Bloody Easy Blood Administration Module 3 Transfusion Reactions
Bloody Easy Blood Administration Module 3 – Transfusion Reactions Content derived from Bloody Easy Blood Administration Handbook Version 2, 2015 Prepared by Ana Lima, RN
Learning Objectives • Identify the signs and symptoms of an acute transfusion reaction • List the different types of acute transfusion reactions • Describe the clinical management, reaction investigation and reporting required when a reaction occurs • Utilize the Ontario TTISS* transfusion reaction chart NOTE: Always consult your hospital policy for information specific to your facility as practice may vary *TTISS - Transfusion Transmitted Injuries Surveillance System
Recognizing Reactions Acute reactions usually occur during or up to 6 hours following the end of a transfusion and may present with: • • • Fever Shaking chills or rigors with or without fever Hives or rash, itchiness, swelling Dyspnea, shortness of breath, or wheezing Hypotension or hypertension Red urine, diffuse bleeding or oozing Lumbar pain, anxiety, pain at the IV site Nausea and vomiting Headache Irritability (pediatric patients)
Recognizing Reactions • Initially it can be challenging to distinguish a minor reaction from a serious reaction based solely on the presenting signs and symptoms. • Any unexpected or suspicious symptom should be reported to the TML* for investigation of a possible transfusion reaction. • Delayed transfusion reactions do not present with symptoms until days or weeks following a transfusion and are not covered in this module. *TML- Transfusion Medicine Laboratory
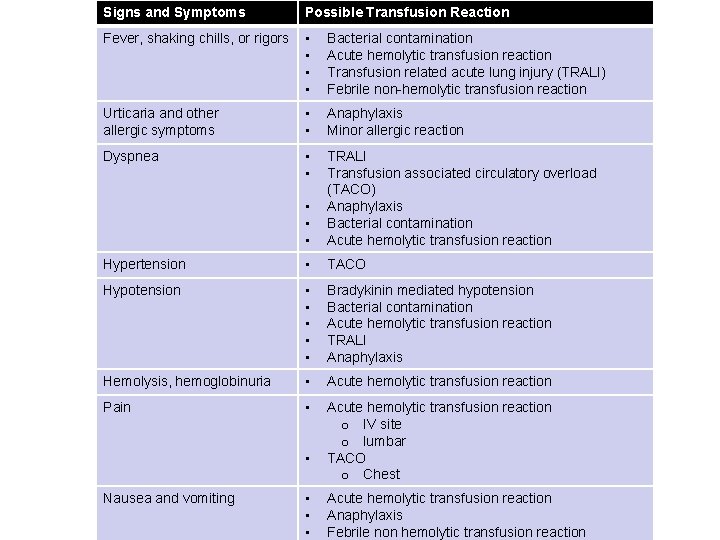
