Bone and Mineral Disorders in Chronic Kidney Disease
Bone and Mineral Disorders in Chronic Kidney Disease Parker Gregg Internal Medicine R 3

Learning Objectives Describe the mechanisms by which bone and mineral disorders develop in CKD Differentiate secondary hyperparathyroidism, adynamic bone disease, and other bone/mineral disorders by lab values and clinical presentation List 3 different medications for the treatment of hyperparathyroidism in CKD and how they differ
Table of Contents Review of normal calcium, phos, PTH, and vitamin D homeostasis How things go so wrong in CKD MKSAP cases to illustrate types of bone and mineral disorders in CKD Monitoring and treatment of bone and mineral disorders in CKD
NORMAL CALCIUM, PHOS, PTH, AND VITAMIN D HOMEOSTASIS
Key Points ECF calcium comes from guts, bones, and kidneys Vitamin D’s main goal is to increase bone mineralization PTH does everything it can to increase ECF calcium, but to keep phos relatively balanced it wastes phos in the urine ECF calcium and vitamin D decrease PTH secretion; phos increases PTH secretion
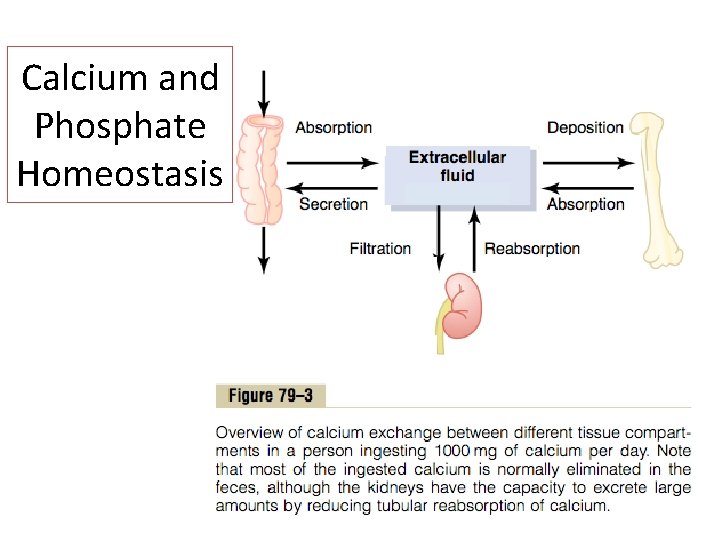
Calcium and Phosphate Homeostasis
Key Points ECF calcium comes from guts, bones, and kidneys Vitamin D’s main goal is to increase bone mineralization PTH does everything it can to increase ECF calcium, but to keep phos relatively balanced it wastes phos in the urine ECF calcium and vitamin D decrease PTH secretion; phos increases PTH secretion
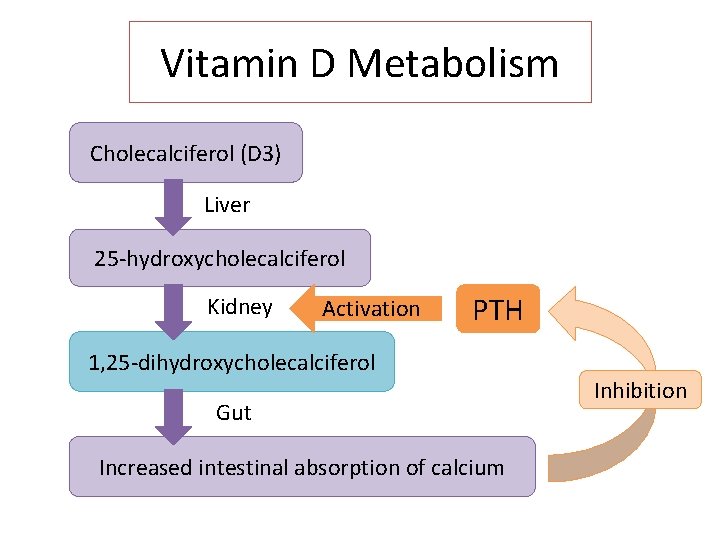
