Board Inservice Review Part 2 Angela M Mills
Board / Inservice Review Part 2 Angela M. Mills, MD Department of Emergency Medicine University of Pennsylvania Health System

HEENT 5%
Orbital Trauma n Orbital floor weakest point – – – n medial wall 2 nd weakest best xray Water’s view teardrop sign on xray Retrobulbar hemorrhage – acute decreased visual acuity, proptosis, dilated non-reactive pupil – consider lateral canthotomy

Orbital Floor Fracture

Tear Drop Sign
Orbital Trauma n Hyphema – usually bleeding from ciliary body vessels after blunt trauma – most common / serious complication rebleeding in 3 -5 days n Retinal detachment – flashing lights or floaters may herald detachment before loss of vision

Retinal Detachment
Orbital Trauma n Alkali burns – liquefaction necrosis – worse than acid burns – irrigate copiously n Acid burns – coagulation necrosis – less destructive
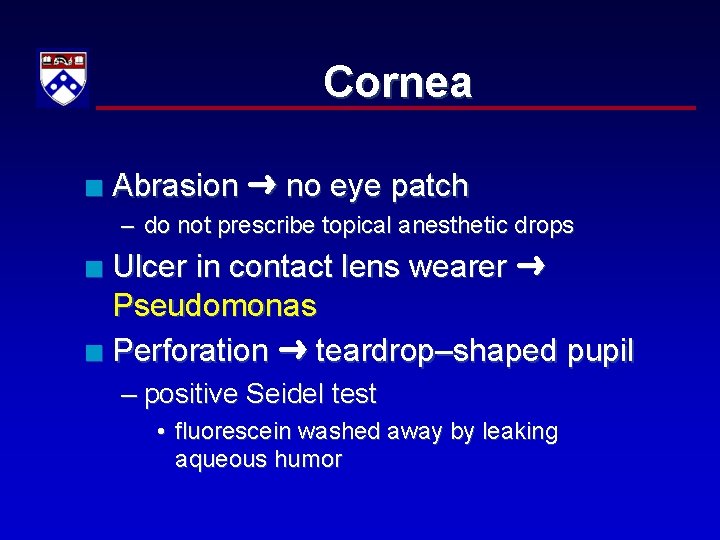
Cornea n Abrasion no eye patch – do not prescribe topical anesthetic drops Ulcer in contact lens wearer Pseudomonas n Perforation teardrop–shaped pupil n – positive Seidel test • fluorescein washed away by leaking aqueous humor
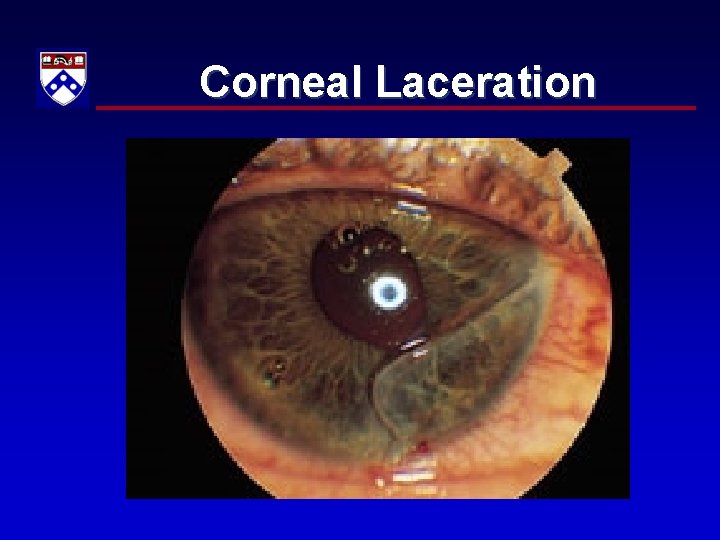
Corneal Laceration
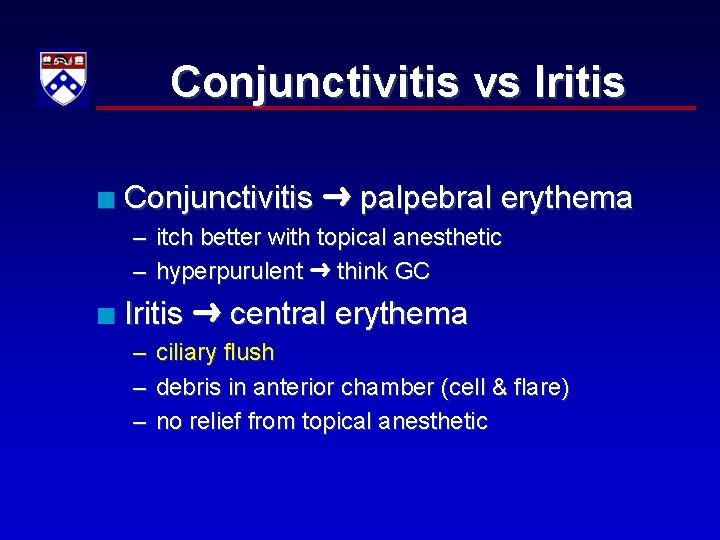
Conjunctivitis vs Iritis n Conjunctivitis palpebral erythema – itch better with topical anesthetic – hyperpurulent think GC n Iritis central erythema – ciliary flush – debris in anterior chamber (cell & flare) – no relief from topical anesthetic
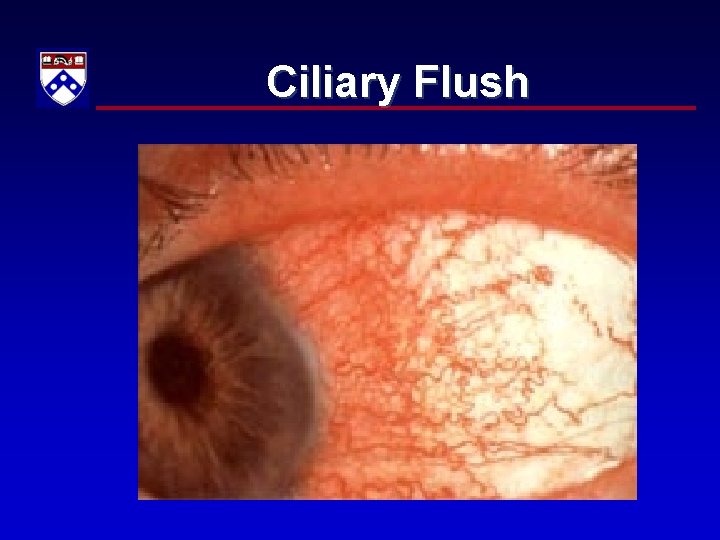
Ciliary Flush
Infection n Preseptal Periorbital – – n eye not involved full EOM normal acuity Staphylococcus most common Septal Orbital (true emergency) – – pain with EOM, proptosis, decreased vision may be dental / sinus origin Staphylococcus most common Mucormycosis: DM, immunocompromised
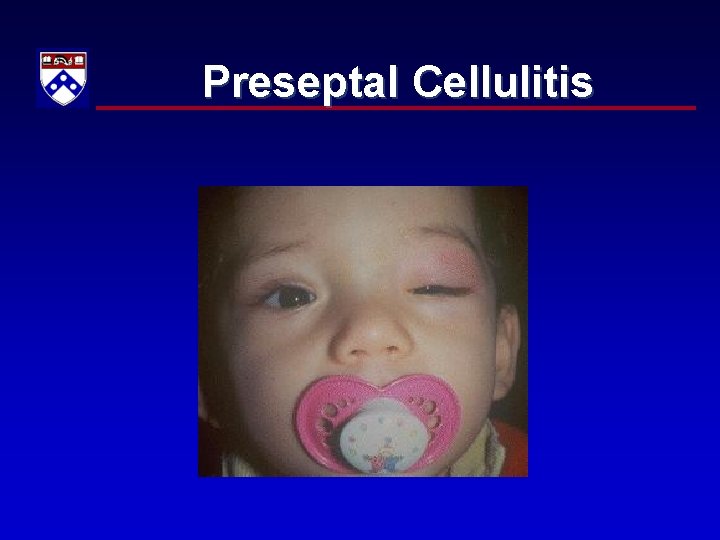
Preseptal Cellulitis
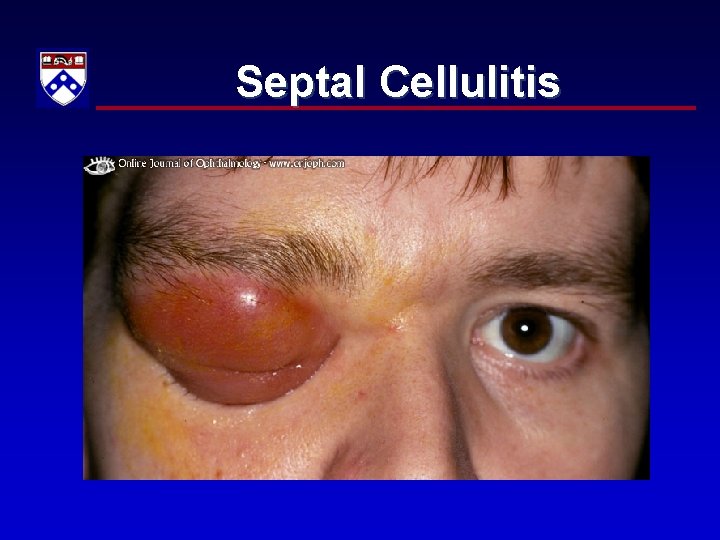
Septal Cellulitis
Herpes n Herpes Keratitis – Dendritic / branching pattern – Avoid steroids n Hutchinson’s sign – Zoster of nose tip
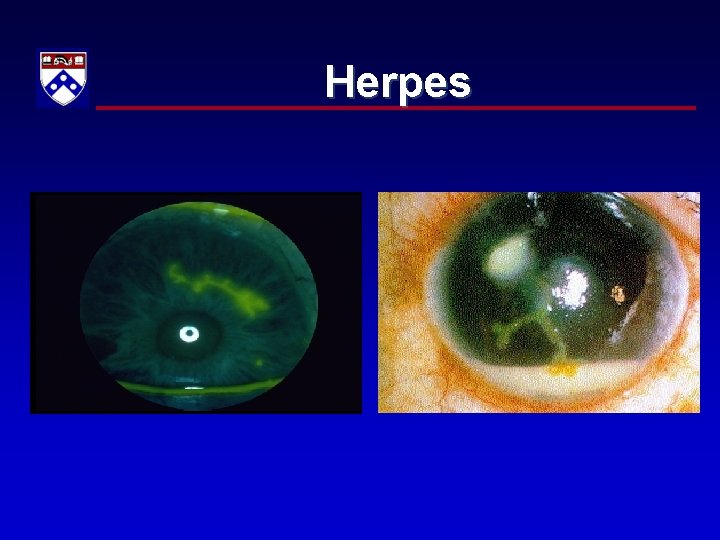
Herpes
Sudden Vision Loss Glaucoma haloes n Retinal detachment curtain n Amaurosis fugax transient n CRAO sudden, painless n Vitreous hemorrhage floaters n Temporal arteritis tender scalp n
Glaucoma Optic neuropathy 2/2 increased IOP n Acute angle closure mimic acute abd n Begins abruptly, dark room n Red painful eye, HA, n/v n Steamy cornea, midposition fixed pupil n Haloes around lights n Elevated IOP (40 – 70 mm Hg) n