Signs and Symptoms Possible Transfusion Reaction Fever, shaking chills, or rigors • • Bacterial contamination Acute hemolytic transfusion reaction Transfusion related acute lung injury (TRALI) Febrile non-hemolytic transfusion reaction Urticaria and other allergic symptoms • • Anaphylaxis Minor allergic reaction Dyspnea • • • TRALI Transfusion associated circulatory overload (TACO) Anaphylaxis Bacterial contamination Acute hemolytic transfusion reaction Hypertension • TACO Hypotension • • • Bradykinin mediated hypotension Bacterial contamination Acute hemolytic transfusion reaction TRALI Anaphylaxis Hemolysis, hemoglobinuria • Acute hemolytic transfusion reaction Pain • Acute hemolytic transfusion reaction o IV site o lumbar TACO o Chest • Nausea and vomiting • • • Acute hemolytic transfusion reaction Anaphylaxis Febrile non hemolytic transfusion reaction
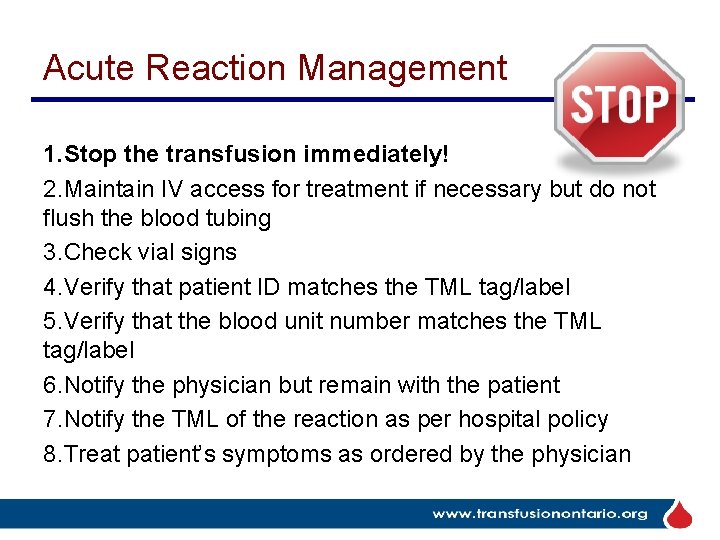
Acute Reaction Management 1. Stop the transfusion immediately! 2. Maintain IV access for treatment if necessary but do not flush the blood tubing 3. Check vial signs 4. Verify that patient ID matches the TML tag/label 5. Verify that the blood unit number matches the TML tag/label 6. Notify the physician but remain with the patient 7. Notify the TML of the reaction as per hospital policy 8. Treat patient’s symptoms as ordered by the physician
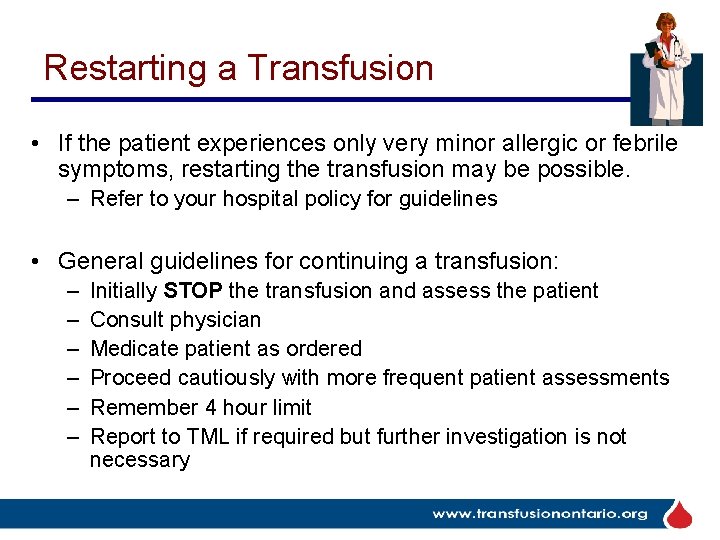
Restarting a Transfusion • If the patient experiences only very minor allergic or febrile symptoms, restarting the transfusion may be possible. – Refer to your hospital policy for guidelines • General guidelines for continuing a transfusion: – – – Initially STOP the transfusion and assess the patient Consult physician Medicate patient as ordered Proceed cautiously with more frequent patient assessments Remember 4 hour limit Report to TML if required but further investigation is not necessary
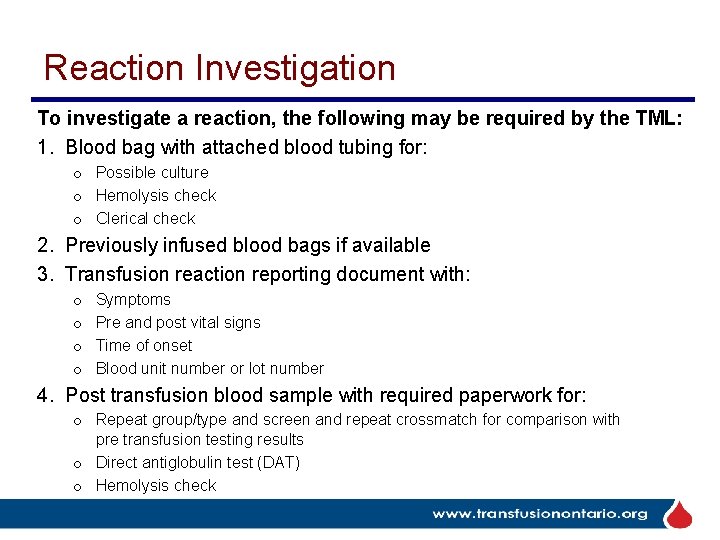