Vitamin D Metabolism Cholecalciferol (D 3) Liver 25 -hydroxycholecalciferol Kidney Activation PTH 1, 25 -dihydroxycholecalciferol Gut Increased intestinal absorption of calcium Inhibition
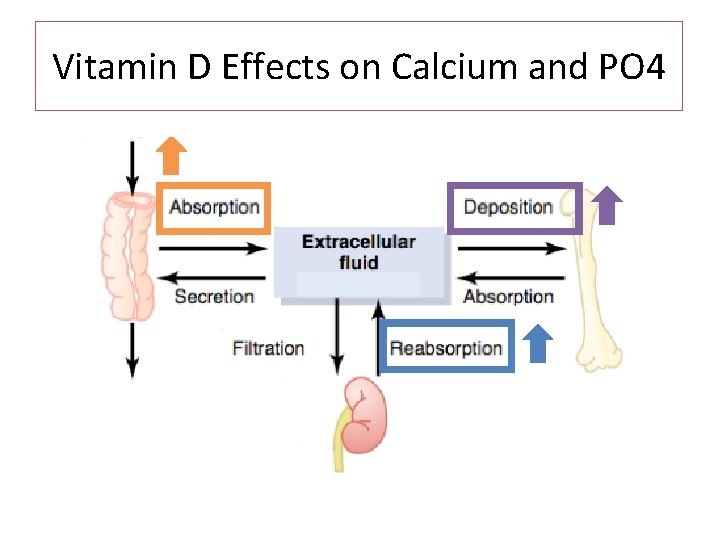
Vitamin D Effects on Calcium and PO 4
Key Points ECF calcium comes from guts, bones, and kidneys Vitamin D’s main goal is to increase bone mineralization PTH does everything it can to increase ECF calcium, but to keep phos relatively balanced it wastes phos in the urine ECF calcium and vitamin D decrease PTH secretion; phos increases PTH secretion
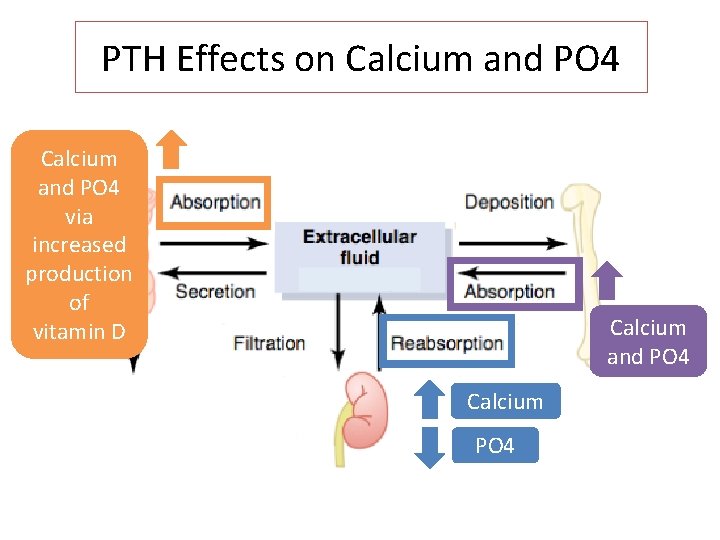
PTH Effects on Calcium and PO 4 via increased production of vitamin D Calcium and PO 4 Calcium PO 4
Key Points ECF calcium comes from guts, bones, and kidneys Vitamin D’s main goal is to increase bone mineralization PTH does everything it can to increase ECF calcium, but to keep phos relatively balanced it wastes phos in the urine ECF calcium and vitamin D decrease PTH secretion; phos increases PTH secretion
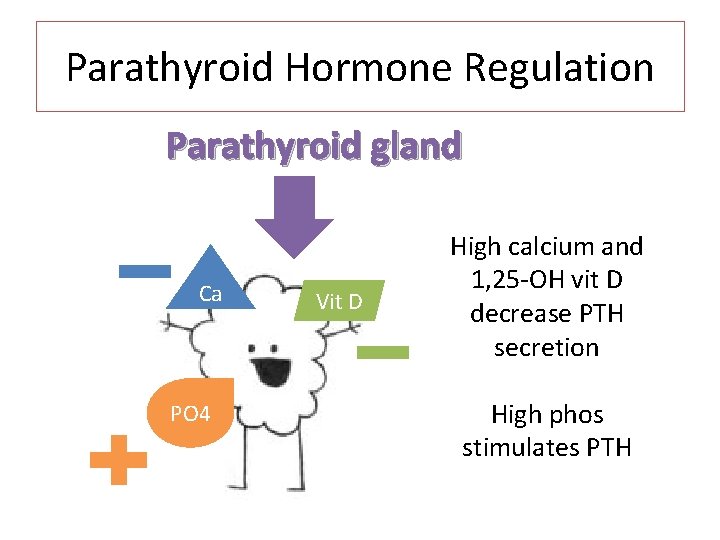
Parathyroid Hormone Regulation Parathyroid gland Ca PO 4 Vit D High calcium and 1, 25 -OH vit D decrease PTH secretion High phos stimulates PTH
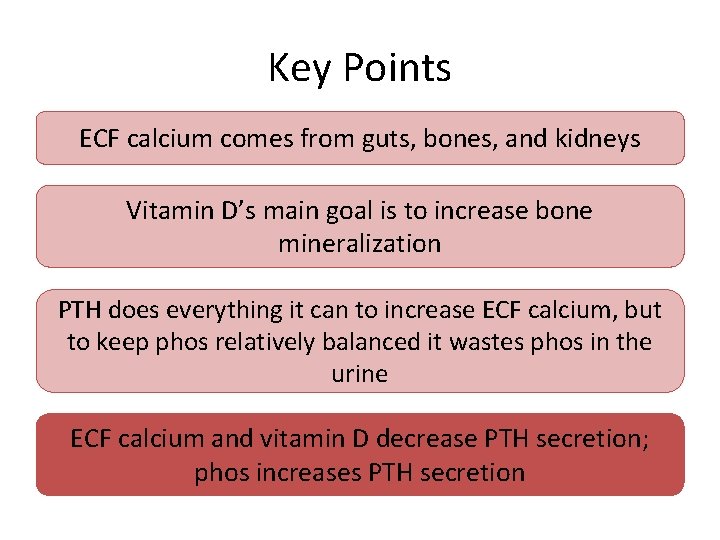
Key Points ECF calcium comes from guts, bones, and kidneys Vitamin D’s main goal is to increase bone mineralization PTH does everything it can to increase ECF calcium, but to keep phos relatively balanced it wastes phos in the urine ECF calcium and vitamin D decrease PTH secretion; phos increases PTH secretion

WHEN THINGS START TO GO WRONG
