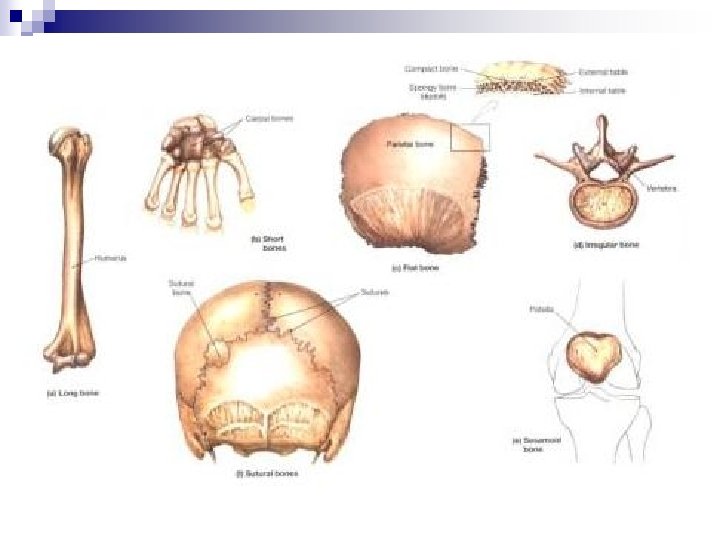
Types of Bones n Long Bones: Bones that are longer than they are wide. ¨ n Short Bones: Closer to equal in length and width. ¨ n E. g. Vertebral bodies, ethmoid and sphenoid bones Sesamoid Bones: Bone contained in a tendon ¨ n E. g. cranium, breastbone Irregular Bones: Elaborate shapes that don’t fit the other types ¨ n E. g. wrist & ankle bones Flat Bones: Enclose/protect organs ¨ n E. g. humerous, radius, femer, etc. E. g. patella (kneecap) Sutures: Small bones located within suture joints.
Bone Processes n Bone Processes: The markings found on the bones. ¨ Tubercle ¨ Tuberosity ¨ Fovea ¨ Foramen ¨ Condyles ¨ Fossa
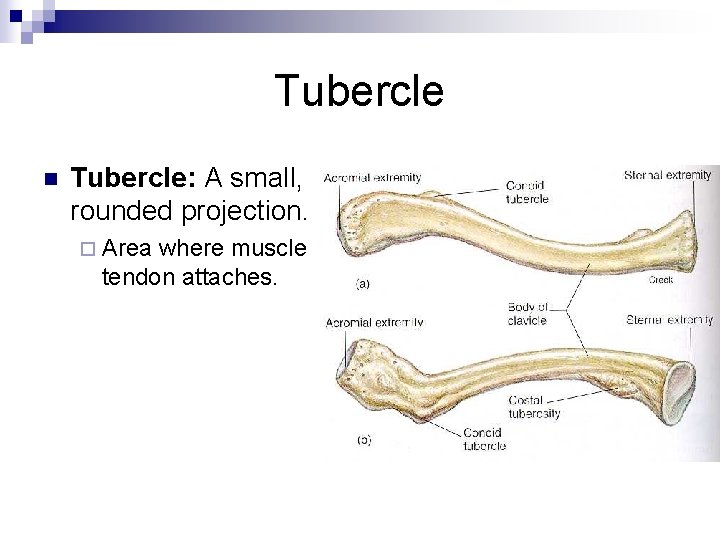
Tubercle n Tubercle: A small, rounded projection. ¨ Area where muscle tendon attaches.
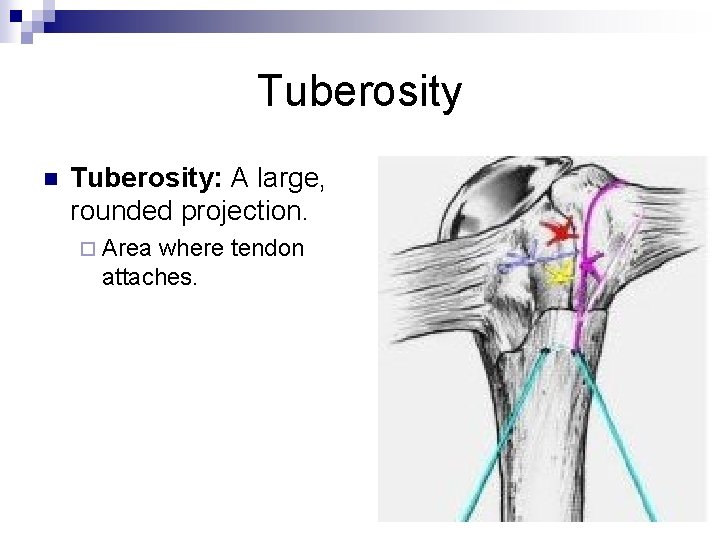
Tuberosity n Tuberosity: A large, rounded projection. ¨ Area where tendon attaches.