Reaction Investigation To investigate a reaction, the following may be required by the TML: 1. Blood bag with attached blood tubing for: o Possible culture o Hemolysis check o Clerical check 2. Previously infused blood bags if available 3. Transfusion reaction reporting document with: o o Symptoms Pre and post vital signs Time of onset Blood unit number or lot number 4. Post transfusion blood sample with required paperwork for: o Repeat group/type and screen and repeat crossmatch for comparison with pre transfusion testing results o Direct antiglobulin test (DAT) o Hemolysis check
Reaction Investigation Depending on patient signs and symptoms, additional testing my be required: • Next voided urine for hemoglobin testing – Monitor urine output if hemolysis suspected • Chest x-ray if patient has new respiratory symptoms • Blood cultures from the patient: – Drawn from a different vein – Antibiotics should be started immediately if bacterial sepsis suspected – Report immediately to the TML as the blood supplier/manufacturer must be alerted • Other blood samples may be required to investigate: – Anaphylactic reactions – TRALI – Acute hemolytic transfusion reaction
Reaction Investigation • The TML must report serious reactions to blood components/products to the manufacturer or the Canada Vigilance Program. Other components/products may be implicated and need to be recalled. • The TML may also report reactions to Ontario TTISS, which collects transfusion reaction data in order to monitor and improve transfusion safety for all patients.
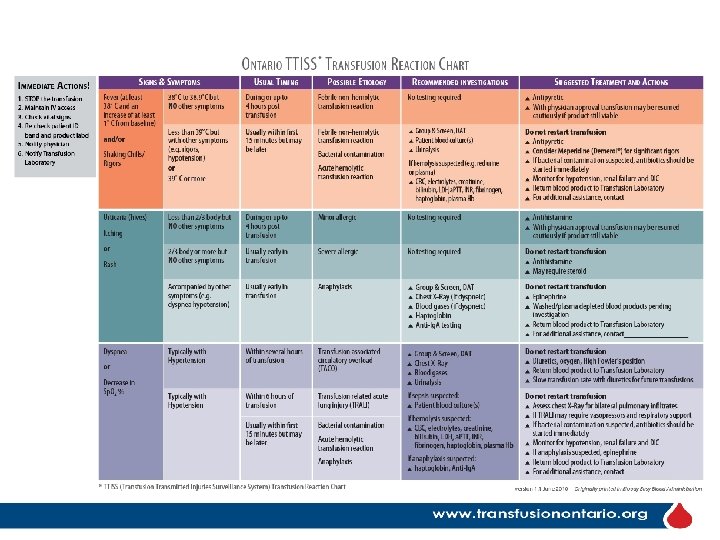
Ontario TTISS Transfusion Reaction Chart The Ontario TTISS Educational Committee has developed a Reaction Chart that is available for all hospitals to use. • Editable versions of the chart can be obtained from the ORBCo. N website – www. transfusionontario. org under TTISS Resources • As well it is included in the ORBCo. N handbook – Bloody Easy Blood Administration • The chart categorizes reactions by signs and symptoms and recommends investigations as well as suggested treatment and actions.
