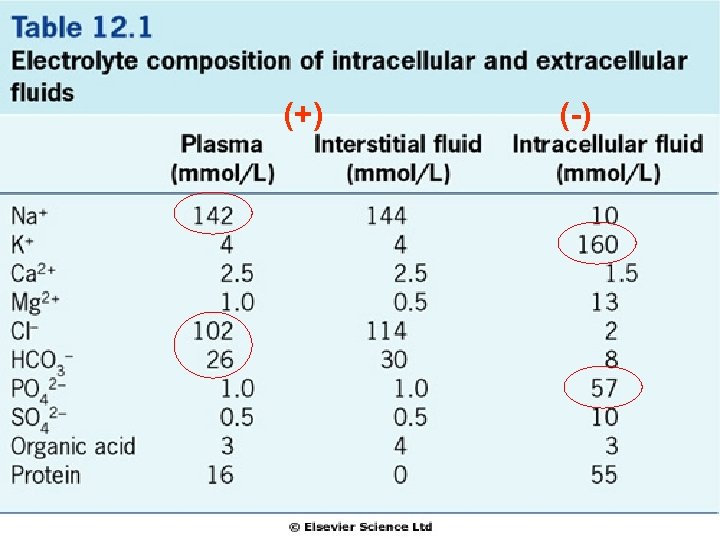
BODY WATER DISTRIBUTION Total body water 55 60
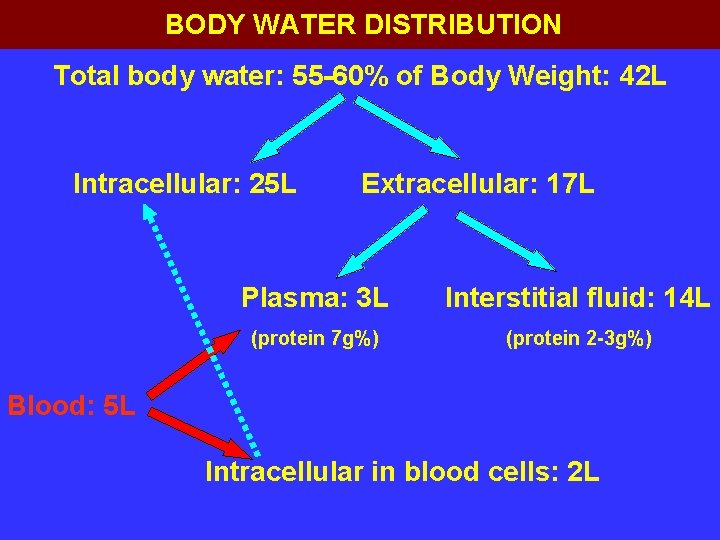
BODY WATER DISTRIBUTION Total body water: 55 -60% of Body Weight: 42 L Intracellular: 25 L Extracellular: 17 L Plasma: 3 L Interstitial fluid: 14 L (protein 7 g%) (protein 2 -3 g%) Blood: 5 L Intracellular in blood cells: 2 L

2100 m. L 350 m. L 100 m. L 1400 m. L 100 m. L

![ΩΣΜΩΤΙΚΟΤΗΤΑ ΠΛΑΣΜΑΤΟΣ Plasma Osmolality= [Na+]osm + [Glucose]osm + [Ουρία]osm Posm= 2 x plasma[Na+] + ΩΣΜΩΤΙΚΟΤΗΤΑ ΠΛΑΣΜΑΤΟΣ Plasma Osmolality= [Na+]osm + [Glucose]osm + [Ουρία]osm Posm= 2 x plasma[Na+] +](http://slidetodoc.com/presentation_image_h/16137f1195624bc46659a1b8657b10d5/image-10.jpg)
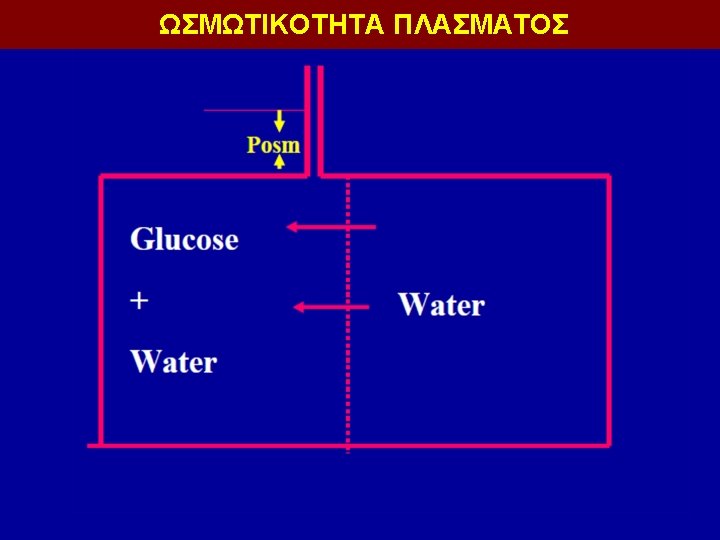
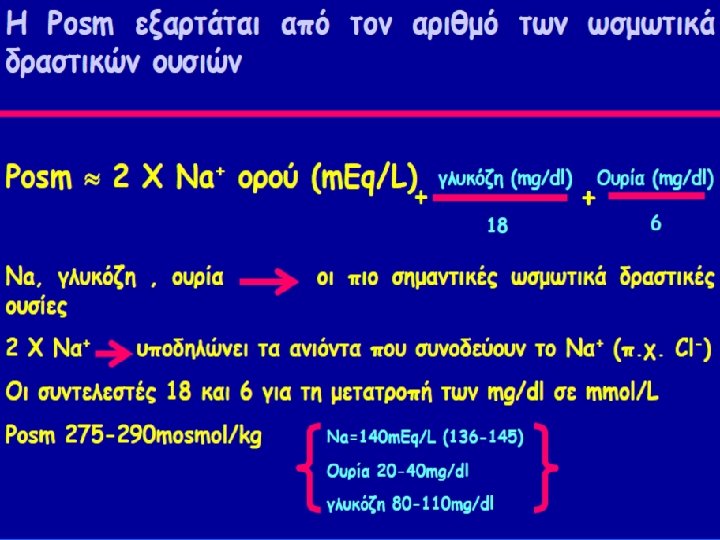
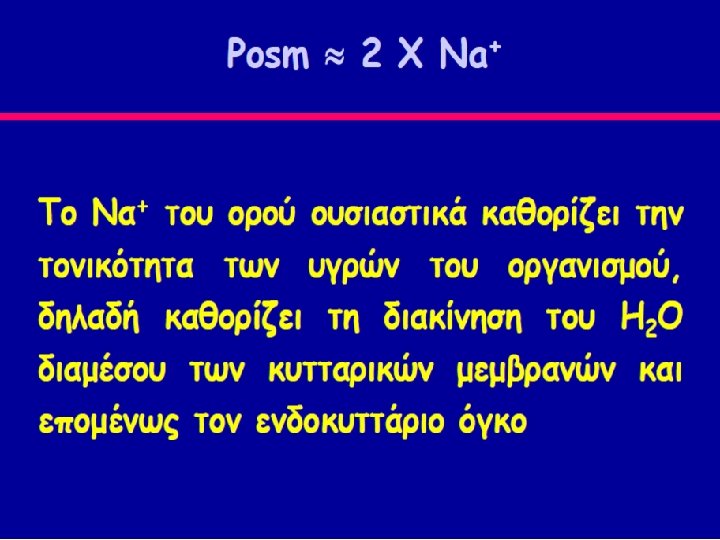