Glaucoma Treatment Timolol decrease IOP n Pilocarpine open angle n Acetazolamide decrease aqueous humor production n Apraclonidine (alpha-adrenergic) n Mannitol osmotically drains eye n

Acute Angle Glaucoma
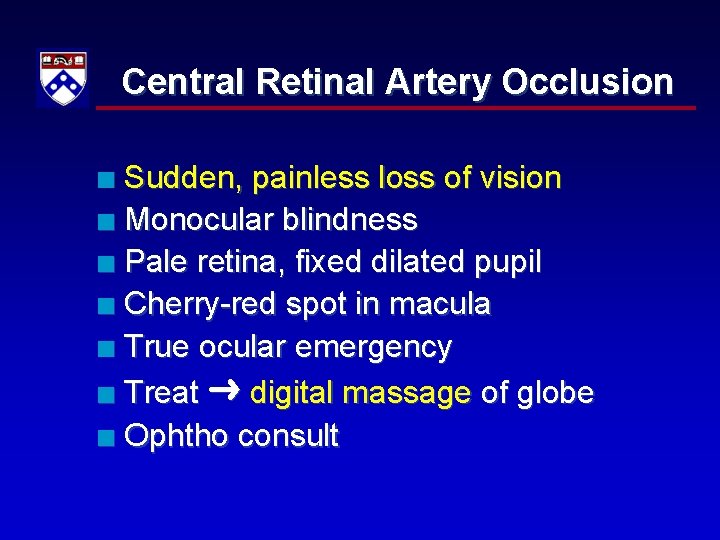
Central Retinal Artery Occlusion Sudden, painless loss of vision n Monocular blindness n Pale retina, fixed dilated pupil n Cherry-red spot in macula n True ocular emergency n Treat digital massage of globe n Ophtho consult n
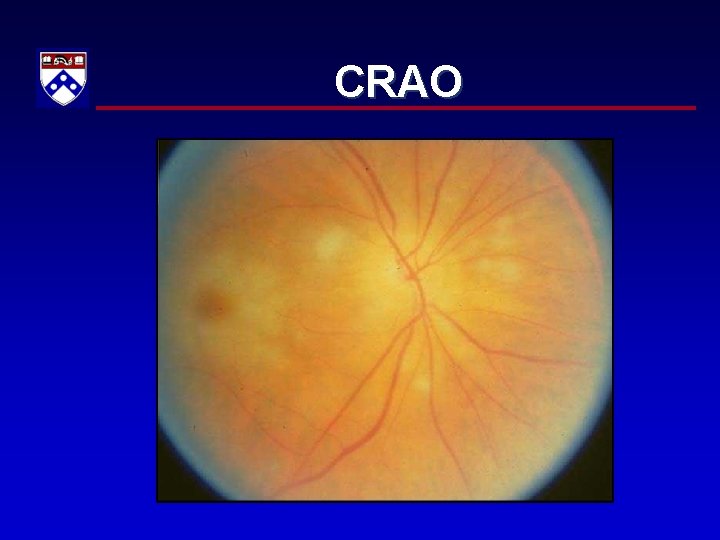
CRAO
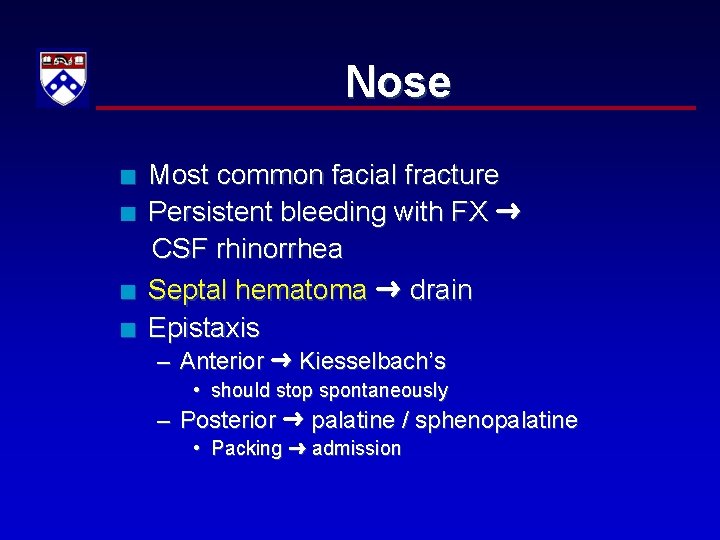
Nose n n Most common facial fracture Persistent bleeding with FX CSF rhinorrhea Septal hematoma drain Epistaxis – Anterior Kiesselbach’s • should stop spontaneously – Posterior palatine / sphenopalatine • Packing admission
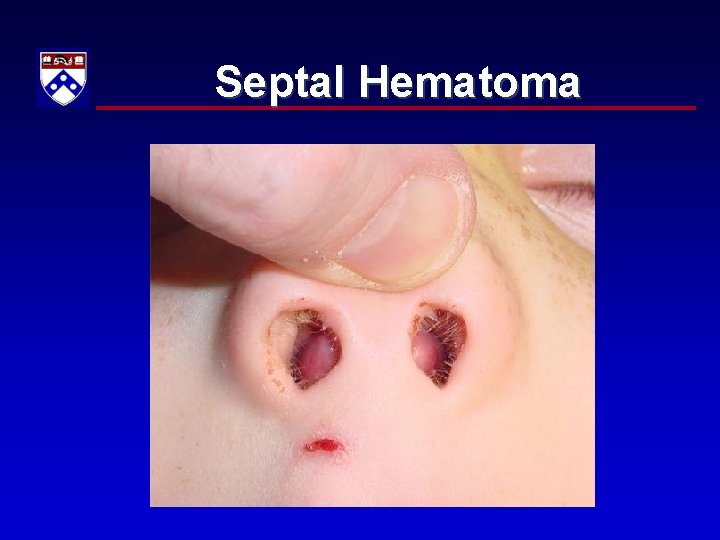
Septal Hematoma
Otitis n Otitis Externa swimmer’s ear – Staph acetic acid / abx – malignant otitis externa skull base osteomyelitis • Pseudomonas admission, ABX n Otitis Media S. pneumoniae, H. flu – Otalgia + fever amoxicillin n Bullous myringitis Mycoplasma – erythromycin
Dental Most common nontraumatic dental emergency pain from caries / abscesses n Most important concern airway n Implant avulsed teeth ASAP n – Or preserve in Hank’s sol’n, milk, saliva n Dental fractures Ellis class I, III – enamel, dentin, pulp
ANUG n Acute Necrotizing Ulcerative Gingivostomatitis – Trench-mouth, Vincent’s infection – Fiery, red, swollen, painful gums – Fusobacteria and spirochetes – Local compresses and systemic ABX
Ludwig’s Angina n Sublingual / submandibular cellulitis – connective tissue, fascia, muscle Dysphonia, trismus, tongue elevation, airway compromise n Odontogenic infection (molars) n Mixed aerobic / anaerobic n
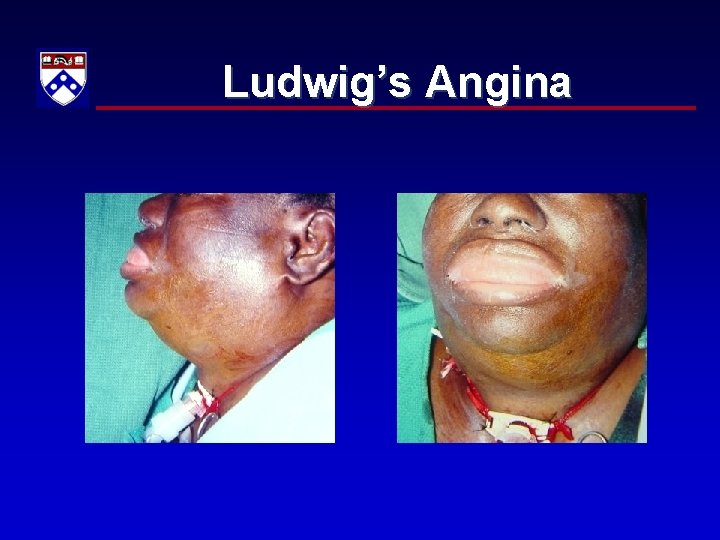
Ludwig’s Angina
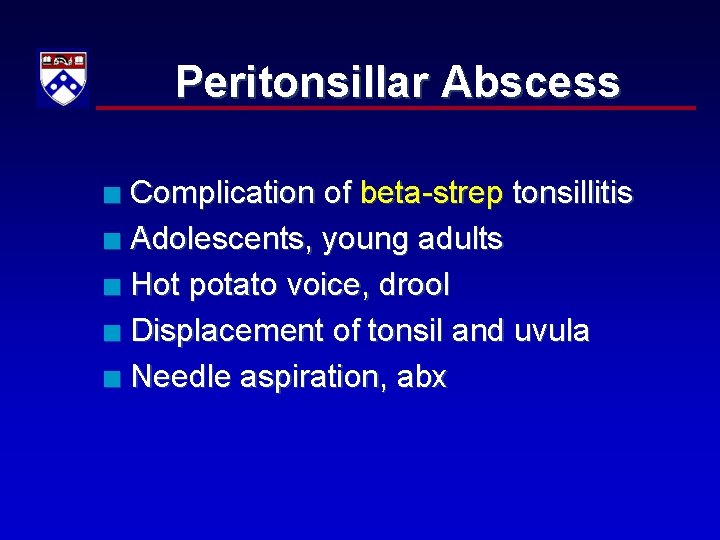
Peritonsillar Abscess Complication of beta-strep tonsillitis n Adolescents, young adults n Hot potato voice, drool n Displacement of tonsil and uvula n Needle aspiration, abx n
Tonsillitis
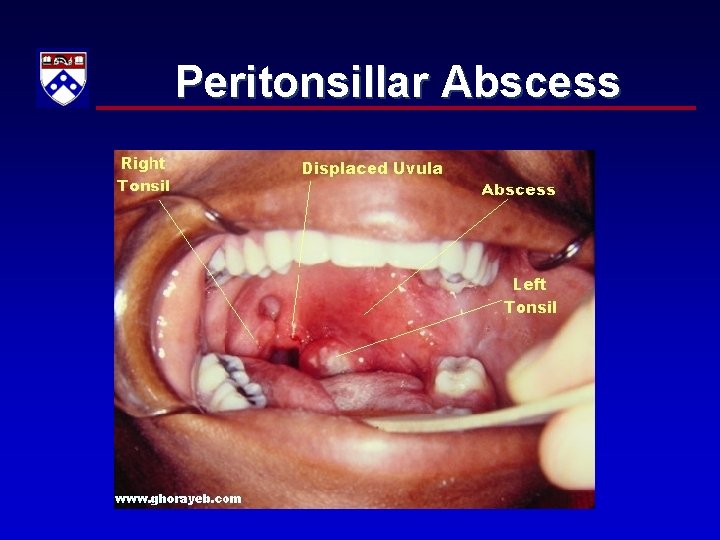
Peritonsillar Abscess
ENT n Ramsay-Hunt Syndrome – Herpes zoster involving TM and external ear canal, pharynx, facial nerve paralysis, cornea Ear trauma drain subperichondral hematoma n Angioedema of tongue ACE inhibitors n

Angioedema
Hematology 2%
Blood Products 1 U PRBC ↑ Hgb ~ 1 gm% n Hematocrit ~ 3 x Hgb n 1 U platelets ↑ count 5, 000 – 10, 000 n Autotransfusion: no functional plt, fibrinogen n Universal donor O-negative n Treat symptoms, not numbers n
Blood Products Most common reaction febrile n Most serious reaction hemolytic n Disease transmission virtually zero n Most common disease transmission Hepatitis C n Massive transfusion risks n – hypothermia, thrombocytopenia, hypocalcemia, coagulation defects