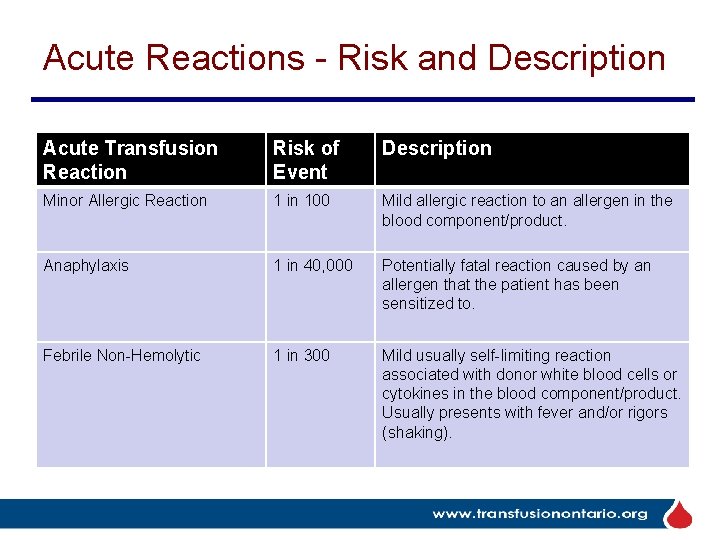
Acute Reactions - Risk and Description Acute Transfusion Reaction Risk of Event Description Minor Allergic Reaction 1 in 100 Mild allergic reaction to an allergen in the blood component/product. Anaphylaxis 1 in 40, 000 Potentially fatal reaction caused by an allergen that the patient has been sensitized to. Febrile Non-Hemolytic 1 in 300 Mild usually self-limiting reaction associated with donor white blood cells or cytokines in the blood component/product. Usually presents with fever and/or rigors (shaking).
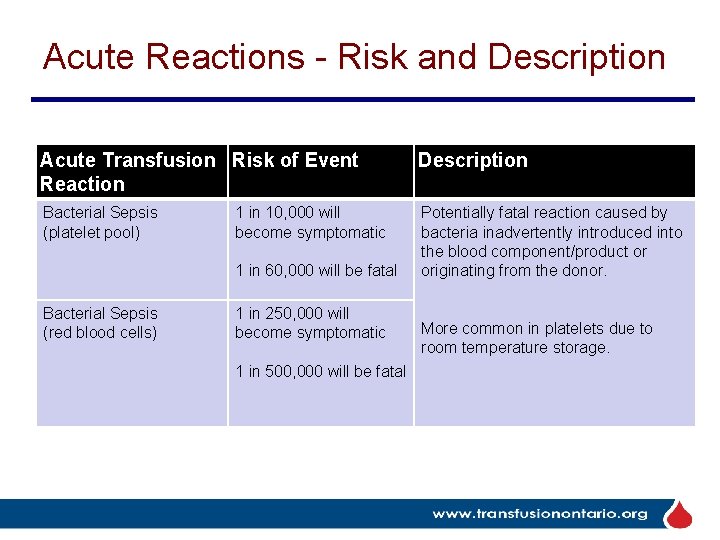
Acute Reactions - Risk and Description Acute Transfusion Risk of Event Reaction Description Bacterial Sepsis (platelet pool) Potentially fatal reaction caused by bacteria inadvertently introduced into the blood component/product or originating from the donor. 1 in 10, 000 will become symptomatic 1 in 60, 000 will be fatal Bacterial Sepsis (red blood cells) 1 in 250, 000 will become symptomatic 1 in 500, 000 will be fatal More common in platelets due to room temperature storage.
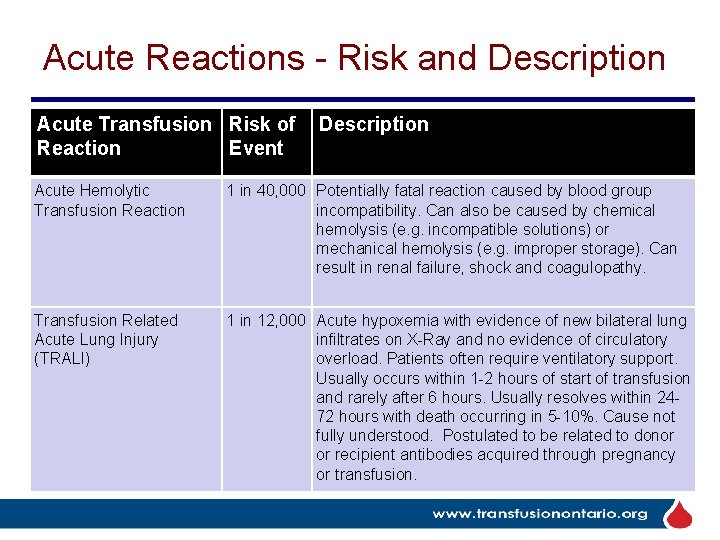
Acute Reactions - Risk and Description Acute Transfusion Risk of Reaction Event Description Acute Hemolytic Transfusion Reaction 1 in 40, 000 Potentially fatal reaction caused by blood group incompatibility. Can also be caused by chemical hemolysis (e. g. incompatible solutions) or mechanical hemolysis (e. g. improper storage). Can result in renal failure, shock and coagulopathy. Transfusion Related Acute Lung Injury (TRALI) 1 in 12, 000 Acute hypoxemia with evidence of new bilateral lung infiltrates on X-Ray and no evidence of circulatory overload. Patients often require ventilatory support. Usually occurs within 1 -2 hours of start of transfusion and rarely after 6 hours. Usually resolves within 2472 hours with death occurring in 5 -10%. Cause not fully understood. Postulated to be related to donor or recipient antibodies acquired through pregnancy or transfusion.
