BOLD FORWARD CDICoding Reconciliation Collaboration CDICoding Partnership Karen

BOLD. FORWARD. CDI-Coding Reconciliation & Collaboration CDI-Coding Partnership Karen O’Lessker, MBA, RHIA Proprietary and confidential. Do not distribute.
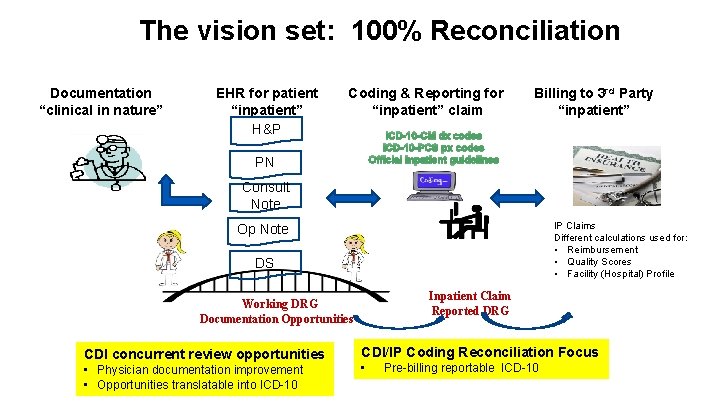
The vision set: 100% Reconciliation Documentation “clinical in nature” EHR for patient “inpatient” H&P Coding & Reporting for “inpatient” claim Billing to 3 rd Party “inpatient” ICD-10 -CM dx codes ICD-10 -PCS px codes Official Inpatient guidelines PN Consult Note IP Claims Different calculations used for: • Reimbursement • Quality Scores • Facility (Hospital) Profile Op Note DS Inpatient Claim Reported DRG Working DRG Documentation Opportunities CDI concurrent review opportunities • Physician documentation improvement • Opportunities translatable into ICD-10 CDI/IP Coding Reconciliation Focus • Pre-billing reportable ICD-10
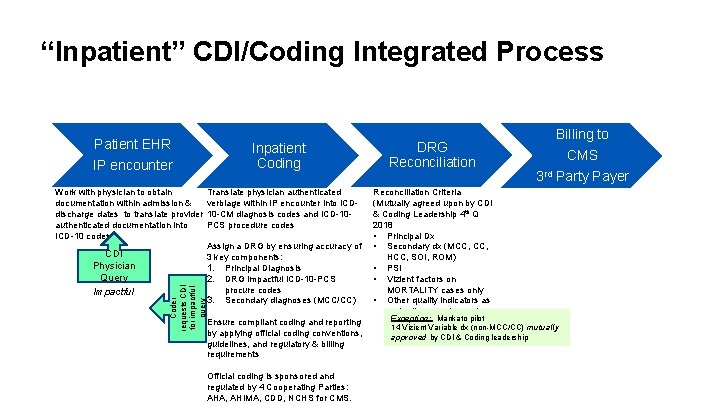
“Inpatient” CDI/Coding Integrated Process Patient EHR IP encounter CDI Physician Query Impactful Coder requests CDI for impactful query Work with physician to obtain documentation within admission & discharge dates to translate provider authenticated documentation into ICD-10 codes Inpatient Coding Translate physician authenticated verbiage within IP encounter into ICD 10 -CM diagnosis codes and ICD-10 PCS procedure codes Assign a DRG by ensuring accuracy of 3 key components: 1. Principal Diagnosis 2. DRG impactful ICD-10 -PCS procure codes 3. Secondary diagnoses (MCC/CC) Ensure compliant coding and reporting by applying official coding conventions, guidelines, and regulatory & billing requirements Official coding is sponsored and regulated by 4 Cooperating Parties: AHA, AHIMA, CDD, NCHS for CMS. DRG Reconciliation Billing to CMS 3 rd Party Payer Reconciliation Criteria (Mutually agreed upon by CDI & Coding Leadership 4 th Q 2018 • Principal Dx • Secondary dx (MCC, HCC, SOI, ROM) • PSI • Vizient factors on MORTALITY cases only • Other quality indicators as mutually agreed upon by Exception: Mankato pilot CDI physicians, CDI & 14 Vizient Variable dx (non-MCC/CC) mutually Coding leadership approved by CDI & Coding leadership
