BMDAS 5005160115 Indications for Use The ARCTIC SUN

BMD/AS 50/0516/0115
Indications for Use: The ARCTIC SUN® Temperature Management System is a thermal regulating system, indicated for monitoring and controlling patient temperature in adult and pediatric patients of all ages. Contraindications There are no known contraindications for the use of a non-invasive thermoregulatory system. Do not place ARCTICGEL™ Pads on skin that has signs of ulcerations, burns, hives or rash. Do not remove the fabric release liner of the Neonatal ARCTICGEL™ Pad and expose the hydrogel. Do not place ARCTICGEL™ Pads on immature (non-keratinized) skin or premature babies. While there are no known allergies to hydrogel materials, caution should be exercised with any patient with a history of skin allergies or sensitivities. Warnings When using the ARCTIC SUN® Temperature Management System, note that all othermal conductive systems, in use while warming or cooling with this device may interfere with patient temperature control. Cautions Due to underlying medical or physiological conditions, some patients are more susceptible to skin damage from pressure and heat or cold. Patients at risk include those with poor tissue perfusion or poor skin integrity due to edema, diabetes, peripheral vascular disease, poor nutritional status, steroid use or high dose vasopressor therapy. Examine the patient’s skin under the A RCTICGEL™ Pads. Skin injury may occur as a cumulative result of pressure, time and temperature. Carefully remove ARCTICGEL™ Pads from the patient’s skin at the completion of use. Aggressive removal or removal of cold pads from the patient’s skin may result in skin tears. The rate of temperature change and potentially the final achievable patient temperature is affected by many factors. Treatment application, monitoring and results are the responsibility of the attending physician. If the patient does not reach target temperature in a reasonable time or the patient is not able to be maintained at the target temperature, the skin may be exposed to low or high water temperatures for an extended period of time which may increase the risk for skin injury. Please consult package insert for more detailed safety information and instructions for use. BMD/AS 50/0516/0115
Disclosure Product Training and Education: Any discussion regarding BARD® products during this presentation is limited to information that is consistent with BARD® labeling for these products. BMD/AS 50/0516/0115
Learning Objectives Upon completion of this module, the participant will be able to: • Recognize role of Targeted Temperature Management (TTM) • Review TTM evidence-based practice • Discuss patient management during TTM • Identifying and addressing shivering • Fever control BMD/AS 50/0516/0115

Why are we here today? BMD/AS 50/0516/0115
Pathophysiology BMD/AS 50/0516/0115
Global Ischemia • Transient (5 – 30 minutes) complete or nearly complete lack of blood flow • Lack of blood supply leads to ischemia • If blood flow is not restored within 30 minutes, widespread necrosis occurs Polderman, KH. (2004). Int Care Med. 30(4), 556 -575. BMD/AS 50/0516/0115
Focal Ischemia • Results from occlusion of a single cerebral blood vessel • Necrosis occurs near the occluded vessel if reperfusion does not occur within 60 min • Surrounding area (penumbra) may be salvaged if reperfusion occurs Polderman, KH. (2004). Int Care Med. 30(4), 556 -575. BMD/AS 50/0516/0115