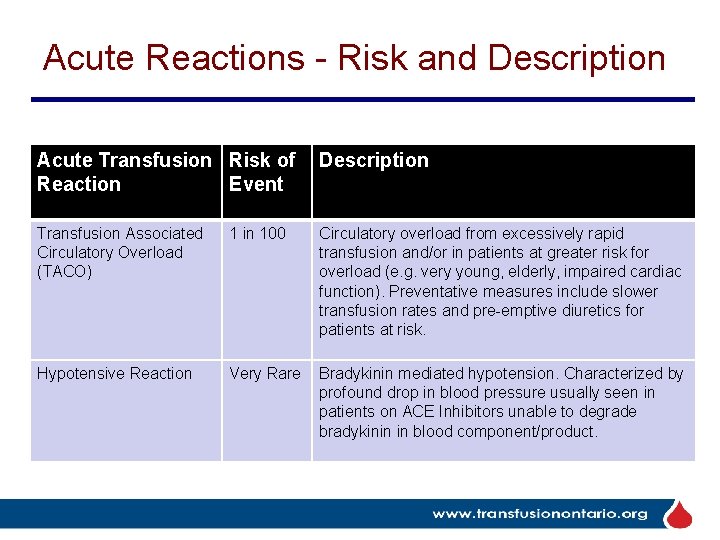
Acute Reactions - Risk and Description Acute Transfusion Risk of Reaction Event Description Transfusion Associated Circulatory Overload (TACO) 1 in 100 Circulatory overload from excessively rapid transfusion and/or in patients at greater risk for overload (e. g. very young, elderly, impaired cardiac function). Preventative measures include slower transfusion rates and pre-emptive diuretics for patients at risk. Hypotensive Reaction Very Rare Bradykinin mediated hypotension. Characterized by profound drop in blood pressure usually seen in patients on ACE Inhibitors unable to degrade bradykinin in blood component/product.
Assessment Quiz
1. Signs and symptoms that may be associated with a transfusion reaction include: a. b. c. d. e. Rash Fever Lumbar/Lower back pain Dyspnea All of the above
2. Serious reactions such as an Acute Hemolytic Transfusion Reaction usually present more than 6 hours after the completion of the transfusion. a. True b. False
