BLS CPAP Continuous Positive Airway Pressure Objectives 1
BLS CPAP Continuous Positive Airway Pressure
Objectives 1. Why CPAP? 2. Respiratory A&P Review 3. How does CPAP work? 4. Indications 5. Contraindications 6. CPAP Methods

What is CPAP? ▪ Continuous Positive Airway Pressure ▪ A non-invasive alternative to intubation ▪ May reduce need for intubation by up to 60% ▪ Does not require any sedation ▪ It provides comfort to the patient with acute respiratory distress by reducing work of breathing
What is CPAP? ▪ Established therapeutic alternative ▪ Easily applied, easily discontinued ▪ CPAP is a viable alternative in many patients that need more than just supplemental 02, but don’t yet require intubation ▪ CPAP is not a cure; it is a bridge device.
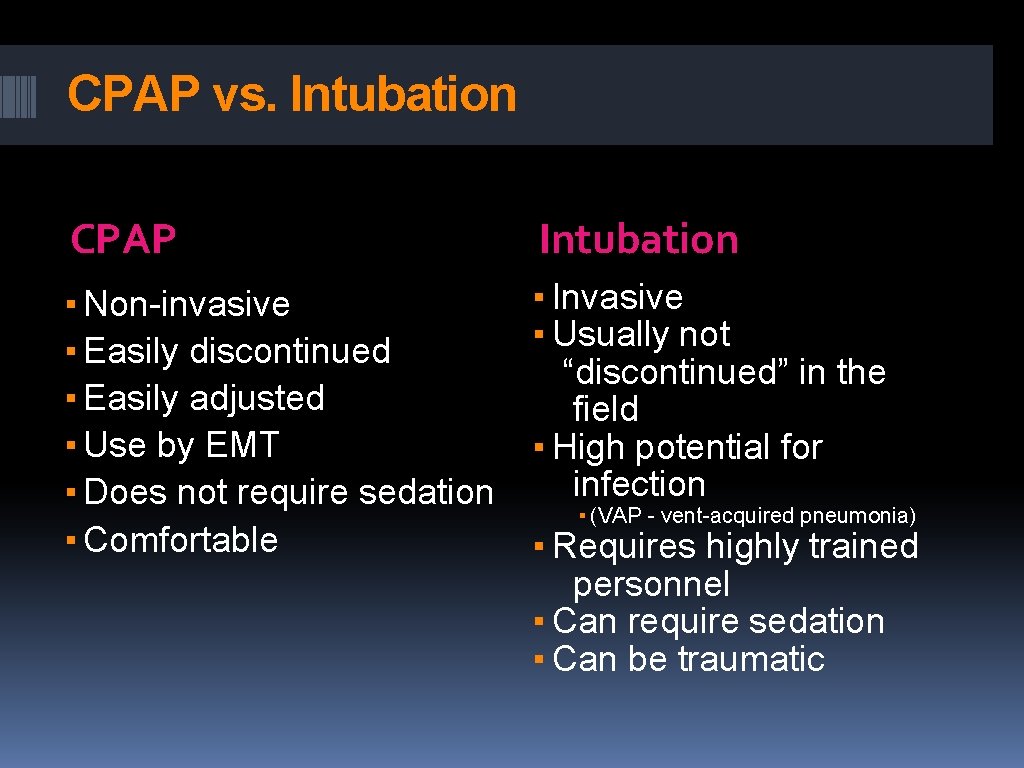
CPAP vs. Intubation CPAP Intubation ▪ Non-invasive ▪ Easily discontinued ▪ Easily adjusted ▪ Use by EMT ▪ Does not require sedation ▪ Comfortable ▪ Invasive ▪ Usually not “discontinued” in the field ▪ High potential for infection ▪ (VAP - vent-acquired pneumonia) ▪ Requires highly trained personnel ▪ Can require sedation ▪ Can be traumatic
Why BLS CPAP? ▪ “The primary question asked at the time was whether patients who received CPAP by BLS personnel would suffer greater complications than those given CPAP by paramedics. After a year of study, officials found no difference, and actually found that BLS use of CPAP helped reduce the need for ALS for these patients. In several cases during the pilot program, BLS agencies that used CPAP transported patients with COPD without an ALS intercept. This was because, despite being in their scope of practice, many ALS agencies didn’t have CPAP, and the patients had improved to such a degree that an ALS intercept and intervention was no longer needed. This also freed up ALS resources to respond to additional or more critical calls. ” ▪ “Bring it to the BLS: EMT-B success with CPAP requires education and training”, Keith Wesley, MD ▪ Wisconsin, 2005
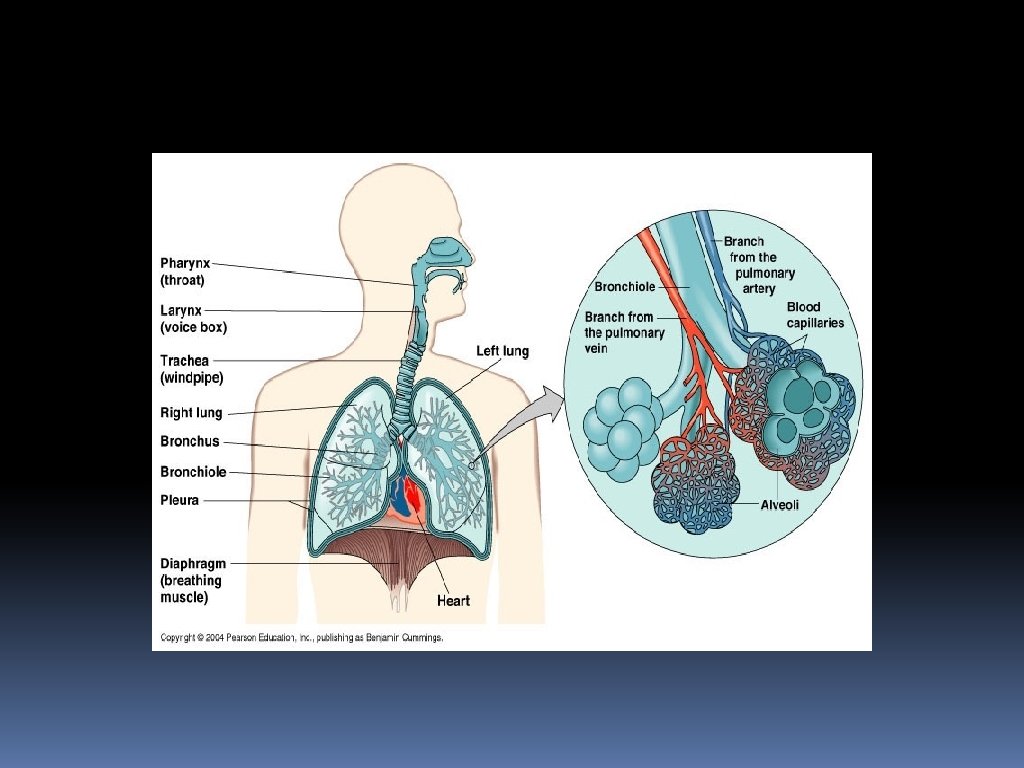
Respiratory A&P Review Upper airway structures ▪ Nasopharynx ▪ Oropharynx ▪ Tongue ▪ Epiglottis/Glottis ▪ Vocal cords Lower airway structures ▪ Trachea ▪ Carina ▪ Mainstem bronchi ▪ Secondary bronchi ▪ Bronchioles ▪ Alveoli
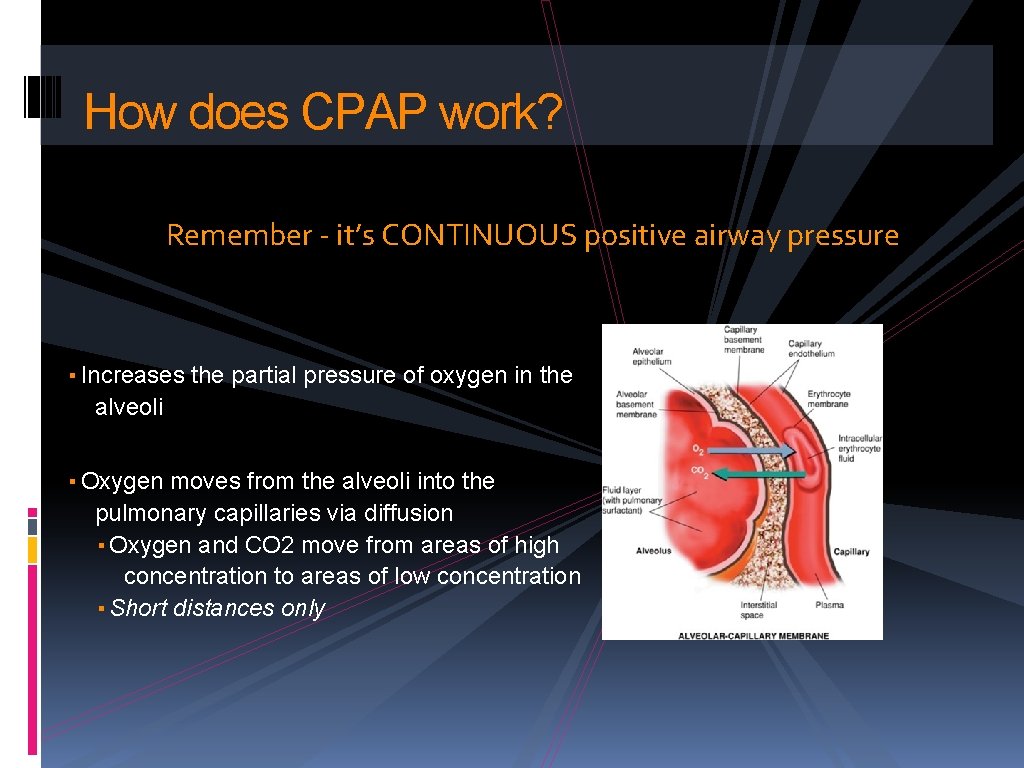
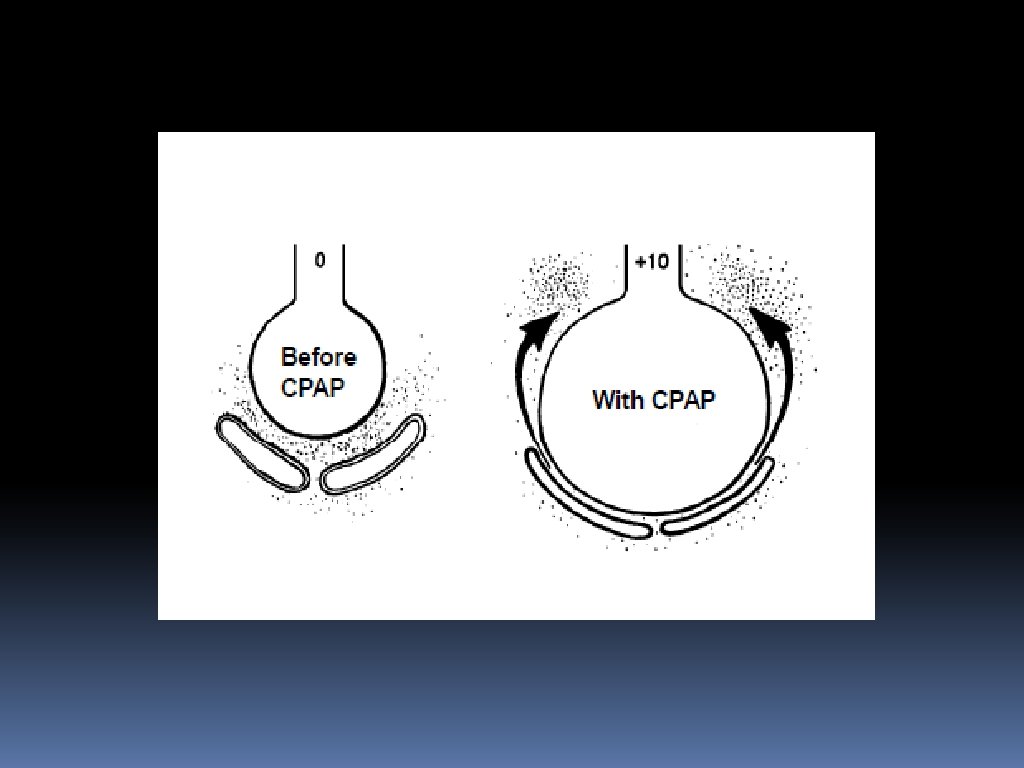
How does CPAP work? Remember - it’s CONTINUOUS positive airway pressure ▪ Increases the partial pressure of oxygen in the alveoli ▪ Oxygen moves from the alveoli into the pulmonary capillaries via diffusion ▪ Oxygen and CO 2 move from areas of high concentration to areas of low concentration ▪ Short distances only
How does CPAP work? ▪ Increases the partial pressure of oxygen in the alveoli (physics!) ▪ Reinflates collapsed airways and alveoli ▪ Pushes fluid out of the alveoli back into the vasculature ▪ Increases surface area of inflated alveoli How does it do that other stuff?