Neuronal Damage from Ischemia • Complex negative cascade of reactions at cellular level • May begin minutes after injury and continue up to 72 hours or longer • Chain of events is called secondary injury or reperfusion injury Polderman, KH. (2008). Lancet. 371, 1955 -69. BMD/AS 50/0516/0115
Ischemic Cascade 1 -3 • Mitochondrial dysfunction • Release of excitatory neurotransmitter glutamate • Excess release of calcium • Disruption of cell membranes • Free radical production • Blood brain barrier dysfunction 1. Polderman, KH. (2008). Lancet. 371, 1955 -69. 2. Lee, K (2012). The Neuro. ICU Book. New York: Mc. Graw Hill Companies, Inc. p. 192. 3. Malhotra, R. & Lee, K. (2012). The Neuro ICU Book. New York: Mc. Graw Hill Companies, Inc. pp. 188 -201. BMD/AS 50/0516/0115
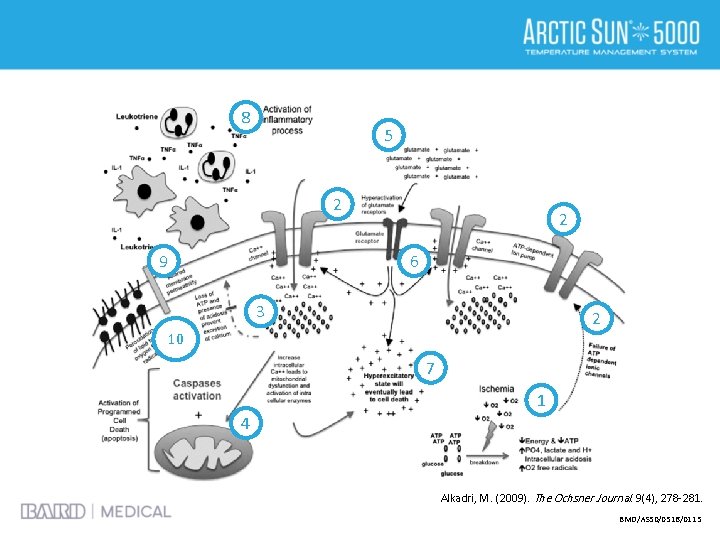
8 5 2 9 2 6 3 2 10 7 1 4 Alkadri, M. (2009). The Ochsner Journal. 9(4), 278 -281. BMD/AS 50/0516/0115

“preventing ischemic injury is central to all neuroprotective strategies” Polderman, KH. (2008). Lancet. 371, 1955 -69. BMD/AS 50/0516/0115

Targeted Temperature and Patient Management BMD/AS 50/0516/0115
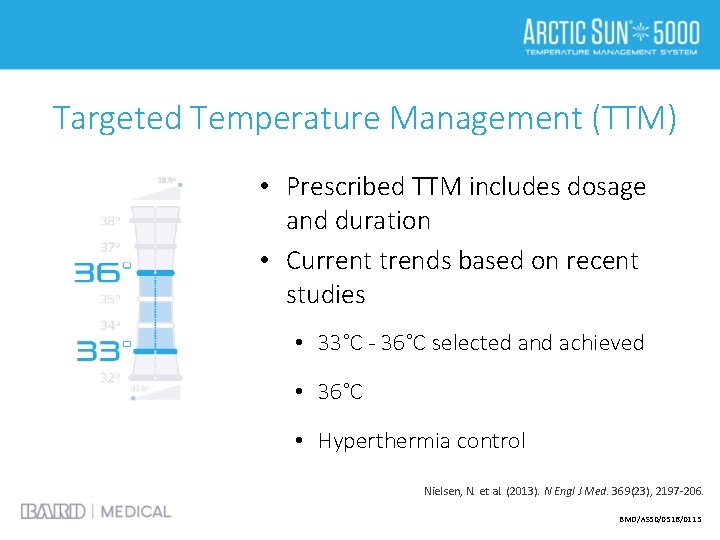
Targeted Temperature Management (TTM) • Prescribed TTM includes dosage and duration • Current trends based on recent studies • 33°C - 36°C selected and achieved • 36°C • Hyperthermia control Nielsen, N. et al. (2013). N Engl J Med. 369(23), 2197 -206. BMD/AS 50/0516/0115
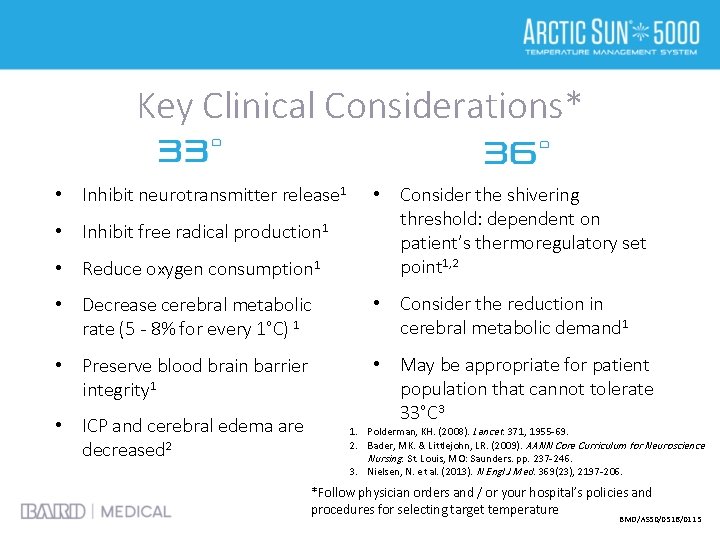
Key Clinical Considerations* • Inhibit neurotransmitter release 1 • Reduce oxygen consumption 1 • Consider the shivering threshold: dependent on patient’s thermoregulatory set point 1, 2 • Decrease cerebral metabolic rate (5 - 8% for every 1°C) 1 • Consider the reduction in cerebral metabolic demand 1 • Preserve blood brain barrier integrity 1 • May be appropriate for patient population that cannot tolerate 33°C 3 • Inhibit free radical production 1 • ICP and cerebral edema are decreased 2 1. Polderman, KH. (2008). Lancet. 371, 1955 -69. 2. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 3. Nielsen, N. et al. (2013). N Engl J Med. 369(23), 2197 -206. *Follow physician orders and / or your hospital’s policies and procedures for selecting target temperature BMD/AS 50/0516/0115
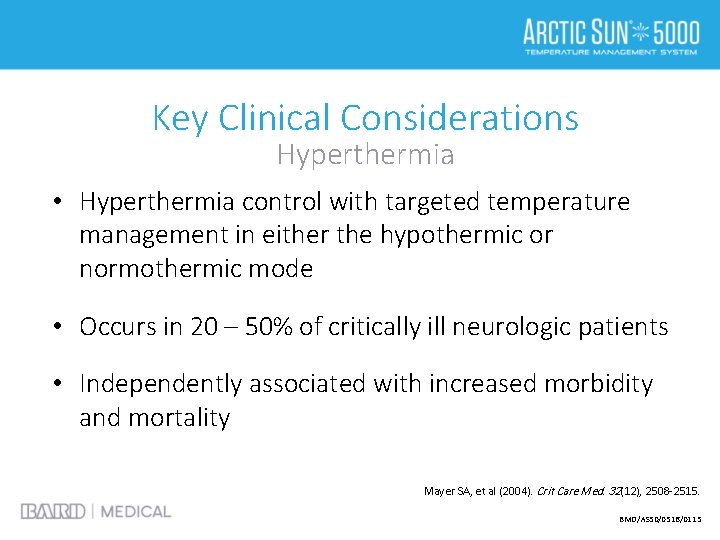
Key Clinical Considerations Hyperthermia • Hyperthermia control with targeted temperature management in either the hypothermic or normothermic mode • Occurs in 20 – 50% of critically ill neurologic patients • Independently associated with increased morbidity and mortality Mayer SA, et al (2004). Crit Care Med. 32(12), 2508 -2515. BMD/AS 50/0516/0115
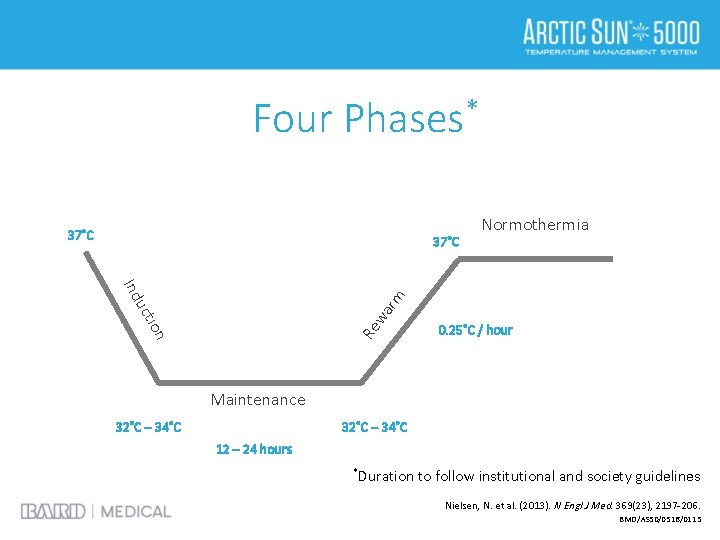
Four Phases* 37˚C Ind Re ion wa uct rm Normothermia 0. 25˚C / hour Maintenance 32˚C – 34˚C 12 – 24 hours *Duration to follow institutional and society guidelines Nielsen, N. et al. (2013). N Engl J Med. 369(23), 2197 -206. BMD/AS 50/0516/0115
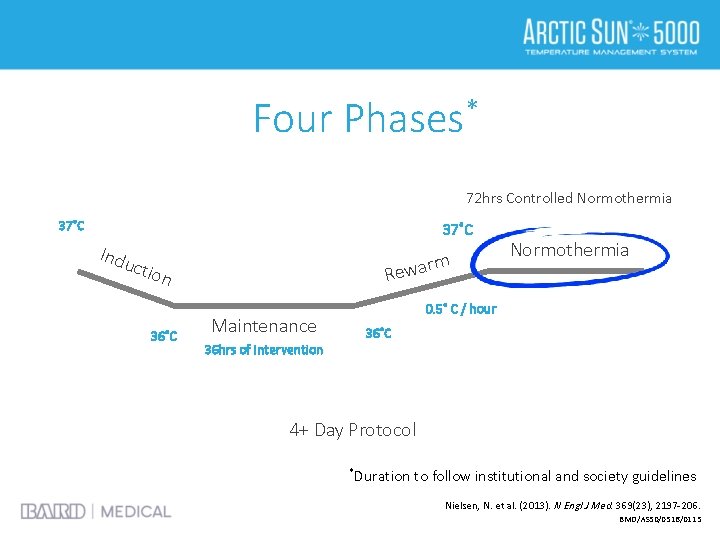
Four Phases* 72 hrs Controlled Normothermia 37˚C Indu rm Rewa ctio n 36˚C Maintenance 36 hrs of Intervention Normothermia 0. 5˚ C / hour 36˚C 4+ Day Protocol *Duration to follow institutional and society guidelines Nielsen, N. et al. (2013). N Engl J Med. 369(23), 2197 -206. BMD/AS 50/0516/0115

