Bloodborne Pathogens Infection Prevention Practices Personal Protective Equipment
Bloodborne Pathogens Infection Prevention Practices Personal Protective Equipment Fall 2014 Communication Disorders and Sciences University of Oregon
Infection Control Procedures • These slides are intended to serve as a guideline for standard precautions and infection control procedures. A student clinician and intern should always refer to the facility rules and regulations
OSHA • The Occupational Health and Safety Administration (OSHA) is a federal agency that regulates the work place in an attempt to assure that all workers have a safe working environment
Joint Commission for the Accreditation of Healthcare Organizations (JCAHO) • JCAHO establishes standards for hospitals and other health care facilities • Each facility creates specific protocols for each department within the facility based on program needs
Modes of Transmission • Contact Transmission – Direct contact between infected person and a susceptible host – Indirect contact between susceptible host and a contaminated object – Droplet contact between an infectious organism and the mucus membranes of a susceptible host • Vehicle Route of Transmission – Disease is transmitted via a contaminated object such as food, water or blood • Airborne Transmission – Disease travels by droplet nuclei or dust particles through the airway – Kemp et al. (1995). Infection Control for the Professions of Audiology and Speech. Language Pathology. Singular Publishing.
Cross Contamination • The most common source of microbes capable of causing infection and diseases in humans is humans themselves – Coughing and sneezing expel and suspend particles of moisture in the air. These particles make it from one respiratory tract to another person’s respiratory tract • Individuals constantly touch various parts of their skin, mouth and nose, then inadvertently touch another person, or a surface that is touched by another person • Hands are the most common vehicle for spreading infection and cross contamination • Hand washing represents the best, preventive measure in the home and at work – Kemp et al. (1995). Infection Control for the Professions of Audiology and Speech. Language Pathology. Singular Publishing.
Principal Bloodborne Pathogens of Concern in Healthcare • Hepatitis B Virus (HBV) • Hepatitis C Virus (HCV) • Human Immunodeficiency Virus (HIV)
Hepatitis B Virus • Serious disease that affects liver • Ranges from mild illness to life-long liver disease • Acute HBV - Symptoms last only a few weeks; symptoms often absent • Chronic HBV- can cause liver damage, liver failure, liver cancer, or even death • An estimated 1. 4 million people in the US have chronic Hepatitis C • Transmission – Birth (spread from an infected mother to her baby during birth) – Sex with an infected partner Sharing needles, syringes, or other druginjection equipment – Sharing items such as razors or toothbrushes with an infected person – Direct contact with the blood or open sores of an infected person – Exposure to blood from needlesticks or other sharp instruments From: http: //www. cdc. gov/hepatitis/B/b. FAQ. htm#overview
Vaccination for HBV • Vaccination gives protection from Hepatitis B, possibly life-long – 3 -4 shots over 6 -month period – Safety of vaccination • Very safe vaccine • Contains non-infectious material • Mild problems (soreness, fever) From: http: //www. cdc. gov/hepatitis/B/b. FAQ. htm#overview
Hepatitis C Virus Contagious liver disease Ranges from mild illness to life-long liver disease No vaccination available for Hepatitis C An estimated 3. 2 million people in the US have Hepatitis C. They often do not know they have hepatitis as they do not feel/look sick. • Transmission • • – – Sharing needles, syringes, or other equipment to inject drugs Needlestick injuries in health care settings Being born to a mother who has Hepatitis C Less common: sharing personal items that have been in contact with blood; sexual contact From: http: //www. cdc. gov/hepatitis/C/c. FAQ. htm#overview
HIV/AIDS • HIV - human immunodeficiency virus; can lead to acquired immunodeficiency syndrome (AIDS) • No vaccine, no cure available – lifelong disease • HIV can be controlled through antiretroviral therapy • Transmission – – Sexual contact with someone who has HIV Sharing needles, syringes etc. Needlestick injuries in health care settings Being born to a mother who has HIV From: http: //www. cdc. gov/hiv/basics/index. html
Tuberculosis (TB) • Airborne disease • Transmission – Transmission through coughing, sneezing, shouting, or singing. Transmission of TB occurs when other person inhales TB droplet nuclei. – Particles can remain in air for several hours. – Not transmitted through surface contact. • Symptoms – – – – Cough for 3 or more weeks Pain in chest Coughing up blood Weakness or fatigue Weight loss, no appetite Chills & fever Sweating at night From: http: //www. cdc. gov/tb/topic/basics/default. htm