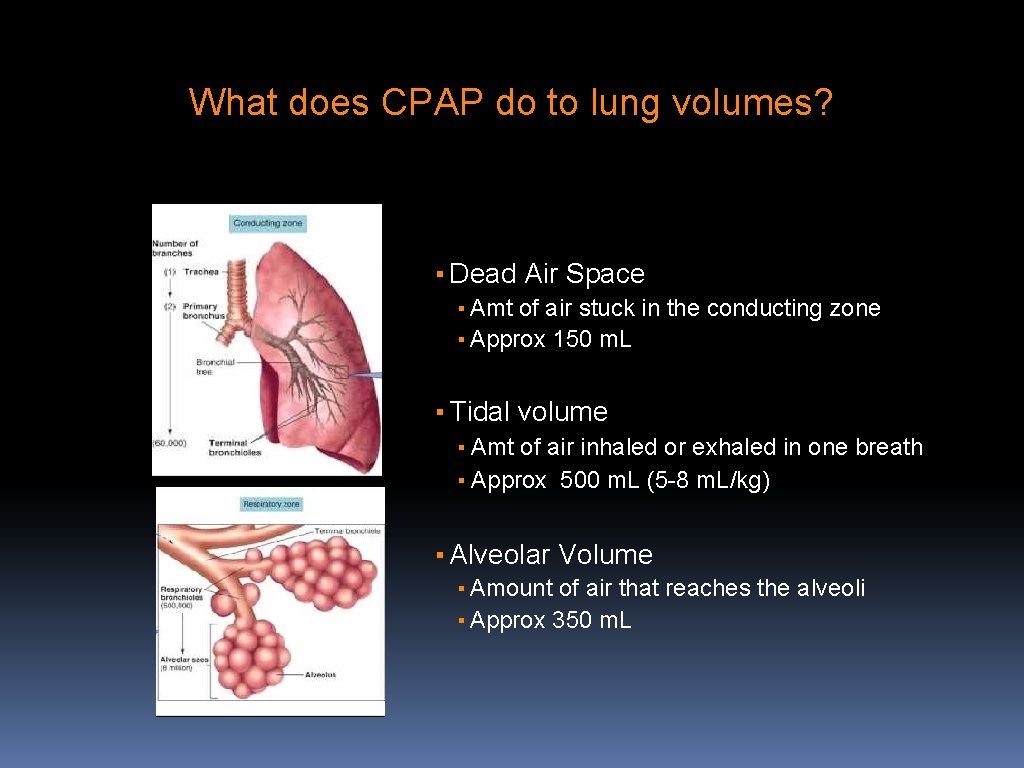
What does CPAP do to lung volumes? ▪ Dead Air Space ▪ Amt of air stuck in the conducting zone ▪ Approx 150 m. L ▪ Tidal volume ▪ Amt of air inhaled or exhaled in one breath ▪ Approx 500 m. L (5 -8 m. L/kg) ▪ Alveolar Volume ▪ Amount of air that reaches the alveoli ▪ Approx 350 m. L
Functional Residual Capacity ▪ Air left in the lungs after passive expiration ▪ Approx 2400 m. L in adult, 70 kg male ▪ CPAP increases it ▪ Physiologic reserve for gas exchange ▪ Increased FRC = Increased gas exchange
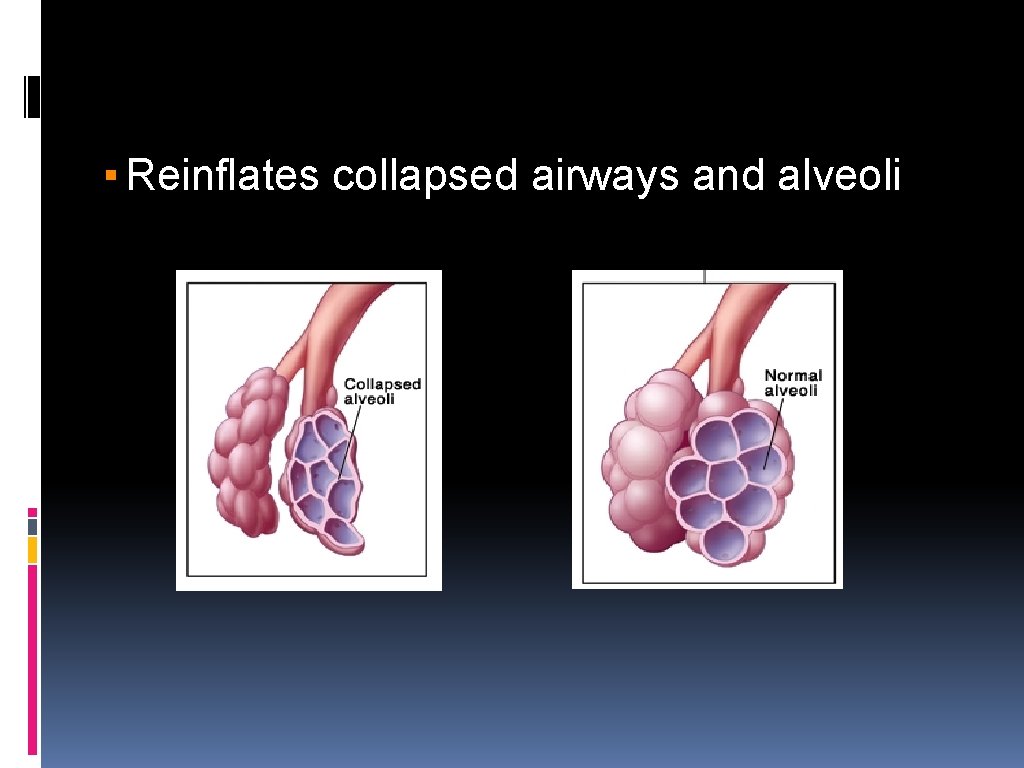
▪ Reinflates collapsed airways and alveoli
PEEP! ▪ Positive End Expiratory Pressure ▪ Pressure in the lungs/alveoli at the end of expiration ▪ Helps to keep the airways inflated ▪ Physiological PEEP = 3 -5 cm H 2 O ▪ Coughing, grunting, pursed lip breathing are all ways a patient can increase PEEP ▪ Auto-PEEP
Lung recruitment at different levels of PEEP https: //youtu. be/o. KH 7 Cts. Eg. Hw Ventilation with/without PEEP https: //youtu. be/w 9 u 6 ZI 8 HS 6 Y