CKD Bone and mineral disorders
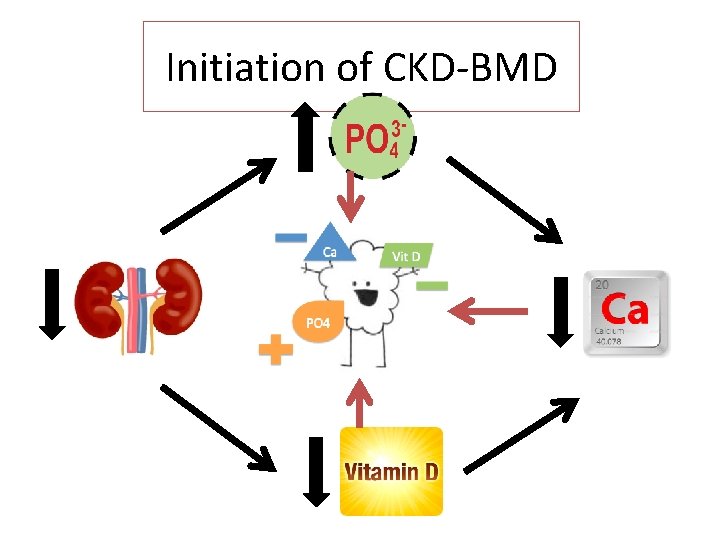
Initiation of CKD-BMD

Initiation of CKD-BMD Decreased GFR Decreased filtration of phos Hyperphosphatemia Hypocalcemia Increased PTH Early secondary hyperparathyroidism maintains normal calcium and phos levels
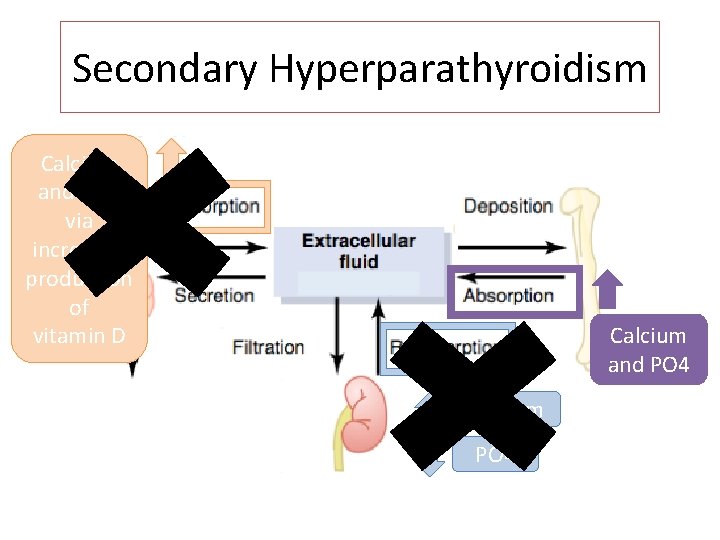
Secondary Hyperparathyroidism Calcium and PO 4 via increased production of vitamin D Calcium and PO 4 Calcium PO 4
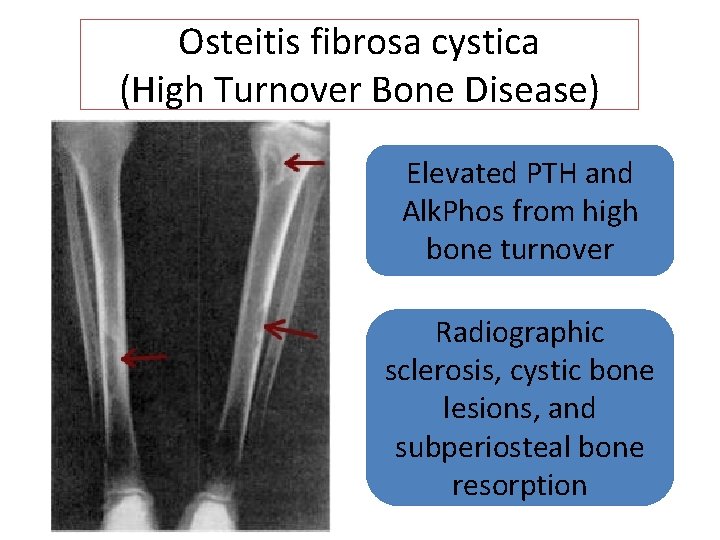
Osteitis fibrosa cystica (High Turnover Bone Disease) Elevated PTH and Alk. Phos from high bone turnover Radiographic sclerosis, cystic bone lesions, and subperiosteal bone resorption
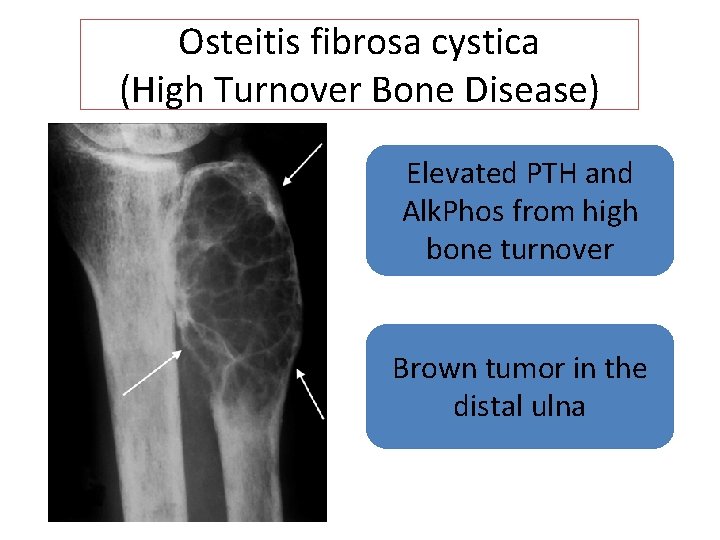
Osteitis fibrosa cystica (High Turnover Bone Disease) Elevated PTH and Alk. Phos from high bone turnover Brown tumor in the distal ulna
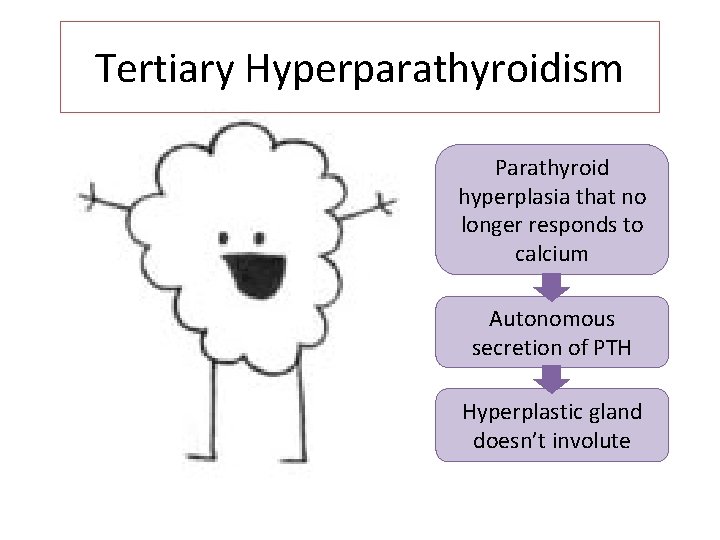
Tertiary Hyperparathyroidism Parathyroid hyperplasia that no longer responds to calcium Autonomous secretion of PTH Hyperplastic gland doesn’t involute
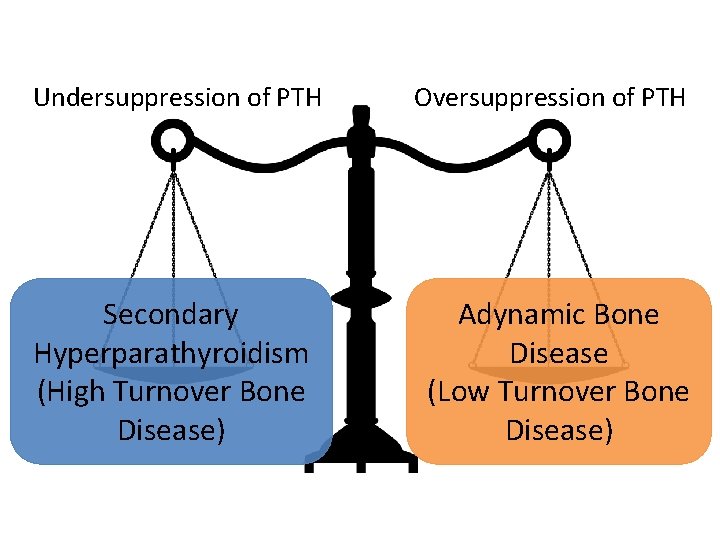
Undersuppression of PTH Secondary Hyperparathyroidism (High Turnover Bone Disease) Oversuppression of PTH Adynamic Bone Disease (Low Turnover Bone Disease)
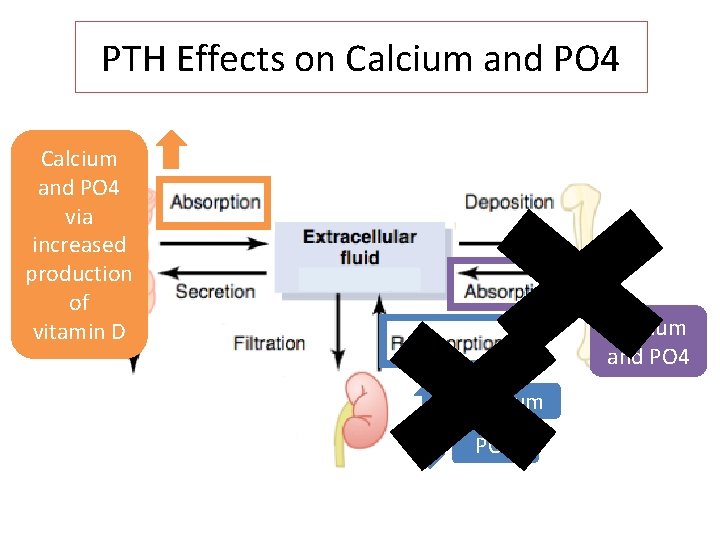
PTH Effects on Calcium and PO 4 via increased production of vitamin D Calcium and PO 4 Calcium PO 4
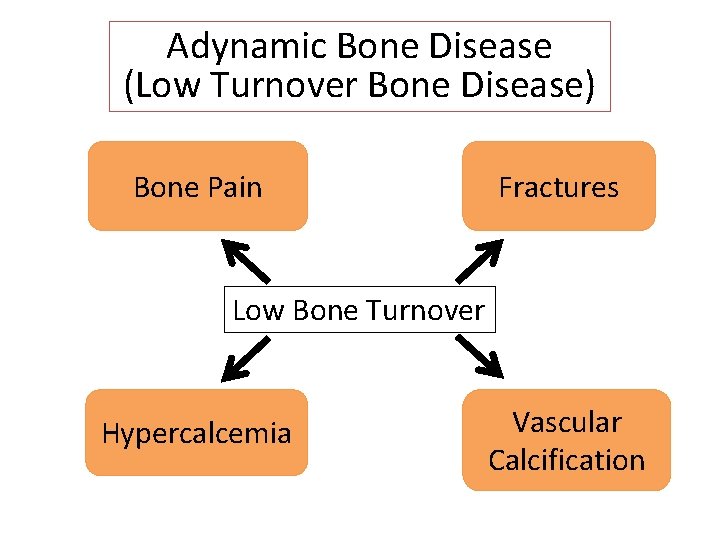
Adynamic Bone Disease (Low Turnover Bone Disease) Bone Pain Fractures Low Bone Turnover Hypercalcemia Vascular Calcification

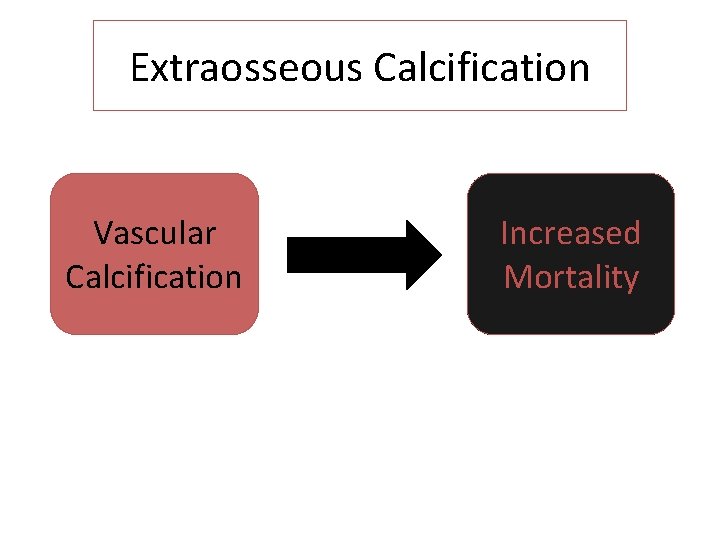