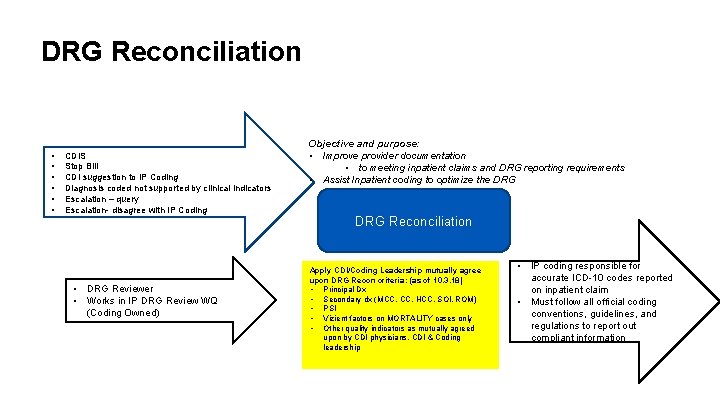
DRG Reconciliation • • • CDIS Stop Bill CDI suggestion to IP Coding Diagnosis coded not supported by clinical indicators Escalation – query Escalation- disagree with IP Coding • DRG Reviewer • Works in IP DRG Review WQ (Coding Owned) Objective and purpose: • Improve provider documentation • to meeting inpatient claims and DRG reporting requirements • Assist Inpatient coding to optimize the DRG Reconciliation Apply CDI/Coding Leadership mutually agree upon DRG Recon criteria: (as of 10. 3. 18) • Principal Dx • Secondary dx (MCC, HCC, SOI, ROM) • PSI • Vizient factors on MORTALITY cases only • Other quality indicators as mutually agreed upon by CDI physicians, CDI & Coding leadership • IP coding responsible for accurate ICD-10 codes reported on inpatient claim • Must follow all official coding conventions, guidelines, and regulations to report out compliant information
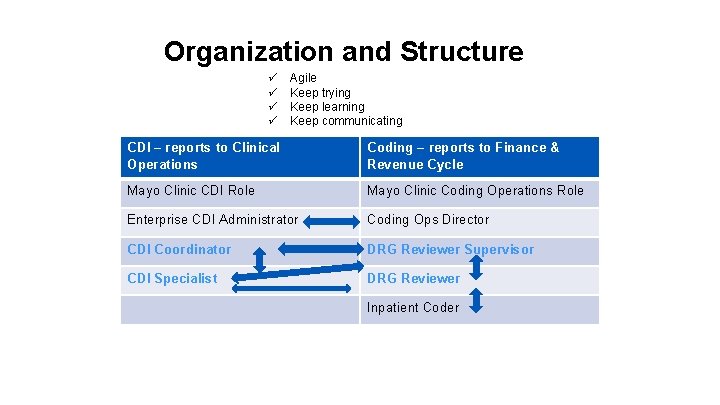
Organization and Structure ü ü Agile Keep trying Keep learning Keep communicating CDI – reports to Clinical Operations Coding – reports to Finance & Revenue Cycle Mayo Clinic CDI Role Mayo Clinic Coding Operations Role Enterprise CDI Administrator Coding Ops Director CDI Coordinator DRG Reviewer Supervisor CDI Specialist DRG Reviewer Inpatient Coder
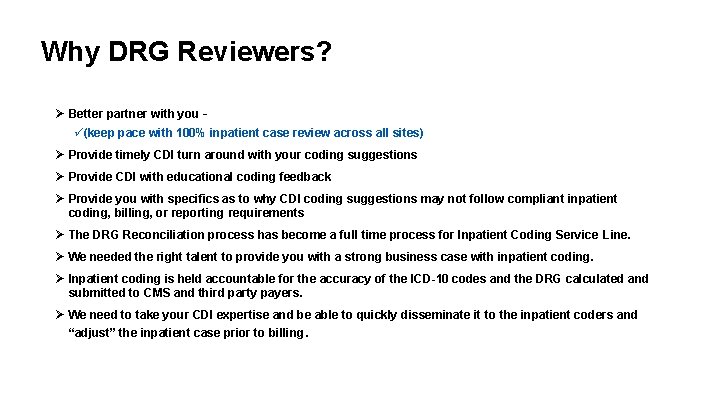
Why DRG Reviewers? Ø Better partner with you – ü(keep pace with 100% inpatient case review across all sites) Ø Provide timely CDI turn around with your coding suggestions Ø Provide CDI with educational coding feedback Ø Provide you with specifics as to why CDI coding suggestions may not follow compliant inpatient coding, billing, or reporting requirements Ø The DRG Reconciliation process has become a full time process for Inpatient Coding Service Line. Ø We needed the right talent to provide you with a strong business case with inpatient coding. Ø Inpatient coding is held accountable for the accuracy of the ICD-10 codes and the DRG calculated and submitted to CMS and third party payers. Ø We need to take your CDI expertise and be able to quickly disseminate it to the inpatient coders and “adjust” the inpatient case prior to billing.