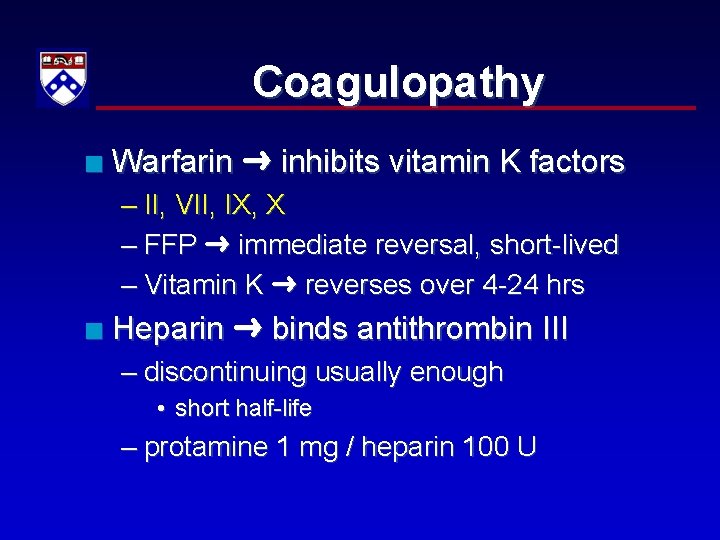
Coagulopathy n Warfarin inhibits vitamin K factors – II, VII, IX, X – FFP immediate reversal, short-lived – Vitamin K reverses over 4 -24 hrs n Heparin binds antithrombin III – discontinuing usually enough • short half-life – protamine 1 mg / heparin 100 U
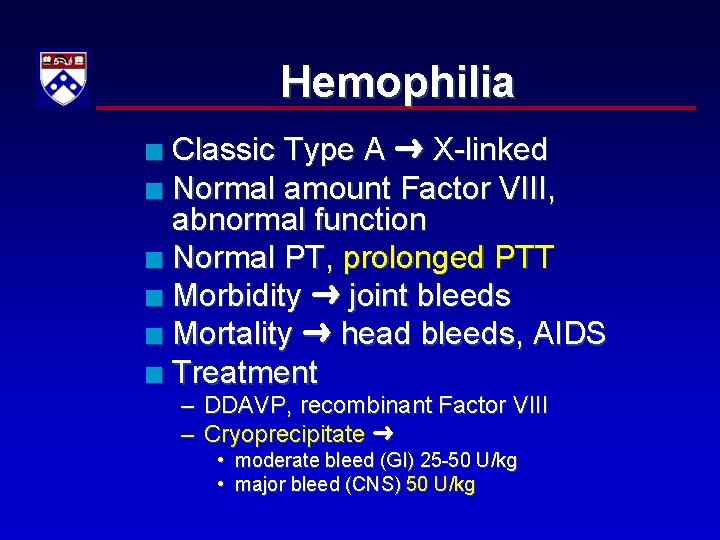
Hemophilia Classic Type A X-linked n Normal amount Factor VIII, abnormal function n Normal PT, prolonged PTT n Morbidity joint bleeds n Mortality head bleeds, AIDS n Treatment n – DDAVP, recombinant Factor VIII – Cryoprecipitate • moderate bleed (GI) 25 -50 U/kg • major bleed (CNS) 50 U/kg
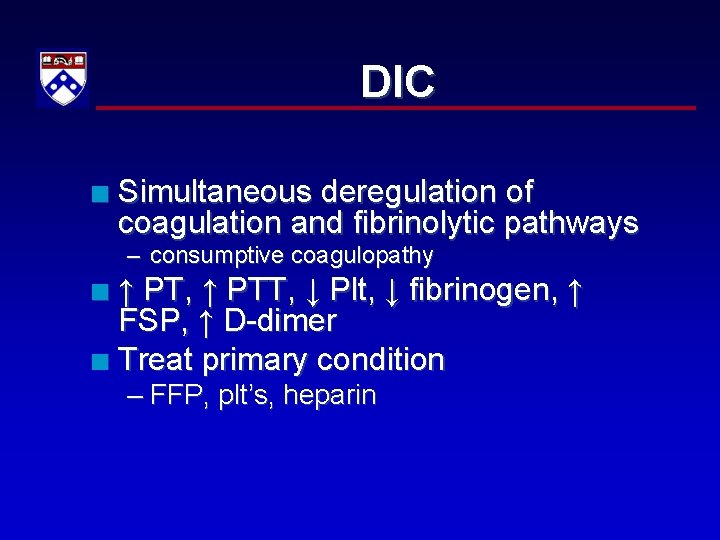
DIC n Simultaneous deregulation of coagulation and fibrinolytic pathways – consumptive coagulopathy ↑ PT, ↑ PTT, ↓ Plt, ↓ fibrinogen, ↑ FSP, ↑ D-dimer n Treat primary condition n – FFP, plt’s, heparin
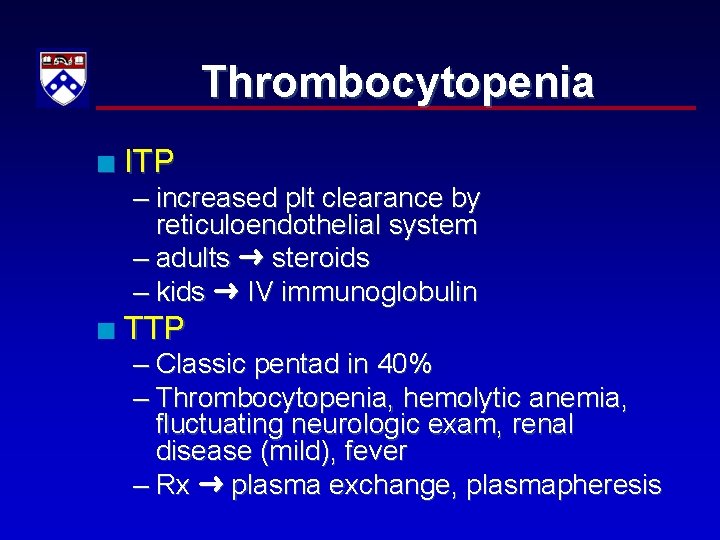
Thrombocytopenia n ITP – increased plt clearance by reticuloendothelial system – adults steroids – kids IV immunoglobulin n TTP – Classic pentad in 40% – Thrombocytopenia, hemolytic anemia, fluctuating neurologic exam, renal disease (mild), fever – Rx plasma exchange, plasmapheresis
Von Willebrand’s Disease Most common genetic bleeding d/o n Autosomal dominant n Prolonged bleeding time n Normal PT, prolonged PTT ~ 25% n n Platelet count normal, ↓ function n Rx DDAVP, FFP, cryoprecipitate
Anemia n Most common human enzyme defect G 6 PD deficiency – hemolysis with oxidants n Hemolytic-uremia syndrome – renal failure, hemolysis, fever, low platelets – diarrhea precursor E. coli 0157: H 7 most common
Sickle Cell Disease n Vaso-occlusive painful – evaluate for precipitating causes • infection, dehydration, trauma, cold exposure – labs not useful in Dx, r/o complications Aplastic BM failure, ↓Hct, ↓RC n Hemolytic ↓Hct, ↑ RC n Sequestration large spleen in kids n RX IVF, analgesia, O 2, transfuse prn n
Sickle Cell Disease n Acute chest syndrome – secondarily infected pulmonary infarction – high mortality, severe ↓ in pulm fxn n Infectious crises – especially children < 5 – functional asplenia – encapsulated organisms (pneumococcus) & Salmonella, S. aureus (osteo)
Oncology Leukemia blast crisis flu-like sx’s with ↑ immature cells n Leukemoid reaction ↑ WBC due to infection, resembles leukemia n Neutropenia (<1000 /ml) death n Multiple myeloma n – plasma cell malignancy – pain in back, ribs – Hypercalcemia ~ 30%, hyperviscosity