Extraosseous Calcification Vascular Calcification Increased Mortality
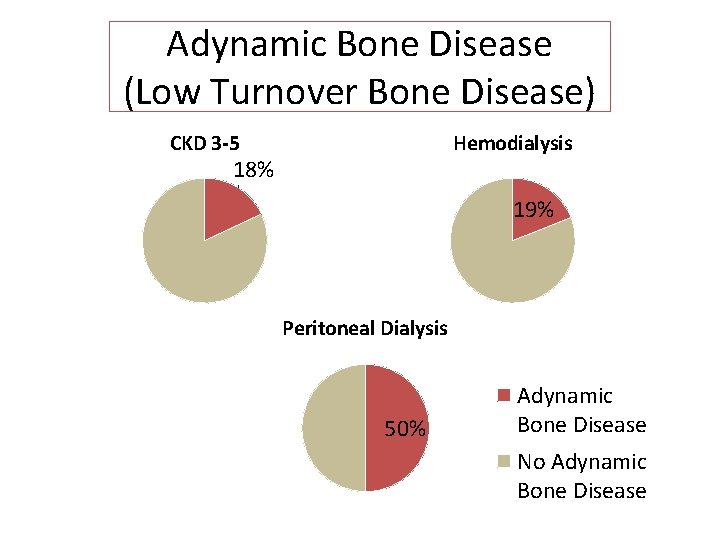
Adynamic Bone Disease (Low Turnover Bone Disease) CKD 3 -5 Hemodialysis 18% 19% Peritoneal Dialysis 50% Adynamic Bone Disease No Adynamic Bone Disease
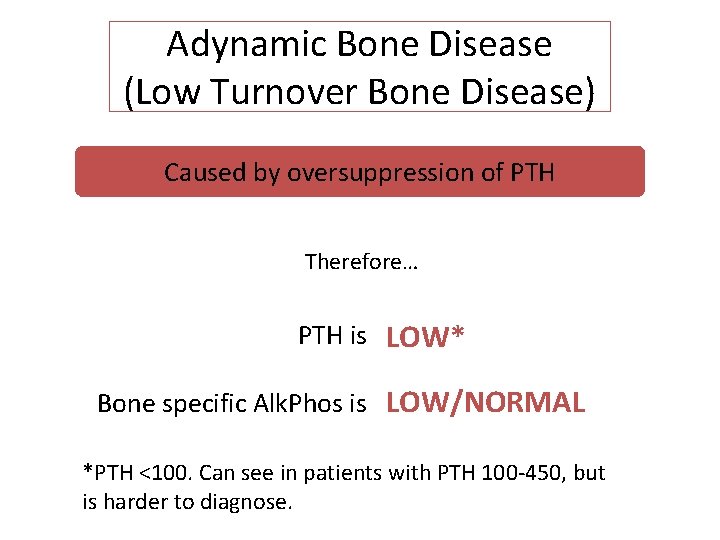
Adynamic Bone Disease (Low Turnover Bone Disease) Caused by oversuppression of PTH Therefore… PTH is LOW* Bone specific Alk. Phos is LOW/NORMAL *PTH <100. Can see in patients with PTH 100 -450, but is harder to diagnose.
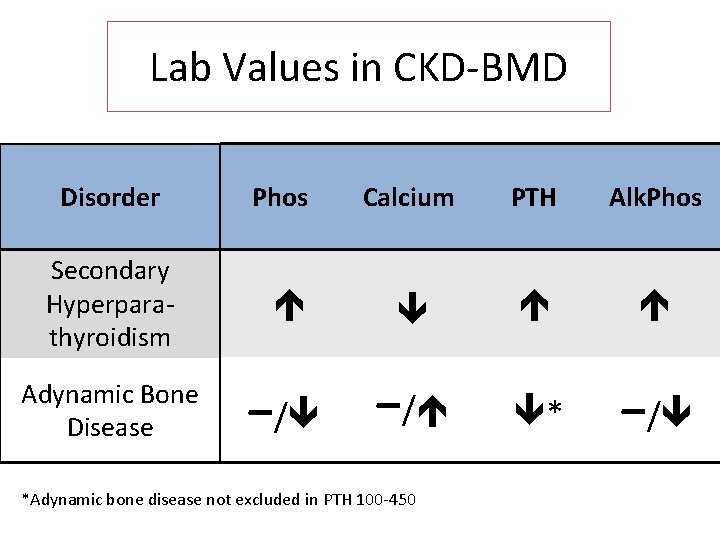
Lab Values in CKD-BMD Disorder Phos Calcium PTH Alk. Phos Secondary Hyperparathyroidism Adynamic Bone Disease −/ *Adynamic bone disease not excluded in PTH 100 -450
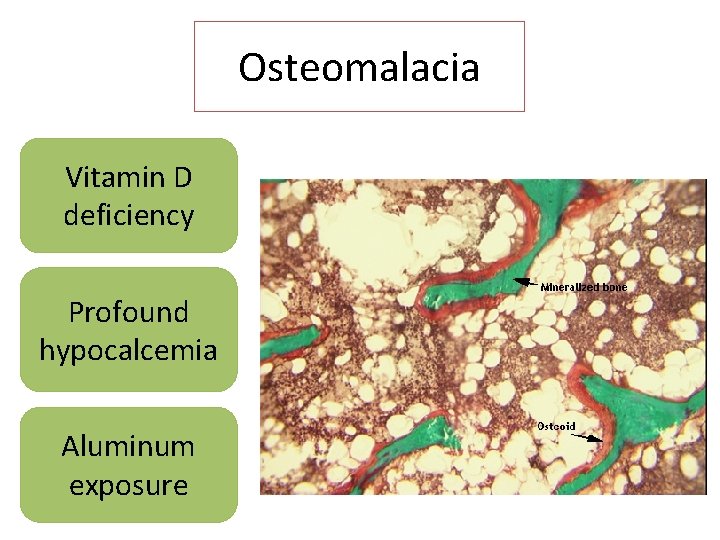
Osteomalacia Vitamin D deficiency Profound hypocalcemia Aluminum exposure
Mixed Osteodystrophy Osteomalacia High or low turnover bone disease
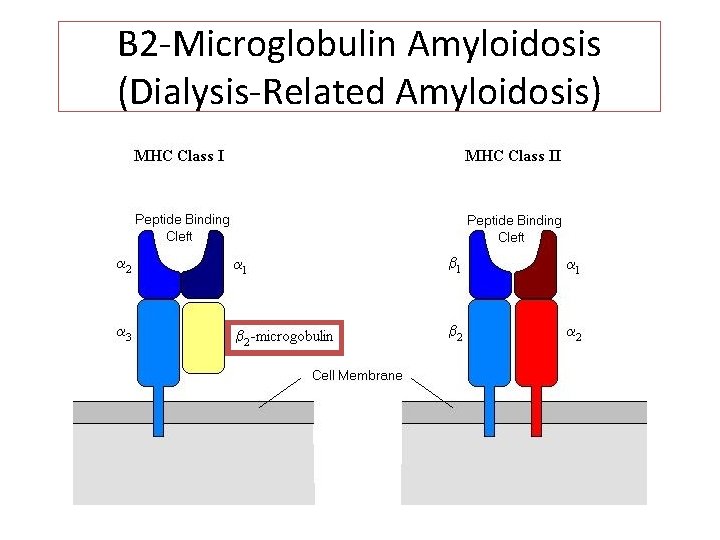
B 2 -Microglobulin Amyloidosis (Dialysis-Related Amyloidosis)
B 2 Microglobulin Amyloidosis (Dialysis-Related Amyloidosis)
MKSAP QUESTIONS
MKSAP Question 1 A 59 year-old woman is evaluated for a 2 -week history of right hip pain. She has chronic kidney disease treated with peritoneal dialysis. Medications are epoetin alfa, calcium acetate, calcitriol, and a multivitamin. She has no history of exposure to aluminum-containing medications. On physical examination, vital signs are normal. There is tenderness over the right lateral trochanter. Internal and external rotation of the hip elicit pain.