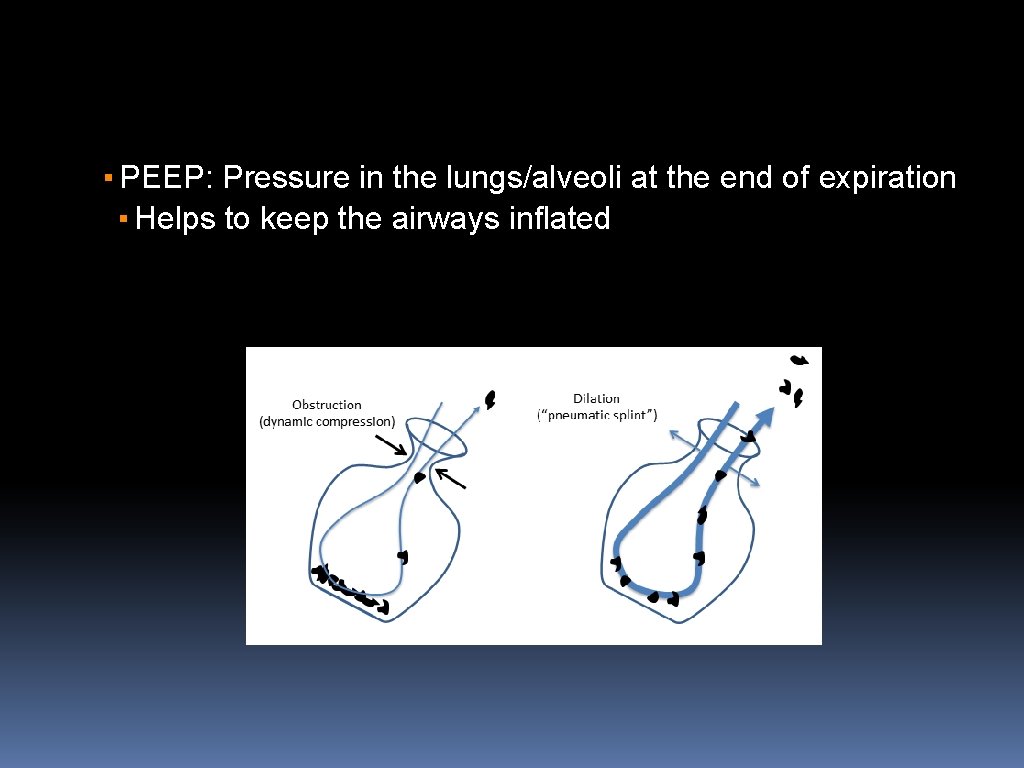
▪ PEEP: Pressure in the lungs/alveoli at the end of expiration ▪ Helps to keep the airways inflated
Can there be TOO much PEEP? ▪ At levels above 10 cm H 2 O… ▪ Intrathoracic pressure is increased ▪ Preload can be decreased, leading to decreased cardiac output ▪ Beneficial for the hypertensive CHF patient ▪ Not so much for the cardiogenic shock patient (wet lungs and low BP)
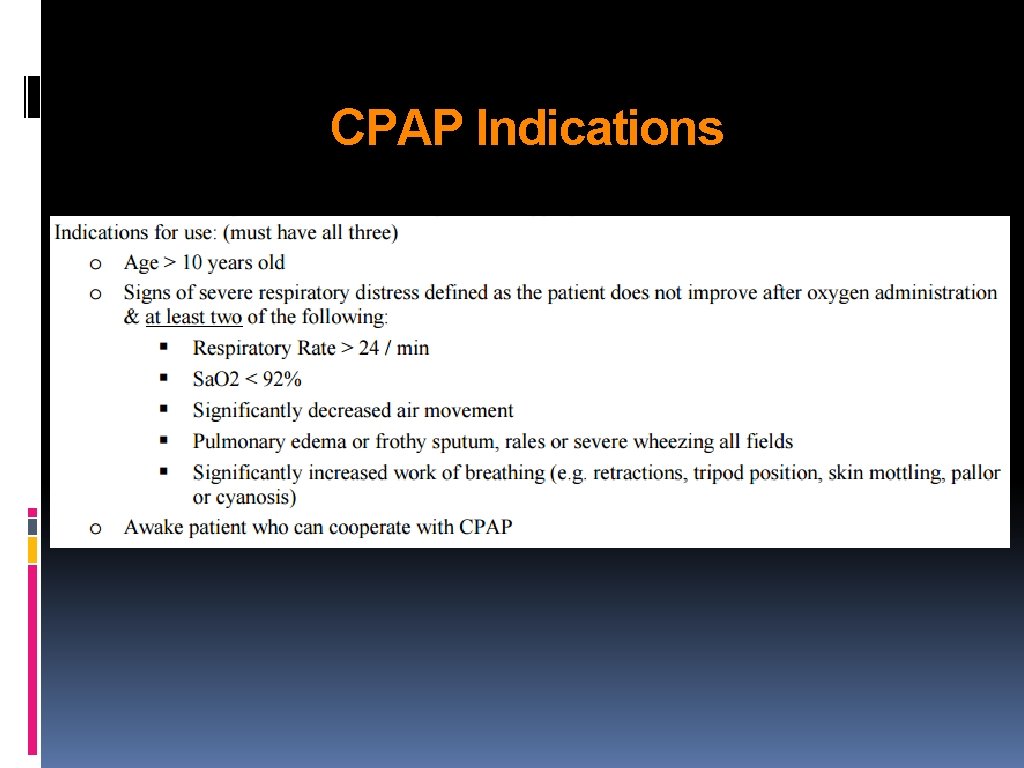
CPAP Indications
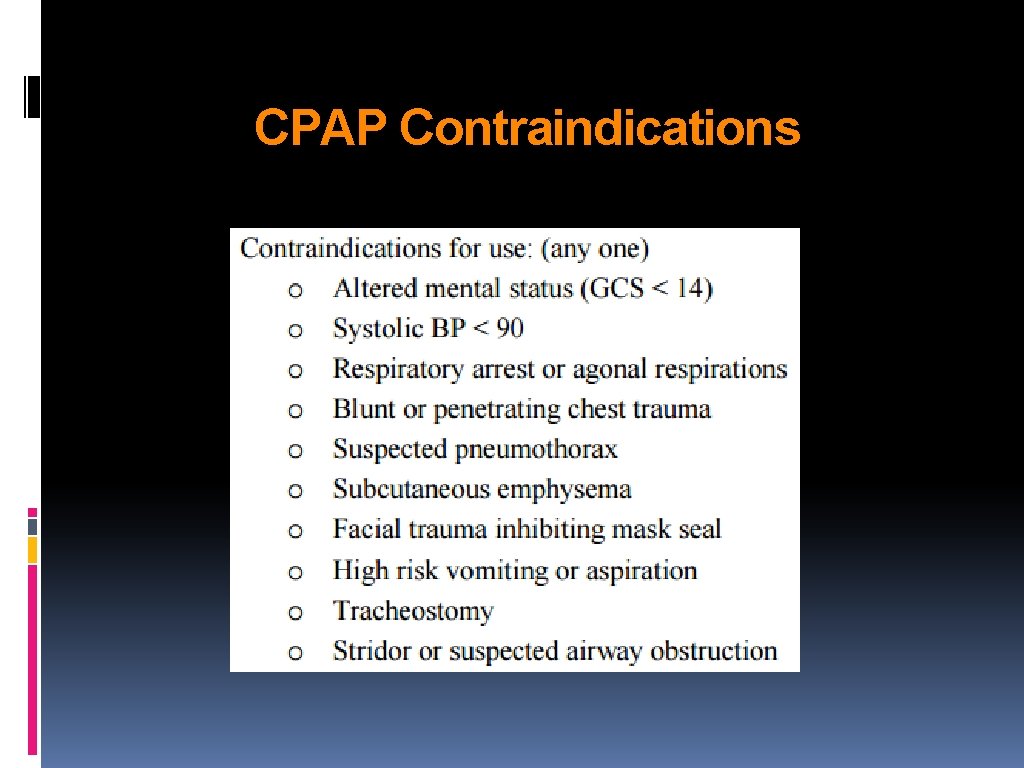
CPAP Contraindications
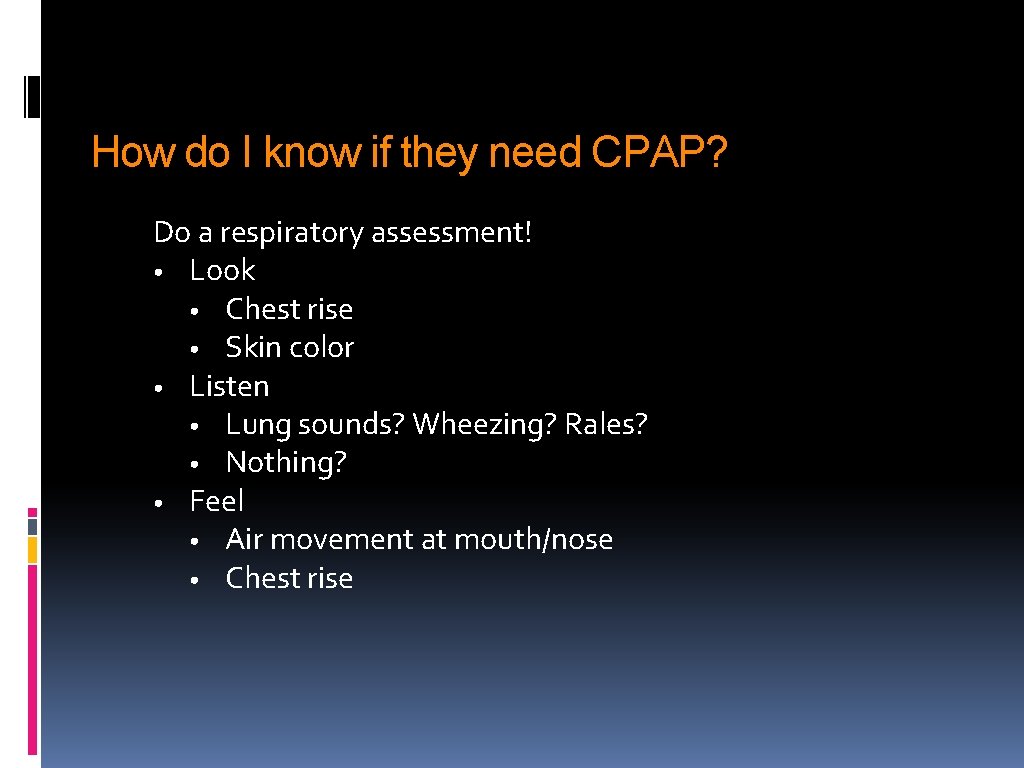
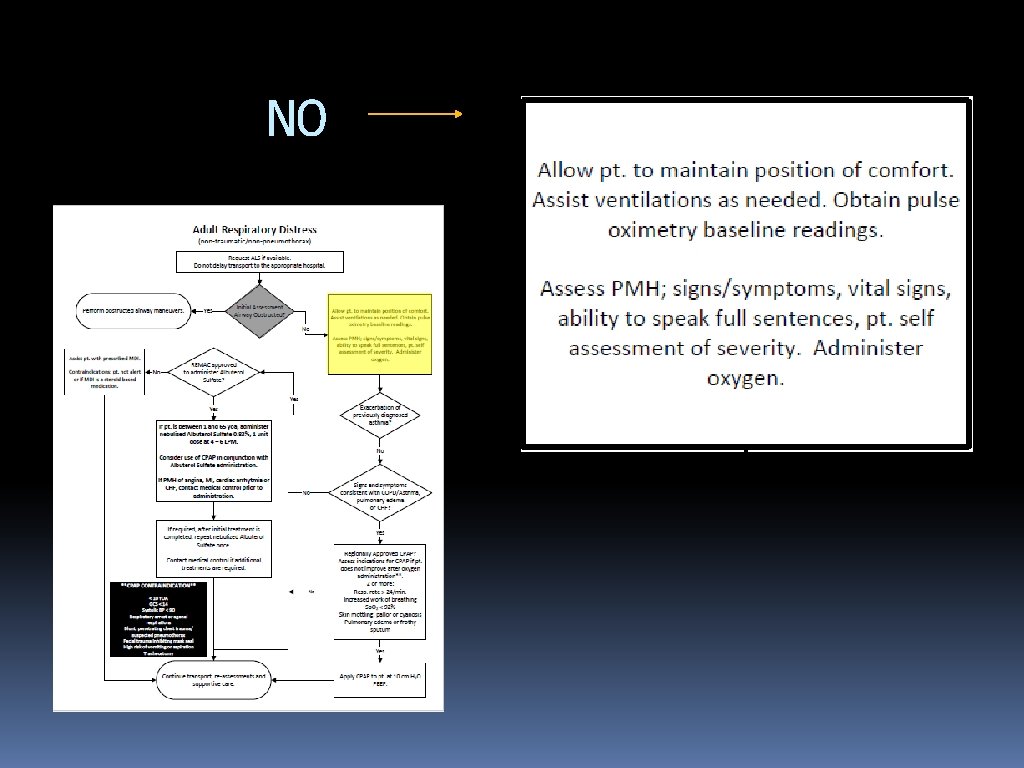
How do I know if they need CPAP? Do a respiratory assessment! • Look • Chest rise • Skin color • Listen • Lung sounds? Wheezing? Rales? • Nothing? • Feel • Air movement at mouth/nose • Chest rise
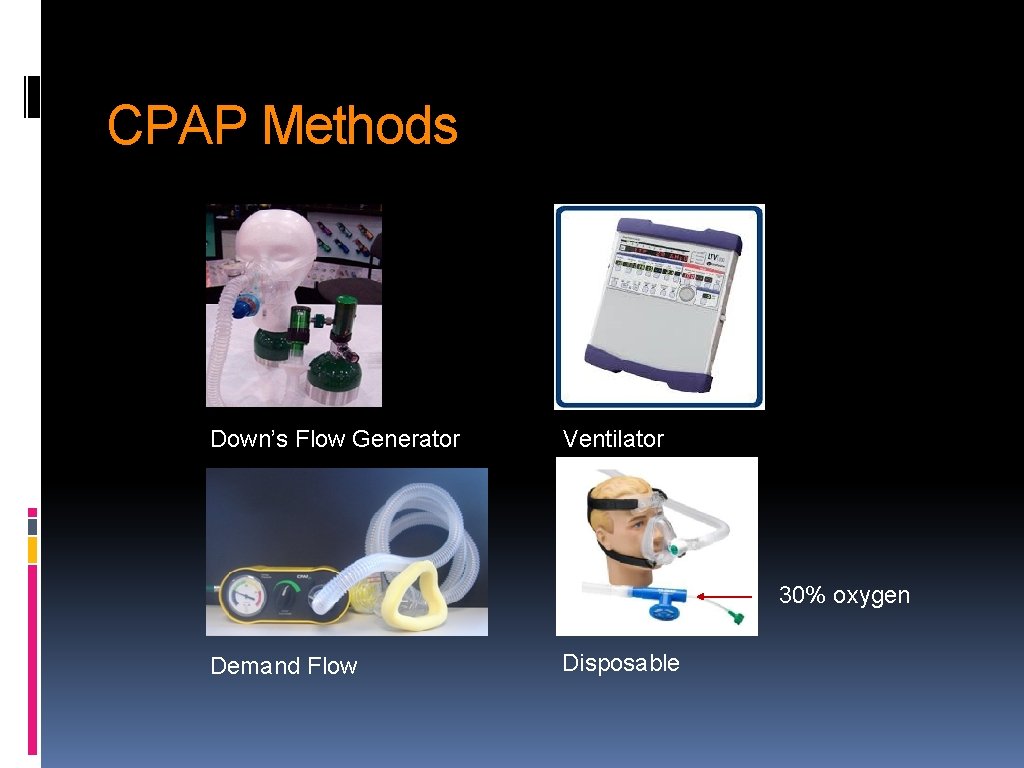
CPAP Methods Down’s Flow Generator Ventilator 30% oxygen Demand Flow Disposable