3. You assess Luke White after the first 15 minutes of his transfusion and notice a red rash appearing on his chest and upper arms. What should you do first? a. Stop the transfusion and complete a patient assessment b. Increase the rate of infusion so the transfusion will finish before the symptoms worsen c. Slow the transfusion and reassess Luke in another 15 minutes d. Check Luke’s vital signs
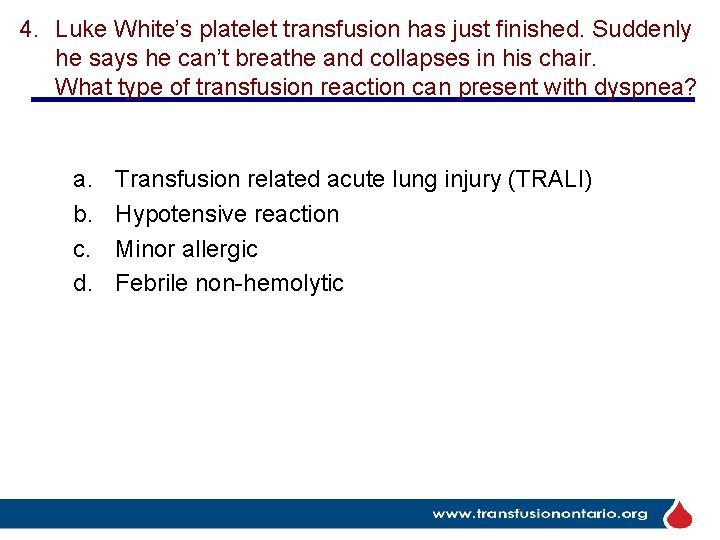
4. Luke White’s platelet transfusion has just finished. Suddenly he says he can’t breathe and collapses in his chair. What type of transfusion reaction can present with dyspnea? a. b. c. d. Transfusion related acute lung injury (TRALI) Hypotensive reaction Minor allergic Febrile non-hemolytic
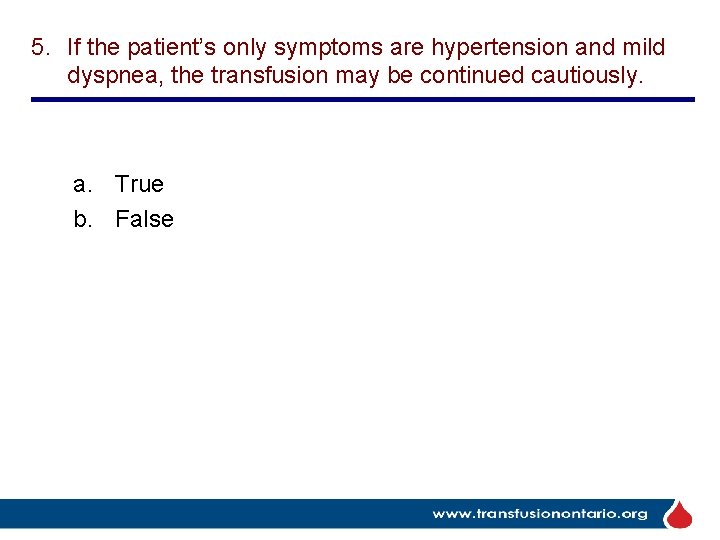
5. If the patient’s only symptoms are hypertension and mild dyspnea, the transfusion may be continued cautiously. a. True b. False
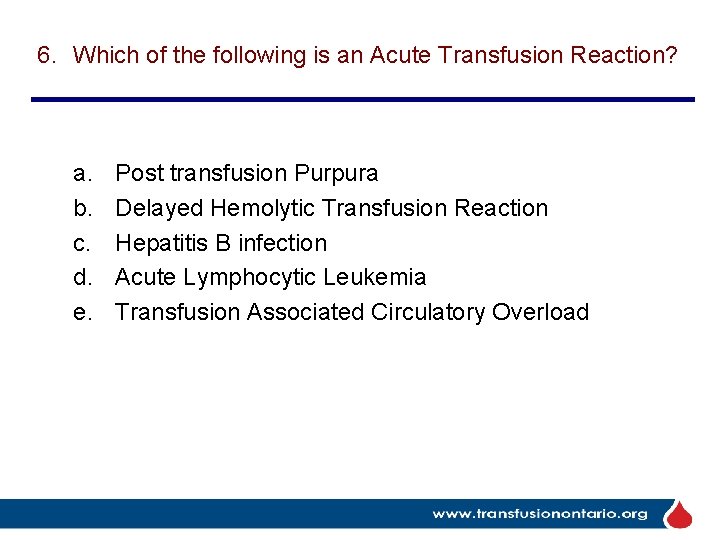
6. Which of the following is an Acute Transfusion Reaction? a. b. c. d. e. Post transfusion Purpura Delayed Hemolytic Transfusion Reaction Hepatitis B infection Acute Lymphocytic Leukemia Transfusion Associated Circulatory Overload