MKSAP Question 1 Laboratory studies: Phosphorus 5. 6 mg/d. L Calcium 10. 2 mg/d. L Alkaline phosphatase 86 U/L Intact PTH 21 pg/m. L 1, 25 -dihydroxyvitamin D 52 pg/m. L 25 -hydroxyvitamin D 15 ng/m. L
MKSAP Question 1 Plain radiograph of the right hip shows diffuse osteopenia. An area of lucency is seen along the medial aspect of the femoral neck on the right side consistent with a stress fracture.
MKSAP Question 1 Which of the following is most likely the cause of this patient’s bone disease? A. Adynamic bone disease B. B 2 -Microglobulin-associated amyloidosis C. Osteitis fibrosa cystica D. Osteomalacia
MKSAP Question 1 Osteopenia, fracture, bone pain, serum PTH level <100 pg/m. L, and normal Alk. Phos level are consistent with adynamic bone disease, which is a leading cause of bone disorders in patients with stage 5 CKD. Risk factors: advanced age, DM, poor nutrition, and oversuppression of PTH with therapeutic agents
MKSAP Question 1 This patient’s 1, 25 -dihydroxyvitamin D level >30 pg/m. L is consistent with repletion of vitamin D stores with calcitriol. The relatively low 25 hydroxyvitamin D level may be caused by reduced cutaneous synthesis and decreased dietary intake. Decreased hepatic 25 hydroxylation also may occur in patients with CKD.
MKSAP Question 1 Osteitis fibrosa cystica: hyperphosphatemia, hypocalcemia, and 1, 25 -vit. D deficiency -> stimulate PTH secretion -> increase bone turnover. Radiographic sclerosis and subperiosteal bone resorption, elevated PTH, elevated Alk. Phos
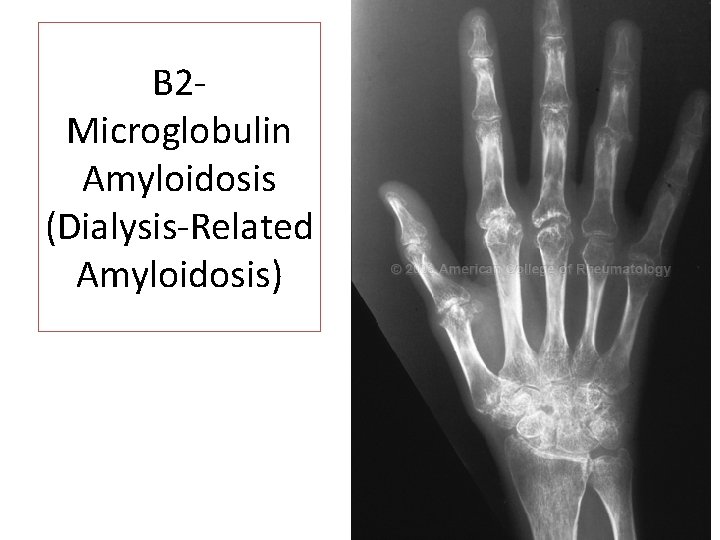
MKSAP Question 1 B 2 -microglobulin-associated amyloidosis: cystic bone lesion at the end of long bones that can enlarge over time, resulting in pathologic fractures Osteomalacia: uncommon. Usually after exposure to aluminum-containing phosphate binders. Usually have elevated serum PTH.
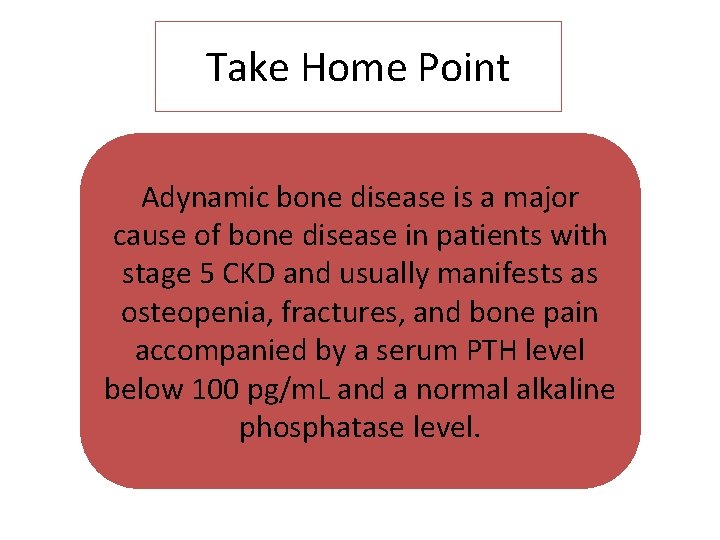
Take Home Point Adynamic bone disease is a major cause of bone disease in patients with stage 5 CKD and usually manifests as osteopenia, fractures, and bone pain accompanied by a serum PTH level below 100 pg/m. L and a normal alkaline phosphatase level.
MKSAP Question 2 A 33 year-old woman comes for follow up examination for a left fibula fracture due to a fall 1 week ago. She has hypertension and stage 5 CKD treated with home hemodialysis. Medications are lisinopril, sevelamer, epoetin alfa, paricalcitol, and kidney vitamins.