Four Phases* 37˚C Normothermia ion wa rm uct Ind 32˚C – 36˚C Re Time to Initiation 0. 25˚C / 16 hrs Maintenance 24 hours *Duration to follow institutional and society guidelines Nielsen, N. et al. (2013). N Engl J Med. 369(23), 2197 -206. BMD/AS 50/0516/0115
What’s the latest news in the TTM field? 2010 Comatose adult patients with ROSC should be cooled to 32°C to 34°C for 12 to 24 hours Field, JM. et al (2010). Circulation. 122(18): S 640 -S 664. BMD/AS 50/0516/0115
What’s the latest news in the TTM field? 2010 Comatose adult patients with ROSC should be cooled to 32°C to 34°C for 12 to 24 hours 2015 All comatose adult patients with ROSC should have TTM… 1. Field, JM. et al (2010). Circulation. 122(18): S 640 -S 664. 2. Neumar, RW. et al (2015). Circulation. 132: S 313 -S 367. BMD/AS 50/0516/0115
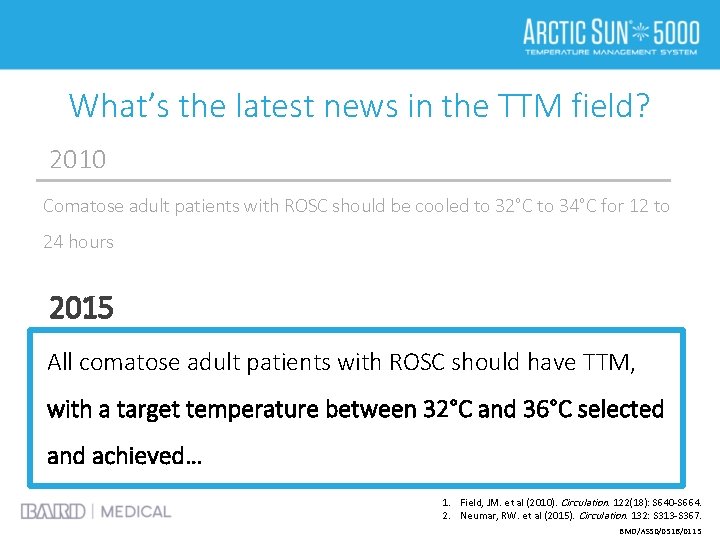
What’s the latest news in the TTM field? 2010 Comatose adult patients with ROSC should be cooled to 32°C to 34°C for 12 to 24 hours 2015 All comatose adult patients with ROSC should have TTM, with a target temperature between 32°C and 36°C selected and achieved… 1. Field, JM. et al (2010). Circulation. 122(18): S 640 -S 664. 2. Neumar, RW. et al (2015). Circulation. 132: S 313 -S 367. BMD/AS 50/0516/0115

What’s the latest news in the TTM field? 2010 Comatose adult patients with ROSC should be cooled to 32°C to 34°C for 12 to 24 hours 2015 All comatose adult patients with ROSC should have TTM, with a target temperature between 32°C and 36°C selected and achieved, then maintained constantly for 24 hours 1. Field, JM. et al (2010). Circulation. 122(18): S 640 -S 664. 2. Neumar, RW. et al (2015). Circulation. 132: S 313 -S 367. BMD/AS 50/0516/0115
What’s the latest news in the TTM field? Select and Maintain • Specific conditions of the patient may favor selection of one temperature over another • Allowing patients to warm above 36°C would be inconsistent with current TTM recommendations Neumar, RW. et al (2015). Circulation. 132: S 313 -S 367. BMD/AS 50/0516/0115
What’s the latest news in the TTM field? Prehospital Initiation Routine prehospital cooling of patients after ROSC with rapid infusion of cold intravenous fluids is no longer recommended Neumar, RW. et al (2015). Circulation. 132: S 313 -S 367. BMD/AS 50/0516/0115
What’s the latest news in the TTM field? Actively Preventing Fever • Fever has the potential of worsening ischemic injury • Actively preventing fever in comatose patients after TTM • The simplest method to prolonged hyperthermia prevention may be to leave the devices / strategies used for TTM in place Neumar, RW. et al (2015). Circulation. 132: S 313 -S 367. BMD/AS 50/0516/0115
Physiological Effects of Therapeutic Hypothermia* Cardiovascular • ↓ BP, HR, CO 1 -3 • EKG Changes – Prolonged PR interval 1, 2 – Widening QRS complex 1, 2 – Increased QT wave 1, 2 – J or Osborn wave 1 *Representative of target temperatures 32 - 35°C 1. Mehta, S. (2010). PA: HMP Communications. pp. 603 -612. 2. Nunnally, ME. (2010). Mount Prospect: SCCM. pp. 21 -27. 3. Tischerman, SA. & Stertz, F. (2010). New York: Springer Science. pp. 235 -246. BMD/AS 50/0516/0115
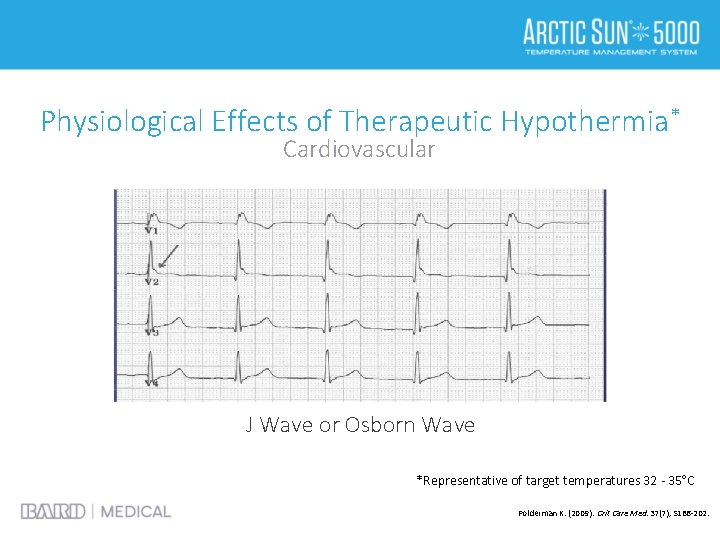
Physiological Effects of Therapeutic Hypothermia* Cardiovascular J Wave or Osborn Wave *Representative of target temperatures 32 - 35°C Polderman K. (2009). Crit Care Med. 37(7), S 186 -202.