Okay, they need CPAP. Now what? • • • Prepare your equipment Tell the patient what’s happening Monitor appropriately Have the pt hold the mask themselves PEEP at 10 cm H 2 O Coach the patient Place head straps Monitor patient response/tolerance Vitals every 5 minutes Watch for leaks, gastric distention, changes in mental status or respiratory drive Continue meds (albuterol, NTG) Tell the hospital your patient is on CPAP!
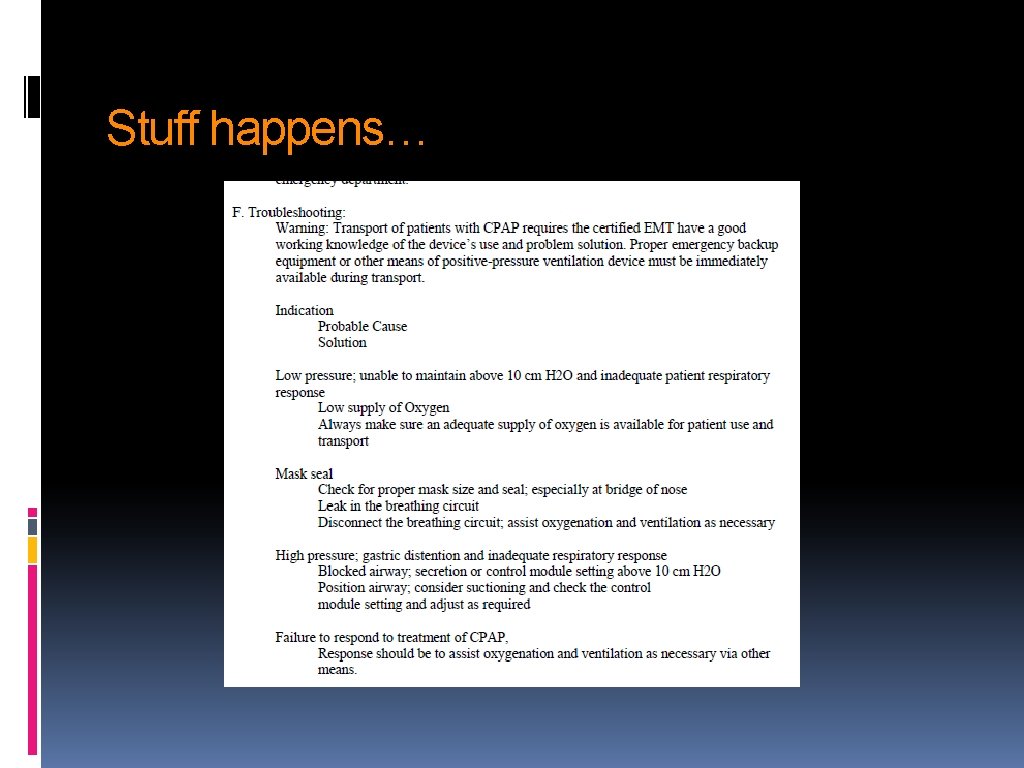
Stuff happens…
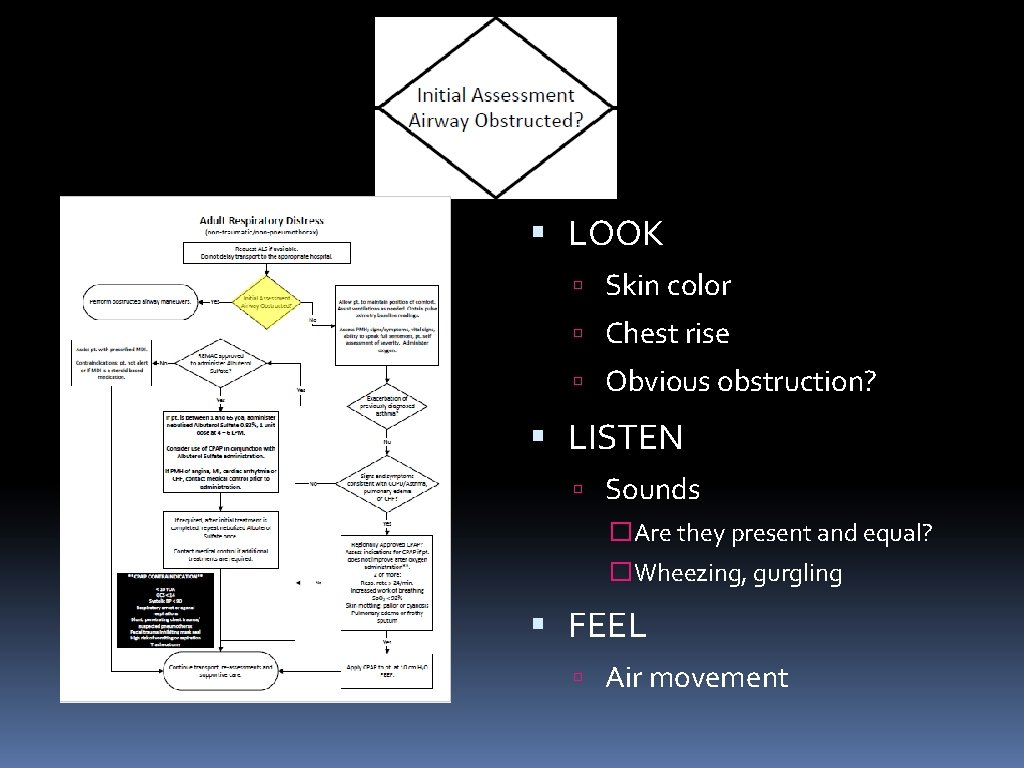
LOOK Skin color Chest rise Obvious obstruction? LISTEN Sounds �Are they present and equal? �Wheezing, gurgling FEEL Air movement
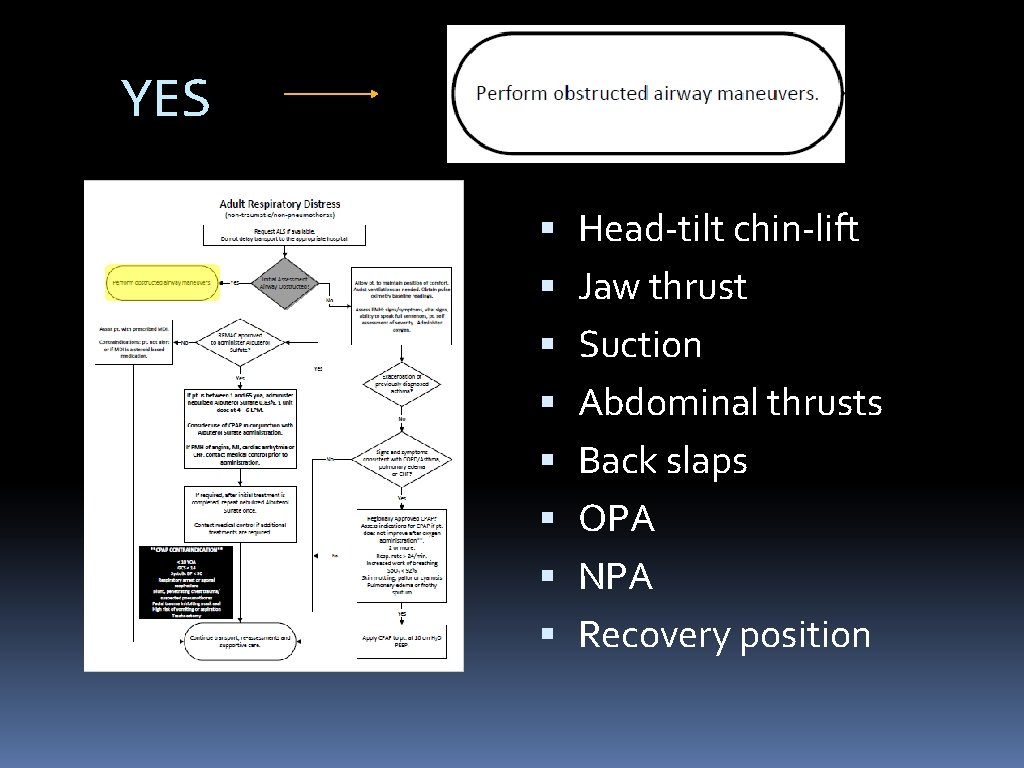
YES Head-tilt chin-lift Jaw thrust Suction Abdominal thrusts Back slaps OPA NPA Recovery position
NO
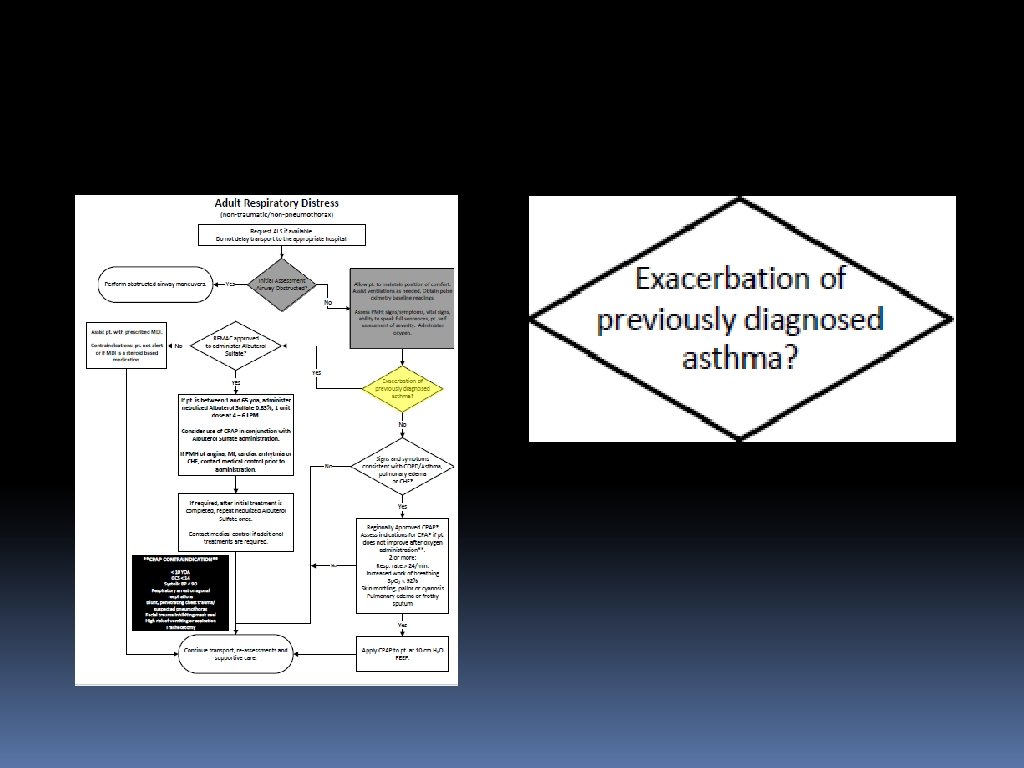
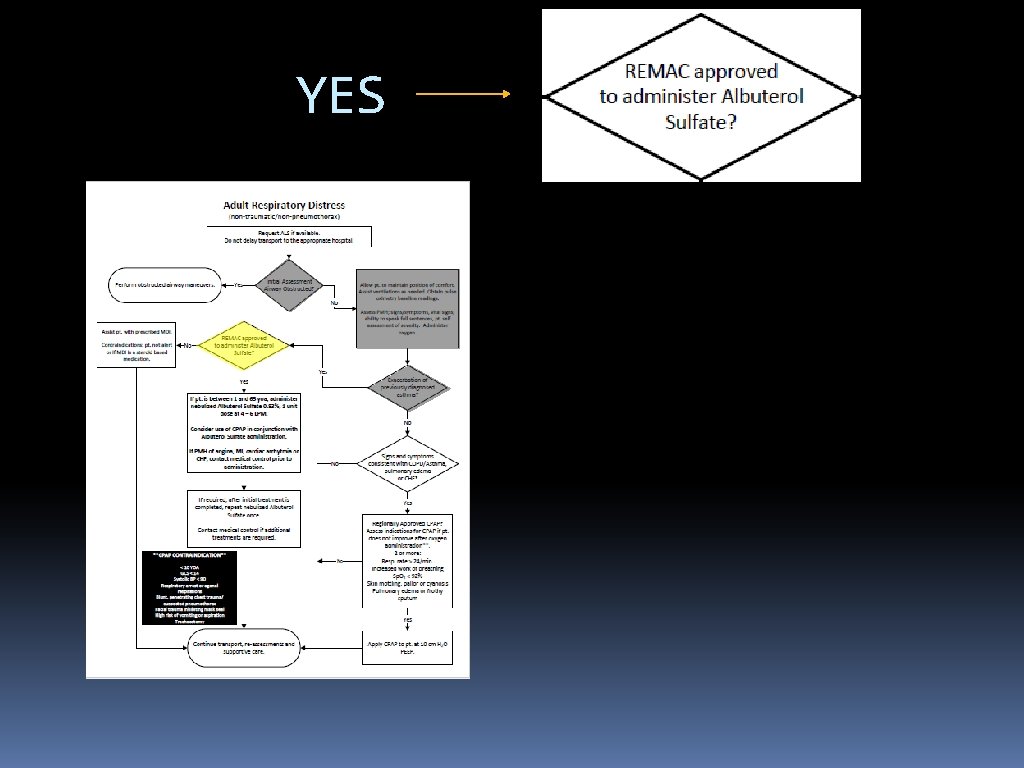
YES
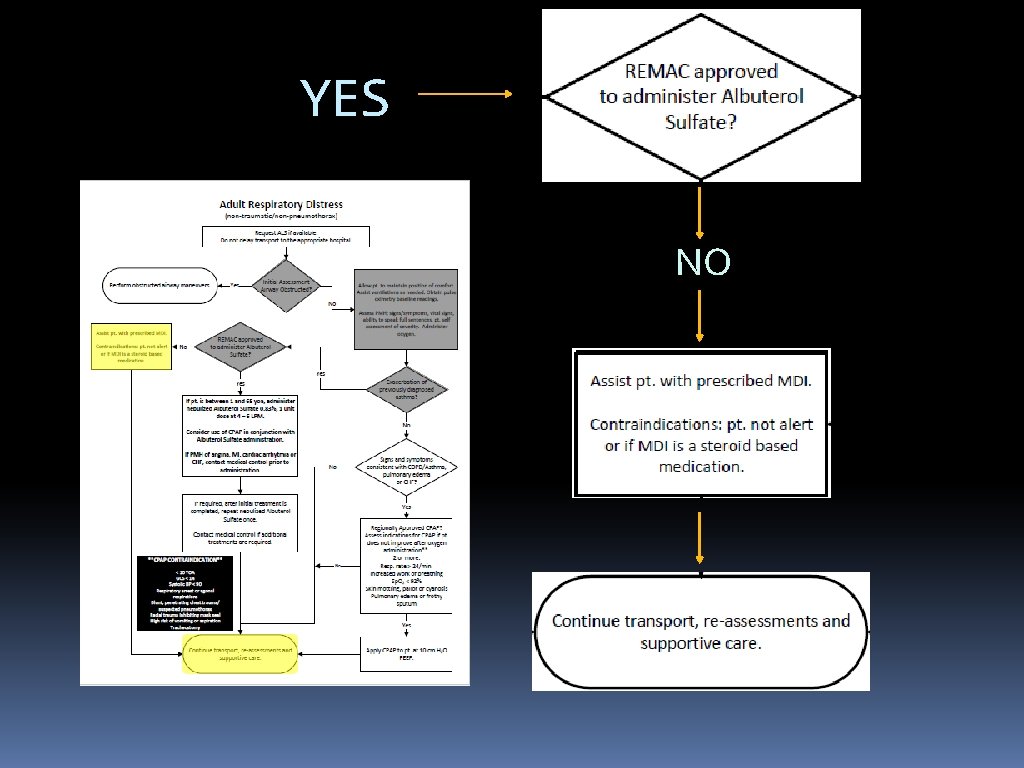
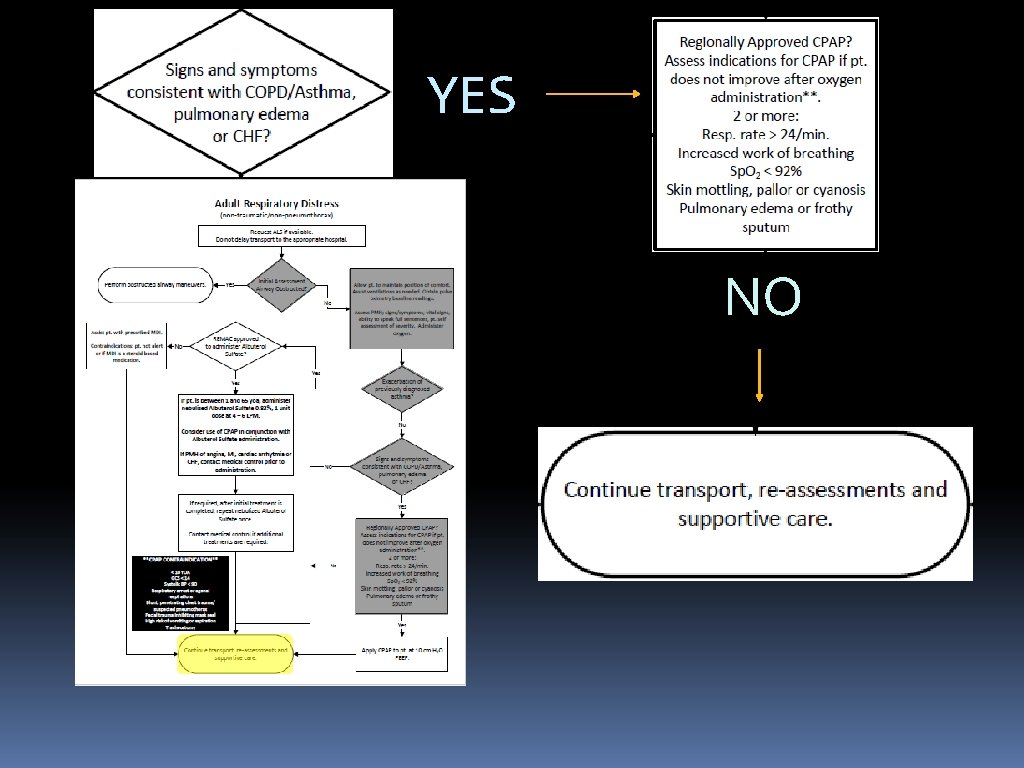
YES NO