MKSAP Question 2 On physical examination, temperature is normal, blood pressure is 130/70 mm. Hg, pulse rate is 88/min, and respiration rate is 12/min. BMI is 29. Cardiopulmonary exam is normal. An arteriovenous fistula is present in the left forearm. Except for a cast on her left leg, musculoskeletal examination is normal and reveals no bone pain.
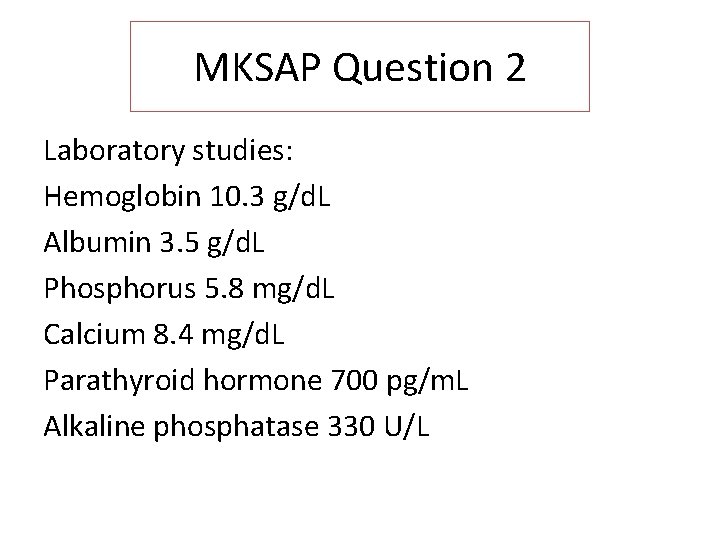
MKSAP Question 2 Laboratory studies: Hemoglobin 10. 3 g/d. L Albumin 3. 5 g/d. L Phosphorus 5. 8 mg/d. L Calcium 8. 4 mg/d. L Parathyroid hormone 700 pg/m. L Alkaline phosphatase 330 U/L
MKSAP Question 2 Which of the following is the most likely cause of this patient’s bone disease? A. Adynamic bone disease B. Avascular necrosis C. Osteoporosis D. Secondary hyperparathyroidism
MKSAP Question 2 CKD is associated with progressive alterations in mineral and bone metabolism that can cause bone disease. In patients with ESRD, the kidney’s inability to excrete phosphorus leads to hyperphosphatemia. Loss of kidney function also is associated with 1, 25 -vit. D deficiency. Hyperphosphatemia along with decreased 1, 25 vit. D levels result in hypocalcemia, which leads to direct stimulation of PTH secretion.
MKSAP Question 2 Furthermore, decreased 1, 25 -vit. D levels cause increased production of PTH. Therefore, bone disease due to secondary hyperparathyroidism, the most common bone pathologic finding seen in patients with ESRD, develops. This patient’s hyperphosphatemia, hypocalcemia, and elevated serum PTH and Alk. Phos are consistent with secondary hyperparathyroidism.
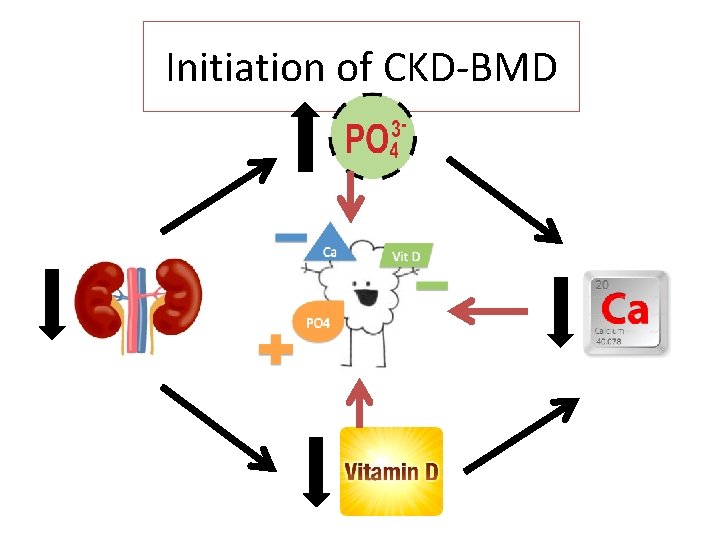
Initiation of CKD-BMD
