BLOODBORNE PATHOGEN AWARENESS TRAINING PRESENTED BY Texas Family
BLOODBORNE PATHOGEN AWARENESS TRAINING PRESENTED BY Texas Family Medicine Preceptorship Program UT Medical School at Houston Environmental Health & Safety
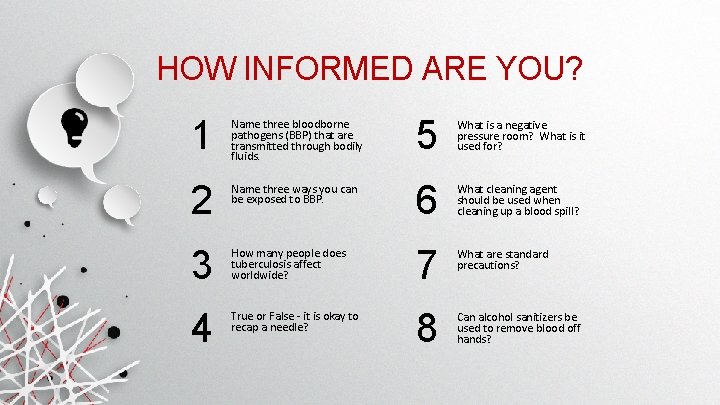
HOW INFORMED ARE YOU? 1 Name three bloodborne pathogens (BBP) that are transmitted through bodily fluids. 5 What is a negative pressure room? What is it used for? 2 Name three ways you can be exposed to BBP. 6 What cleaning agent should be used when cleaning up a blood spill? 3 How many people does tuberculosis affect worldwide? 7 What are standard precautions? 4 True or False - it is okay to recap a needle? 8 Can alcohol sanitizers be used to remove blood off hands?
TRAINING OUTLINE What is a bloodborne pathogen? What do UTHSC-H statistics say? Preventive measures Needlestick injury & exposure information TB presentation & isolation Your rights Blood or other potentially infectious material (OPIM) spill clean up
OSHA Bloodborne Pathogen Standard 29 CFR 1910. 1030 OSHA Bloodborne Pathogen Standard The standard was originally issued in 1991, and was later revised for the prevention of contaminated sharps injuries, needlesticks In 2001 the revised standard, Needlestick Safety and Prevention Act included: • Education and selection of sharps injury reduction devices (e. g. , selfsheathing needles) • Maintenance of a contaminated Sharps Injury Log

Texas Department of State Health Service BLOODBORNE PATHOGEN CONTROL Exposure Control Plan: • Reflect advanced technology that eliminate or reduce exposures • Document annually consideration for safer medical devices • Solicit input from employees at higher risk of occupational exposure. POWERPOINT PRESENTATION
B loodborne PATHOGENS (BBP) Pathogenic microorganisms present in human blood or other potentially infectious material (OPIM), and can infect and cause disease in humans. These pathogens include, but are not limited to, hepatitis B virus (HBV), hepatitis C virus, and human immunodeficiency virus (HIV).
B loodborne PATHOGENS (BBP) - HIV - HBV - HCV - T. pallidum - Herpes Virus - M. tuberculosis - typically an aerosol hazard - Human T-Lymphotropic Virus Type l (HTLV-l)
B loodborne PATHOGENS (BBP) Body fluids that can harbor BBP: - Blood - Semen and vaginal secretions - Saliva involved in dental procedures - Synovial fluid - Cerebrospinal fluid - Human tissue and cell cultures - All body fluids containing blood e. g. fluids: pleural, pericardial, amniotic

2 1 3 FIRST SECOND THIRD Mucous membrane contact Percutaneous inoculation Exposure to broken/damaged skin - Splash in eyes, nose, or mouth - Misuse of sharps (broken glass, needles, scalpels) - Risk increases if contact involves a large area of broken/damaged skin or if contact is prolonged OCCUPATIONAL EXPOSURE* * Risk increases with high titer levels in the source
How do you get exposed? • • • Needlesticks or cuts from used needles or sharps Contact of eyes, nose, mouth or broken skin with blood Assaults – bites, cuts, knife wounds Punctures Splashes What should I do if I get exposed? REPORT ASAP, then: • Needlestick and cuts – wash with soap and water • Splashes – flush nose, mouse, or skin with water • Splashes in the eyes – irrigate with water, saline, or sterile wash