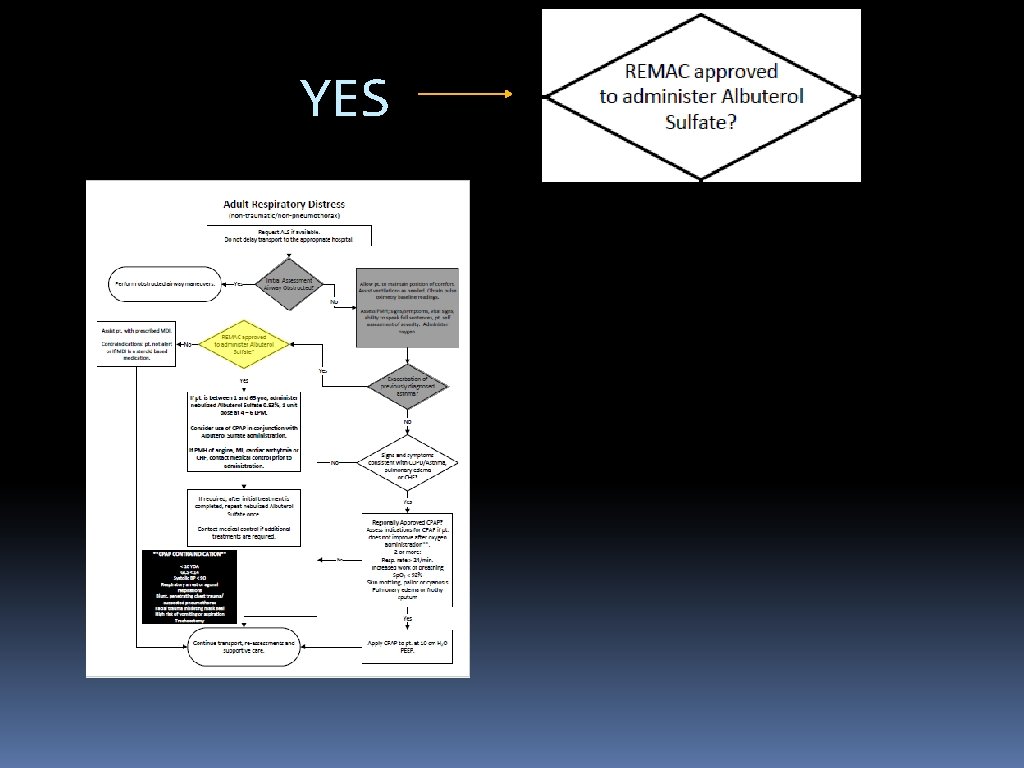
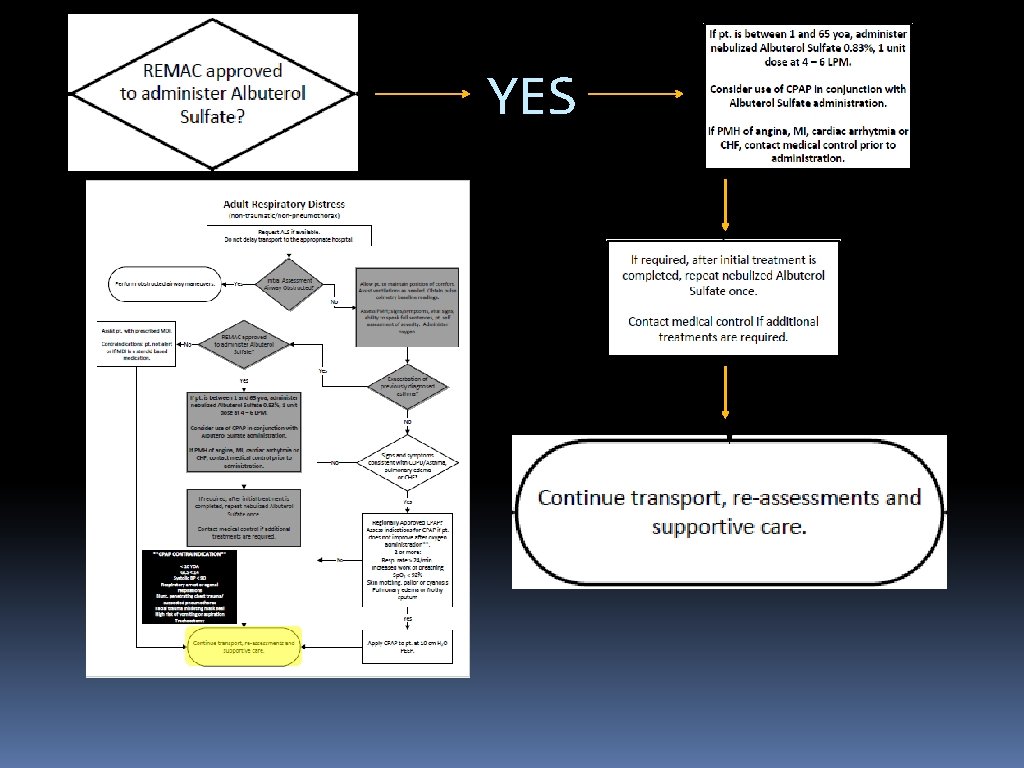
YES
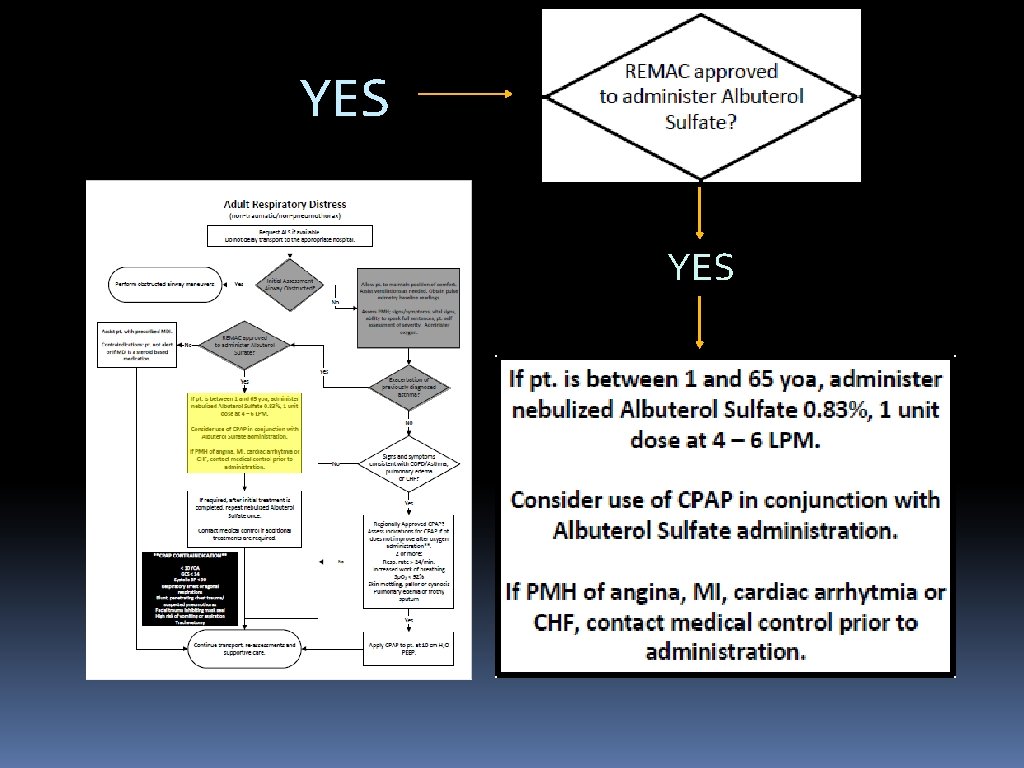
YES
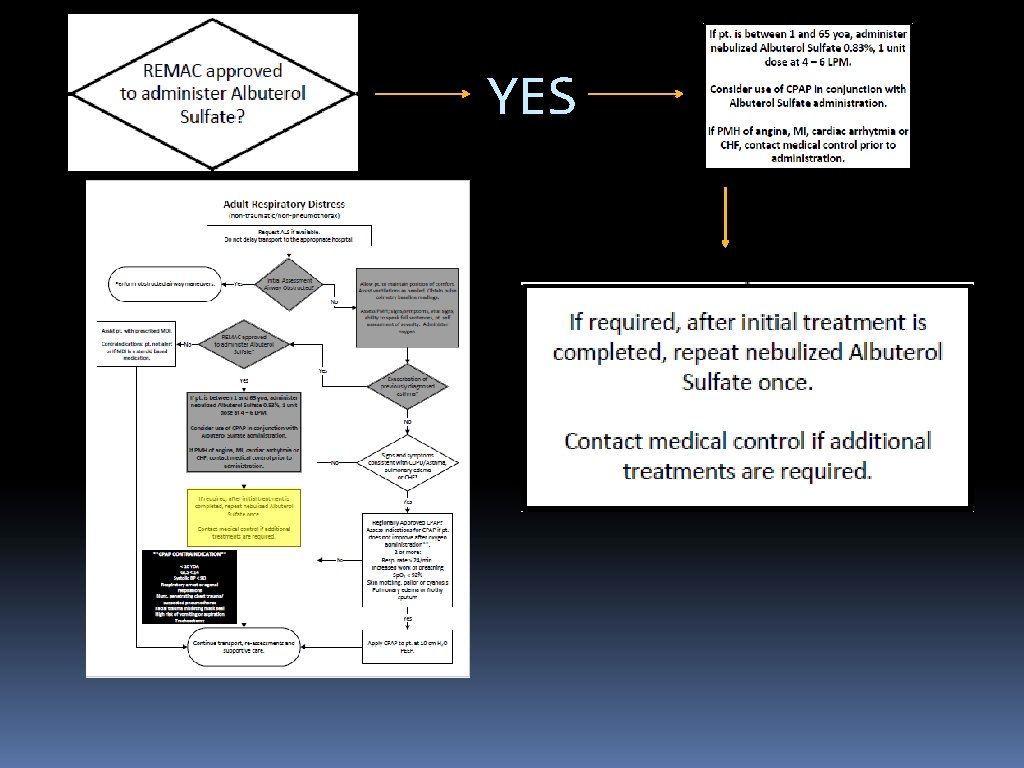
YES
YES
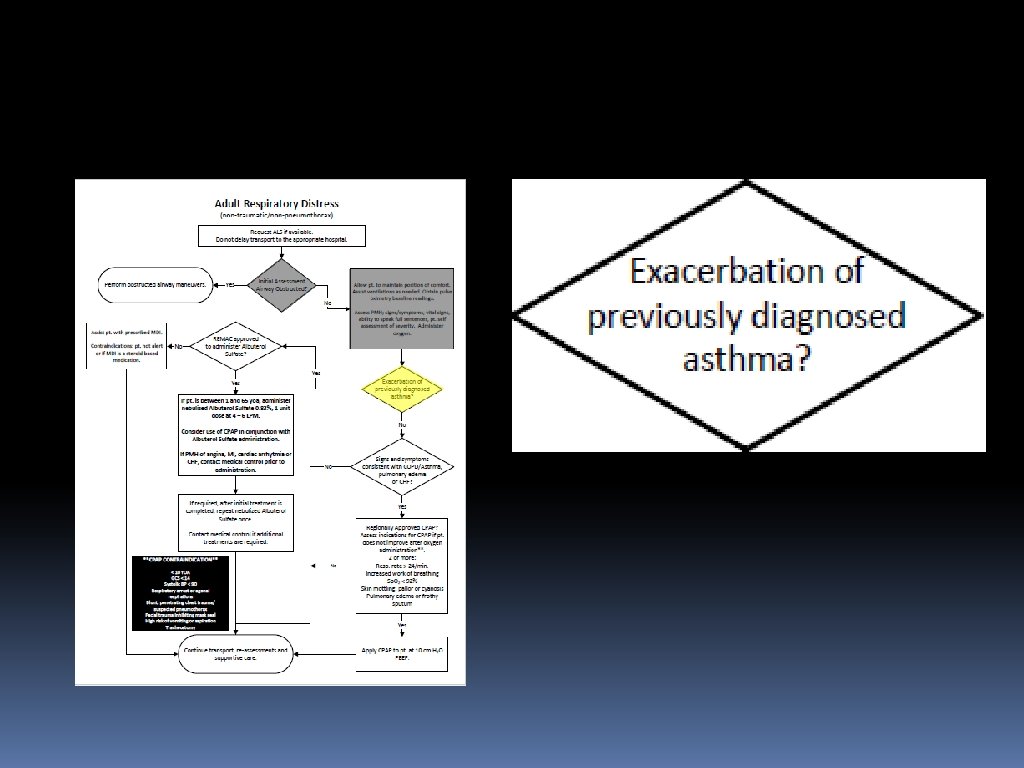
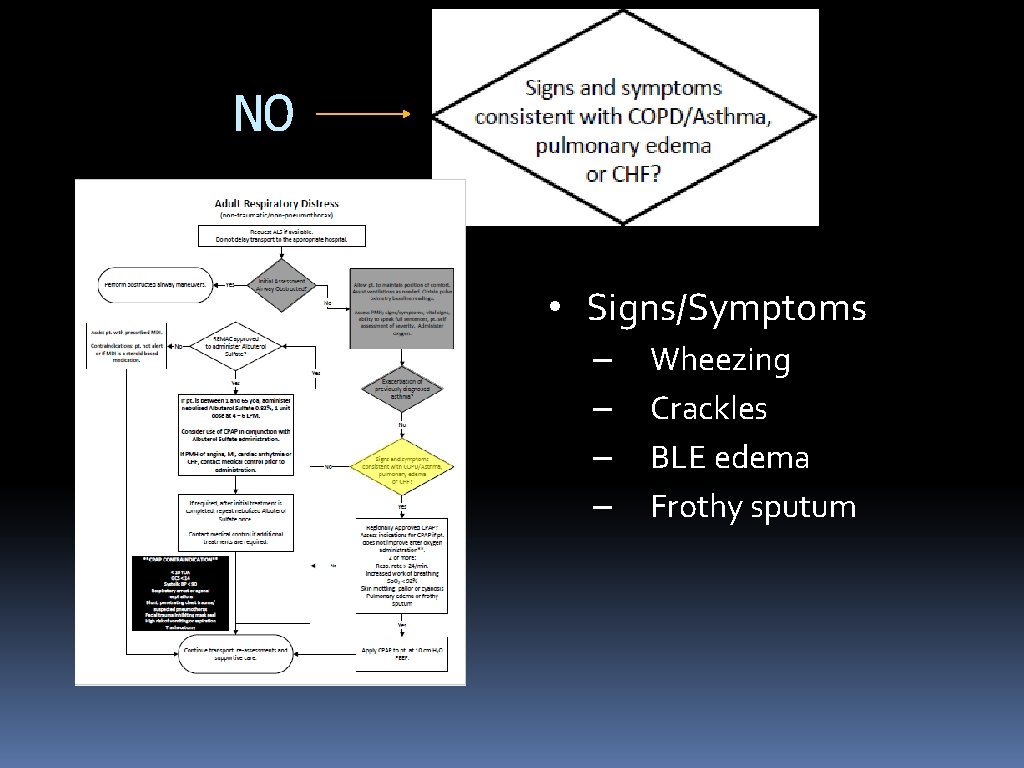
NO • Signs/Symptoms – – Wheezing Crackles BLE edema Frothy sputum
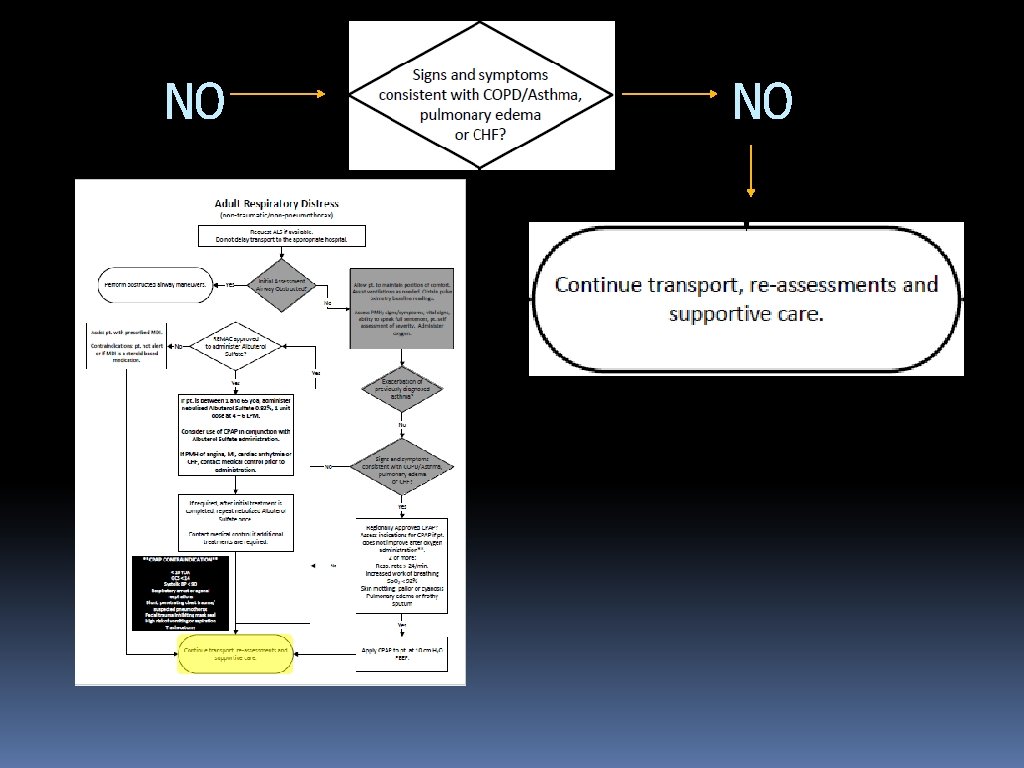
NO NO
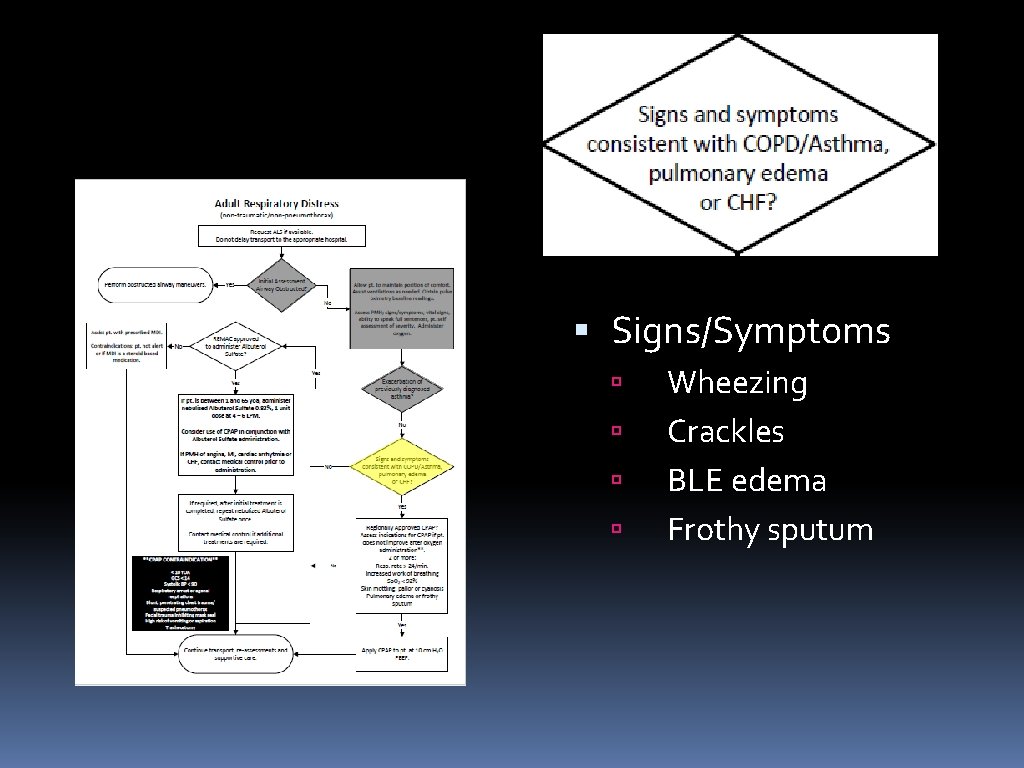
Signs/Symptoms Wheezing Crackles BLE edema Frothy sputum
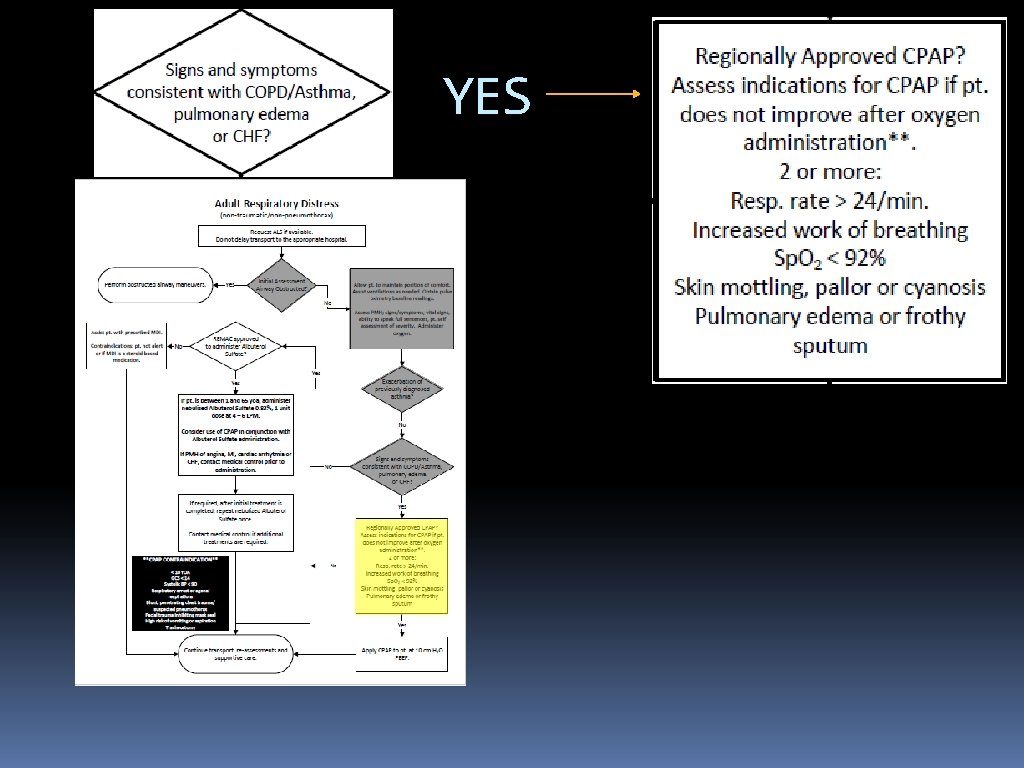
YES
YES NO
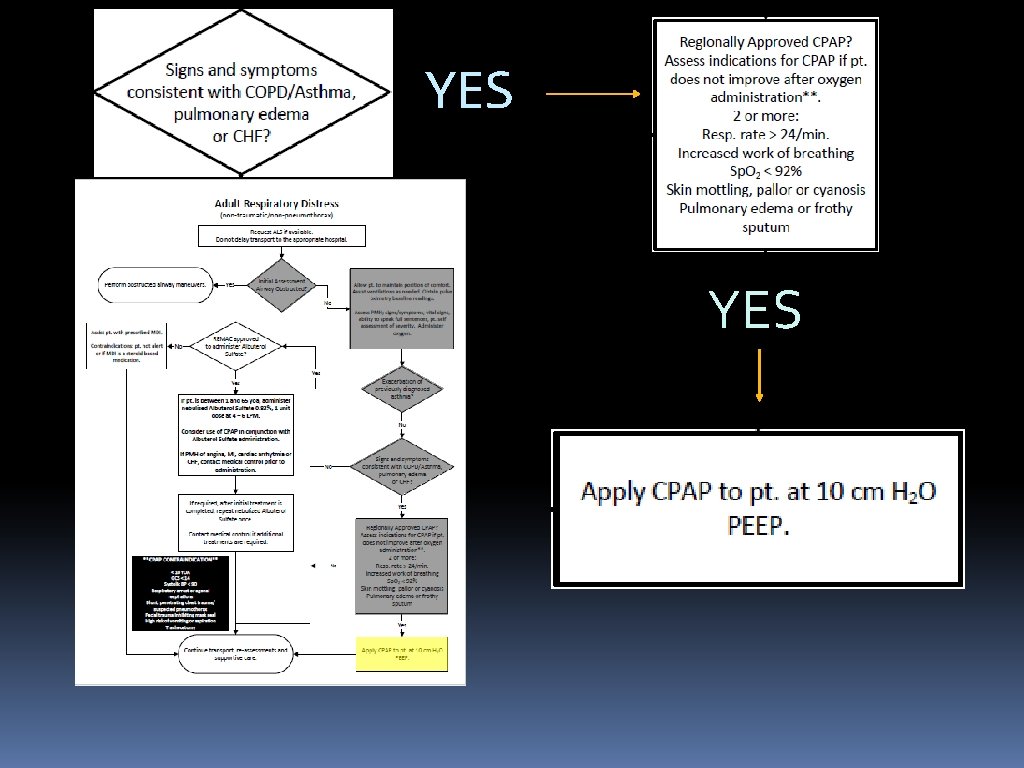
YES
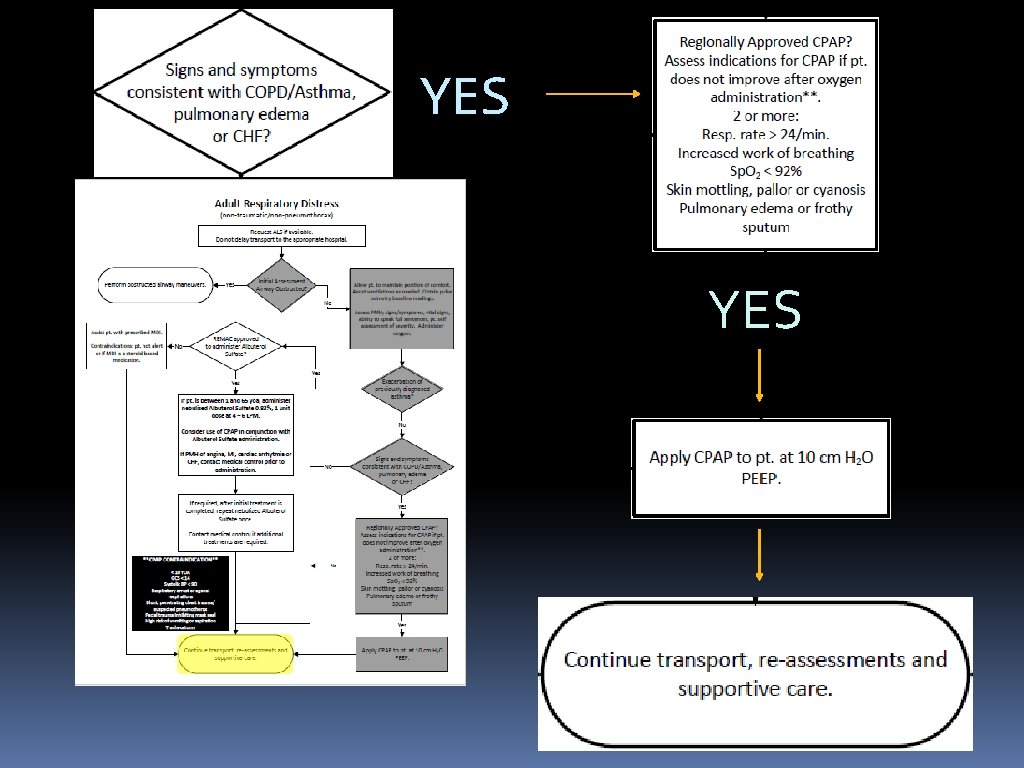
YES
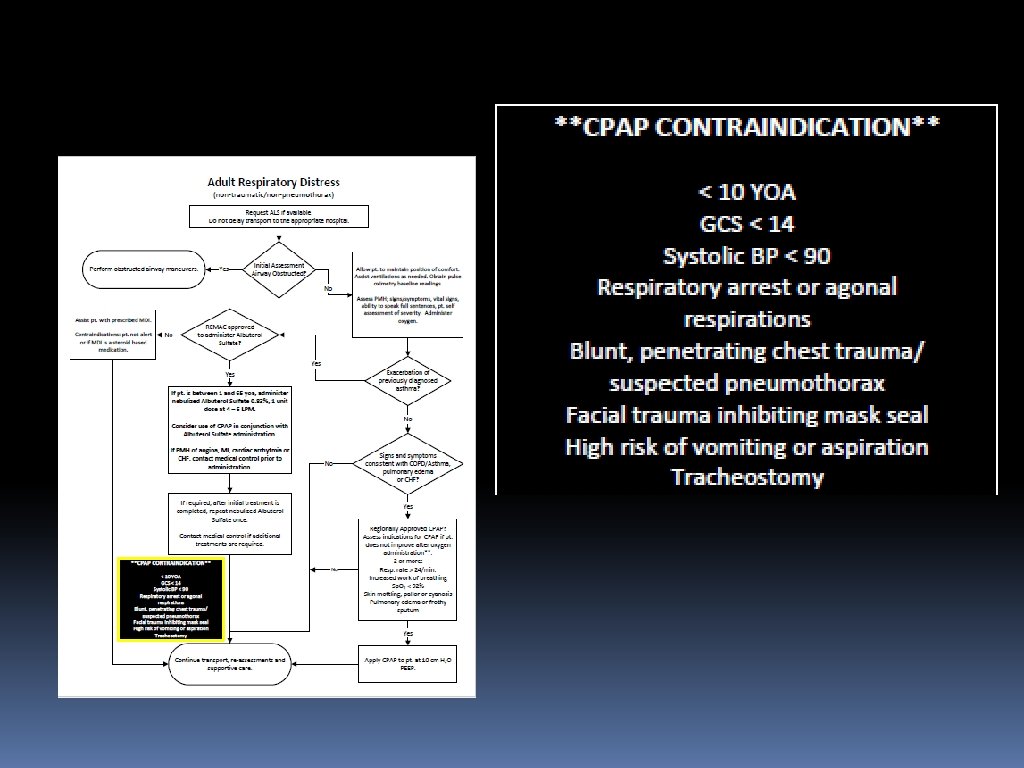
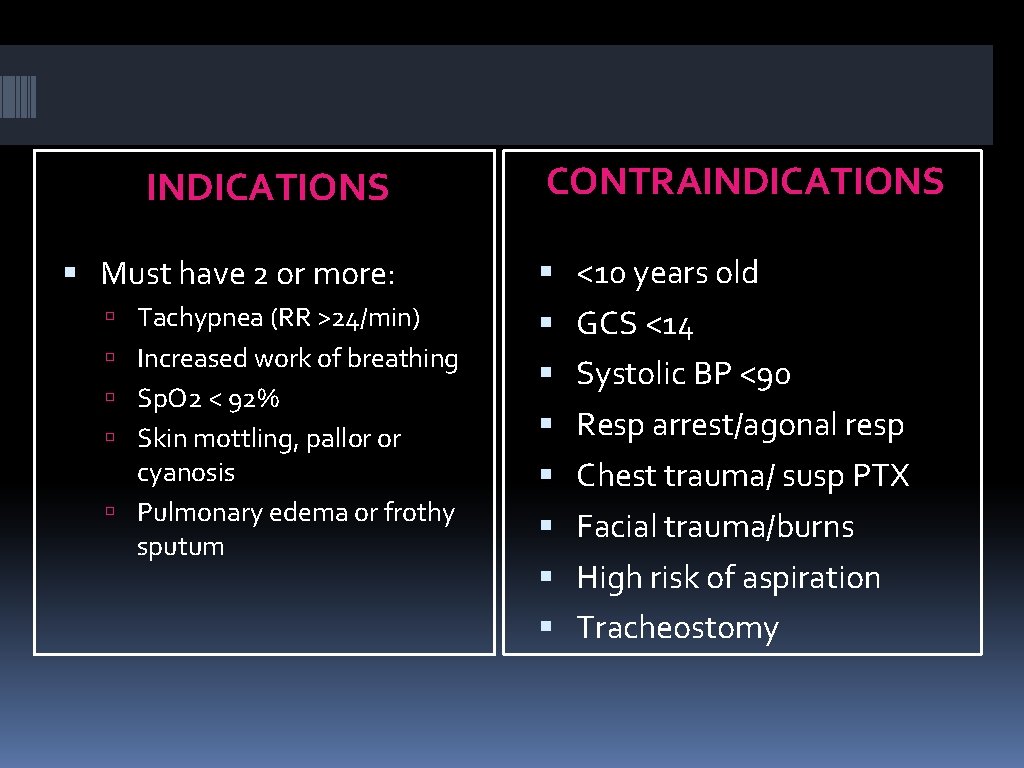
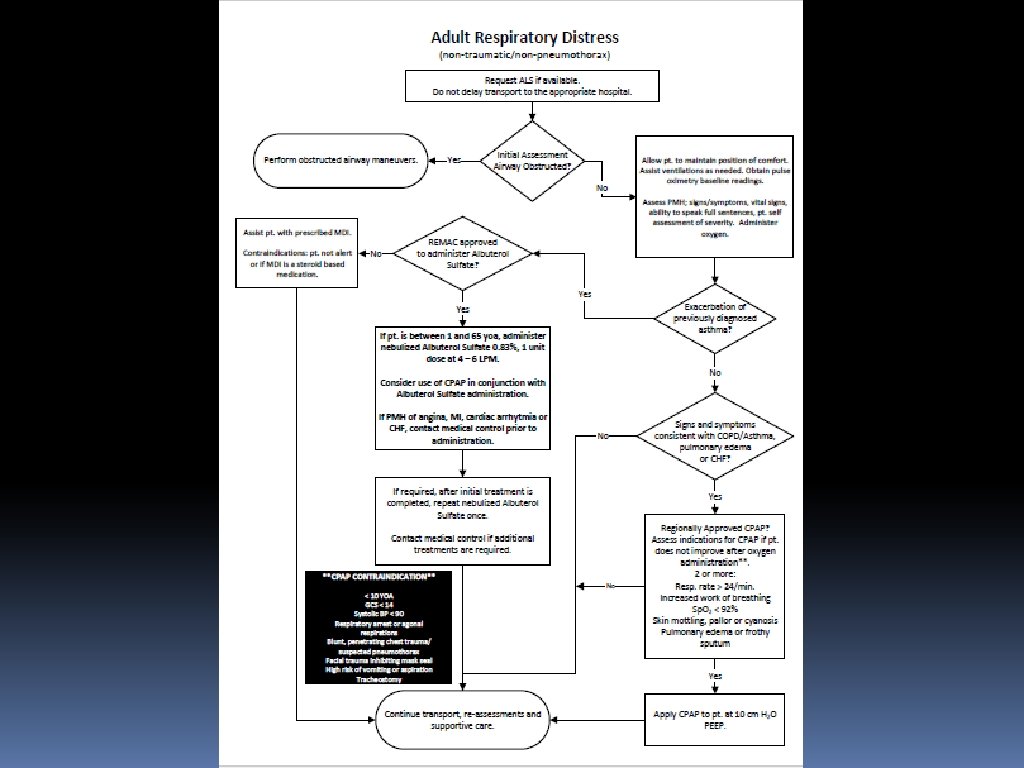
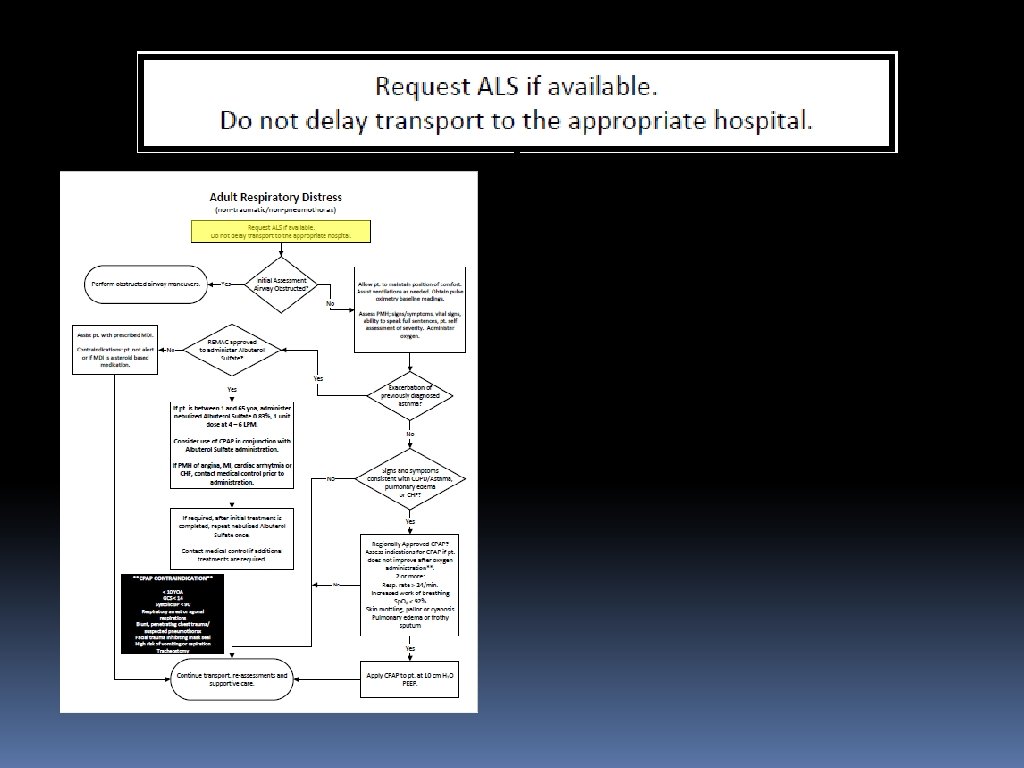
INDICATIONS Must have 2 or more: Tachypnea (RR >24/min) Increased work of breathing Sp. O 2 < 92% Skin mottling, pallor or cyanosis Pulmonary edema or frothy sputum CONTRAINDICATIONS <10 years old GCS <14 Systolic BP <90 Resp arrest/agonal resp Chest trauma/ susp PTX Facial trauma/burns High risk of aspiration Tracheostomy