ΩΣΜΩΤΙΚΟΤΗΤΑ ΠΛΑΣΜΑΤΟΣ Plasma Osmolality= [Na+]osm + [Glucose]osm + [Ουρία]osm Posm= 2 x plasma[Na+] + [Glucose] mg/d. L x 10 / MW + [Ουρία] mg/d. Lx 10 / MW Posm = 2 [Na+] meq/L + Glucose mg/d. L + Ουρία mg/d. L 18 6 Plasma Osmolality : 275 -290 mosm/kg Effective Posm = 2 [Na+] meq/L + Glucose mg/d. L (Tonicity) 18
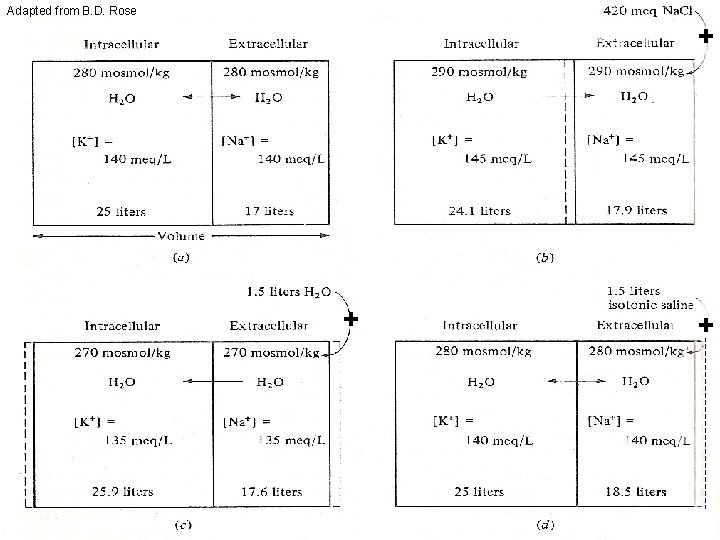
Adapted from B. D. Rose + + +
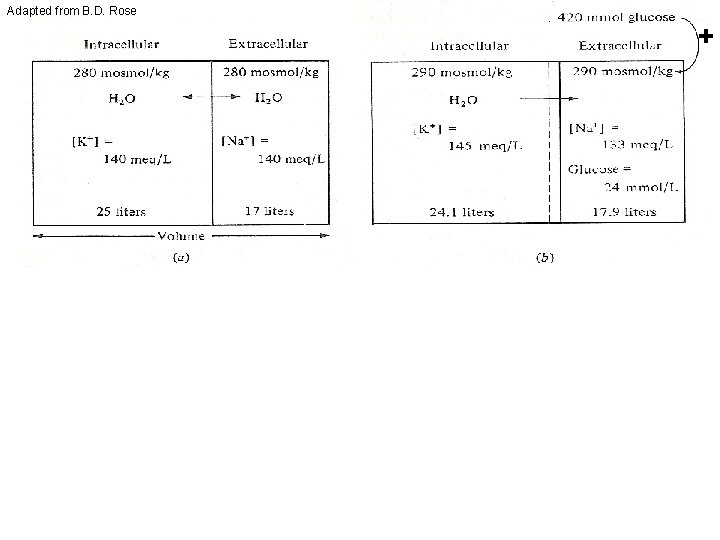
Adapted from B. D. Rose + 133 meq/L Glucose= 24 mmol/L + +

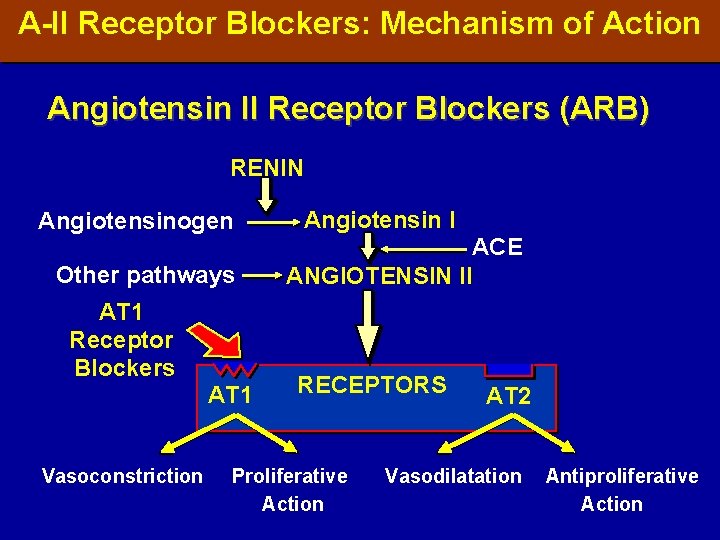
A-II Receptor Blockers: Mechanism of Action Angiotensin II Receptor Blockers (ARB) RENIN Angiotensinogen Other pathways AT 1 Receptor Blockers AT 1 Vasoconstriction Angiotensin I ACE ANGIOTENSIN II RECEPTORS Proliferative Action AT 2 Vasodilatation Antiproliferative Action
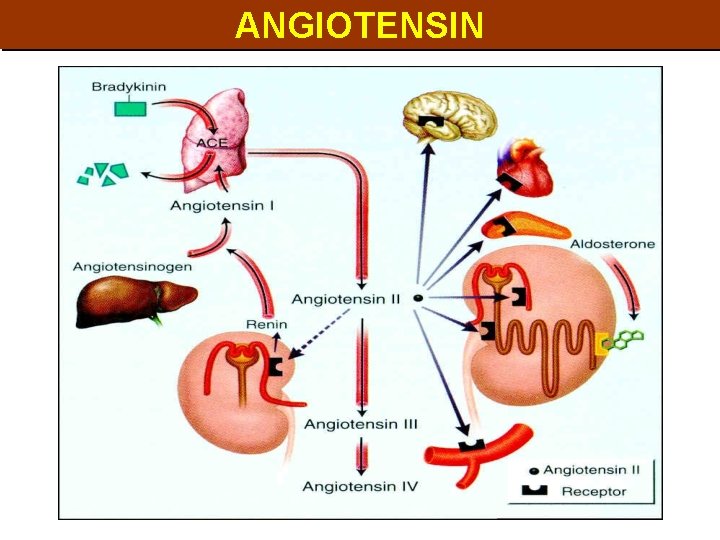
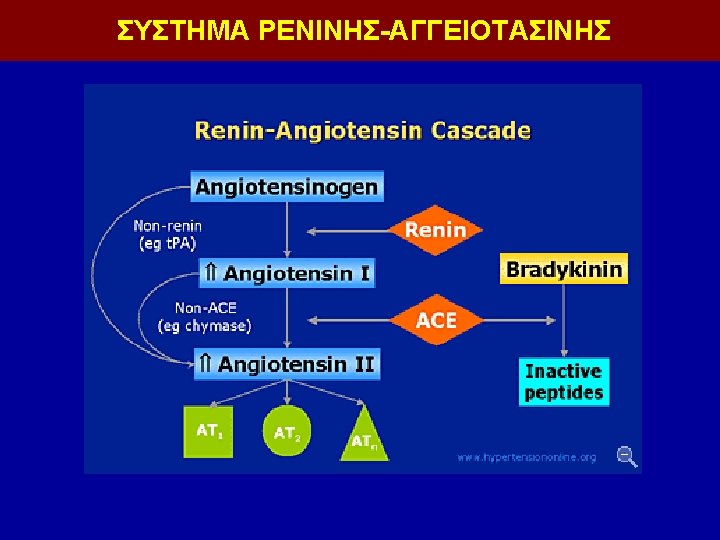
ANGIOTENSIN

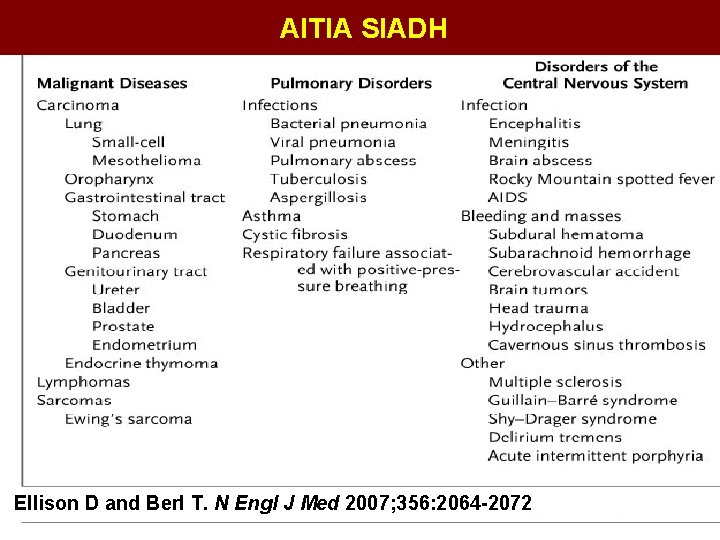
ΑΙΤΙΑ SIADH Ellison D and Berl T. N Engl J Med 2007; 356: 2064 -2072