Physiological Effects of Therapeutic Hypothermia* • Hematological 1 – Impaired clotting cascade – Impaired platelet function: potential increase in bleeding risk – Decreased WBC count • Renal – ↑ Diuresis 2, 4 – Electrolyte loss 3 • Gastrointestinal 1 – Impaired bowel function / motility *Representative of target temperatures 32 - 35°C 1. Mehta, S. (2010). PA: HMP Communications. pp. 603 -612. 2. Bader MK and Littlejohn LR (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 3. Nunnally, ME. (2010). Mount Prospect: SCCM. pp. 21 -27. 4. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
Physiological Effects of Therapeutic Hypothermia* • Systemic – ↓ O 2 consumption and CO 2 production 1, 3 – Left shift on oxyhemoglobin curve: O 2 is not readily released to the tissues 4 – Lactic acidosis 4 • Endocrine 1, 3 – ↓ Insulin secretion • Immune suppression 1 – ↑ Infection: wound infections and pneumonia • Other 1 – Shivering – Drug metabolism prolonged *Representative of target temperatures 32 - 35°C 1. Mehta, S. (2010). PA: HMP Communications. pp. 603 -612. 2. Bader MK and Littlejohn LR (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 3. Nunnally, ME. (2010). Mount Prospect: SCCM. pp. 21 -27. 4. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115

Shivering • A physiological reflex mechanism that occurs when the body needs to produce or maintain heat • The primary center for shivering is found in the posterior hypothalamus Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. BMD/AS 50/0516/0115
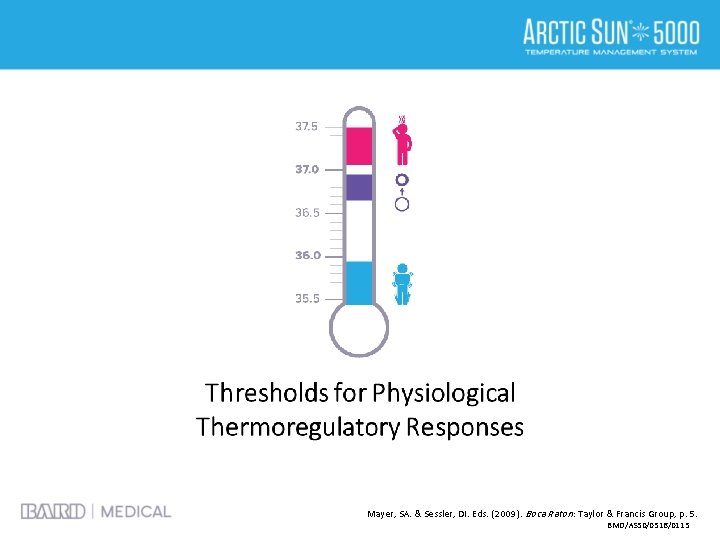
Mayer, SA. & Sessler, DI. Eds. (2009). Boca Raton : Taylor & Francis Group, p. 5. BMD/AS 50/0516/0115
Shivering • Involuntary sympathetic response to generate heat 4 – Vasoconstriction – Piloerection • Leads to increased: 1 -4 – Metabolic rate – Metabolic demand – Oxygen consumption – Carbon dioxide production 1. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 2. Lee, K (2012). The Neuro. ICU Book. New York: Mc. Graw Hill Companies, Inc. p. 192. 3. Nunnally, ME. (2010). Mount Prospect: SCCM. pp. 21 -27. 4. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
Shivering Management • Counter warming is the first line therapy for shivering treatment 1 • Sedation prevents increased metabolism 1 • Paralytic agents affect shivering 1 -3 Precautions: difficult to identify seizures, select agent with anticonvulsant properties, continuous EEG may be utilized, drug metabolism is affected, appropriate dosing must be tailored to the specific conditions of the patients and must be tightly monitored 1. Mehta, S. (2010). PA: HMP Communications. pp. 603 -612. 2. Nunnally, ME. (2010). Mount Prospect: SCCM. pp. 21 -27. 3. Lee, K (2012). The Neuro. ICU Book. New York: Mc. Graw Hill Companies, Inc. p. 192. BMD/AS 50/0516/0115
Phases of Therapy Induction Phase • Careful monitoring of fluid balance • Glucose control • Monitor for hypertension • Electrolyte management • Prevention of shivering General Considerations: This list may vary depending on the patient’s underlying condition. 1. 2. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
