BMS 234 Medical Ethics ETHICS IN TERMINALLY ILL
BMS 234 Medical Ethics ETHICS IN TERMINALLY ILL PATIENTS
Outline ■ Terminal illness. ■ Palliative care. ■ Geriatric care. ■ Decision making.
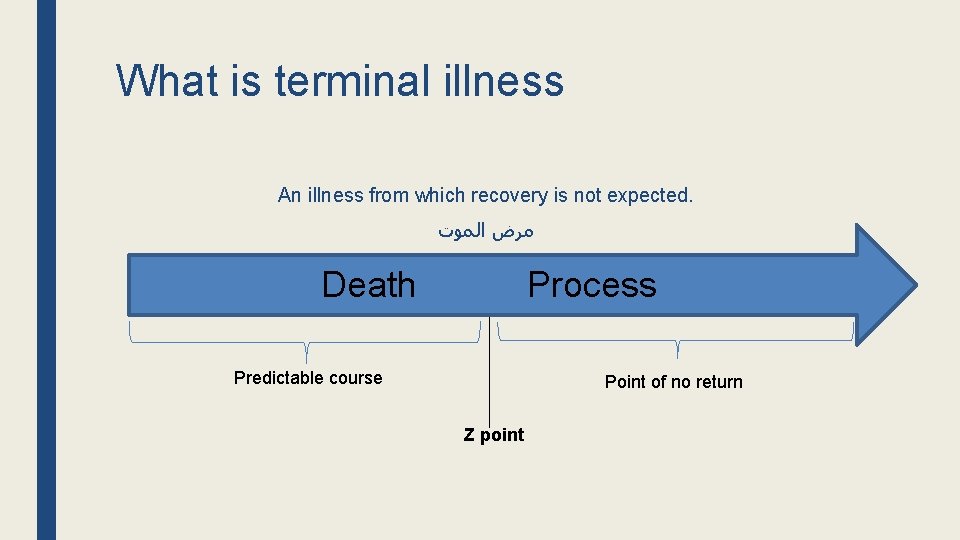
What is terminal illness An illness from which recovery is not expected. ﻣﺮﺽ ﺍﻟﻤﻮﺕ Death Process Predictable course Point of no return Z point
Is terminal illness diagnosis always accurate? some patients who were told they were going to die have lived for years, but such cases are few in actual practice. Death Process Predictable course Point of no return Z point
Why do we learn about it ■ As health professionals you will be dealing with terminally ill patients. Therefore you need to know the before and after death ethical and legal guideline. ■ As a health professional you need to consider the issue from the patients and families point of view. ■ Artificial Life support has created more ethical and practical problems.
What are the needs of terminally ill patients ■ Medical Support. ■ Psychological support. ■ Spiritual support.
Medical treatment for terminally ill patients ■ A terminally ill patient should receive treatment for the original disease. ■ The balance between benefits and side effects should be considered. ■ If interventions are unlikely to produce any significant benefit for the patient (medical futility) only palliative care and symptomatic treatments are given.
What is palliative care ■ Measures taken to make the remaining life of a terminal patient as comfortable as possible and includes pain relief, support (psychological, social, and spiritual), nutrition, hydration, etc. Palliative care starts when the hope for cure of the disease disappears.

Medical care for Palliative care patients ■ Pain Control ■ Nutrition and hydration. ■ Symptomatic treatments. ■ Palliative surgery. ■ Palliative radiotherapy.
Pain control ■ Pain control is the core of palliative care. ■ It may be problematic because some analgesics such as morphia may cause respiratory depression. ■ Analgesics affect the level of consciousness (Anesthesia).
Level of Anesthesia Patient’s choice - Semiconscious with pain. - Unconscious without pain.
Nutrition and Hydration ■ Terminal patients continue receiving nutrition, hydration, and general supportive care without discrimination.
Symptomatic Treatments ■ Symptomatic treatment such as infection control can be given to terminally ill patients. ■ The benefit should outweigh side effects especially for aggressive treatments.
Palliative surgery ■ An operation performed on an incurable cancer, that are not expected to cure the cancer but to control symptoms and improve the quality of life.
Palliative radiotherapy It is radiotherapy performed on an incurable cancer that are not expected to cure the cancer but to control symptoms and improve the quality of life.

Geriatric care A specialty that focuses on health care of elderly people.
Why is it important ■ Some geriatric patients experience mental deterioration that impairs the ability to make informed decisions.
What decisions need to be taken for terminally ill patients ■ Decision to withhold or withdraw aggressive treatment that has no net benefit. ■ Do not resuscitate (DNR). ■ Withdraw support for patients on artificial life support. ■ Organ donation.
Who makes decisions for terminally ill patients 1 - The patient ■ A competent terminal patient must take his/her own decisions. ■ Competent patient: A person who has the intellectual/cognitive capacity to understand act on the information he/she is given. ■ A patient should sign a statement of what should be done after loss of consciousness. ■ It is recommended that health care workers discuss the decisions with the patient.
When a patient loses the capacity for decision making, he/she loses the right to autonomy and a substitute decision maker has to make the necessary decisions.
Who makes decisions for terminally ill patients 2 - A proxy decision maker A person chosen by the patient to take decisions for him/her when he/she is unable to take decisions.
Who makes decisions for terminally ill patients 3 - A substitute decision maker If no proxy decision maker was previously designated a substitute decision maker is chosen in the following order: 1. A member of the family. 2. Emergency situations: a doctor. 3. Non-emergency situations: A governmental authority (court or hospital administrative)
ANY QUESTIONS?
Case scenario 1 A thoracic surgeon wanted to carry out a de-bulking operation to decrease lung cancer mass to enable the patient to breathe easier; he told the patient of the high risk of death from hemorrhage. The 85 -year-old patient was drowsy because of medication and was suspected of suffering from dementia. The doctor was not sure whether the patient was capable of understanding the explanations given and making serious decisions about the operation, and the patient had no relatives nearby.
Case scenario 2 A 30 -year-old patient with multiple sclerosis had 5 of good health, and designated her husband as the decision maker. When she lost consciousness, the doctors needed a decision whether to put her on life support. The husband, who had remarried by then and lived in a separate house, decided against life support because it would prolong her suffering. Her father intervened and decided for life support because that would be in her best interests.
Case scenario 3 A 90 -year-old in ICU with stage 4 widely metastasized cancer and multi-organ failure was told by the doctors that there was nothing they could do to reverse the course of the disease, and that they could only provide symptomatic treatment. He asked to be discharged to die at home. His children objected, saying that he needed complex nursing that they could not provide at home.

Reference Hussein GM, Alkabba AF, Kasule OH. Professionalism and Ethics Handbook for Residents (PEHR): A Practical Guide. Ware J, Kattan T (eds). 1 st Edition. Riyadh, Saudi Arabia: Saudi Commission for Health Specialties, 2015.
- Slides: 27