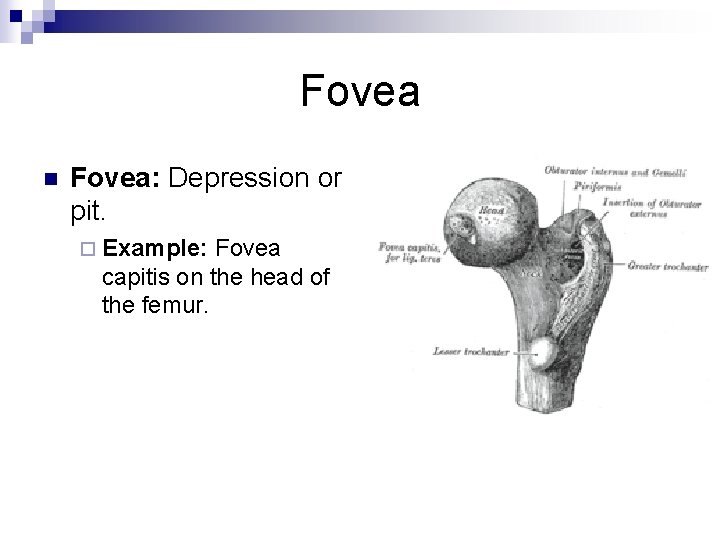
Fovea n Fovea: Depression or pit. ¨ Example: Fovea capitis on the head of the femur.
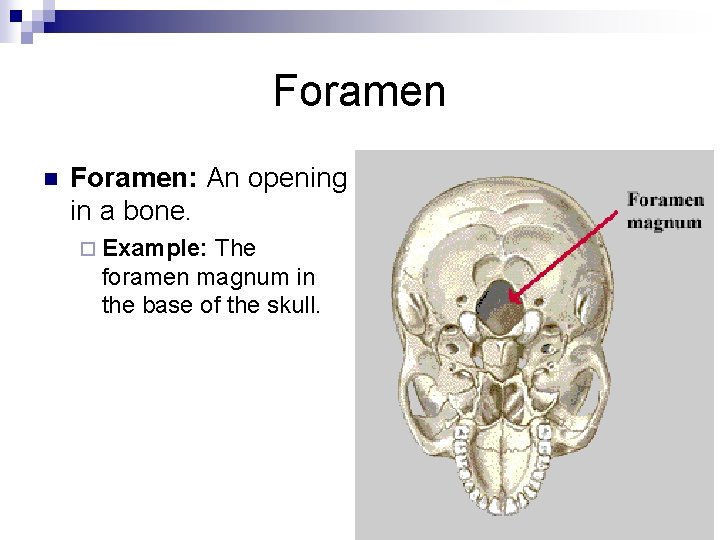
Foramen n Foramen: An opening in a bone. ¨ Example: The foramen magnum in the base of the skull.
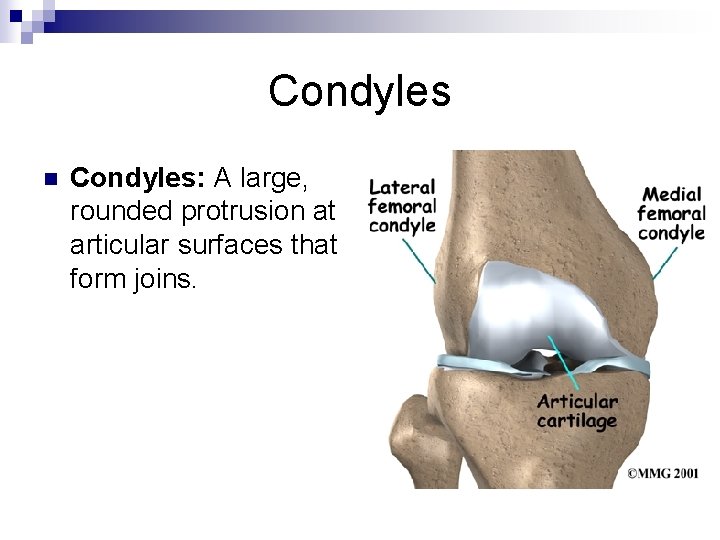
Condyles n Condyles: A large, rounded protrusion at articular surfaces that form joins.