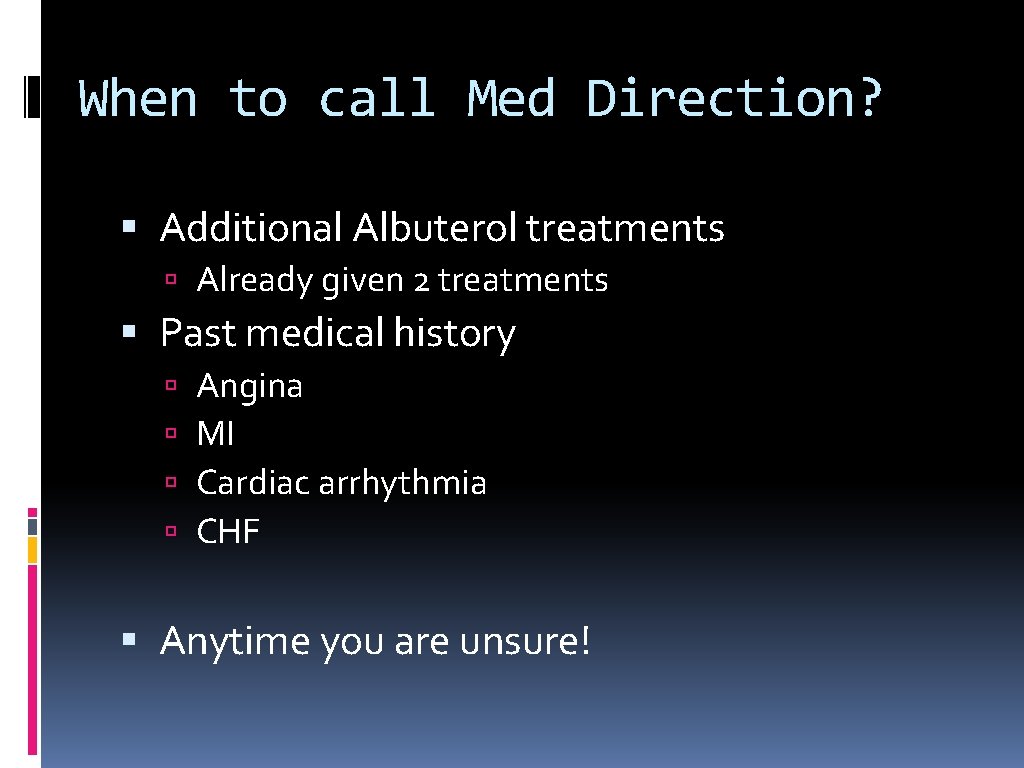
When to call Med Direction? Additional Albuterol treatments Already given 2 treatments Past medical history Angina MI Cardiac arrhythmia CHF Anytime you are unsure!
CASES! to CPAP or not to CPAP? That is the question….
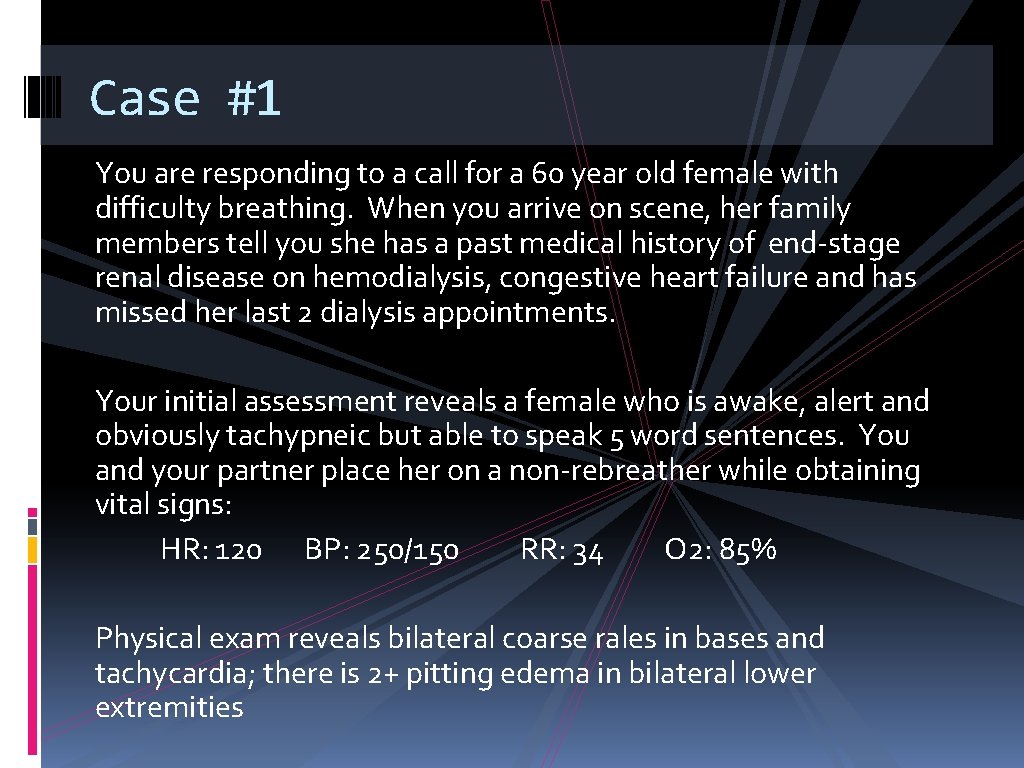
Case #1 You are responding to a call for a 60 year old female with difficulty breathing. When you arrive on scene, her family members tell you she has a past medical history of end-stage renal disease on hemodialysis, congestive heart failure and has missed her last 2 dialysis appointments. Your initial assessment reveals a female who is awake, alert and obviously tachypneic but able to speak 5 word sentences. You and your partner place her on a non-rebreather while obtaining vital signs: HR: 120 BP: 250/150 RR: 34 O 2: 85% Physical exam reveals bilateral coarse rales in bases and tachycardia; there is 2+ pitting edema in bilateral lower extremities