Testing for TB • TB skin test, TB blood test – A positive TB skin/blood test can be caused by latent TB infection or active TB disease • Positive skin test – person has been infected with TB bacteria • Negative skin test –No reaction to test; latent TB infection or active TB disease highly unlikely – TB skin test, aka PPD test (purified protein derivative) or Mantoux tuberculin skin test – TB blood test, aka IGRA – Quanti. FERON®-TB test (QFT) • http: //www. cdc. gov/tb/topic/testing/default. htm • http: //www. cdc. gov/mmwr/preview/mmwrhtml/rr 5202 a 2. htm
Standard Precautions in Healthcare Settings • A healthcare worker is to assume that every client/patient is a potential carrier of an infectious disease • An effective infection control program begins with this mindset • Standard Precautions are meant to safeguard workers and their clients/patients against all potentially infectious body substances
Standard Precautions in Healthcare Settings • The CDC recommends Standard Precautions for the care of all patients, regardless of their diagnosis or presumed infection status. • Standard Precautions apply to 1) blood; 2) all body fluids, secretions, and excretions, except sweat, regardless of whether or not they contain visible blood; 3) non-intact skin; and 4) mucous membranes. Standard precautions are designed to reduce the risk of transmission of microorganisms from both recognized and unrecognized sources of infection in hospitals. – Standard precautions includes the use of: hand washing, appropriate personal protective equipment such as gloves, gowns, masks, whenever touching or exposure to patients' body fluids is anticipated. From: https: //www. osha. gov/SLTC/etools/hospital/hazards/univprec/univ. html
Standard Precautions Handwashing Protocol • Wash before and after each patient/client, after cleaning toys and after removing gloves – Remove all rings, and place in a safe place – If water is not available, use a no-rinse alcohol-based sanitizer if hands not visibly soiled. – Start with water, add soap, and lather up scrubbing palms, the backs of your hands, wrist and lower forearms. Minimum 20 seconds (sing 2 x Happy Birthday!), don’t forget to clean fingernails and between fingers – Thoroughly rinse of soap under running water – Dry hands by blotting, using a paper towel – Turn off water using the paper towel, not your clean hands – Use hand lotion as needed to keep hands from chapping.
Standard Precautions Alcohol-Based Hand Sanitizers • Use sanitizers with 60 -95% alcohol concentration • Use only if hands are not visibly dirty or greasy • Advantage – Hand sanitizers require less time than hand-washing with soap and water. - Rub hands until dry – Bottles/dispensers can be placed at the point of care so they are more accessible than soap and water. • Note - Soap and water are more effective than hand sanitizers at removing or inactivating certain kinds of germs (e. g. , Cryptosporidium, norovirus, and Clostridium difficile. ) From: http: //www. cdc. gov/handhygiene/; http: //www. cdc. gov/handwashing/showme-the-science-hand-sanitizer. html
Standard Precautions Protocol for proper use of gloves • Use latex-free (nitrile or vinyl) examination gloves. • Gloves should fit properly. • Wash hands or use sanitizer prior to putting gloves on and after taking gloves off. • Change gloves between patients. If a glove becomes torn or perforated, replace it. Never reuse disposable gloves • If client questions use of gloves, explain that gloves are worn to protect client, and are a precautionary measure • Place bandages on open sores or cuts prior to putting on gloves • Double-glove when treating patients known to be infected with HIV or Hepatitis B
Standard Precautions Removing gloves • Peel off one glove from the wrist to the fingertip, then grasp it in the gloved hand • Using the bared hand, peel off the second glove from the inside, touching the first glove inside the second glove as it is removed • Immediately dispose of glove in appropriate container, DO NOT place gloves on table, etc, to dispose of later • Wash hands thoroughly when completed
Universal Precautions - Bloodborne Pathogens • “Universal precautions is an approach to infection control to treat all human blood and certain human body fluids as if they were known to be infectious for HIV, HBV and other bloodborne pathogens, ” (Bloodborne Pathogens Standard 29 CFR 1910. 1030(b) definitions). • “Blood is the single most important source of HIV, HBV, and other bloodborne pathogens in the occupational setting. ” http: //www. cdc. gov/mmwr/preview/mmwrhtml/00000039. htm • Protective barriers – Wear gloves, gowns, masks, and protective eyewear depending on exposure risk – “Universal precautions do not apply to saliva. …Gloves need not be worn when feeding patients and when wiping saliva from skin. “http: //www. cdc. gov/mmwr/preview/mmwrhtml/00000039. htm • “Immediately and thoroughly wash hands and other skin surfaces that are contaminated with blood, body fluids containing visible blood, or other body fluids to which universal precautions apply. ” http: //www. cdc. gov/mmwr/preview/mmwrhtml/00000039. htm • Take care to prevent injuries from needles or other sharp instruments. Use puncture-resistant containers for disposal.