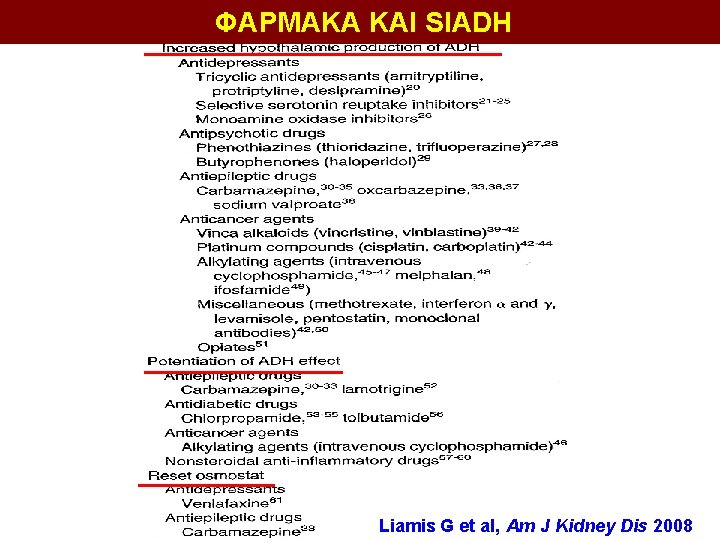
ΦΑΡΜΑΚΑ ΚΑΙ SIADH Liamis G et al, Am J Kidney Dis 2008
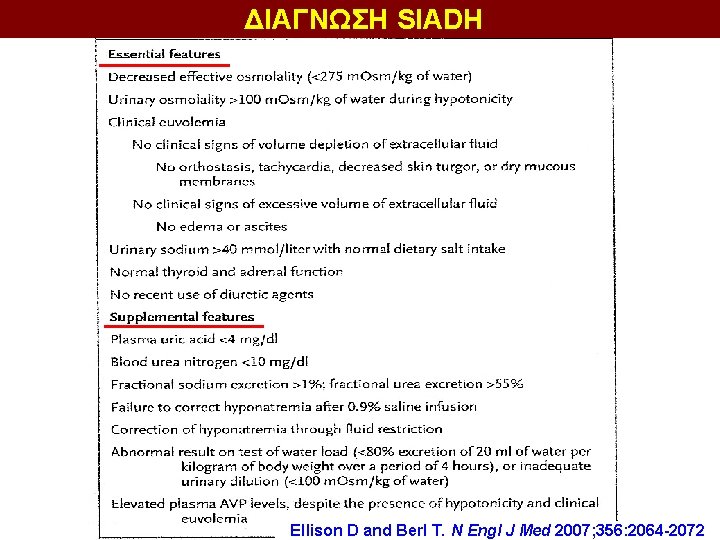
ΔΙΑΓΝΩΣΗ SIADH Ellison D and Berl T. N Engl J Med 2007; 356: 2064 -2072


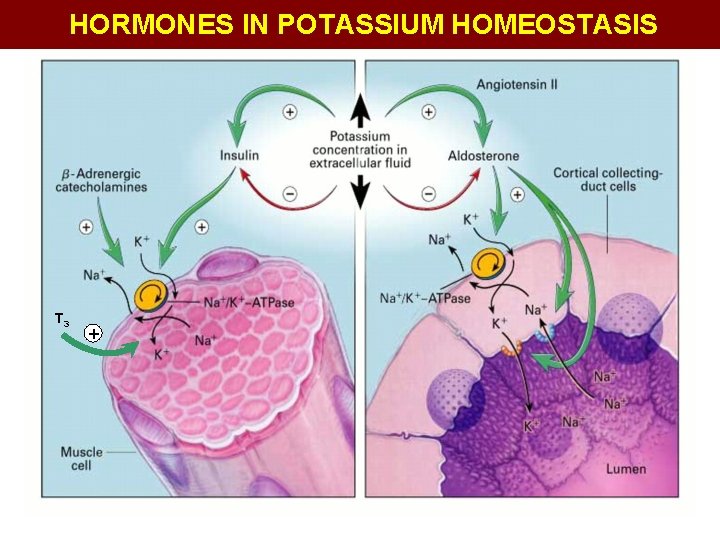
HORMONES IN POTASSIUM HOMEOSTASIS T 3 +
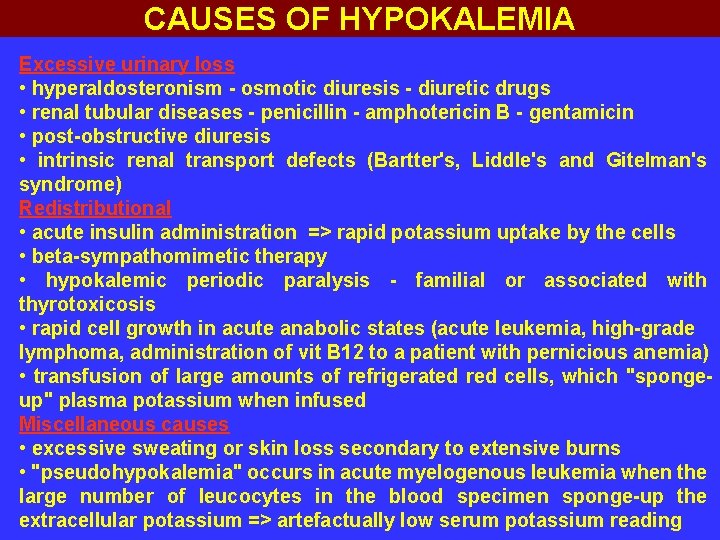
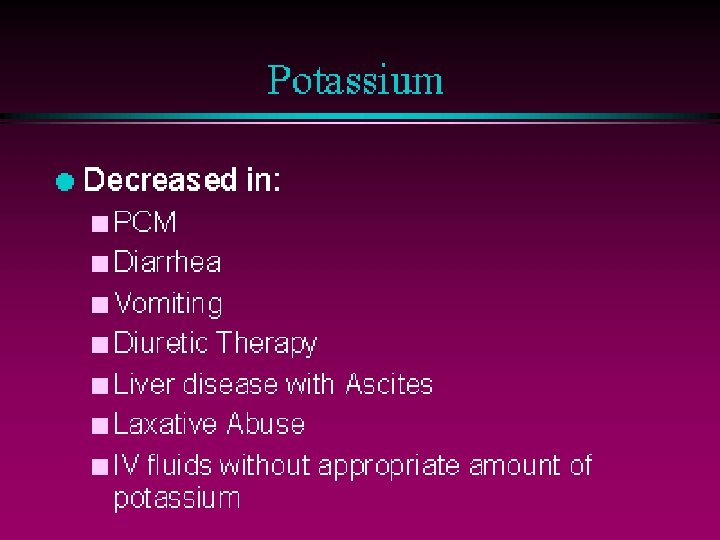
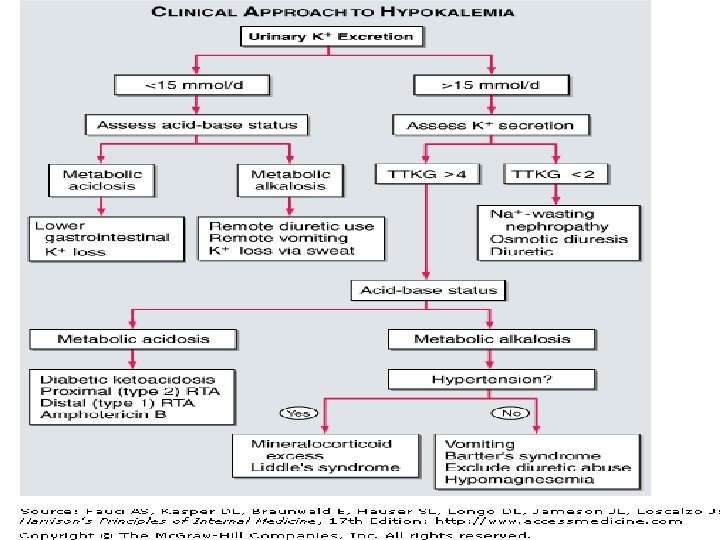
CAUSES OF HYPOKALEMIA Excessive urinary loss • hyperaldosteronism - osmotic diuresis - diuretic drugs • renal tubular diseases - penicillin - amphotericin B - gentamicin • post-obstructive diuresis • intrinsic renal transport defects (Bartter's, Liddle's and Gitelman's syndrome) Redistributional • acute insulin administration => rapid potassium uptake by the cells • beta-sympathomimetic therapy • hypokalemic periodic paralysis - familial or associated with thyrotoxicosis • rapid cell growth in acute anabolic states (acute leukemia, high-grade lymphoma, administration of vit B 12 to a patient with pernicious anemia) • transfusion of large amounts of refrigerated red cells, which "spongeup" plasma potassium when infused Miscellaneous causes • excessive sweating or skin loss secondary to extensive burns • "pseudohypokalemia" occurs in acute myelogenous leukemia when the large number of leucocytes in the blood specimen sponge-up the extracellular potassium => artefactually low serum potassium reading

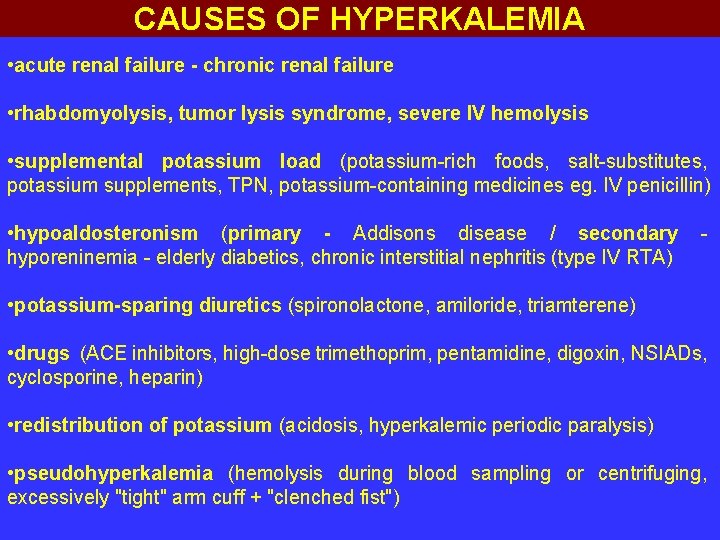
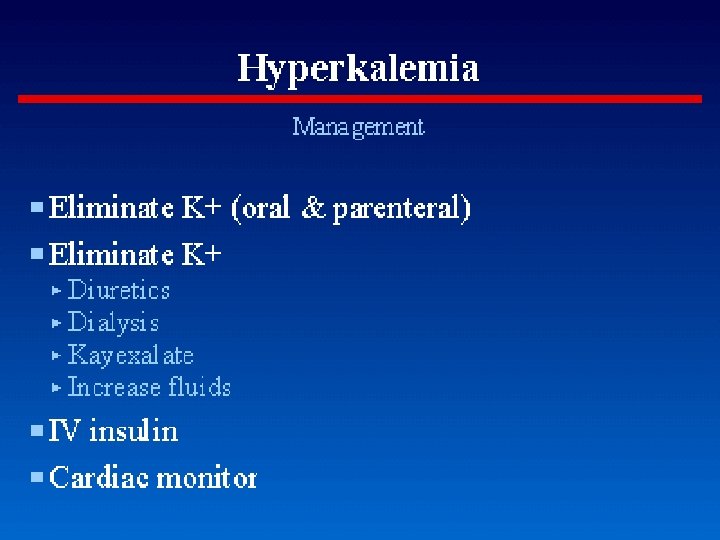
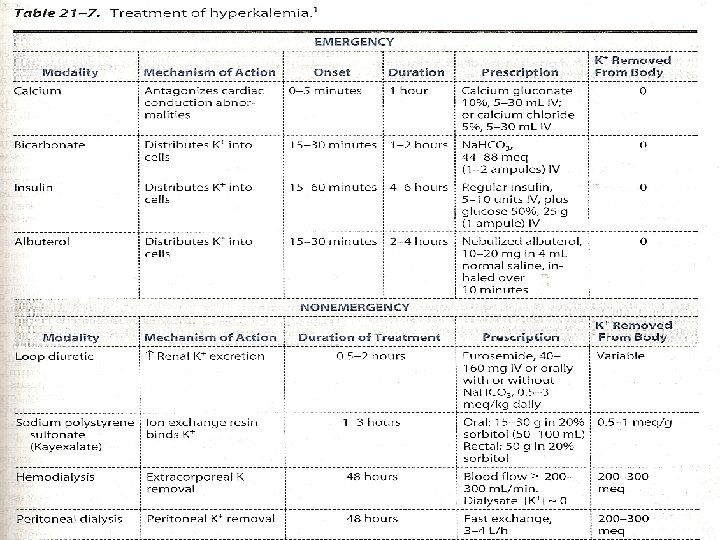
CAUSES OF HYPERKALEMIA • acute renal failure - chronic renal failure • rhabdomyolysis, tumor lysis syndrome, severe IV hemolysis • supplemental potassium load (potassium-rich foods, salt-substitutes, potassium supplements, TPN, potassium-containing