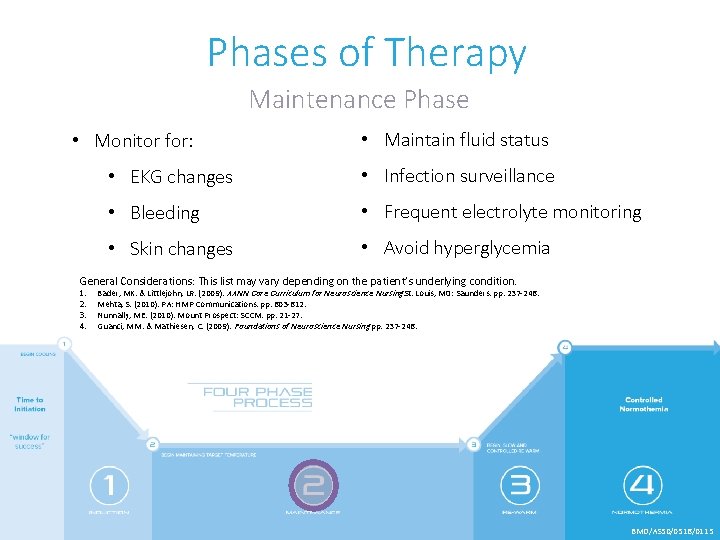
Phases of Therapy Maintenance Phase • Monitor for: • Maintain fluid status • EKG changes • Infection surveillance • Bleeding • Frequent electrolyte monitoring • Skin changes • Avoid hyperglycemia General Considerations: This list may vary depending on the patient’s underlying condition. 1. 2. 3. 4. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. Mehta, S. (2010). PA: HMP Communications. pp. 603 -612. Nunnally, ME. (2010). Mount Prospect: SCCM. pp. 21 -27. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
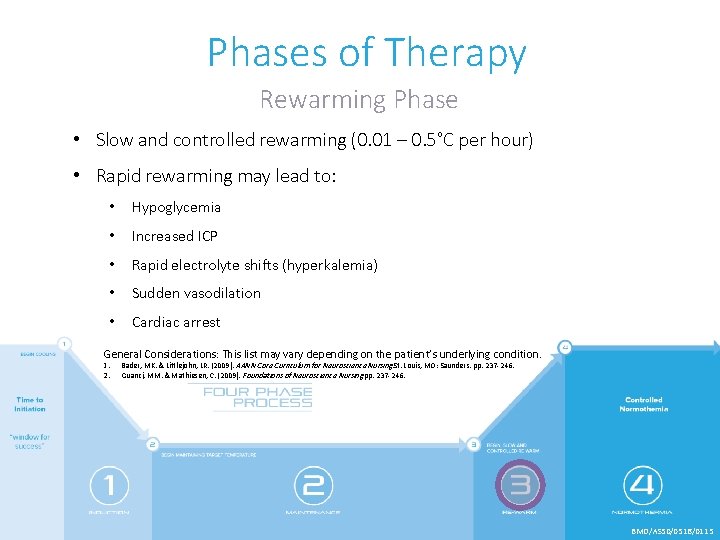
Phases of Therapy Rewarming Phase • Slow and controlled rewarming (0. 01 – 0. 5°C per hour) • Rapid rewarming may lead to: • Hypoglycemia • Increased ICP • Rapid electrolyte shifts (hyperkalemia) • Sudden vasodilation • Cardiac arrest General Considerations: This list may vary depending on the patient’s underlying condition. 1. 2. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
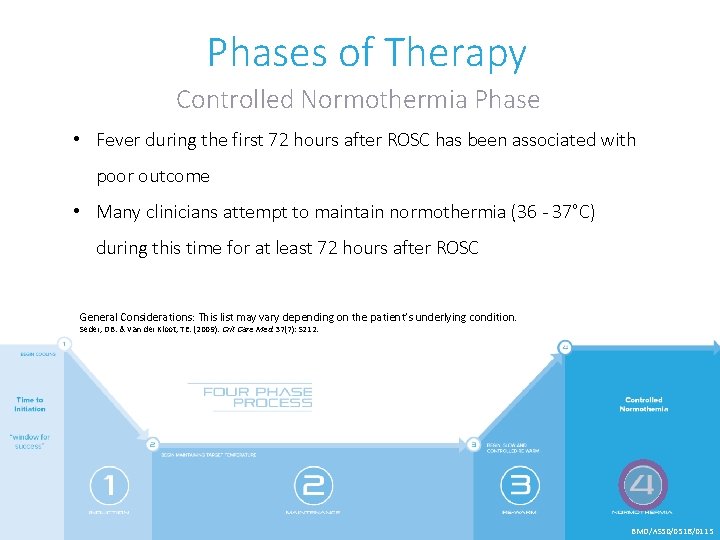
Phases of Therapy Controlled Normothermia Phase • Fever during the first 72 hours after ROSC has been associated with poor outcome • Many clinicians attempt to maintain normothermia (36 - 37°C) during this time for at least 72 hours after ROSC General Considerations: This list may vary depending on the patient’s underlying condition. Seder, DB. & Van der Kloot, TE. (2009). Crit Care Med. 37(7): S 212. BMD/AS 50/0516/0115

Neuroprognostication • TTM alters the ability to obtain a clinical neuro exam • Drug clearance is decreased so sedatives may be present up to 48 - 72 hours • Decisions regarding withdrawal of care must be delayed until adequate clinical exam can be performed • Follow your institution’s guidelines for prognostication 1. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 2. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. 3. Blondin, NA. , & Greer, DM. (2011). The Neurologist. 17(5): 241 -248. BMD/AS 50/0516/0115

Controlled Normothermia BMD/AS 50/0516/0115
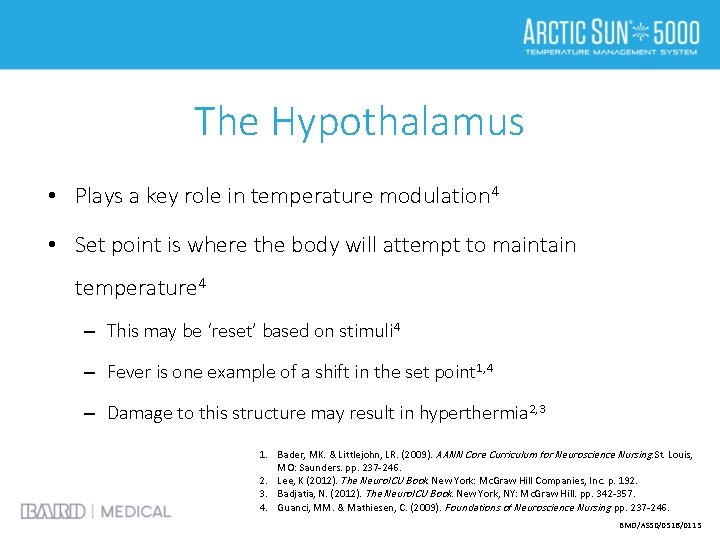
The Hypothalamus • Plays a key role in temperature modulation 4 • Set point is where the body will attempt to maintain temperature 4 – This may be ‘reset’ based on stimuli 4 – Fever is one example of a shift in the set point 1, 4 – Damage to this structure may result in hyperthermia 2, 3 1. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 2. Lee, K (2012). The Neuro. ICU Book. New York: Mc. Graw Hill Companies, Inc. p. 192. 3. Badjatia, N. (2012). The Neuro. ICU Book. New York, NY: Mc. Graw Hill. pp. 342 -357. 4. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
Prevalence of Hyperthermia • Defined as temperature > 38°C • Occurs in up to 50% of all neurologically-injured patients What is your institution’s definition of a fever? Mayer, SA. & Sessler, DI. Eds. (2009). Boca Raton : Taylor & Francis Group, p. 5. BMD/AS 50/0516/0115