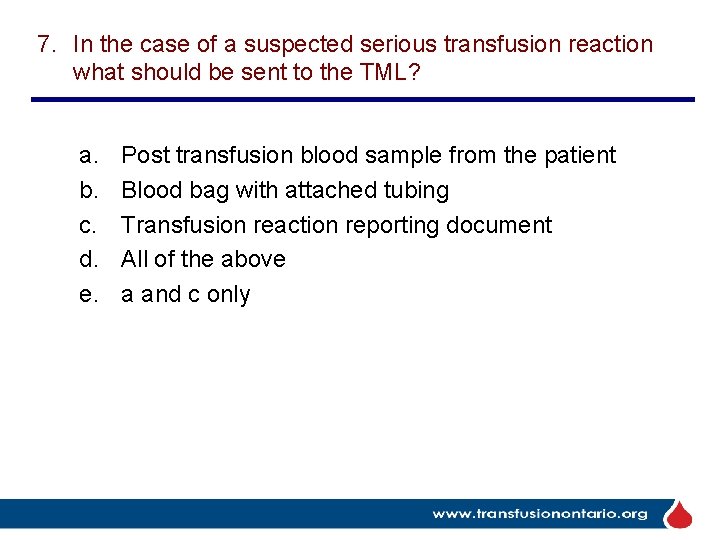
7. In the case of a suspected serious transfusion reaction what should be sent to the TML? a. b. c. d. e. Post transfusion blood sample from the patient Blood bag with attached tubing Transfusion reaction reporting document All of the above a and c only
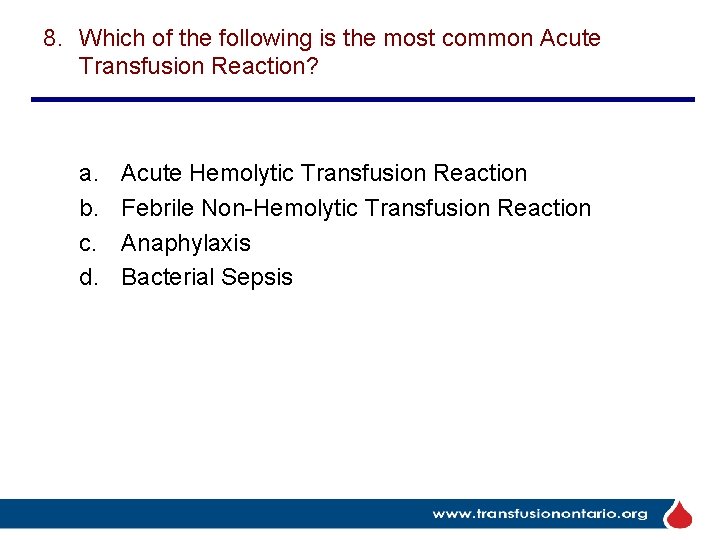
8. Which of the following is the most common Acute Transfusion Reaction? a. b. c. d. Acute Hemolytic Transfusion Reaction Febrile Non-Hemolytic Transfusion Reaction Anaphylaxis Bacterial Sepsis
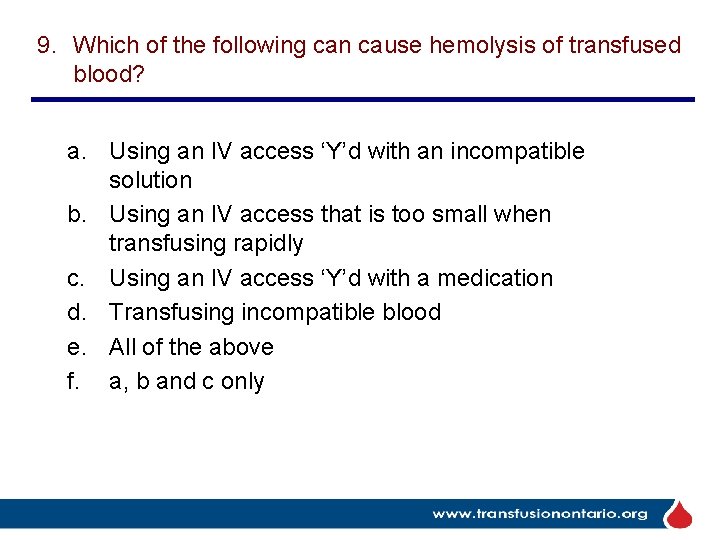
9. Which of the following can cause hemolysis of transfused blood? a. Using an IV access ‘Y’d with an incompatible solution b. Using an IV access that is too small when transfusing rapidly c. Using an IV access ‘Y’d with a medication d. Transfusing incompatible blood e. All of the above f. a, b and c only
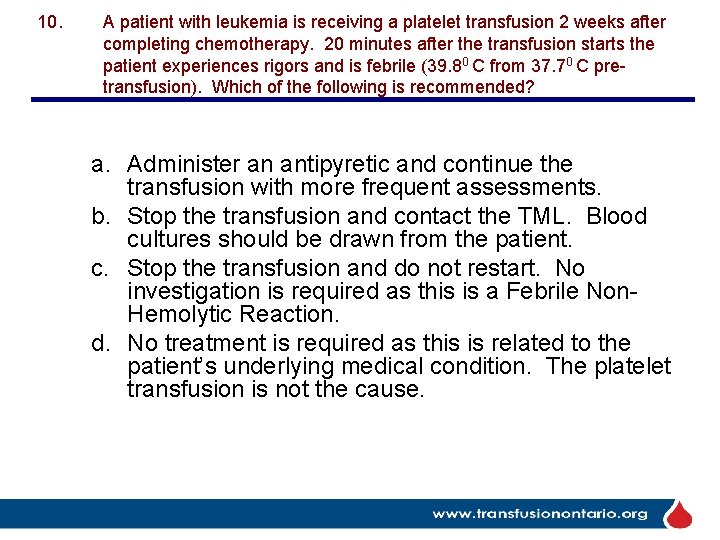