medicines eg. IV penicillin) • hypoaldosteronism (primary - Addisons disease / secondary hyporeninemia - elderly diabetics, chronic interstitial nephritis (type IV RTA) - • potassium-sparing diuretics (spironolactone, amiloride, triamterene) • drugs (ACE inhibitors, high-dose trimethoprim, pentamidine, digoxin, NSIADs, cyclosporine, heparin) • redistribution of potassium (acidosis, hyperkalemic periodic paralysis) • pseudohyperkalemia (hemolysis during blood sampling or centrifuging, excessively "tight" arm cuff + "clenched fist")
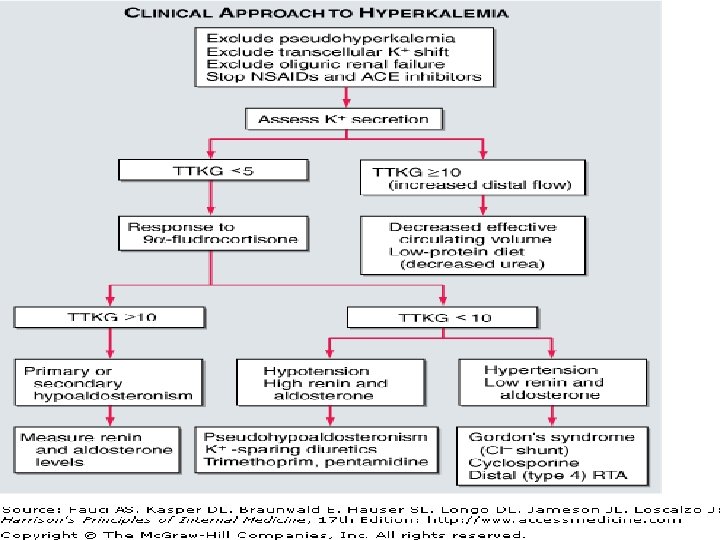
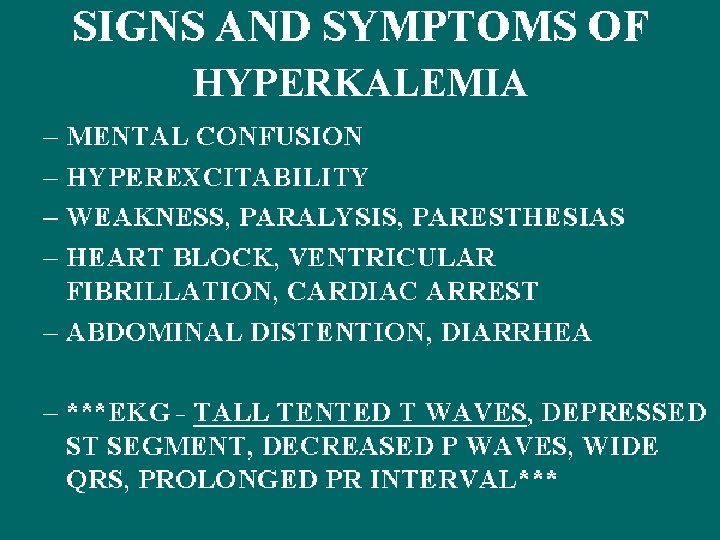
HYPERKALEMIA
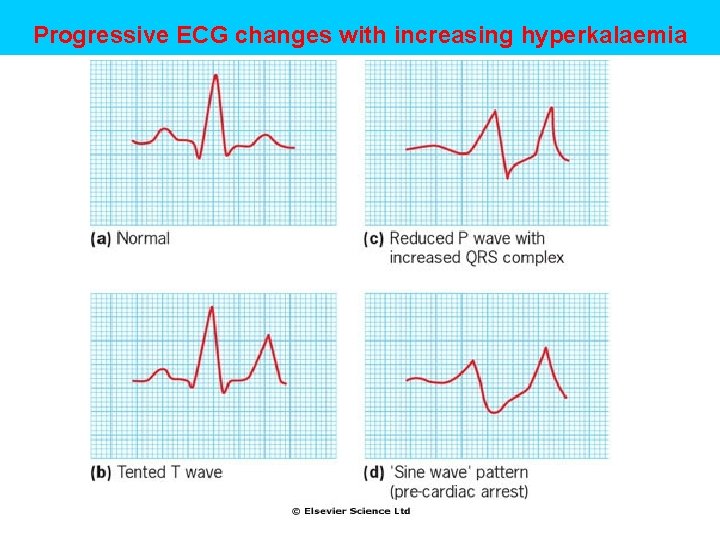
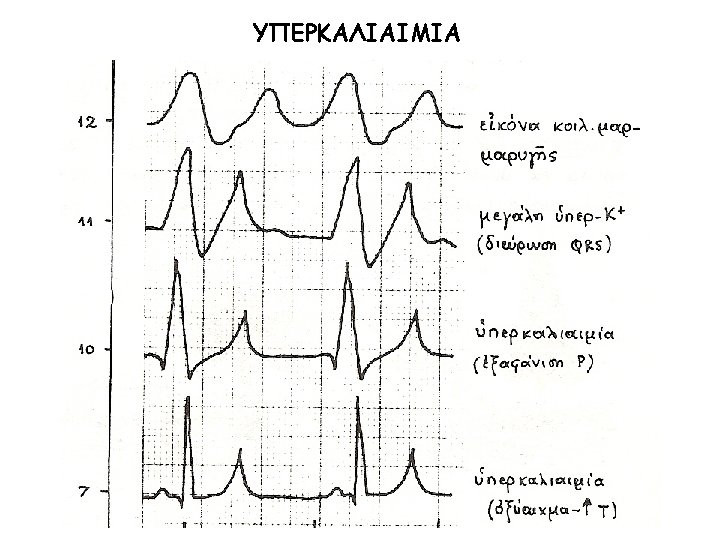
Progressive ECG changes with increasing hyperkalaemia
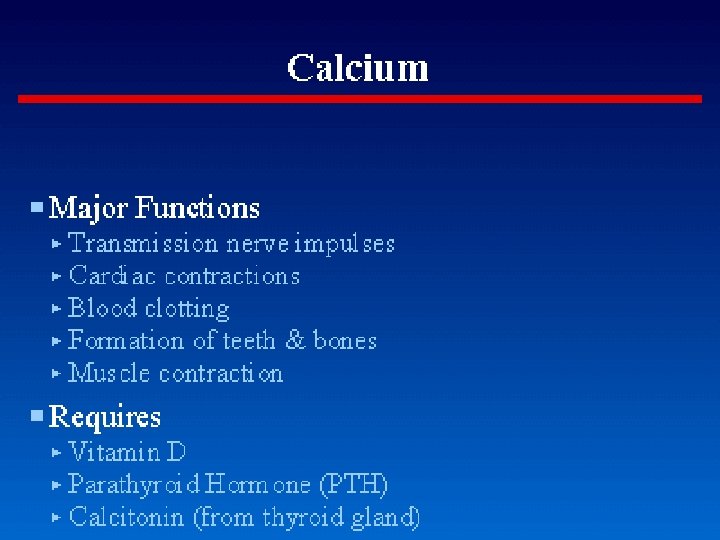
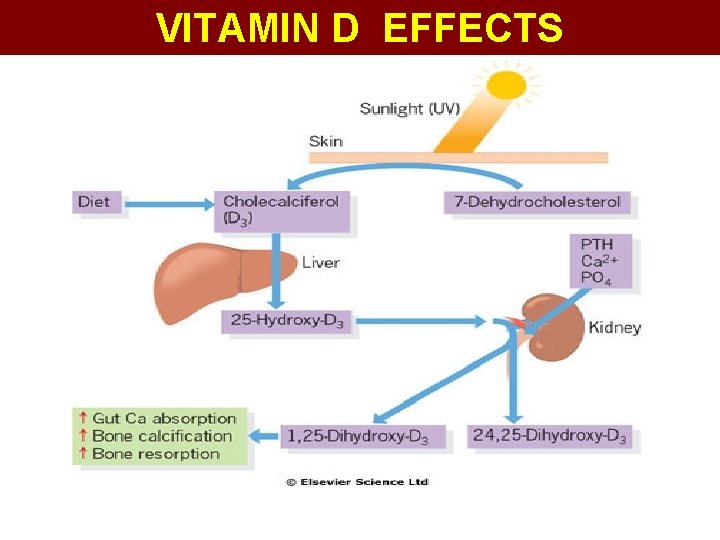
VITAMIN D EFFECTS
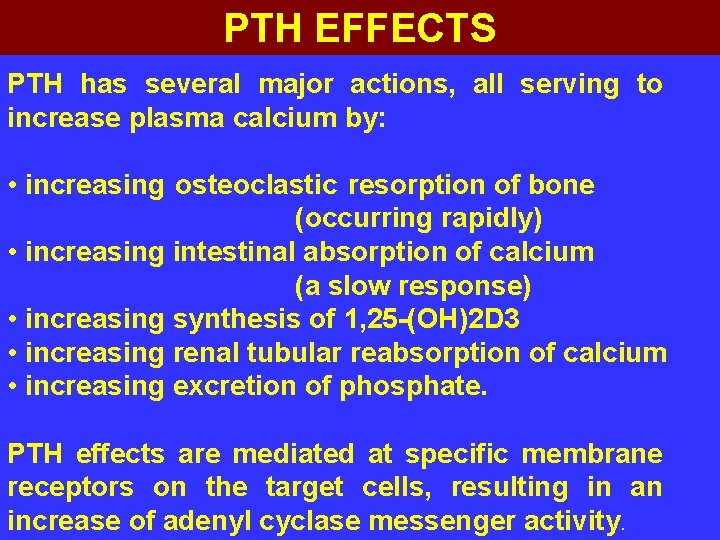