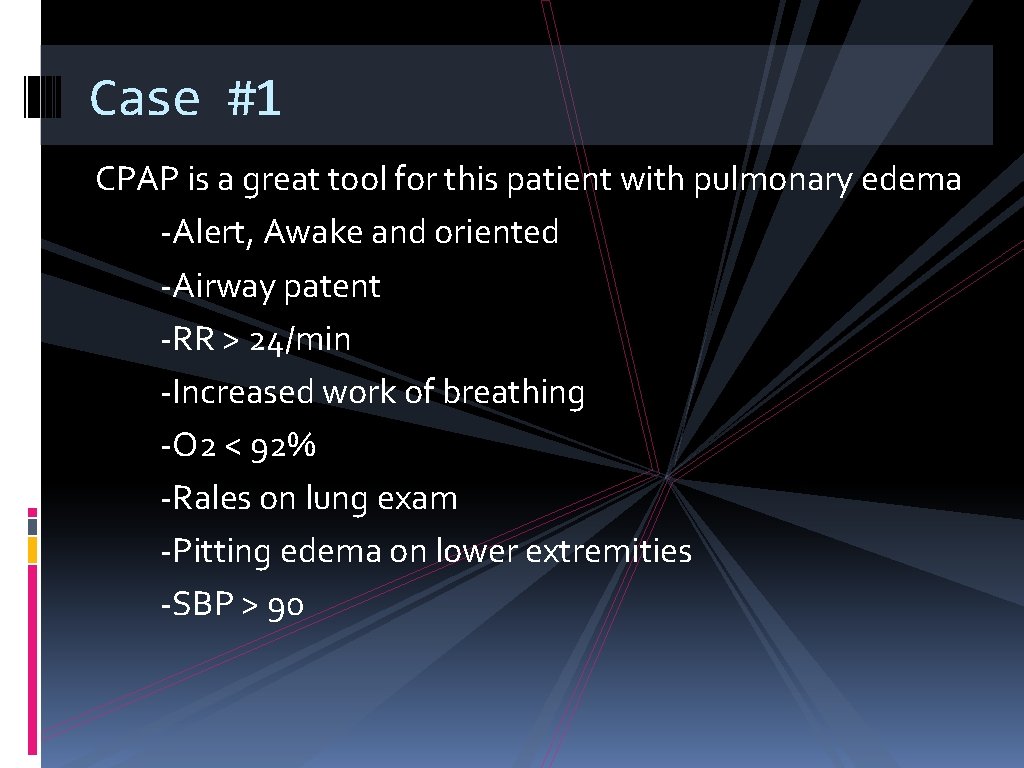
Case #1 CPAP is a great tool for this patient with pulmonary edema -Alert, Awake and oriented -Airway patent -RR > 24/min -Increased work of breathing -O 2 < 92% -Rales on lung exam -Pitting edema on lower extremities -SBP > 90
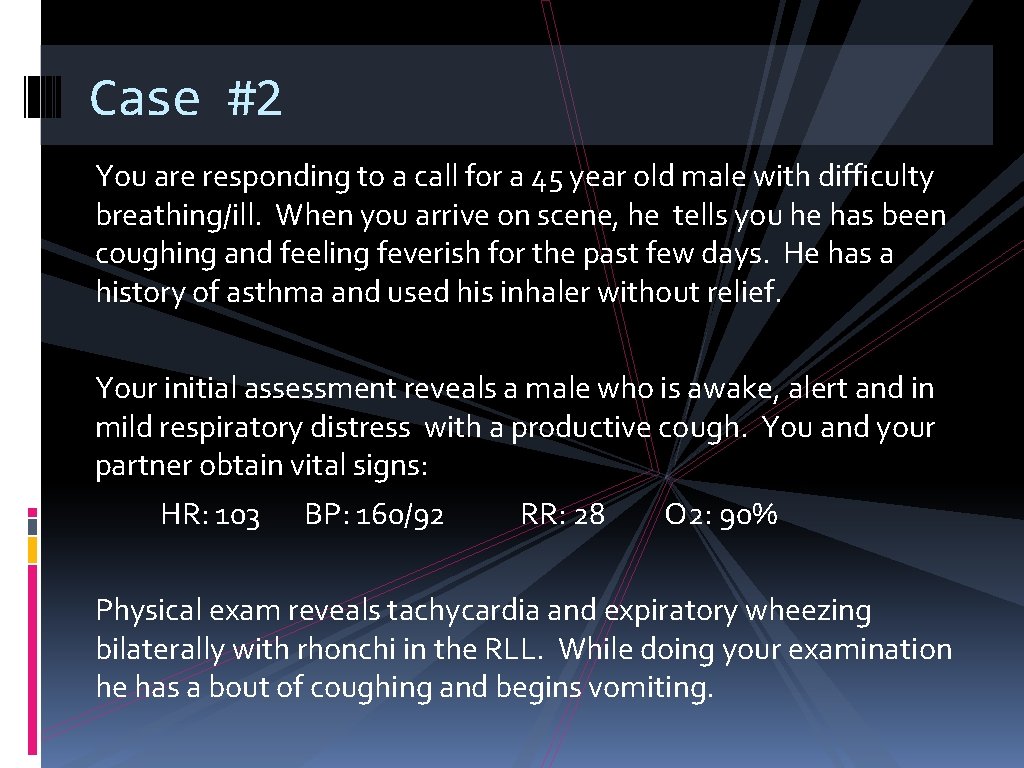
Case #2 You are responding to a call for a 45 year old male with difficulty breathing/ill. When you arrive on scene, he tells you he has been coughing and feeling feverish for the past few days. He has a history of asthma and used his inhaler without relief. Your initial assessment reveals a male who is awake, alert and in mild respiratory distress with a productive cough. You and your partner obtain vital signs: HR: 103 BP: 160/92 RR: 28 O 2: 90% Physical exam reveals tachycardia and expiratory wheezing bilaterally with rhonchi in the RLL. While doing your examination he has a bout of coughing and begins vomiting.