Airborne Precautions in Health Care Settings • Used for diseases such as tuberculosis, measles, and chickenpox • Patient is in private room that allows control of airborne diseases • People entering the room must wear respiratory protection
Droplet Precautions in Health Care Settings • Used for diseases such as meningococcal disease, pertussis (whooping cough) and influenza • Transmission requires close contact as droplets travel only about 3 to 5 feet • Use surgical mask when having close contact • Educate patient and family on respiratory etiquette (cover your cough, hand hygiene) – Cover your cough poster http: //www. cdc. gov/flu/protect/pdf/covercough_school 8 -5 x 11. pdf
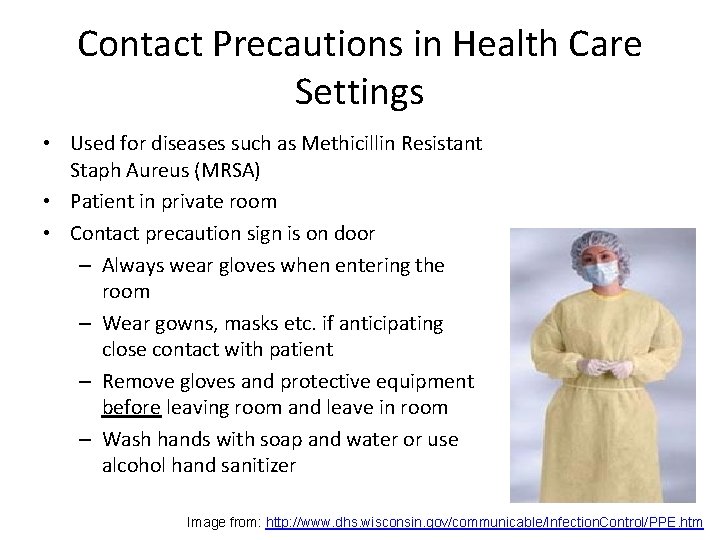
Contact Precautions in Health Care Settings • Used for diseases such as Methicillin Resistant Staph Aureus (MRSA) • Patient in private room • Contact precaution sign is on door – Always wear gloves when entering the room – Wear gowns, masks etc. if anticipating close contact with patient – Remove gloves and protective equipment before leaving room and leave in room – Wash hands with soap and water or use alcohol hand sanitizer Image from: http: //www. dhs. wisconsin. gov/communicable/Infection. Control/PPE. htm
HEDCO Clinic Cleaning Surfaces in the Client Room • Each clinic room has disposable gloves, alcoholbased hand sanitizers and infection control cleaning supplies, including wipes for disinfecting tables and chairs after each session. • Each table is to be wiped down with antibacterial wipes (located in each room) after client leaves the room. • If an accident occurs involving blood, use the bloodborne pathogen kit located in the kitchen area above the sink for disposal.
HEDCO Clinic Cleaning Toys and Other Material • Toys should be cleaned after each session. You are responsible for cleaning the toys you use. • Use the antibacterial wipes that are located in each clinic room to clean the toys. • Return toys to the appropriate place when dry. • Audiology: Audiological headsets should be wiped down with alcohol wipes after each use. Dispose of alcohol wipes in waste basked lined with plastic bags immediately after use.
HEDCO Clinic Use of Tongue Depressors • Each clinic room has disposable tongue depressors. • Prior to an oral examination, be careful not to touch with your bare hands the part of the tongue depressor that will be inserted into the client’s mouth. • Dispose of depressor immediately after use.
Fire and Electrical Safety • Lalla?
Hazard Communications • According to OSHA, hazardous materials include chemicals that can cause physical hazards (such as flammability) and health hazards (such as irritation, lung damage, and cancer. ) https: //www. osha. gov/Publications/osha 3111. html • Students in speech-language pathology may be exposed to these materials in their offcampus medical placements. Facilities will provide training specific to their regulations.
Final words …. • • Protect yourself and your clients/patients Many diseases are preventable Familiarize yourself with facility regulations Always follow infection prevention practices and facility regulations!
- Slides: 29