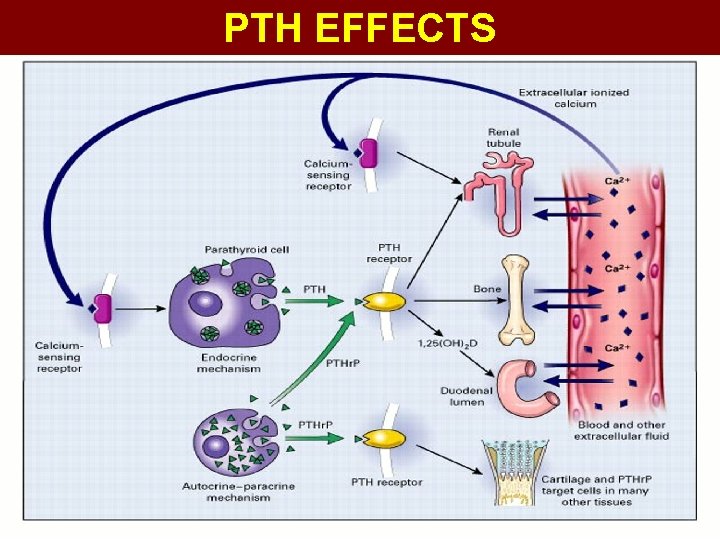
PTH EFFECTS PTH has several major actions, all serving to increase plasma calcium by: • increasing osteoclastic resorption of bone (occurring rapidly) • increasing intestinal absorption of calcium (a slow response) • increasing synthesis of 1, 25 -(OH)2 D 3 • increasing renal tubular reabsorption of calcium • increasing excretion of phosphate. PTH effects are mediated at specific membrane receptors on the target cells, resulting in an increase of adenyl cyclase messenger activity.
PTH EFFECTS
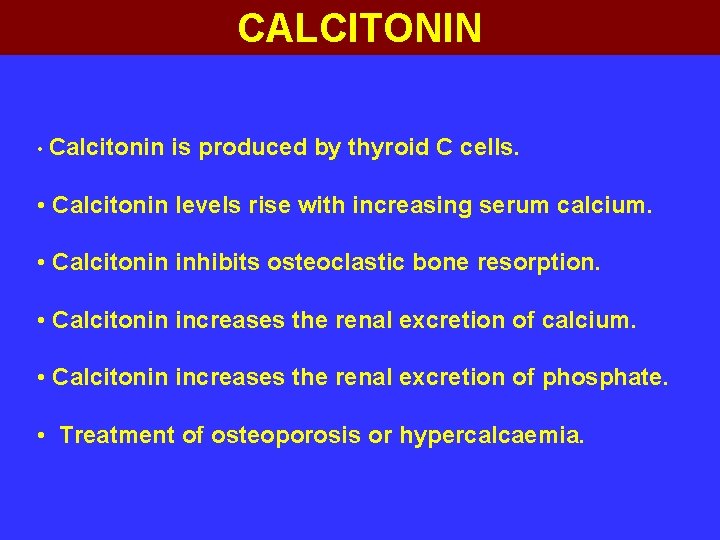
CALCITONIN • Calcitonin is produced by thyroid C cells. • Calcitonin levels rise with increasing serum calcium. • Calcitonin inhibits osteoclastic bone resorption. • Calcitonin increases the renal excretion of calcium. • Calcitonin increases the renal excretion of phosphate. • Treatment of osteoporosis or hypercalcaemia.