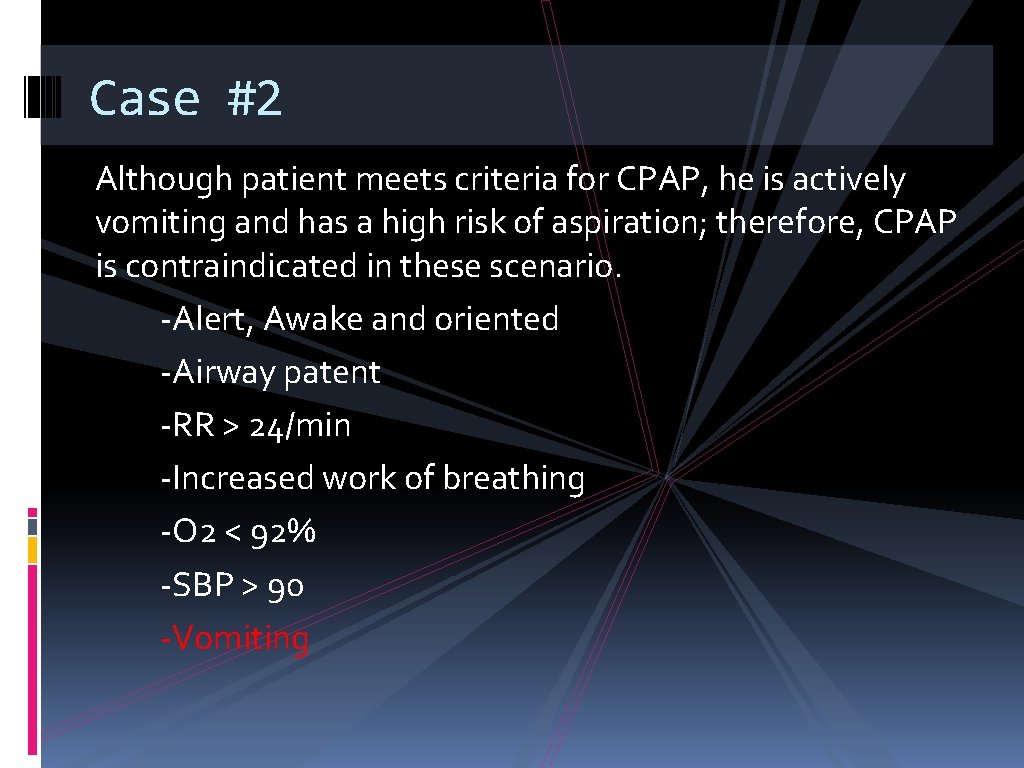
Case #2 Although patient meets criteria for CPAP, he is actively vomiting and has a high risk of aspiration; therefore, CPAP is contraindicated in these scenario. -Alert, Awake and oriented -Airway patent -RR > 24/min -Increased work of breathing -O 2 < 92% -SBP > 90 -Vomiting
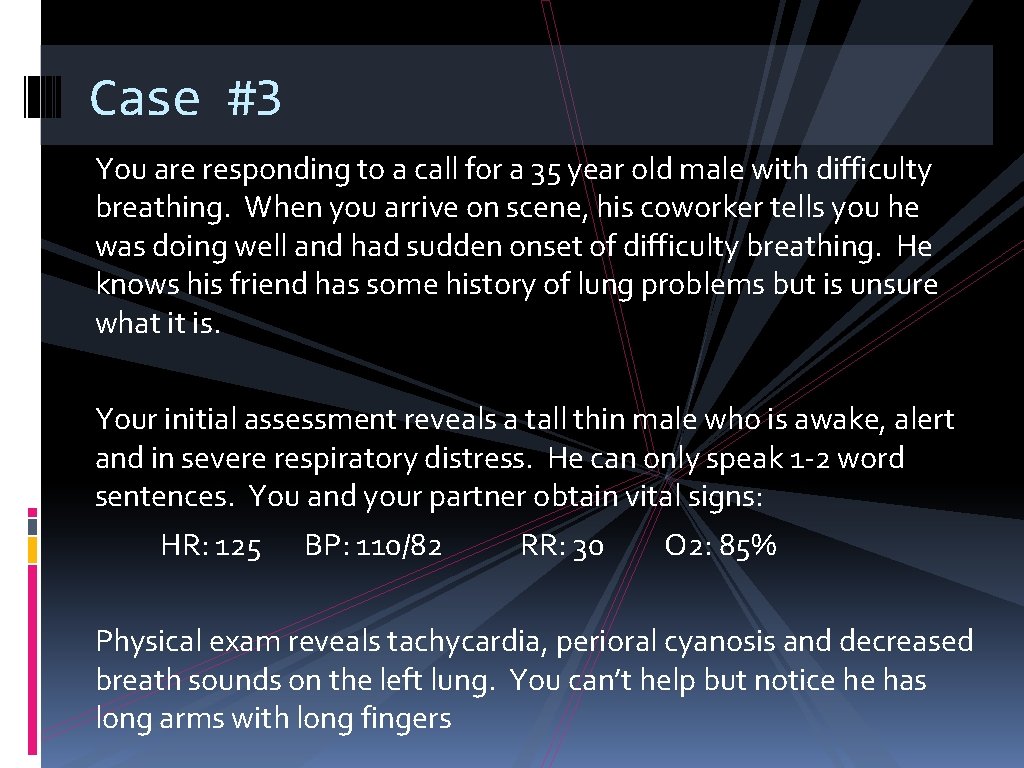
Case #3 You are responding to a call for a 35 year old male with difficulty breathing. When you arrive on scene, his coworker tells you he was doing well and had sudden onset of difficulty breathing. He knows his friend has some history of lung problems but is unsure what it is. Your initial assessment reveals a tall thin male who is awake, alert and in severe respiratory distress. He can only speak 1 -2 word sentences. You and your partner obtain vital signs: HR: 125 BP: 110/82 RR: 30 O 2: 85% Physical exam reveals tachycardia, perioral cyanosis and decreased breath sounds on the left lung. You can’t help but notice he has long arms with long fingers
Case #3 Although patient meets criteria for CPAP, this scenario is concerning for a suspected pneumothorax (Marfan syndrome) which is a contraindication to CPAP. -Alert, Awake and oriented -Airway patent -RR > 24/min -Increased work of breathing -Cyanosis -O 2 < 92% -SBP > 90 -Decreased breath sounds on left
Case #4 You are responding to a call for a 75 year old male with difficulty breathing. When you arrive to the nursing home, the staff tells you he has CHF, ischemic cardiomyopathy, CRF, HTN, s/p MI x 2, COPD, and dementia. During shift change the new nurse noticed he wasn’t acting like himself and looked like he was having difficulty breathing. Your initial assessment reveals an elderly male who is awake, alert to self only and in respiratory distress. He can speak 5 word sentences but has moments where he is not lucid and will not follow basic commands. You and your partner obtain vital signs: HR: 120 BP: 88/50 RR: 35 O 2: 85% Physical exam reveals tachycardia, perioral cyanosis, and bibasilar crackles in his lungs with faint expiratory wheezing.
Case #4 Although patient meets criteria for CPAP, this scenario is concerning for cardiogenic shock and a patient who is unable to follow commands, both of which are contraindications to CPAP. -Airway patent -RR > 24/min -Increased work of breathing -O 2 < 92% -Cyanosis -Unable to follow commands -SBP < 90 -Decreased mental status
Case #5 You are responding to a call for a 25 year old female with difficulty breathing. When you arrive on scene, she tells you she has a PMH of asthma and ran out of her inhalers 2 weeks ago. She was running to catch the bus when she developed difficulty breathing. Your initial assessment reveals a young female who is awake, alert and oriented and in severe respiratory distress. She can speak 2 -3 word sentences and has audible wheezing. You and your partner obtain vital signs: HR: 115 BP: 130/82 RR: 44 O 2: 84% Physical exam reveals tachycardia and diffuse inspiratory and expiratory wheezing bilaterally with decreased aeration throughout all lung fields.
Case #5 Although patient meets criteria for CPAP based on vital signs, she is awake and able to maintain her work of breathing -Airway patent -RR > 24/min -Increased work of breathing -O 2 < 92% Place on O 2, administer albuterol nebs
Case #5 continued You are en route to the hospital. She has received 2 albuterol nebulizers and although she says she feels slightly improved she is also stating she is getting tired and wants to take a nap. You repeat vital signs HR: 125 BP: 140/90 RR: 18 O 2: 89% Physical exam reveals expiratory wheezing bilaterally with improvement in aeration throughout all lung fields. She has intercostal and abdominal retractions and is tripoding.
Case #5 continued Your patient is decompensating and is tiring out. CPAP is useful to help with the work of breathing and as a temporizing measure prior to arriving to the hospital. -Airway patent -RR > 24/min -Increased work of breathing -O 2 < 92% You place her on CPAP at 10 cm H 20 and call ahead to the ED where you are given an order to administer a 3 rd neb with the CPAP. By the time you arrive to the ED, the patient is more awake, is no longer retracting and states she feels significantly improved. She is asking for something to eat.
Case #6 You are responding to a call for a 16 year old male with difficulty breathing. When you arrive on scene, his girlfriend says they were getting high and he overdosed on 4 bags of heroin. She administered the take home Narcan kit which she received 2 days ago from ECMC (when she overdosed). She says he was doing fine for 2 hours and suddenly developed difficulty breathing. He is otherwise healthy. Your initial assessment reveals a young male who is awake, alert and oriented and in respiratory distress. You and your partner obtain vital signs: HR: 120 BP: 125/86 RR: 35 O 2: 84% Physical exam reveals perioral cyanosis with pink frothy sputum at his mouth. He has bibasilar crackles and you notice track marks in bilateral upper extremities.
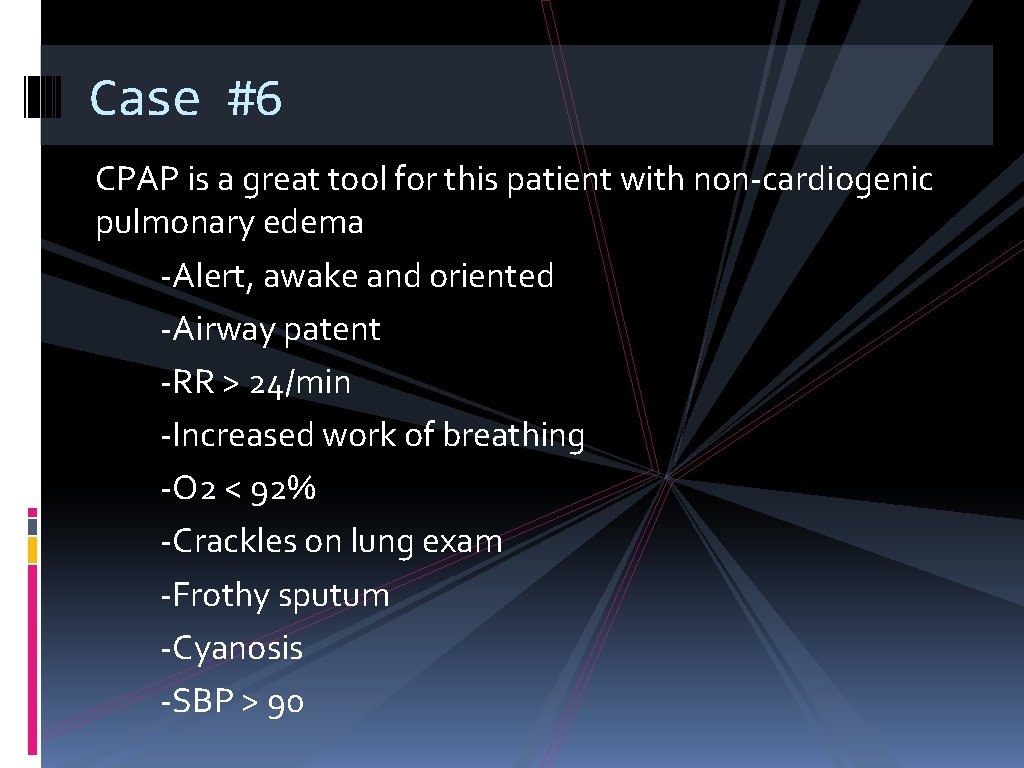
Case #6 CPAP is a great tool for this patient with non-cardiogenic pulmonary edema -Alert, awake and oriented -Airway patent -RR > 24/min -Increased work of breathing -O 2 < 92% -Crackles on lung exam -Frothy sputum -Cyanosis -SBP > 90
Hands-on!
- Slides: 63