Tumor Compressions n n Spinal cord steroids, radiation Upper airway establish definitive airway Pericardial tamponade echocardiogram pericardiocentesis if unstable Superior vena cava syndrome – head/neck/upper chest congestion, facial plethora, ICP increase, papilledema – RX diuretics, steroids, radiation
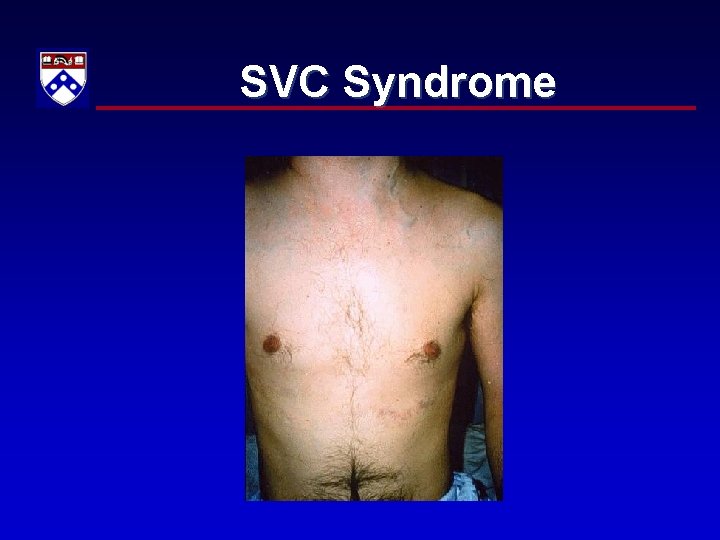
SVC Syndrome
Oncology n Hypercalcemia ↓ QT NSS, furosemide n SIADH ↓Na, normovolemia, ↑ UNa – RX NSS, diuretics n Hyperviscosity syndrome fatigue, HA, CVA, blindness, seizures – RX NSS, phlebotomy n Adrenal insufficiency hydrocortisone – consider in all cancer pts w/ fever, dehydration, hypotension, shock
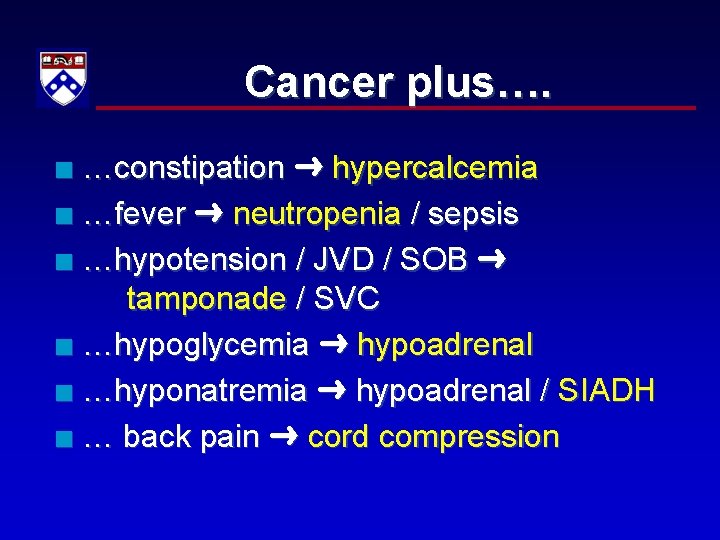
Cancer plus…. …constipation hypercalcemia n …fever neutropenia / sepsis n …hypotension / JVD / SOB tamponade / SVC n …hypoglycemia hypoadrenal n …hyponatremia hypoadrenal / SIADH n … back pain cord compression n
Immunology/ Rheumatology 2%
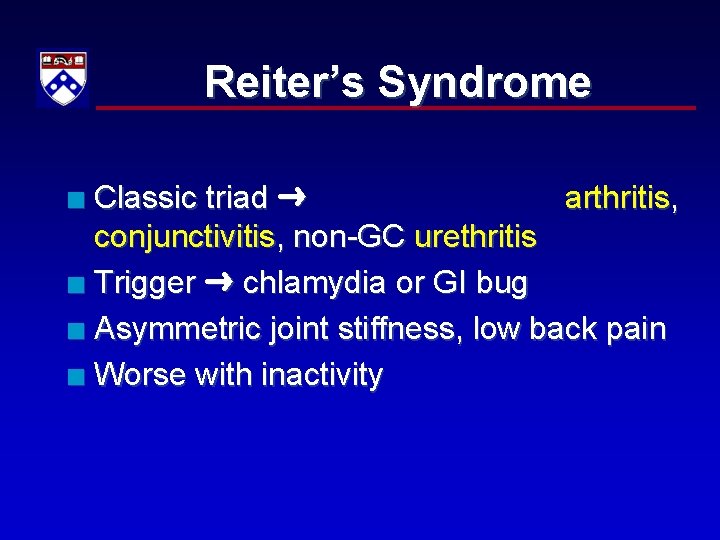
Reiter’s Syndrome Classic triad arthritis, conjunctivitis, non-GC urethritis n Trigger chlamydia or GI bug n Asymmetric joint stiffness, low back pain n Worse with inactivity n
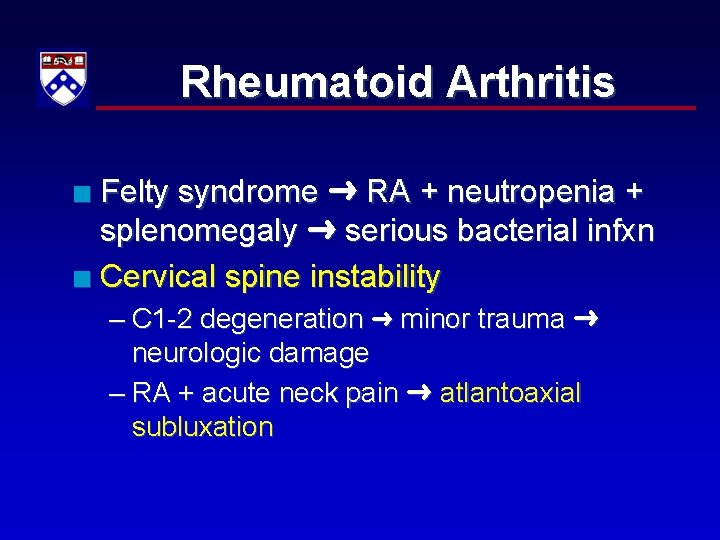
Rheumatoid Arthritis Felty syndrome RA + neutropenia + splenomegaly serious bacterial infxn n Cervical spine instability n – C 1 -2 degeneration minor trauma neurologic damage – RA + acute neck pain atlantoaxial subluxation
Vasculitis Henoch-Schonlein Purpura hypersensitivity vasculitis n Temporal arteritis HA, fatigue, fever, anemia, ↑ sed rate n – RX high dose steroids – complications include blindness
Anaphylaxis / Allergies n Most common cause of death airway obst Hypotension vasodilation, capillary leak n RX epinephrine n – Bronchospasm inhaled ß-agonists – H 1 -blocker diphenhydramine – Systemic corticosteroids – H 2 -blocker
Anaphylaxis Refractory ↓ BP pressors with alpha-adrenergic activity (dopamine, levarterenol) n Resistant to epinephrine if taking ß-blocker glucagon n

Gout vs Pseudogout n Gout – monosodium urate – negative birefringent – needle-shaped – 1 st MTP (75%), males n Pseudogout – calcium pyrophosphate – positive birefringent – rhomboid n RX NSAIDs / colchicine
Septic Joint Monoarticular = Septic until proven o/w n Infection can coexist with crystalline dz n Septic arthritis in pts IVDA S. Aureus n Septic arthritis in pts 14 - 40 yo GC n – females f/c, migratory tenosynovitis, arthritis – characteristic rash in 2/3 • hemorrhagic necrotic pustules w/ surrounding erythema (distal ext) – blood / joint cxs freq negative cervical cx – Ceftriaxone

Disseminated GC
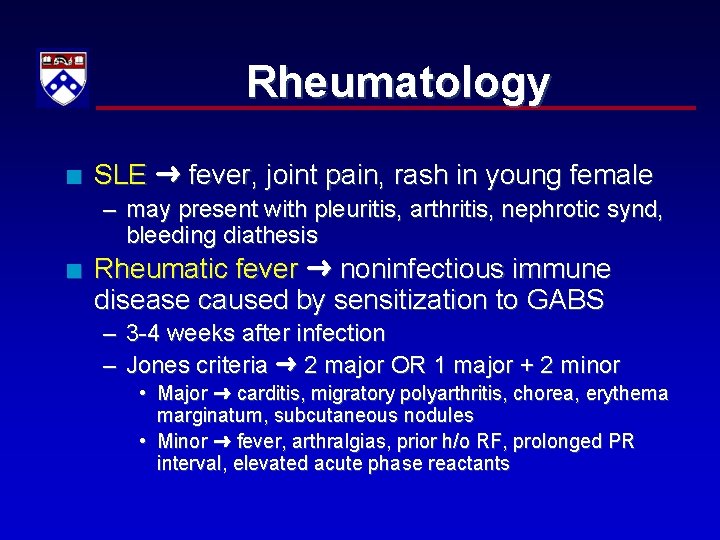