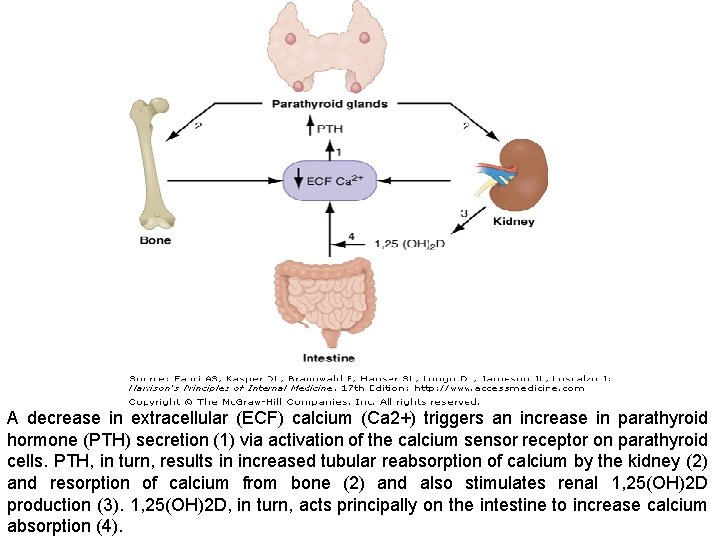
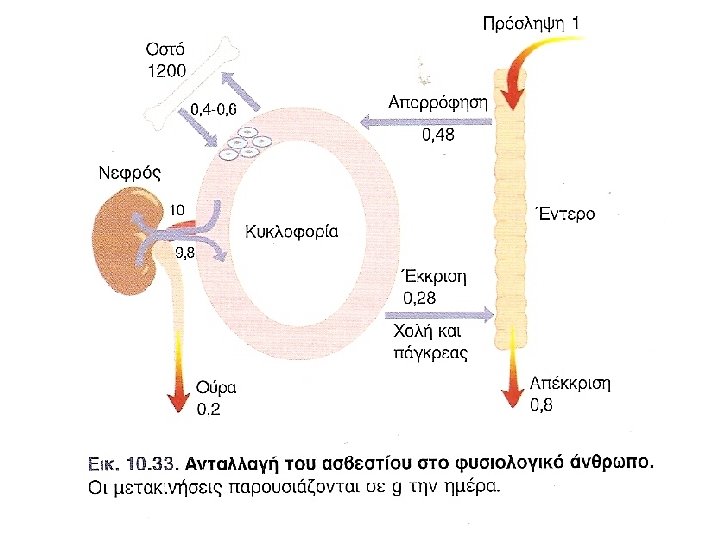
A decrease in extracellular (ECF) calcium (Ca 2+) triggers an increase in parathyroid hormone (PTH) secretion (1) via activation of the calcium sensor receptor on parathyroid cells. PTH, in turn, results in increased tubular reabsorption of calcium by the kidney (2) and resorption of calcium from bone (2) and also stimulates renal 1, 25(OH)2 D production (3). 1, 25(OH)2 D, in turn, acts principally on the intestine to increase calcium absorption (4).
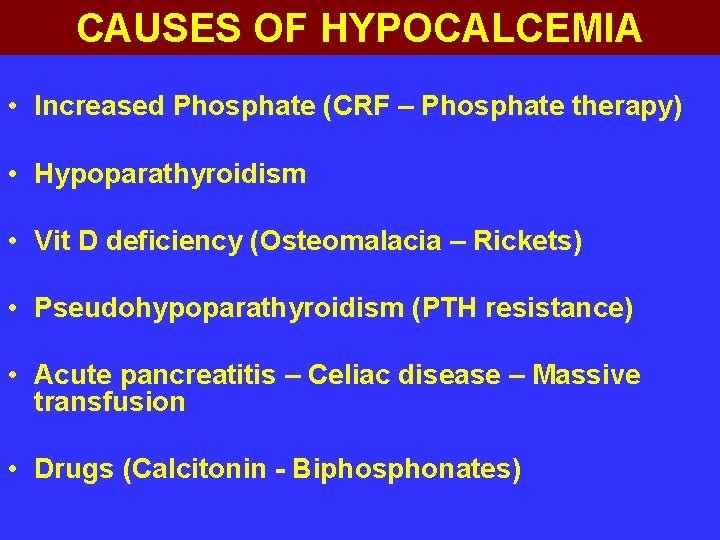
CAUSES OF HYPOCALCEMIA • Increased Phosphate (CRF – Phosphate therapy) • Hypoparathyroidism • Vit D deficiency (Osteomalacia – Rickets) • Pseudohypoparathyroidism (PTH resistance) • Acute pancreatitis – Celiac disease – Massive transfusion • Drugs (Calcitonin - Biphosphonates)

CAUSES OF HYPERCALCEMIA • PTH excess (Primary – Ectopic) • Malignancy (Myeloma – PTHr. P secretion) • Vit D excess (Granuloma – Lymphoma) • Excessive calcium intake • Thyrotoxicosis – Addison’s disease • Drugs (Thiazides – Lithium – Vit A) • Long term immobility
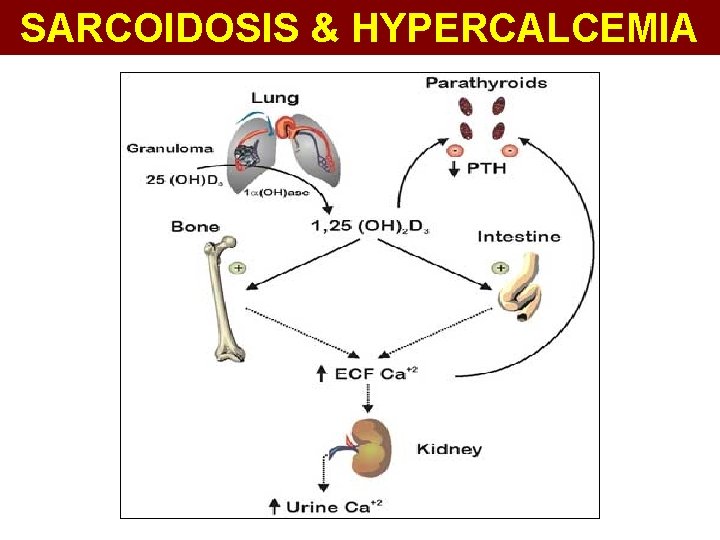
SARCOIDOSIS & HYPERCALCEMIA
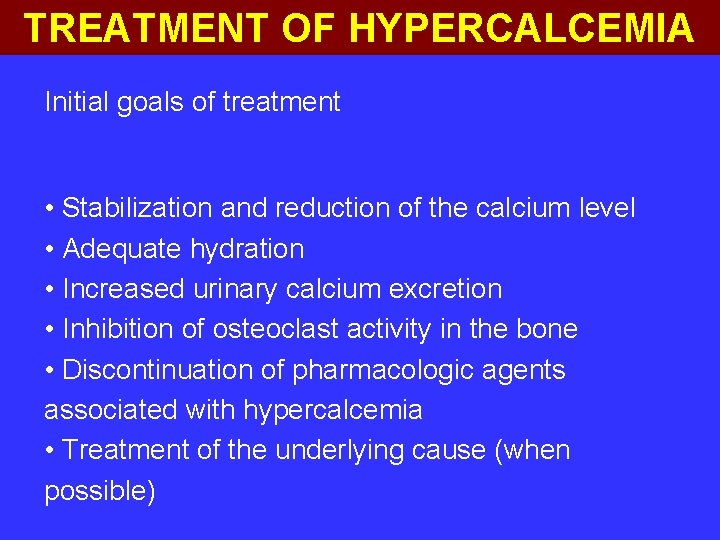
TREATMENT OF HYPERCALCEMIA Initial goals of treatment • Stabilization and reduction of the calcium level • Adequate hydration • Increased urinary calcium excretion • Inhibition of osteoclast activity in the bone • Discontinuation of pharmacologic agents associated with hypercalcemia • Treatment of the underlying cause (when possible)
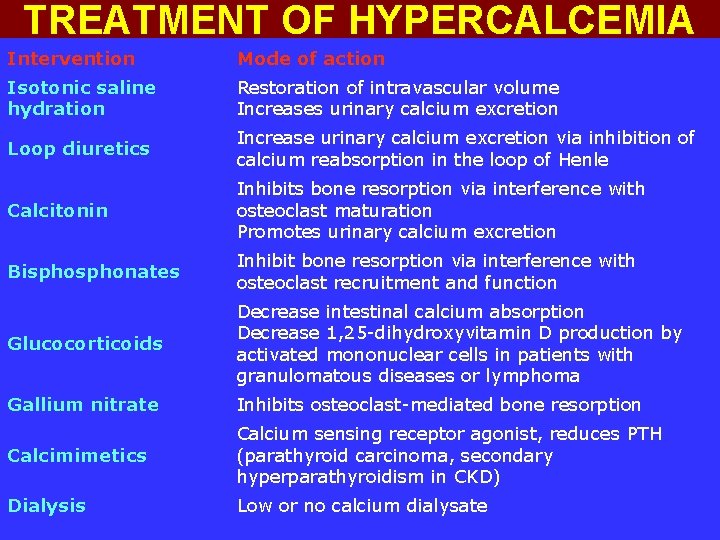
TREATMENT OF HYPERCALCEMIA Intervention Mode of action Isotonic saline hydration Restoration of intravascular volume Increases urinary calcium excretion Loop diuretics Increase urinary calcium excretion via inhibition of calcium reabsorption in the loop of Henle Calcitonin Inhibits bone resorption via interference with osteoclast maturation Promotes urinary calcium excretion Bisphonates Inhibit bone resorption via interference with osteoclast recruitment and function Glucocorticoids Decrease intestinal calcium absorption Decrease 1, 25 -dihydroxyvitamin D production by activated mononuclear cells in patients with granulomatous diseases or lymphoma Gallium nitrate Inhibits osteoclast-mediated bone resorption Calcimimetics Calcium sensing receptor agonist, reduces PTH (parathyroid carcinoma, secondary hyperparathyroidism in CKD) Dialysis Low or no calcium dialysate
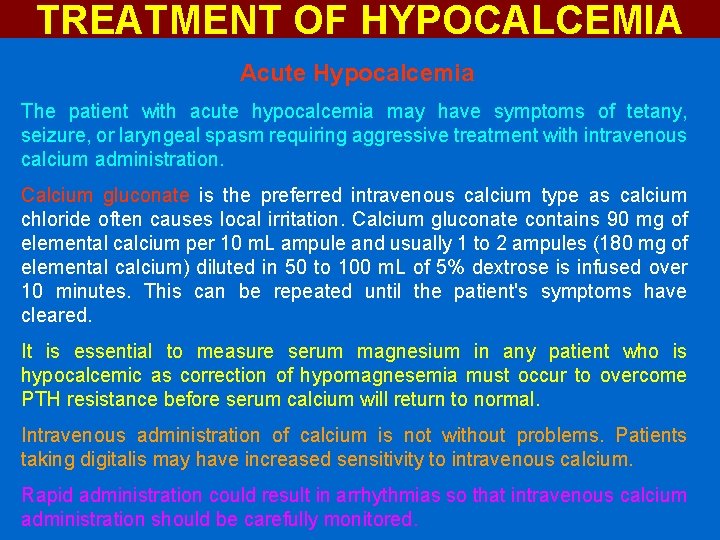