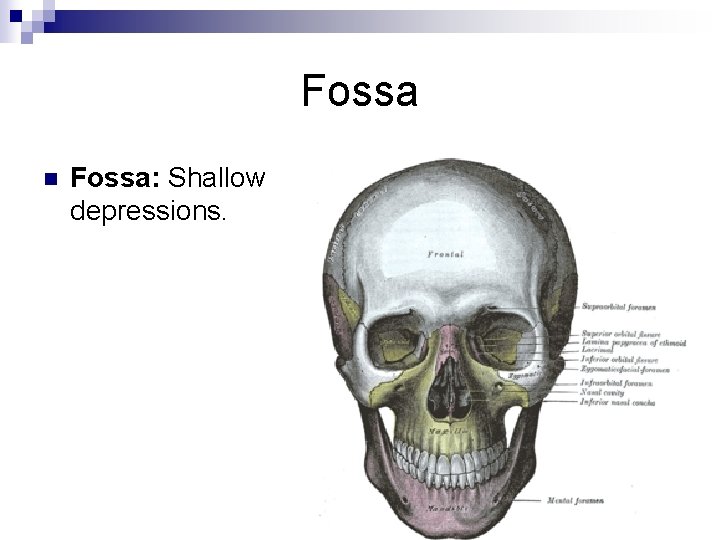
Fossa n Fossa: Shallow depressions.
Bone Remodeling n Bone Remodeling: The process of bone rebuilding itself. ¨ Used as a means of constant renewal and to redistribute the bone matrix (such as at areas of increased stress or to heal injuries). ¨ Typically occurs as a balance between resorption by osteoclasts and deposition of osteoblasts.
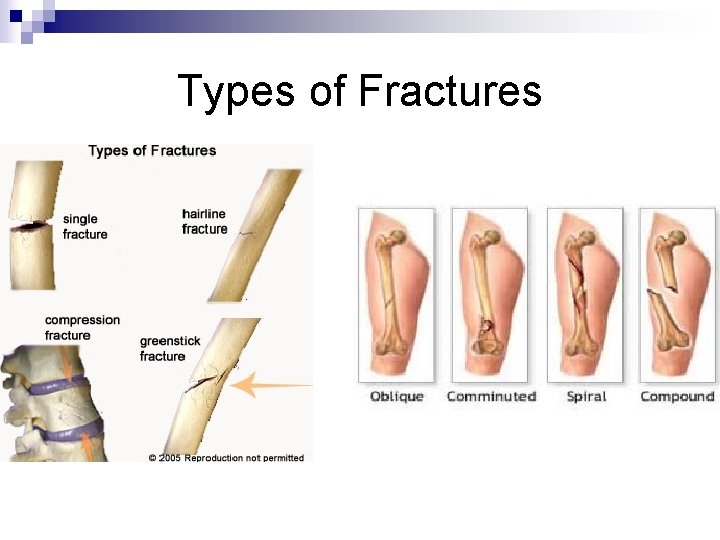
Types of Fractures
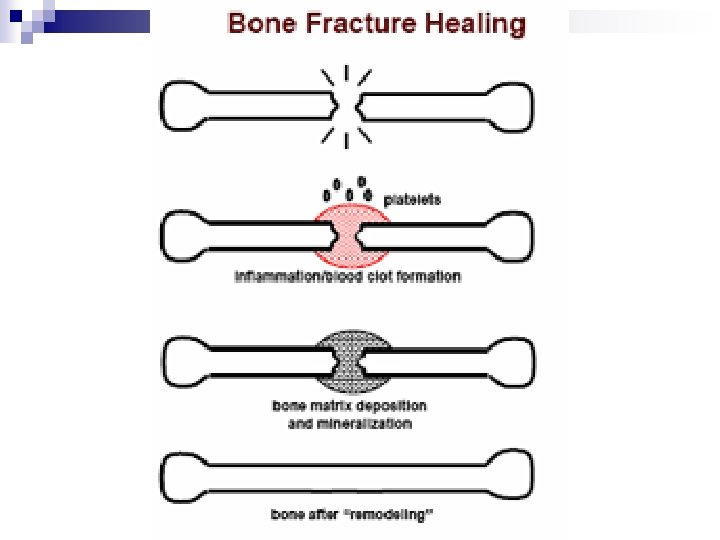
Bone Healing n Stages of Bone Healing/Fracture Healing: ¨ Reactive Phase ¨ Reparative Phase ¨ Remodeling Phase
Fracture Healing n Reactive Phase: ¨ Blood vessels near the fracture constrict to stop further bleeding ¨ Extravascular blood cells (“hematoma”) form a blood clot within a few hours ¨ The blood cells within the clot die, while fibroblasts survive & replicate to create a loose aggregate of cells interspersed with small blood vessels – known as Granulation Tissue