Rheumatology n SLE fever, joint pain, rash in young female – may present with pleuritis, arthritis, nephrotic synd, bleeding diathesis n Rheumatic fever noninfectious immune disease caused by sensitization to GABS – 3 -4 weeks after infection – Jones criteria 2 major OR 1 major + 2 minor • Major carditis, migratory polyarthritis, chorea, erythema marginatum, subcutaneous nodules • Minor fever, arthralgias, prior h/o RF, prolonged PR interval, elevated acute phase reactants
Musculoskeletal Nontraumatic 3%
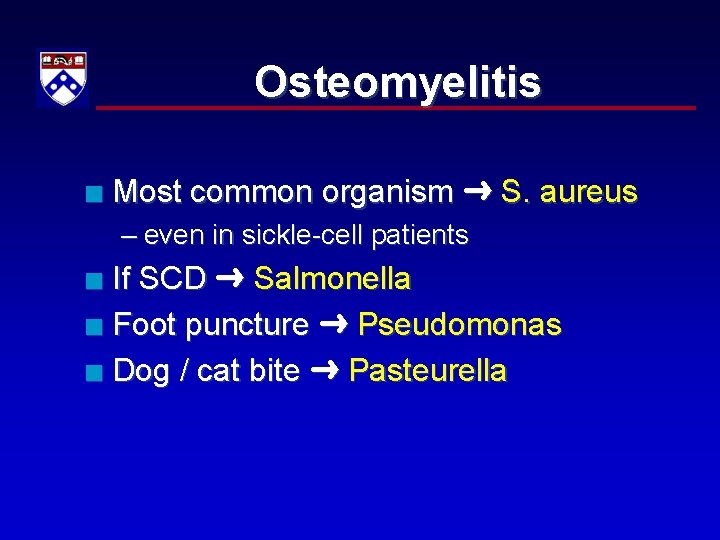
Osteomyelitis n Most common organism S. aureus – even in sickle-cell patients If SCD Salmonella n Foot puncture Pseudomonas n Dog / cat bite Pasteurella n
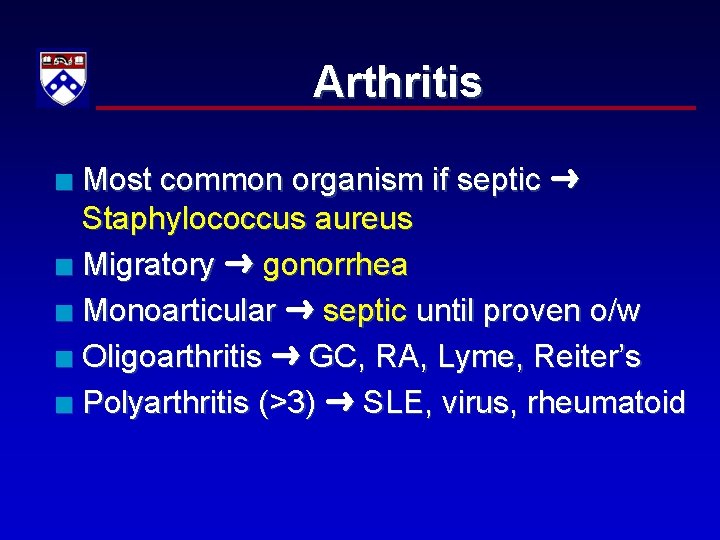
Arthritis Most common organism if septic Staphylococcus aureus n Migratory gonorrhea n Monoarticular septic until proven o/w n Oligoarthritis GC, RA, Lyme, Reiter’s n Polyarthritis (>3) SLE, virus, rheumatoid n
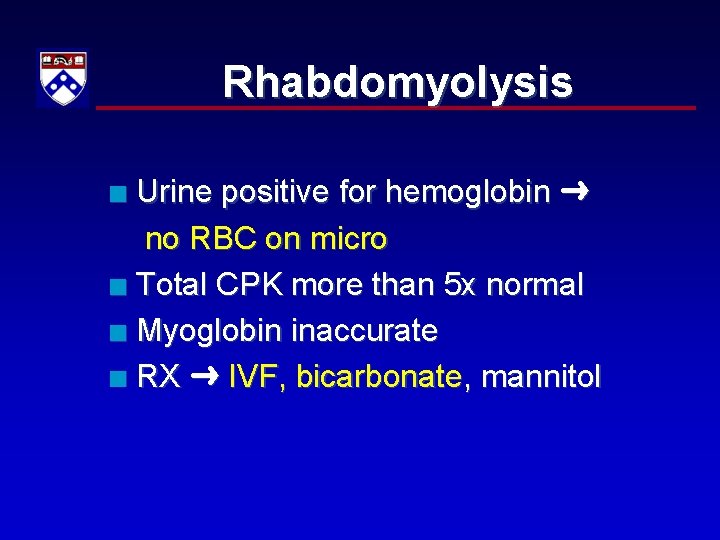
Rhabdomyolysis Urine positive for hemoglobin no RBC on micro n Total CPK more than 5 x normal n Myoglobin inaccurate n RX IVF, bicarbonate, mannitol n
Nervous System 5%
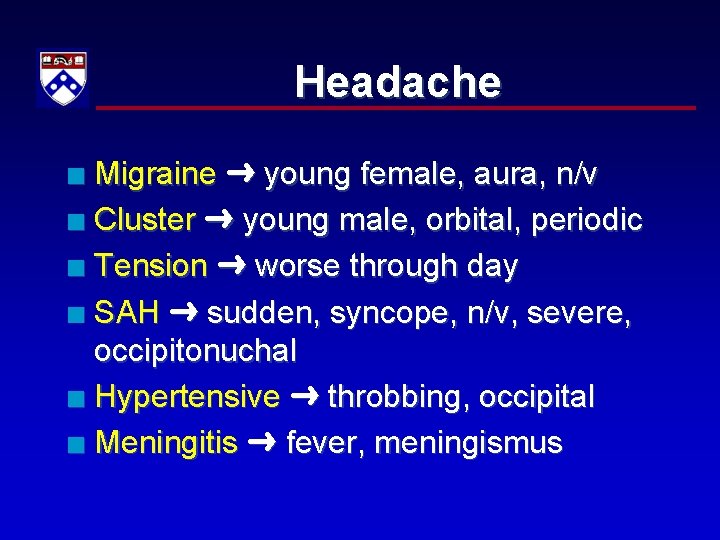
Headache Migraine young female, aura, n/v n Cluster young male, orbital, periodic n Tension worse through day n SAH sudden, syncope, n/v, severe, occipitonuchal n Hypertensive throbbing, occipital n Meningitis fever, meningismus n
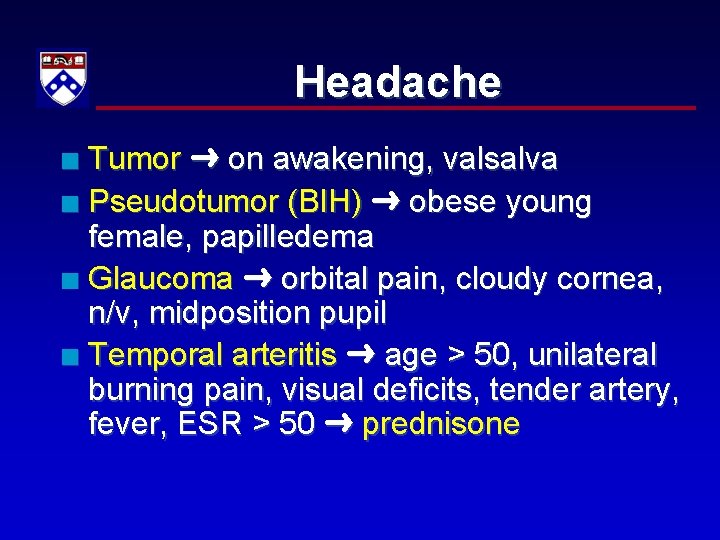
Headache Tumor on awakening, valsalva n Pseudotumor (BIH) obese young female, papilledema n Glaucoma orbital pain, cloudy cornea, n/v, midposition pupil n Temporal arteritis age > 50, unilateral burning pain, visual deficits, tender artery, fever, ESR > 50 prednisone n
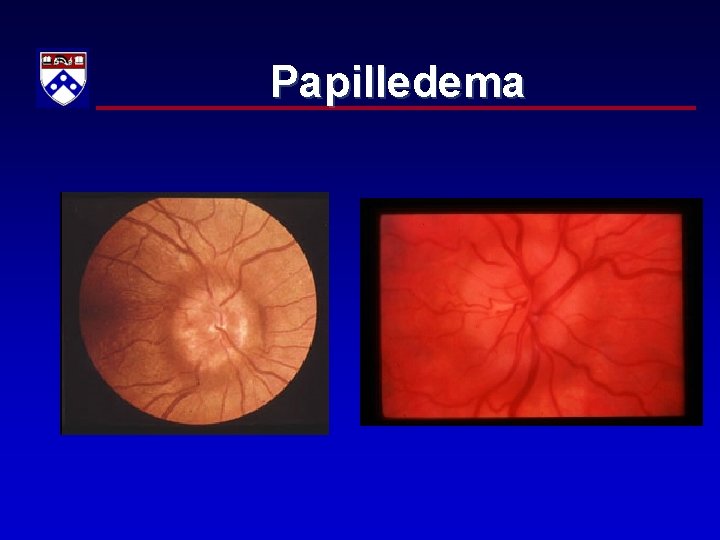
Papilledema
Multiple Sclerosis If distribution of neurologic deficits doesn’t make sense n Most common initial presentation optic neuritis n Pathognomonic B/L internuclear ophthalmoplegia n – double vision w/ lateral gaze
Subarachnoid Hemorrhage Worst HA of life, n/v, HTN, meningismus n 60% have sentinel HA’s n Head CT ~ 93 % sensitive n Must do LP to r/o SAH xanthochromia n RX NSurg, BP control, nimodipine n
Stroke Ischemic vs hemorrhagic n RX O 2, avoid D 5, +TPA n – Rx only severe HTN n TIAs brief, transient focal disturbances of neurologic function – 5 -10% have major infarct each year
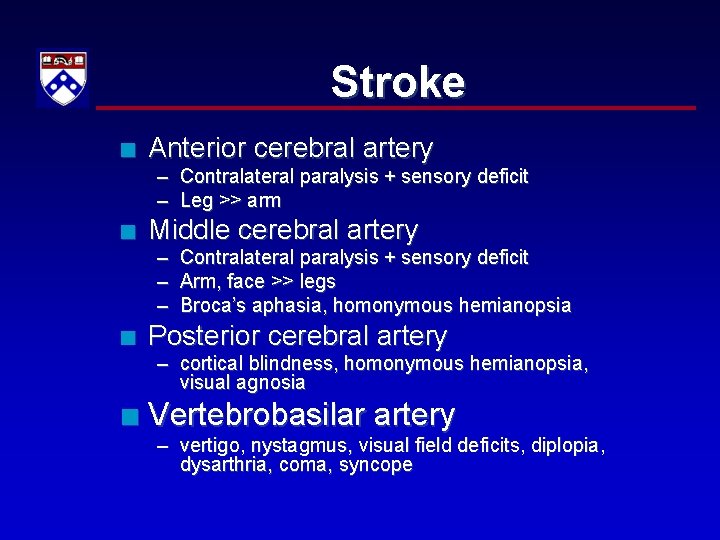
Stroke n Anterior cerebral artery – Contralateral paralysis + sensory deficit – Leg >> arm n Middle cerebral artery – Contralateral paralysis + sensory deficit – Arm, face >> legs – Broca’s aphasia, homonymous hemianopsia n Posterior cerebral artery – cortical blindness, homonymous hemianopsia, visual agnosia n Vertebrobasilar artery – vertigo, nystagmus, visual field deficits, diplopia, dysarthria, coma, syncope