MKSAP Question 2 Adynamic bone disease: hypoparathyroidism caused by excess vitamin D intake and/or calcium loading Osteoporosis: low bone mass, associated with reduced bone strength and increased risk of fractures. Does not affect the concentrations of serum calcium, phosphorus, or Alk. Phos
MKSAP Question 2 Avascular necrosis: transient or permanent lack of blood supply to bone, causing death of bone and bone marrow infarction that results in mechanical failure. Typically present with chronic bone pain and not fracture.
Take Home Point Bone disease due to secondary hyperparathyroidism commonly occurs in patients with ESRD and may be associated with elevated serum PTH and alkaline phosphatase levels, hyperphosphatemia, and hypocalcemia.
MONITORING & TREATMENT
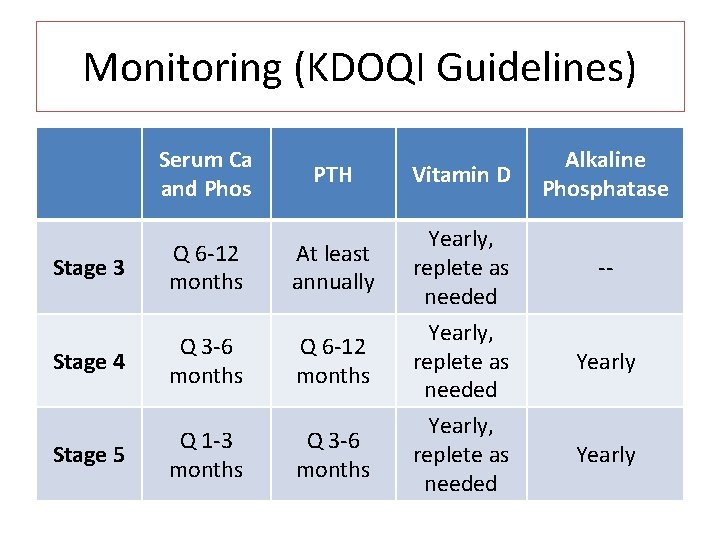
Monitoring (KDOQI Guidelines) Serum Ca and Phos Stage 3 Q 6 -12 months PTH Vitamin D Alkaline Phosphatase At least annually Yearly, replete as needed -- Stage 4 Q 3 -6 months Q 6 -12 months Stage 5 Q 1 -3 months Q 3 -6 months Yearly, replete as needed Yearly
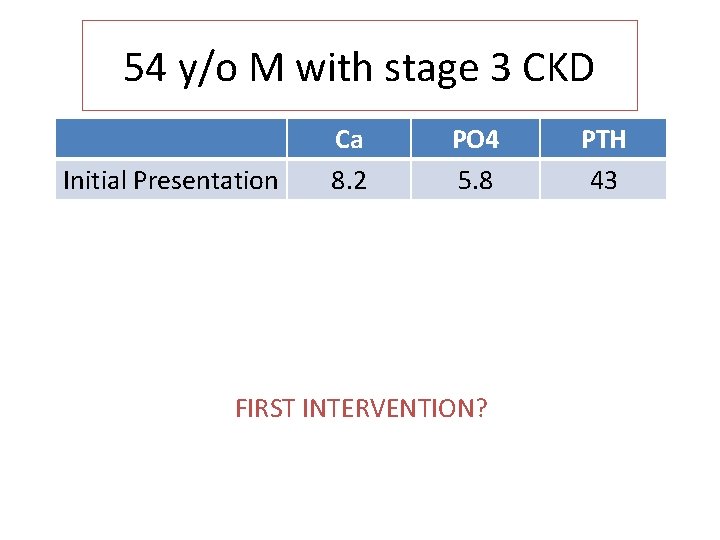
54 y/o M with stage 3 CKD Initial Presentation Ca 8. 2 PO 4 5. 8 FIRST INTERVENTION? PTH 43
Phosphate Restriction
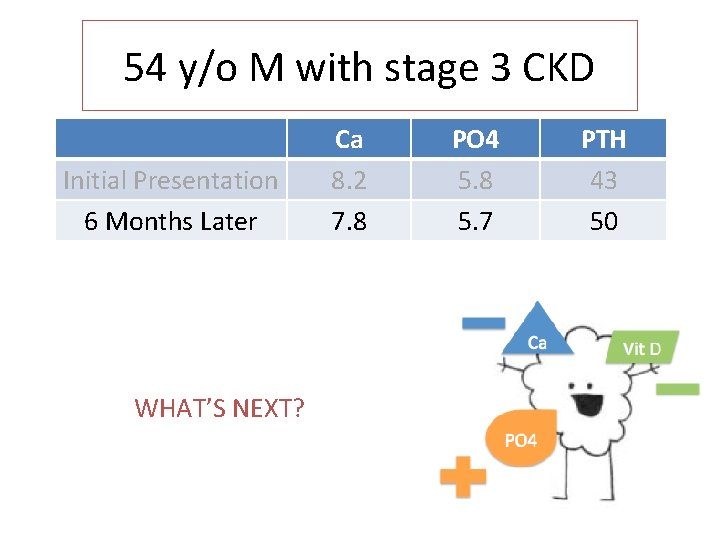
54 y/o M with stage 3 CKD Initial Presentation 6 Months Later WHAT’S NEXT? Ca 8. 2 7. 8 PO 4 5. 8 5. 7 PTH 43 50
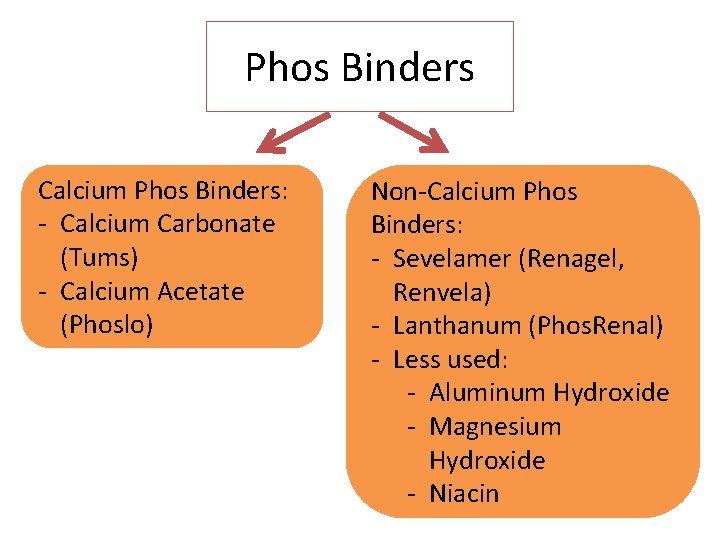
Phos Binders Calcium Phos Binders: - Calcium Carbonate (Tums) - Calcium Acetate (Phoslo) Non-Calcium Phos Binders: - Sevelamer (Renagel, Renvela) - Lanthanum (Phos. Renal) - Less used: - Aluminum Hydroxide - Magnesium Hydroxide - Niacin
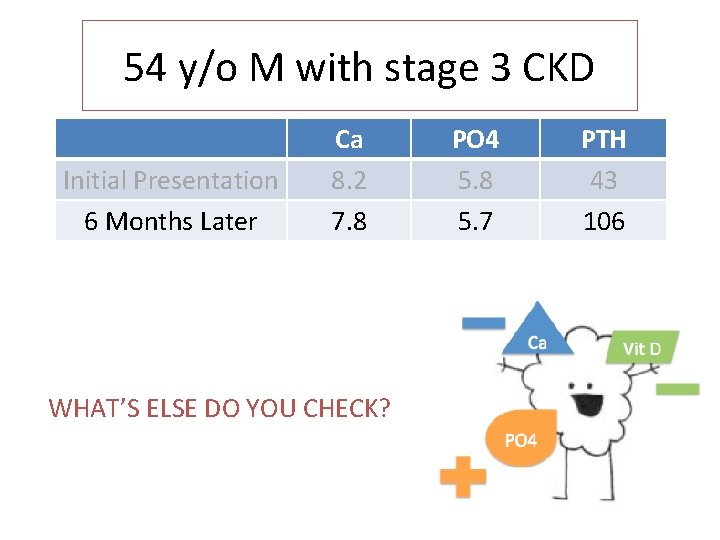
54 y/o M with stage 3 CKD Initial Presentation 6 Months Later Ca 8. 2 7. 8 WHAT’S ELSE DO YOU CHECK? PO 4 5. 8 5. 7 PTH 43 106
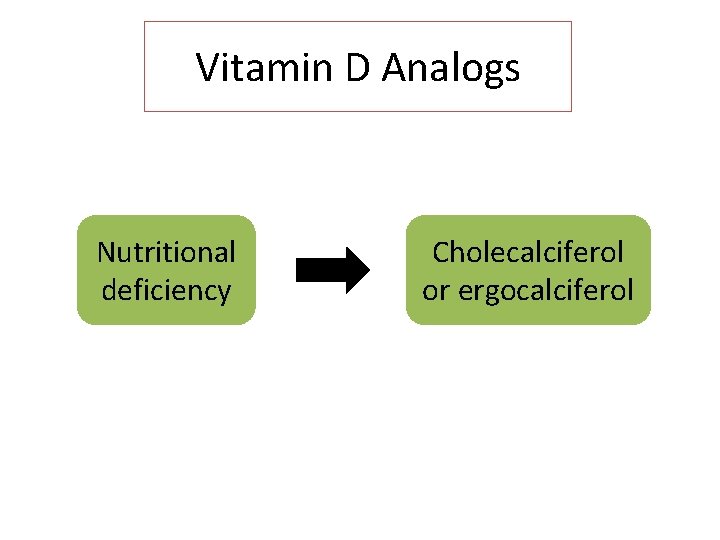
Vitamin D Analogs Nutritional deficiency Cholecalciferol or ergocalciferol