Fever and Brain Injury • Fever after trauma or ischemia may exacerbate damage from the original insult 2 • Hyperthermia may worsen damage after focal and global ischemia 2 • As high as 13% ↑ in metabolic rate associated with every 1°C ↑ in body temperature 1 1. Thompson HJ, Pinto-Martin J & Bullock MR. (2003). J Neurol Neurosug Psychiatry. 74: 614. 2. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
Fever and Hemorrhage • Intraventricular hemorrhage is a strong risk factor fever development 3 • A small amount of blood in CSF may induce fever 3, 4 • Fever has been associated with cerebral vasospasm 1 -3 1. 2. 3. 4. Lee, K. (2012). The Neuro. ICU Book. New York: Mc. Graw Hill Companies, Inc. p. 192. Patel, NC. et al (2010). Textbook of STEMI interventions. Malvern, PA: HMP Communications. pp. 603 -612. Badjatia, N. (2012). The Neuro. ICU Book. New York, NY: Mc. Graw Hill. pp. 342 -357. Lenhardt, R. (2005). Therapeutic Hypothermia. Monticello, NY: Marcel Dekker. BMD/AS 50/0516/0115
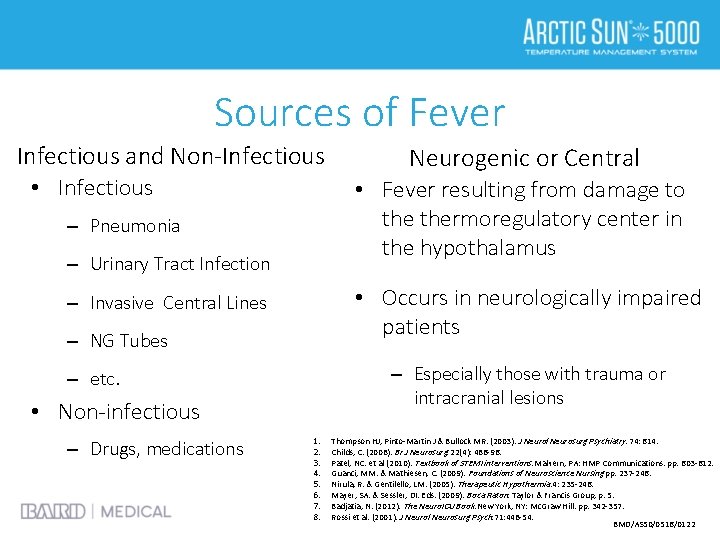
Sources of Fever Infectious and Non-Infectious • Infectious • Fever resulting from damage to thermoregulatory center in the hypothalamus – Pneumonia – Urinary Tract Infection • Occurs in neurologically impaired patients – Invasive Central Lines – NG Tubes – Especially those with trauma or intracranial lesions – etc. • Non-infectious – Drugs, medications Neurogenic or Central 1. 2. 3. 4. 5. 6. 7. 8. Thompson HJ, Pinto-Martin J & Bullock MR. (2003). J Neurol Neurosurg Psychiatry. 74: 614. Childs, C. (2008). Br J Neurosurg. 22(4): 486 -96. Patel, NC. et al (2010). Textbook of STEMI interventions. Malvern, PA: HMP Communications. pp. 603 -612. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. Nirula, R. & Gentilello, LM. (2005). Therapeutic Hypothermia. 4: 235 -246. Mayer, SA. & Sessler, DI. Eds. (2009). Boca Raton: Taylor & Francis Group, p. 5. Badjatia, N. (2012). The Neuro. ICU Book. New York, NY: Mc. Graw Hill. pp. 342 -357. Rossi et al. (2001). J Neurol Neurosurg Psych. 71: 448 -54. BMD/AS 50/0516/0122
Understanding the Effects of Temperature Management BMD/AS 50/0516/0115
METABOLIC DEMAND °C °F BMD/AS 50/0516/0115
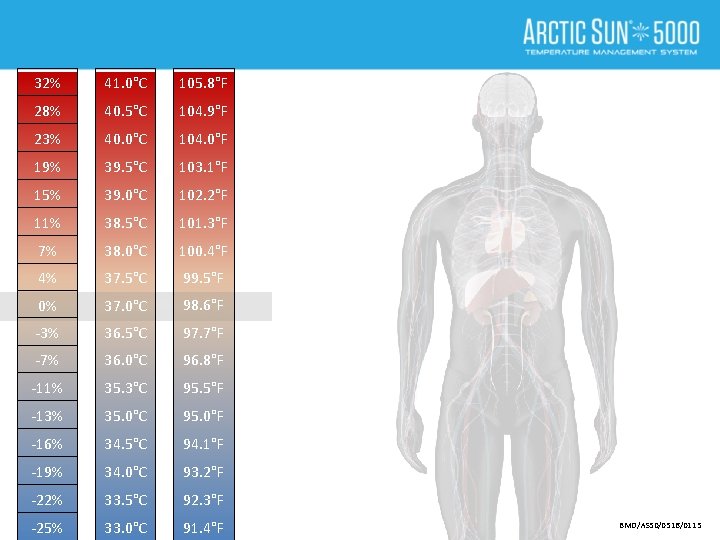
32% 41. 0°C 105. 8°F 28% 40. 5°C 104. 9°F 23% 40. 0°C 104. 0°F 19% 39. 5°C 103. 1°F 15% 39. 0°C 102. 2°F 11% 38. 5°C 101. 3°F 7% 38. 0°C 100. 4°F 4% 37. 5°C 99. 5°F 0% 37. 0°C 98. 6°F -3% 36. 5°C 97. 7°F -7% 36. 0°C 96. 8°F -11% 35. 3°C 95. 5°F -13% 35. 0°C 95. 0°F -16% 34. 5°C 94. 1°F -19% 34. 0°C 93. 2°F -22% 33. 5°C 92. 3°F -25% 33. 0°C 91. 4°F BMD/AS 50/0516/0115

32% 41. 0°C 105. 8°F 28% 40. 5°C 104. 9°F 23% 40. 0°C 104. 0°F 19% 39. 5°C 103. 1°F 15% 39. 0°C 102. 2°F 11% 38. 5°C 101. 3°F 7% 38. 0°C 100. 4°F 4% 37. 5°C 99. 5°F 0% 37. 0°C 98. 6°F -3% 36. 5°C 97. 7°F -7% 36. 0°C 96. 8°F -11% 35. 3°C 95. 5°F -13% 35. 0°C 95. 0°F -16% 34. 5°C 94. 1°F -19% 34. 0°C 93. 2°F -22% 33. 5°C 92. 3°F -25% 33. 0°C 91. 4°F UNCONTROLLED HYPERTHERMIA Increases Metabolic Demand Increases Risk of Cerebral Edema Increases Length of Stay BMD/AS 50/0516/0115