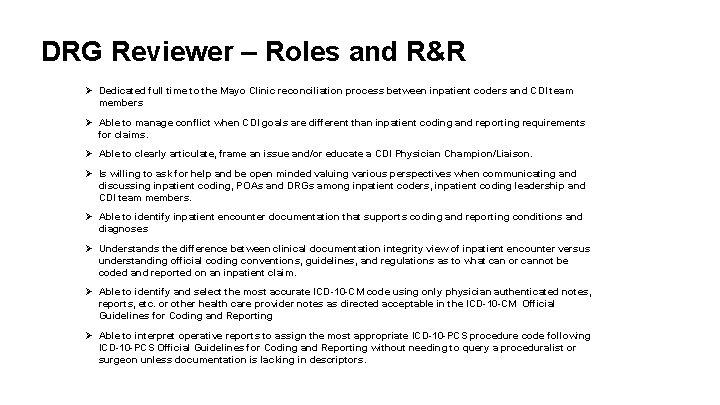
DRG Reviewer – Roles and R&R Ø Dedicated full time to the Mayo Clinic reconciliation process between inpatient coders and CDI team members Ø Able to manage conflict when CDI goals are different than inpatient coding and reporting requirements for claims. Ø Able to clearly articulate, frame an issue and/or educate a CDI Physician Champion/Liaison. Ø Is willing to ask for help and be open minded valuing various perspectives when communicating and discussing inpatient coding, POAs and DRGs among inpatient coders, inpatient coding leadership and CDI team members. Ø Able to identify inpatient encounter documentation that supports coding and reporting conditions and diagnoses Ø Understands the difference between clinical documentation integrity view of inpatient encounter versus understanding official coding conventions, guidelines, and regulations as to what can or cannot be coded and reported on an inpatient claim. Ø Able to identify and select the most accurate ICD-10 -CM code using only physician authenticated notes, reports, etc. or other health care provider notes as directed acceptable in the ICD-10 -CM Official Guidelines for Coding and Reporting Ø Able to interpret operative reports to assign the most appropriate ICD-10 -PCS procedure code following ICD-10 -PCS Official Guidelines for Coding and Reporting without needing to query a proceduralist or surgeon unless documentation is lacking in descriptors.
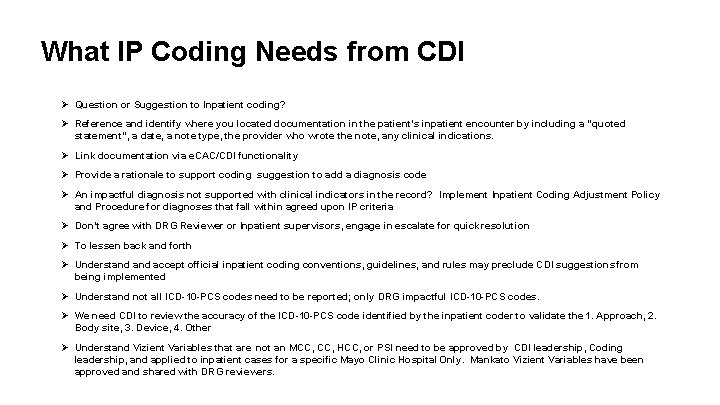
What IP Coding Needs from CDI Ø Question or Suggestion to Inpatient coding? Ø Reference and identify where you located documentation in the patient’s inpatient encounter by including a “quoted statement”, a date, a note type, the provider who wrote the note, any clinical indications. Ø Link documentation via e. CAC/CDI functionality Ø Provide a rationale to support coding suggestion to add a diagnosis code Ø An impactful diagnosis not supported with clinical indicators in the record? Implement Inpatient Coding Adjustment Policy and Procedure for diagnoses that fall within agreed upon IP criteria Ø Don’t agree with DRG Reviewer or Inpatient supervisors, engage in escalate for quick resolution Ø To lessen back and forth Ø Understand accept official inpatient coding conventions, guidelines, and rules may preclude CDI suggestions from being implemented Ø Understand not all ICD-10 -PCS codes need to be reported; only DRG impactful ICD-10 -PCS codes. Ø We need CDI to review the accuracy of the ICD-10 -PCS code identified by the inpatient coder to validate the 1. Approach, 2. Body site, 3. Device, 4. Other Ø Understand Vizient Variables that are not an MCC, HCC, or PSI need to be approved by CDI leadership, Coding leadership, and applied to inpatient cases for a specific Mayo Clinic Hospital Only. Mankato Vizient Variables have been approved and shared with DRG reviewers.

Thank you Proprietary and confidential. Do not distribute.
- Slides: 9