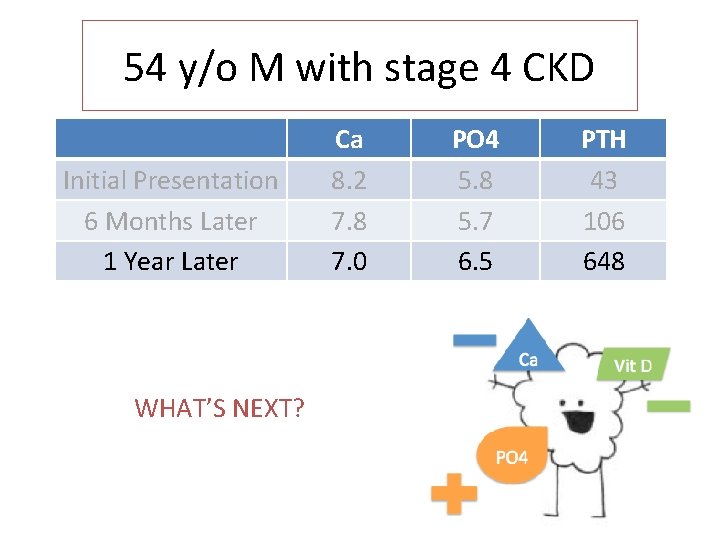
54 y/o M with stage 4 CKD Initial Presentation 6 Months Later 1 Year Later WHAT’S NEXT? Ca 8. 2 7. 8 7. 0 PO 4 5. 8 5. 7 6. 5 PTH 43 106 648
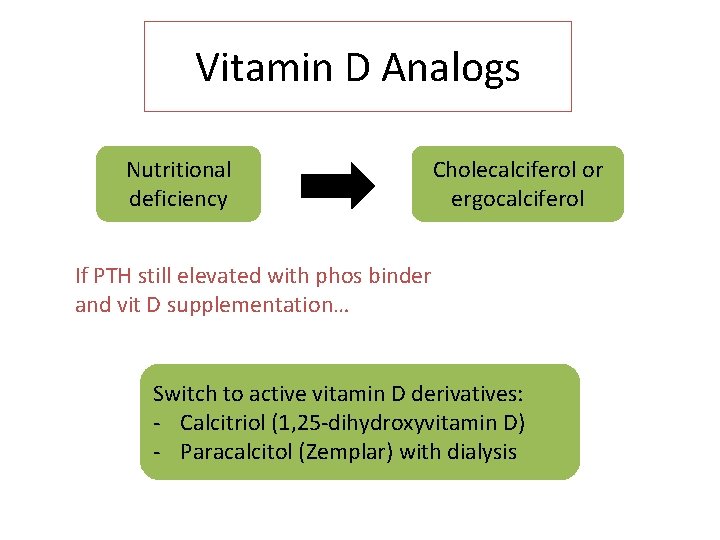
Vitamin D Analogs Nutritional deficiency Cholecalciferol or ergocalciferol If PTH still elevated with phos binder and vit D supplementation… Switch to active vitamin D derivatives: - Calcitriol (1, 25 -dihydroxyvitamin D) - Paracalcitol (Zemplar) with dialysis
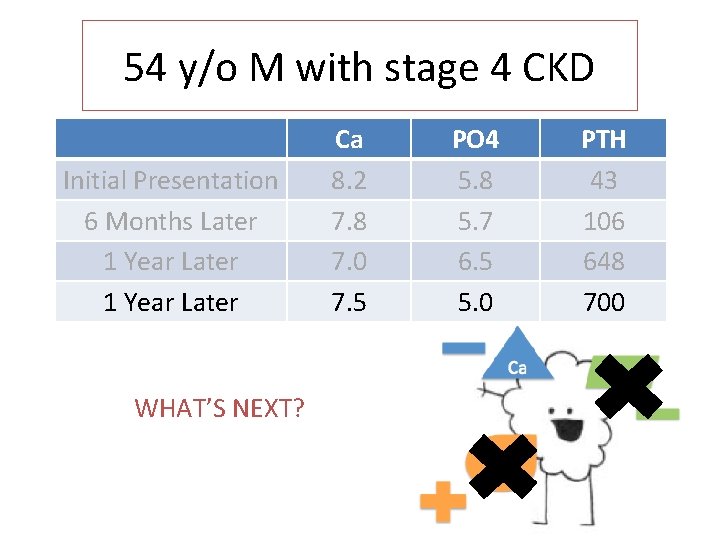
54 y/o M with stage 4 CKD Initial Presentation 6 Months Later 1 Year Later WHAT’S NEXT? Ca 8. 2 7. 8 7. 0 7. 5 PO 4 5. 8 5. 7 6. 5 5. 0 PTH 43 106 648 700
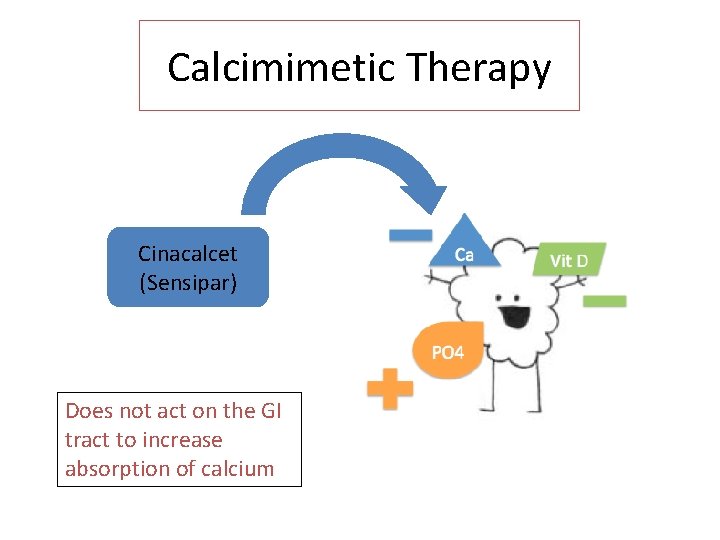
Calcimimetic Therapy Cinacalcet (Sensipar) Does not act on the GI tract to increase absorption of calcium
Parathyroidectomy
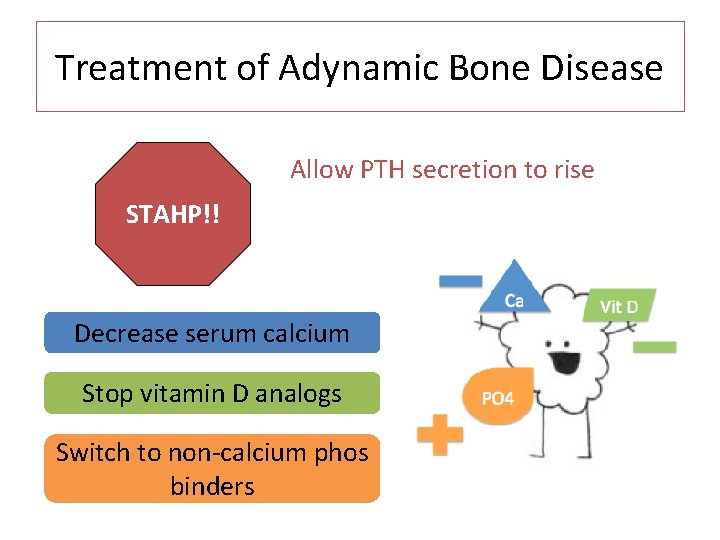
Treatment of Adynamic Bone Disease Allow PTH secretion to rise STAHP!! Decrease serum calcium Stop vitamin D analogs Switch to non-calcium phos binders
Learning Objectives Describe the mechanisms by which bone and mineral disorders develop in CKD Differentiate secondary hyperparathyroidism, adynamic bone disease, and other bone/mineral disorders by lab values and clinical presentation List 3 different medications for the treatment of hyperparathyroidism in CKD and how they differ
Take Home Points You (yes, you!) can reason through how CKD-BMD happens Secondary hyperparathyroidism is the end result of the natural progression of the abnormalities set in motion by hyperphosphatemia Adynamic Bone disease is common, and it is caused by oversuppression of PTH Phos binders, vitamin D analogs, and calcium analogs are all used to treat hyperparathyroidism
QUESTIONS?
- Slides: 72