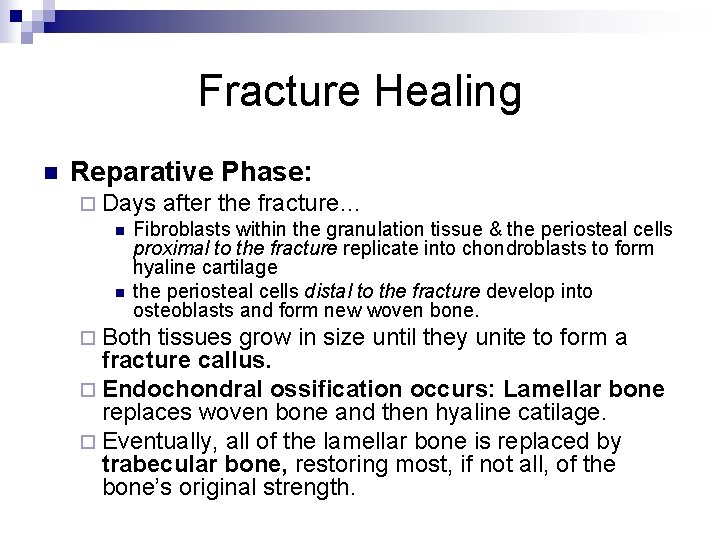
Fracture Healing n Reparative Phase: ¨ Days after the fracture… n Fibroblasts within the granulation tissue & the periosteal cells proximal to the fracture replicate into chondroblasts to form hyaline cartilage n the periosteal cells distal to the fracture develop into osteoblasts and form new woven bone. ¨ Both tissues grow in size until they unite to form a fracture callus. ¨ Endochondral ossification occurs: Lamellar bone replaces woven bone and then hyaline catilage. ¨ Eventually, all of the lamellar bone is replaced by trabecular bone, restoring most, if not all, of the bone’s original strength.
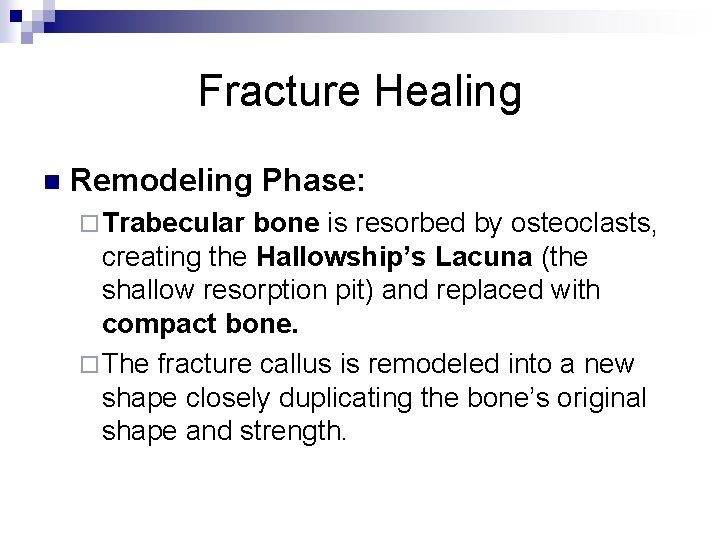
Fracture Healing n Remodeling Phase: ¨ Trabecular bone is resorbed by osteoclasts, creating the Hallowship’s Lacuna (the shallow resorption pit) and replaced with compact bone. ¨ The fracture callus is remodeled into a new shape closely duplicating the bone’s original shape and strength.
- Slides: 49