32% 41. 0°C 105. 8°F 28% 40. 5°C 104. 9°F 23% 40. 0°C 104. 0°F 19% 39. 5°C 103. 1°F 15% 39. 0°C 102. 2°F 11% 38. 5°C 101. 3°F 7% 38. 0°C 100. 4°F 4% 37. 5°C 99. 5°F 0% 37. 0°C 98. 6°F -3% 36. 5°C 97. 7°F -7% 36. 0°C 96. 8°F -11% 35. 3°C 95. 5°F -13% 35. 0°C 95. 0°F -16% 34. 5°C 94. 1°F -19% 34. 0°C 93. 2°F -22% 33. 5°C 92. 3°F -25% 33. 0°C 91. 4°F UNCONTROLLED HYPERTHERMIA BMD/AS 50/0516/0115

32% 41. 0°C 105. 8°F 28% 40. 5°C 104. 9°F 23% 40. 0°C 104. 0°F 19% 39. 5°C 103. 1°F 15% 39. 0°C 102. 2°F 11% 38. 5°C 101. 3°F 7% 38. 0°C 100. 4°F 4% 37. 5°C 99. 5°F 0% 37. 0°C 98. 6°F -3% 36. 5°C 97. 7°F -7% 36. 0°C 96. 8°F -11% 35. 3°C 95. 5°F -13% 35. 0°C 95. 0°F -16% 34. 5°C 94. 1°F -19% 34. 0°C 93. 2°F -22% 33. 5°C 92. 3°F -25% 33. 0°C 91. 4°F UNCONTROLLED HYPERTHERMIA Blankets / Wraps / Tylenol BMD/AS 50/0516/0115
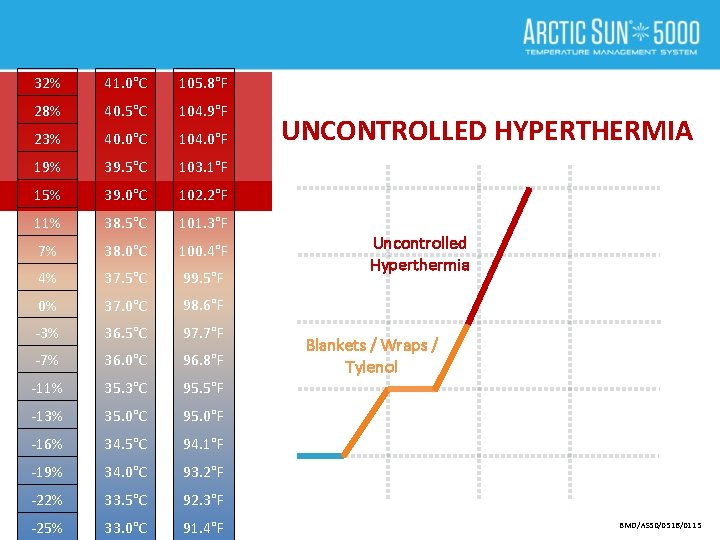
32% 41. 0°C 105. 8°F 28% 40. 5°C 104. 9°F 23% 40. 0°C 104. 0°F 19% 39. 5°C 103. 1°F 15% 39. 0°C 102. 2°F 11% 38. 5°C 101. 3°F 7% 38. 0°C 100. 4°F 4% 37. 5°C 99. 5°F 0% 37. 0°C 98. 6°F -3% 36. 5°C 97. 7°F -7% 36. 0°C 96. 8°F -11% 35. 3°C 95. 5°F -13% 35. 0°C 95. 0°F -16% 34. 5°C 94. 1°F -19% 34. 0°C 93. 2°F -22% 33. 5°C 92. 3°F -25% 33. 0°C 91. 4°F UNCONTROLLED HYPERTHERMIA Uncontrolled Hyperthermia Blankets / Wraps / Tylenol BMD/AS 50/0516/0115
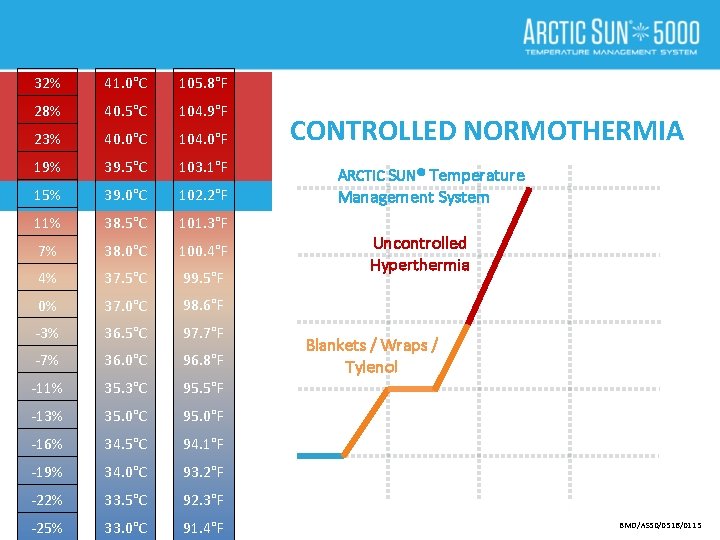
32% 41. 0°C 105. 8°F 28% 40. 5°C 104. 9°F 23% 40. 0°C 104. 0°F 19% 39. 5°C 103. 1°F 15% 39. 0°C 102. 2°F 11% 38. 5°C 101. 3°F 7% 38. 0°C 100. 4°F 4% 37. 5°C 99. 5°F 0% 37. 0°C 98. 6°F -3% 36. 5°C 97. 7°F -7% 36. 0°C 96. 8°F -11% 35. 3°C 95. 5°F -13% 35. 0°C 95. 0°F -16% 34. 5°C 94. 1°F -19% 34. 0°C 93. 2°F -22% 33. 5°C 92. 3°F -25% 33. 0°C 91. 4°F CONTROLLED NORMOTHERMIA ARCTIC SUN® Temperature Management System Uncontrolled Hyperthermia Blankets / Wraps / Tylenol BMD/AS 50/0516/0115

32% 41. 0°C 105. 8°F 28% 40. 5°C 104. 9°F 23% 40. 0°C 104. 0°F 19% 39. 5°C 103. 1°F 15% 39. 0°C 102. 2°F 11% 38. 5°C 101. 3°F 7% 38. 0°C 100. 4°F 4% 37. 5°C 99. 5°F 0% 37. 0°C 98. 6°F -3% 36. 5°C 97. 7°F -7% 36. 0°C 96. 8°F -11% 35. 3°C 95. 5°F -13% 35. 0°C 95. 0°F -16% 34. 5°C 94. 1°F -19% 34. 0°C 93. 2°F -22% 33. 5°C 92. 3°F -25% 33. 0°C 91. 4°F CONTROLLED NORMOTHERMIA ARCTIC SUN® Temperature Management System Uncontrolled Hyperthermia Fever is Broken Blankets / Wraps / Tylenol BMD/AS 50/0516/0115
Uncontrolled Hyperthermia The Evidence Suggests Uncontrolled Hyperthermia Fever is Broken Blankets / Wraps / Tylenol BMD/AS 50/0516/0115
Uncontrolled Hyperthermia The Evidence Suggests Uncontrolled Hyperthermia Fever is Broken Blankets / Wraps / Tylenol BMD/AS 50/0516/0115
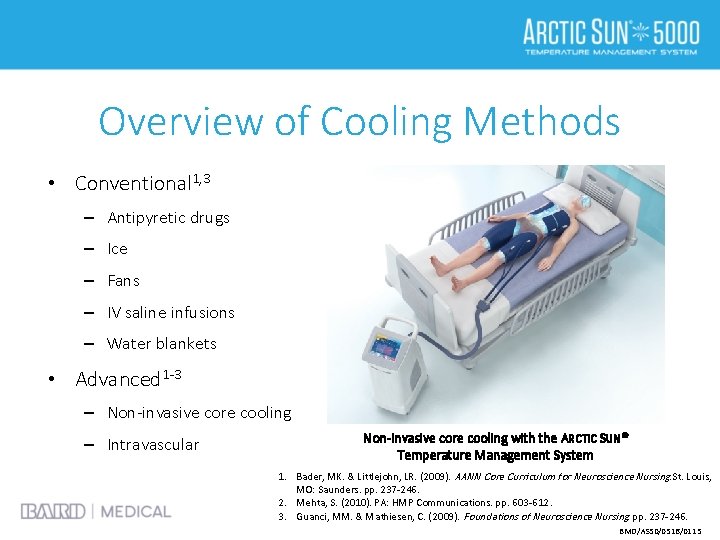
Overview of Cooling Methods • Conventional 1, 3 – Antipyretic drugs – Ice – Fans – IV saline infusions – Water blankets • Advanced 1 -3 – Non-invasive core cooling – Intravascular Non-invasive core cooling with the ARCTIC SUN® Temperature Management System 1. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 2. Mehta, S. (2010). PA: HMP Communications. pp. 603 -612. 3. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
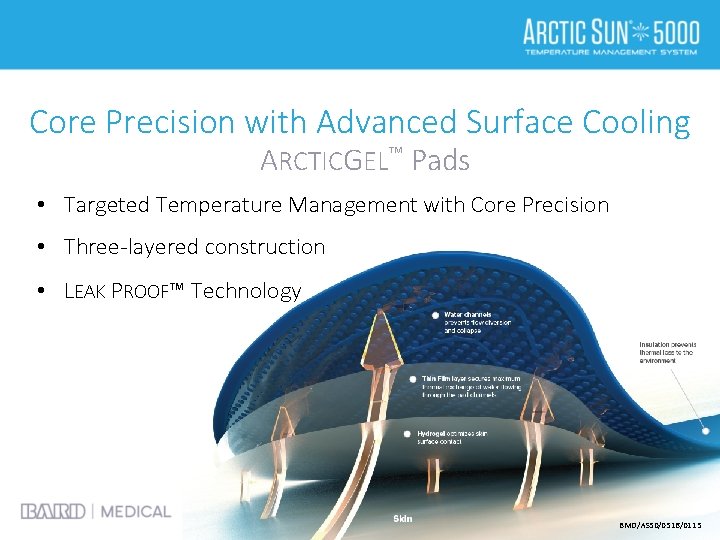