10. A patient with leukemia is receiving a platelet transfusion 2 weeks after completing chemotherapy. 20 minutes after the transfusion starts the patient experiences rigors and is febrile (39. 80 C from 37. 70 C pretransfusion). Which of the following is recommended? a. Administer an antipyretic and continue the transfusion with more frequent assessments. b. Stop the transfusion and contact the TML. Blood cultures should be drawn from the patient. c. Stop the transfusion and do not restart. No investigation is required as this is a Febrile Non. Hemolytic Reaction. d. No treatment is required as this is related to the patient’s underlying medical condition. The platelet transfusion is not the cause.
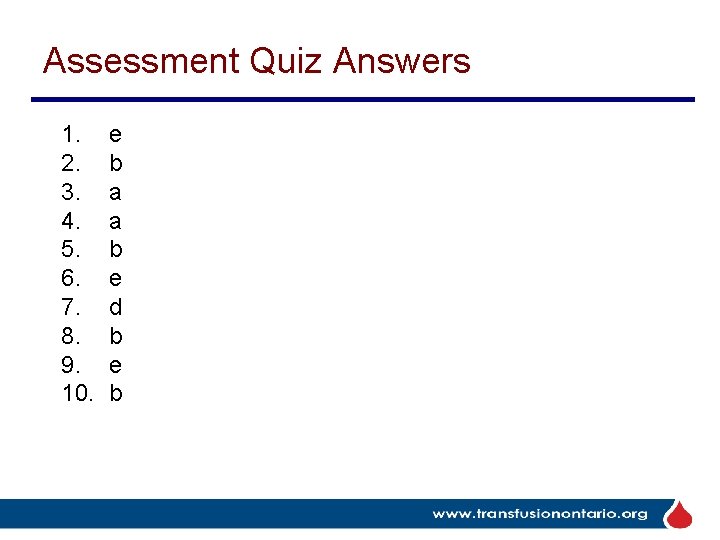
Assessment Quiz Answers 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. e b a a b e d b e b

NAME: Bloody Easy Blood Administration – Module 3 Date: _____
End of Module 3 Module 1 – Transfusing the Patient Module 2 – Indications and Compatibility
For more information please see: Bloody Easy Blood Administration e. Learning module www. transfusionontario. org
- Slides: 31