TREATMENT OF HYPOCALCEMIA Acute Hypocalcemia The patient with acute hypocalcemia may have symptoms of tetany, seizure, or laryngeal spasm requiring aggressive treatment with intravenous calcium administration. Calcium gluconate is the preferred intravenous calcium type as calcium chloride often causes local irritation. Calcium gluconate contains 90 mg of elemental calcium per 10 m. L ampule and usually 1 to 2 ampules (180 mg of elemental calcium) diluted in 50 to 100 m. L of 5% dextrose is infused over 10 minutes. This can be repeated until the patient's symptoms have cleared. It is essential to measure serum magnesium in any patient who is hypocalcemic as correction of hypomagnesemia must occur to overcome PTH resistance before serum calcium will return to normal. Intravenous administration of calcium is not without problems. Patients taking digitalis may have increased sensitivity to intravenous calcium. Rapid administration could result in arrhythmias so that intravenous calcium administration should be carefully monitored.
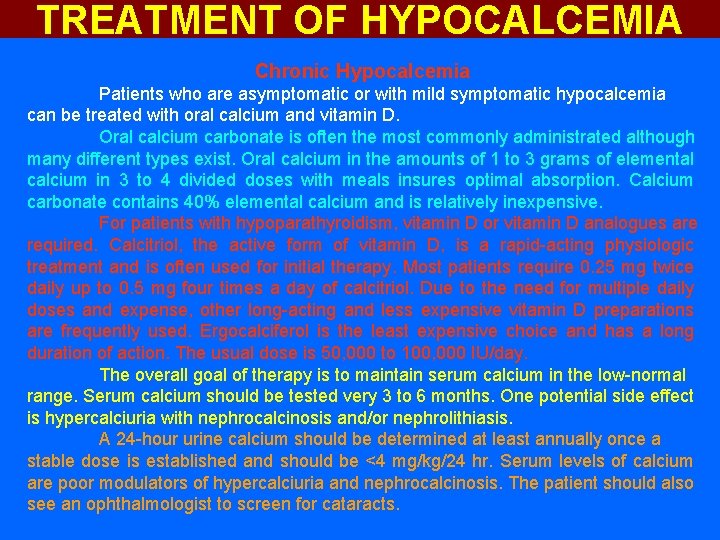
TREATMENT OF HYPOCALCEMIA Chronic Hypocalcemia Patients who are asymptomatic or with mild symptomatic hypocalcemia can be treated with oral calcium and vitamin D. Oral calcium carbonate is often the most commonly administrated although many different types exist. Oral calcium in the amounts of 1 to 3 grams of elemental calcium in 3 to 4 divided doses with meals insures optimal absorption. Calcium carbonate contains 40% elemental calcium and is relatively inexpensive. For patients with hypoparathyroidism, vitamin D or vitamin D analogues are required. Calcitriol, the active form of vitamin D, is a rapid-acting physiologic treatment and is often used for initial therapy. Most patients require 0. 25 mg twice daily up to 0. 5 mg four times a day of calcitriol. Due to the need for multiple daily doses and expense, other long-acting and less expensive vitamin D preparations are frequently used. Ergocalciferol is the least expensive choice and has a long duration of action. The usual dose is 50, 000 to 100, 000 IU/day. The overall goal of therapy is to maintain serum calcium in the low-normal range. Serum calcium should be tested very 3 to 6 months. One potential side effect is hypercalciuria with nephrocalcinosis and/or nephrolithiasis. A 24 -hour urine calcium should be determined at least annually once a stable dose is established and should be <4 mg/kg/24 hr. Serum levels of calcium are poor modulators of hypercalciuria and nephrocalcinosis. The patient should also see an ophthalmologist to screen for cataracts.

- Slides: 112