Epidural abscess IVDA hematogenous spread n Fever, back pain, percussive tenderness n DX CT or MRI n RX antibiotics, NSurg n
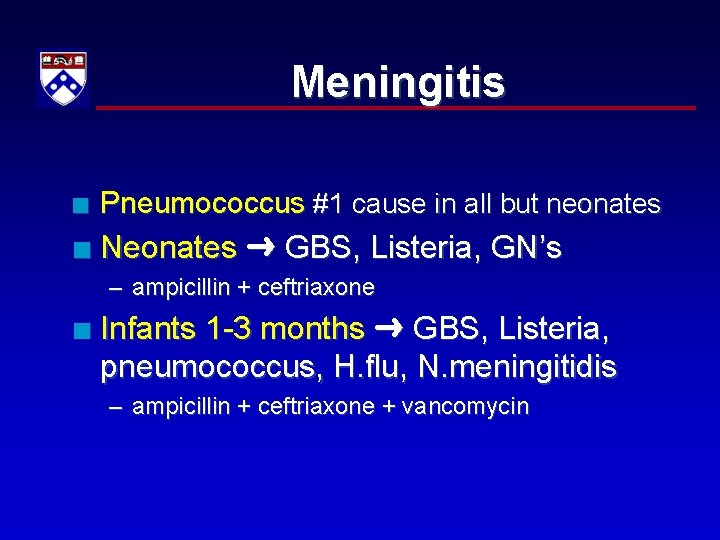
Meningitis n Pneumococcus #1 cause in all but neonates n Neonates GBS, Listeria, GN’s – ampicillin + ceftriaxone n Infants 1 -3 months GBS, Listeria, pneumococcus, H. flu, N. meningitidis – ampicillin + ceftriaxone + vancomycin
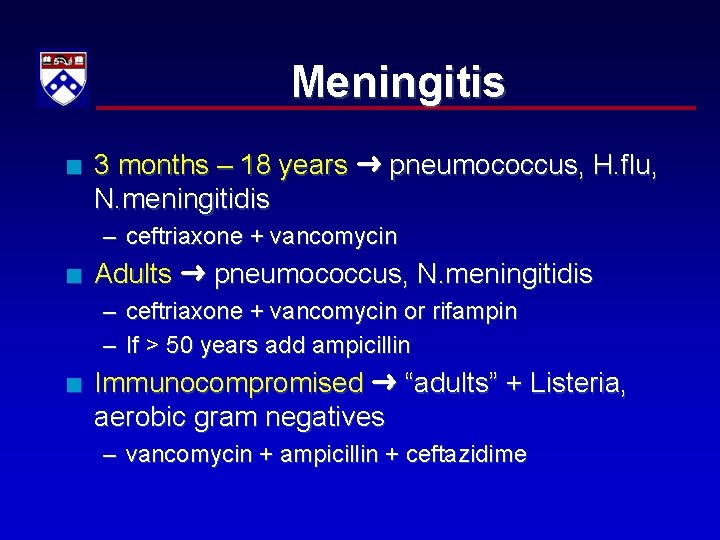
Meningitis n 3 months – 18 years pneumococcus, H. flu, N. meningitidis – ceftriaxone + vancomycin n Adults pneumococcus, N. meningitidis – ceftriaxone + vancomycin or rifampin – If > 50 years add ampicillin n Immunocompromised “adults” + Listeria, aerobic gram negatives – vancomycin + ampicillin + ceftazidime
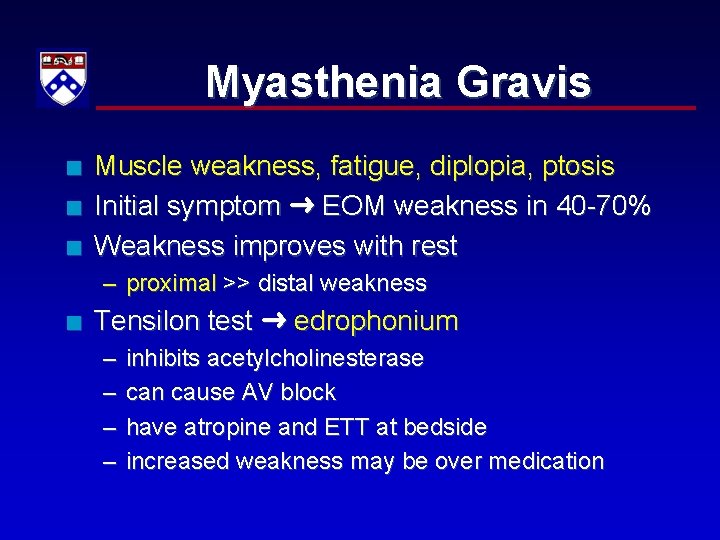
Myasthenia Gravis n n n Muscle weakness, fatigue, diplopia, ptosis Initial symptom EOM weakness in 40 -70% Weakness improves with rest – proximal >> distal weakness n Tensilon test edrophonium – – inhibits acetylcholinesterase can cause AV block have atropine and ETT at bedside increased weakness may be over medication
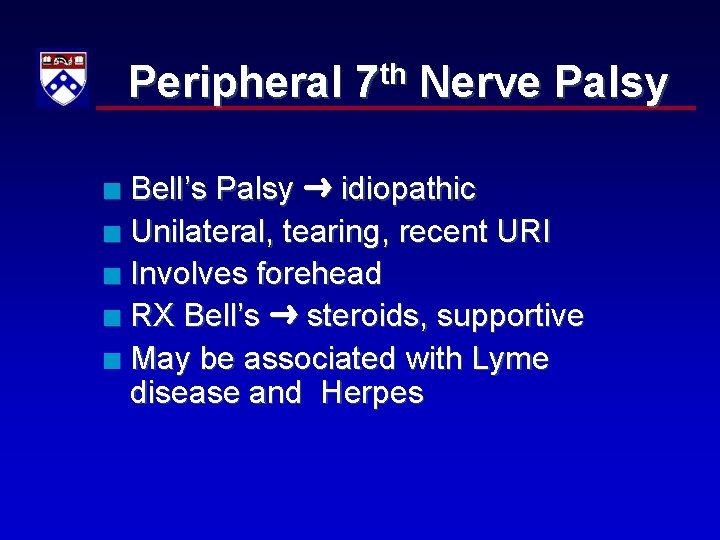
Peripheral 7 th Nerve Palsy Bell’s Palsy idiopathic n Unilateral, tearing, recent URI n Involves forehead n RX Bell’s steroids, supportive n May be associated with Lyme disease and Herpes n

Bell’s Palsy
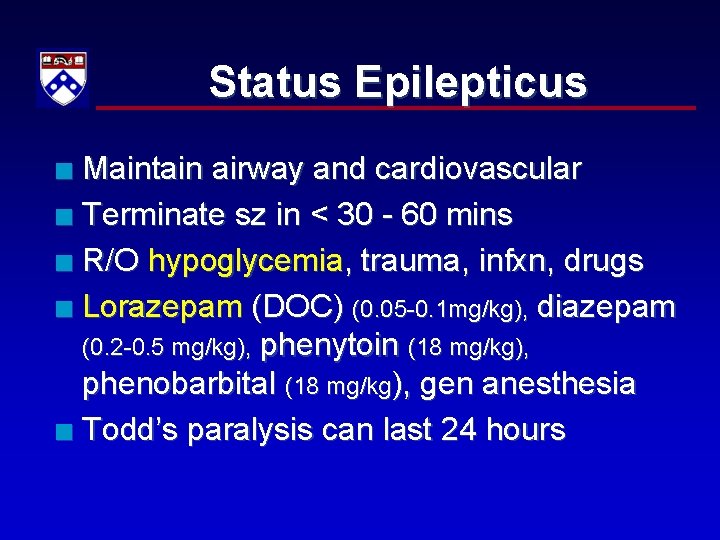
Status Epilepticus Maintain airway and cardiovascular n Terminate sz in < 30 - 60 mins n R/O hypoglycemia, trauma, infxn, drugs n Lorazepam (DOC) (0. 05 -0. 1 mg/kg), diazepam (0. 2 -0. 5 mg/kg), phenytoin (18 mg/kg), phenobarbital (18 mg/kg), gen anesthesia n Todd’s paralysis can last 24 hours n
Psychobehavioral 3%
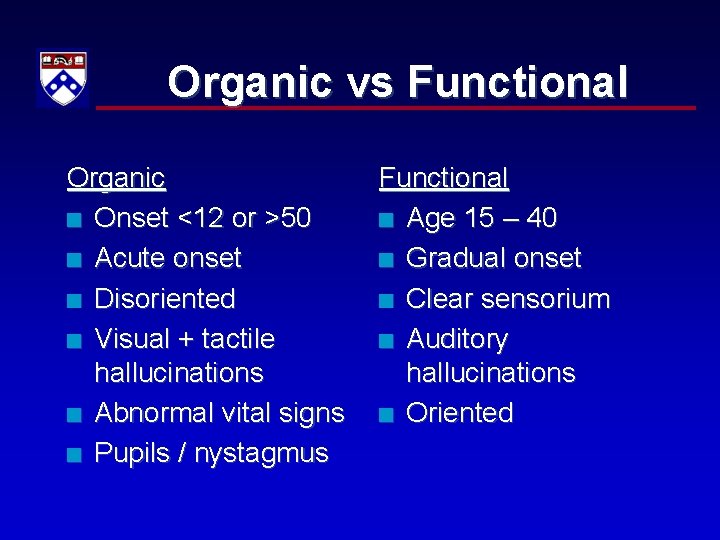
Organic vs Functional Organic n Onset <12 or >50 n Acute onset n Disoriented n Visual + tactile hallucinations n Abnormal vital signs n Pupils / nystagmus Functional n Age 15 – 40 n Gradual onset n Clear sensorium n Auditory hallucinations n Oriented
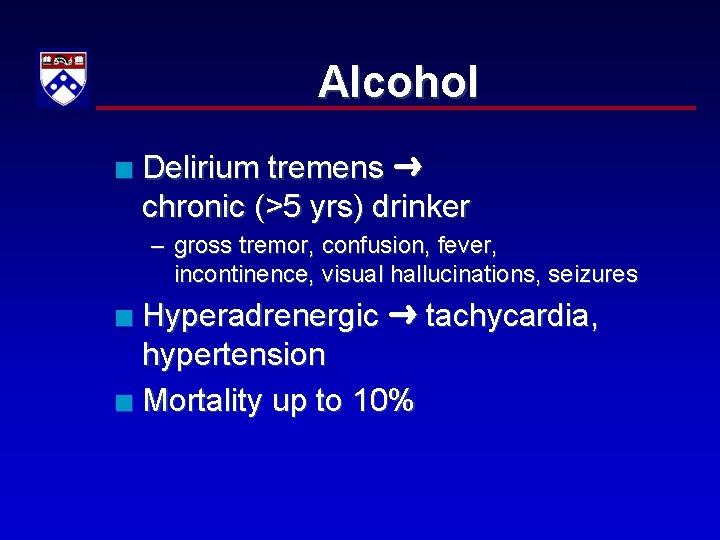
Alcohol n Delirium tremens chronic (>5 yrs) drinker – gross tremor, confusion, fever, incontinence, visual hallucinations, seizures Hyperadrenergic tachycardia, hypertension n Mortality up to 10% n
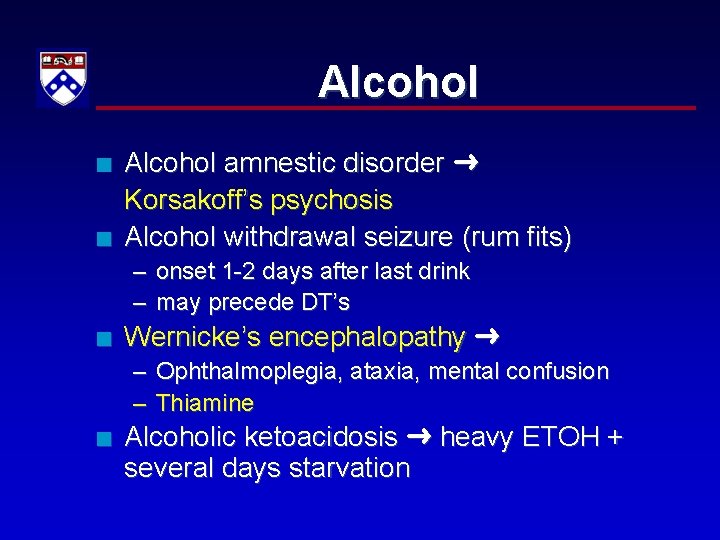
Alcohol n n Alcohol amnestic disorder Korsakoff’s psychosis Alcohol withdrawal seizure (rum fits) – onset 1 -2 days after last drink – may precede DT’s n Wernicke’s encephalopathy – Ophthalmoplegia, ataxia, mental confusion – Thiamine n Alcoholic ketoacidosis heavy ETOH + several days starvation