Core Precision with Advanced Surface Cooling ARCTICGEL™ Pads • Targeted Temperature Management with Core Precision • Three-layered construction • LEAK PROOF™ Technology BMD/AS 50/0516/0115
Nursing Management for Fever • When fever occurs, appropriate diagnostics are needed to ascertain possible etiology 2 • Refractory fever >1 -2 hrs needs aggressive management 2 • Institute shivering management strategies 2 • Monitor fever burden 1 1. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 2. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
Shivering • Set point has been reset 2 • Patients will shiver even when goal is normothermia 2 • Assessment and control of shivering is imperative 1 1. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 2. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
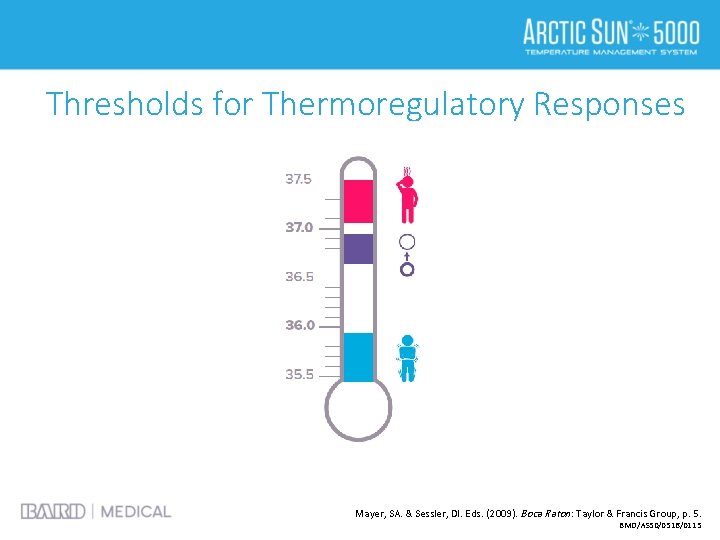
Thresholds for Thermoregulatory Responses Mayer, SA. & Sessler, DI. Eds. (2009). Boca Raton : Taylor & Francis Group, p. 5. BMD/AS 50/0516/0115
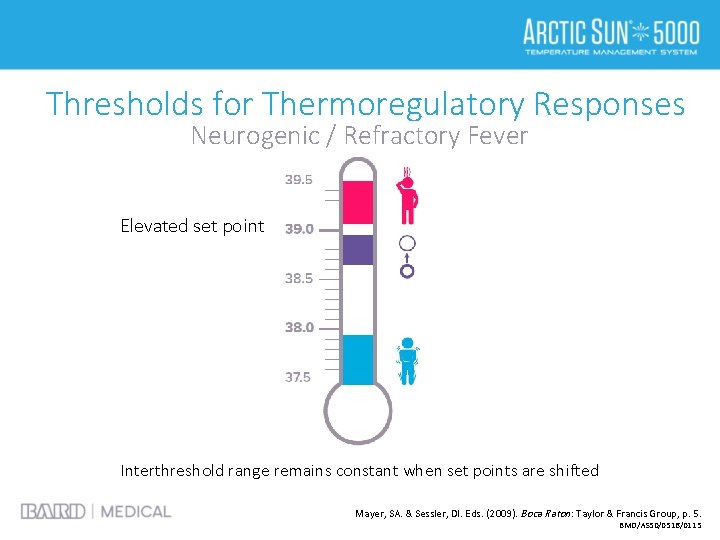
Thresholds for Thermoregulatory Responses Neurogenic / Refractory Fever Elevated set point Interthreshold range remains constant when set points are shifted Mayer, SA. & Sessler, DI. Eds. (2009). Boca Raton : Taylor & Francis Group, p. 5. BMD/AS 50/0516/0115
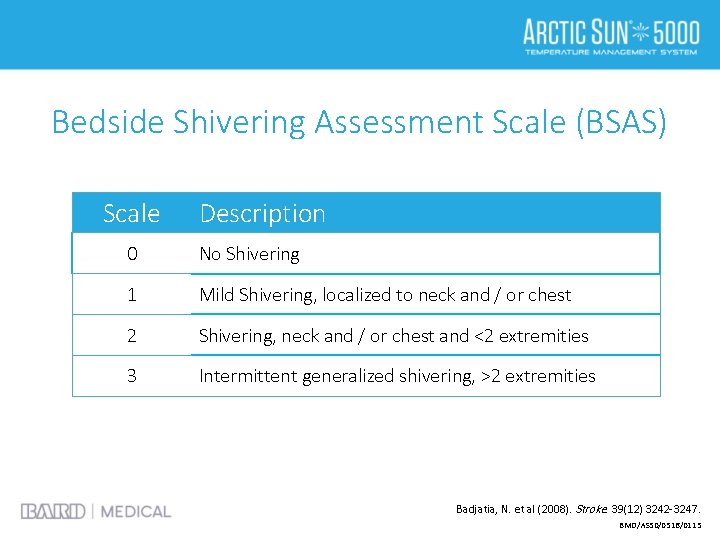
Bedside Shivering Assessment Scale (BSAS) Scale Description 0 No Shivering 1 Mild Shivering, localized to neck and / or chest 2 Shivering, neck and / or chest and <2 extremities 3 Intermittent generalized shivering, >2 extremities Badjatia, N. et al (2008). Stroke. 39(12) 3242 -3247. BMD/AS 50/0516/0115
Counter Warming • May reduce incidence of shivering 2 • Tricks skin receptors into believing the body is warm 2 • Warm air circulating may be used to cover these areas 1 1. Bader, MK. & Littlejohn, LR. (2009). AANN Core Curriculum for Neuroscience Nursing. St. Louis, MO: Saunders. pp. 237 -246. 2. Guanci, MM. & Mathiesen, C. (2009). Foundations of Neuroscience Nursing. pp. 237 -246. BMD/AS 50/0516/0115
Summary • It is important to properly manage patients receiving targeted temperature management • You must be dedicated to shivering control in order to effectively cool patients or to maintain normothermia • Fever in critically ill patients is associated with worse outcomes and length of stay BMD/AS 50/0516/0115
List of References • Badjatia N (2006). Curr Neurol Neurosci Rep. 6(6): 509 -517. • Badjatia NE, et al (2008). Stroke. 39(12): 3232 -3247. • Choi A, et al (2010). Neurocrit Care. 14(3): 389 -394. • Diringer MN, et al (2004). Crit Care Med. 32(7): 1489 -1495. • English MJ & Hemmerling TM (2008). European J Anaesthesiology. 25(7): 531 -537. • Greer DM, et al (2008). Stroke. 39: 3029 -3035. • Mayer SA, et al (2004). Crit Care Med. 32(12): 2508 -2515. • Merchant R (2006). Crit Care Med. 34(12): S 490 -S 494. • Nielsen N, et al (2013). N Engl J Med. 369(23): 2197 -206. • Peberdy, et al (2010) Circulation. 122(18 Suppl 3): S 768 -S 786. • Polderman K (2009). Crit Care Med. 37(7): S 186 -202. • Tomte O, et al (2011). Crit Care Med. 39(3): 443 -9. BMD/AS 50/0516/0115
- Slides: 66