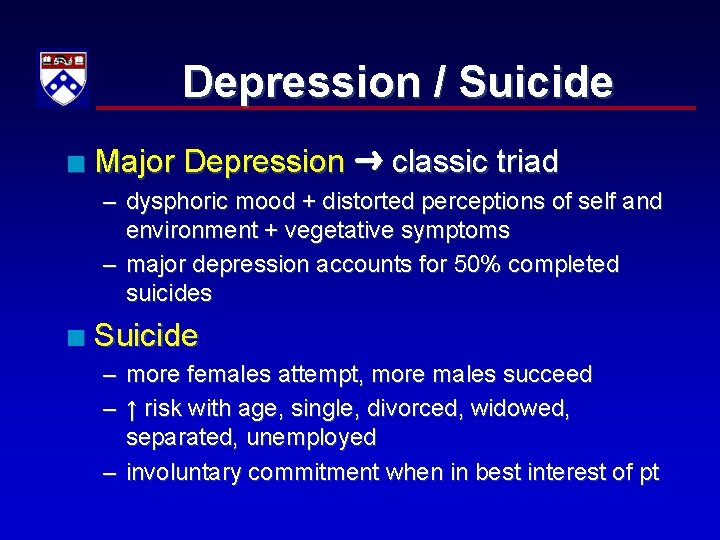
Depression / Suicide n Major Depression classic triad – dysphoric mood + distorted perceptions of self and environment + vegetative symptoms – major depression accounts for 50% completed suicides n Suicide – more females attempt, more males succeed – ↑ risk with age, single, divorced, widowed, separated, unemployed – involuntary commitment when in best interest of pt
Homicide Breach of confidentiality vs safety of others n Case law requires reporting threats of violence against 3 rd parties to police n Legal precedent of “duty to warn” n – Tarasoff v Regents of Univ of California
Child Abuse Unexplained / poorly explained injuries n Injuries incompatible with stated history n Changing history n Significant delay in seeking treatment n Required reporting for ANY suspicion n
Child Abuse Multiple injuries in various stages n Multiplanar front & back, R & L sides n Obvious pattern hand, belt n Injuries in usually well-protected areas trunk, upper arms, upper legs, neck, face, perineal area n
Domestic Abuse Failure to ask n Barriers to ED diagnosis lack of training, fear of offending n Let victim know help available n Some states mandatory reporting n
Elder Abuse Battery physical, psychological, verbal n Neglect, financial abuse n Confusion / disorientation risk factor n
Neuroleptic Side Effects n Extrapyramidal symptoms – Dystonia, akathisia , tardive dyskinesia n n Anticholinergic delirium, fever, dryness, erythema, mydriasis Alpha blockade ↓ BP, syncope
Neuroleptic Malignant Synd Hyperthermia, autonomic disturbances, muscle rigidity n Pts with h/o phenothiazine therapy n Not dose related n Elevated CPK n Rare 0. 5 – 1 % pts n RX IVF, supportive, dantrolene n
Renal / Urogenital 3%
Acute Renal Failure Pre-renal (↓ renal flow) 40 – 80% n Renal (intrinsic, ATN) 25% n Post-renal (prostate) 5% n 50% ↓ creatinine clearance OR 50% ↑ serum creatinine n
Chronic Renal Failure Months to years No symptoms until function < 10% n Causes DM, HTN, glomerulonephropathies n Hyperkalemia life-threatening n
Access Problems Most common problems stenosis, thrombosis n Infection Staph aureus, GN’s n RX vancomycin (1/2 life 5 -7 days) n Peritoneal dialysis n – most common problem infection – RX intraperitoneal abx, IV if febrile
Glomerulonephritis Most common sign periorbital edema n Teenage boys n Hypertension in ~ 80% n Gross hematuria n Consider post-streptococcal infection n
Pyelonephritis Fever + flank pain + CVAT n Leukocyte esterase highly sensitive for pyuria n RX fluoroquinolone n Admit toxic, pregnant, comorbid factors n
Testicular Pain / Swelling Hydrocele transilluminates n Varicocele “bag of worms” n Hernia acute, painful n Epididymitis, testicular torsion, torsion of testicular appendage most common for boards n
Epididymitis Gradual onset of pain, local tenderness n < 40 yo STD organisms n > 40 yo E. coli, klebsiella, proteus n Prehn’s sign NOT reliable n Pain improved with elevation of scrotum n RX NSAIDs, ABX, scrotal support, ice packs n
Testicular Torsion Peak incidence puberty n Occurs at all ages n Acute unilateral pain, swelling n Cremasteric reflex usually absent n Time critical consult first US n – 80 – 100% salvage rate if detorsed within 6 hrs n Manual detorsion “open a book”
Testicular Appendage Torsion Twisting of pedunculated structures on epididymitis or testis n More common than testicular torsion in prepubertal boys n Blue dot sign pathognomonic n – appendage hemorrhage
Fournier’s Gangrene Life-threatening necrotizing infection n Occurs in immunocompromised n – diabetics, alcoholics, IVDU, steroid users Mixed flora streptococcus, B. fragilis, E. coli, clostridium n Antibiotics, surgery, consider HBO n

Fournier’s Gangrene
Urethritis Most common urologic infection n Sexually active male + dysuria = urethritis, NOT UTI n Treat for GC / chlamydia n – Ceftriaxone + doxycycline or azithro
Paraphimosis Can’t reduce retracted foreskin n Edema and venous engorgement arterial compromise, gangrene n True urologic emergency n RX manual reduction, dorsal incision n

Paraphimosis
Phimosis Inability to retract foreskin proximally beyond glans n If meatal tip involved retention n RX dilate ostium, dorsal slit n
Priapism Low flow impaired venous outflow n High flow increased arterial flow n n Causes SCD, injections for impotence n RX trial SC terbutaline – Persistent corpora aspiration, irrigation with phenylephrine n Complications impotence, infection, urinary retention
Renal Stones n Sudden debilitating flank pain n Need to consider AAA n DX by history / PE + UA n Noncontrast helical CT or US – plain film poor reliability – IVP low sensitivity / specificity than CT
Renal Stones Hematuria absent in 10% n Admit infection, single kidney, intractable pain / emesis, RI n Probability of passage n – < 4 mm ~ 90% pass – 4 -6 mm ~ 50% pass – > 6 mm ~ 10% pass
Urology Causes of urinary retention prostate enlargement, meds n Testicular CA age early 20 s n – any asymptomatic testicular mass should be considered cancer until proven otherwise n Prostatitis boggy, enlarged, tender – etiologies and RX same as epididymitis – prostate massage contraindicated
- Slides: 112