Engineering controls Personal Protective Equipment (PPE) Administrative controls Work place practices PREVENTIVE MEASURES
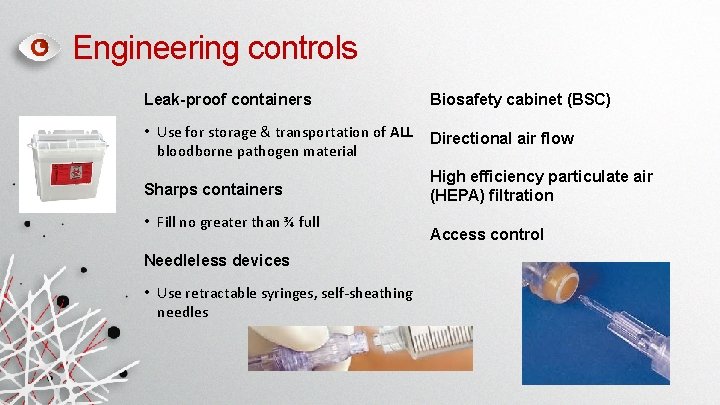
Engineering controls Leak-proof containers Biosafety cabinet (BSC) • Use for storage & transportation of ALL bloodborne pathogen material Directional air flow Sharps containers High efficiency particulate air (HEPA) filtration • Fill no greater than ¾ full Needleless devices • Use retractable syringes, self-sheathing needles Access control
Personal Protective Equipment Face protection • Goggles or safety glasses with side shields Clothing • Lab coats, scrubs, disposable gowns (long pants only and no open toed shoes) • Replaced immediately when contaminated • Lab clothing restricted to work area Gloves • Replaced immediately if torn • Not worn outside the lab area!
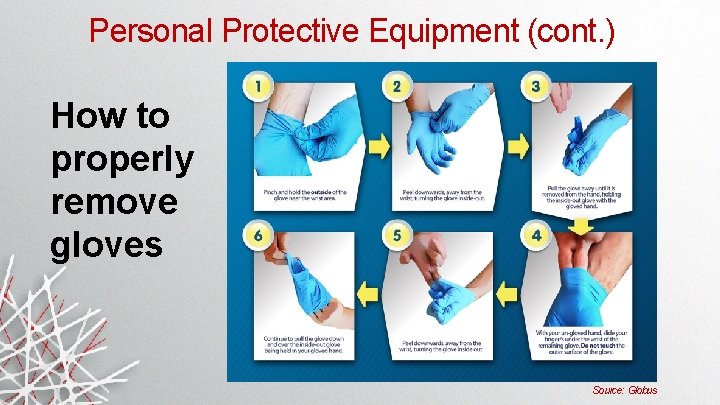
Personal Protective Equipment (cont. ) How to properly remove gloves Source: Globus
Administrative Controls Medical surveillance • TB skin test (PPD) Immunizations • Hepatitis B series Training Management of staff (SOP compliance) Background checks, security clearance
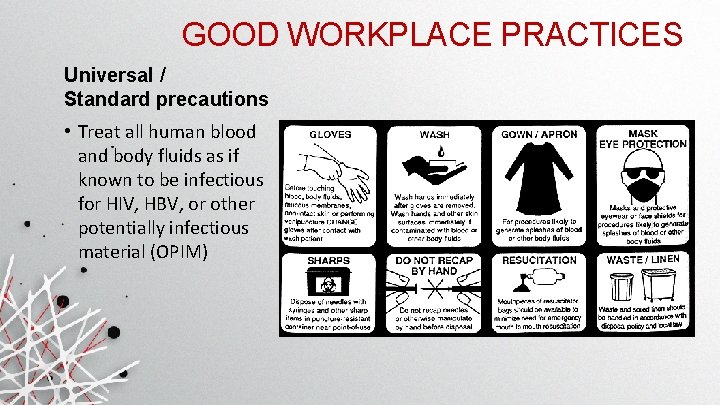
GOOD WORKPLACE PRACTICES Universal / Standard precautions • Treat all human blood and body fluids as if known to be infectious for HIV, HBV, or other potentially infectious material (OPIM)
GOOD WORKPLACE PRACTICES NEVER recap needles! Follow SOPs Survey work area • Note locations of all necessary equipment, waste containers, disinfectants, and soaps Establish & maintain clean & dirty zones DO NOT eat, drink, or apply cosmetics in the work area
GOOD WORKPLACE PRACTICES (cont. ) Decontaminate work surfaces • At start and end of procedures • Immediately after spill • Before removal of equipment Dispose of waste properly Label containers – hazard communication • Chemical & biological working stocks Wash hands frequently, always between patients & always before leaving work area!
GOOD WORKPLACE PRACTICES (cont. ) How can you protect yourself overall? • • • Get the hepatitis B vaccine Review the employer’s Exposure Control Plan Dispose of sharps PROMPTLY into an appropriate container Use sharps devices with safety features Clean work surfaces Use personal protective equipment (such as gloves and face shields)
ROUTINE DECONTAMINATION ALCOHOL BLEACH CIDEX Cleaning agents/disinfectants you will encounter Start from perimeter and work your way in
Hand Hygiene On average only 40% of healthcare workers regularly wash their hands Hospital acquired infections result in transmission of: • MRSA – Methicillin resistant S. aureus • 1. 2 million infections; 48, 000 patient deaths yearly • VRE – Vancomycin resistant Enterococci • $4. 5 billion yearly cost for treatment Methods of contamination: • Moving patients • Taking blood pressure • Touching bedrails Source: Hand Hygiene Resource Center http: //www. handhygiene. org/
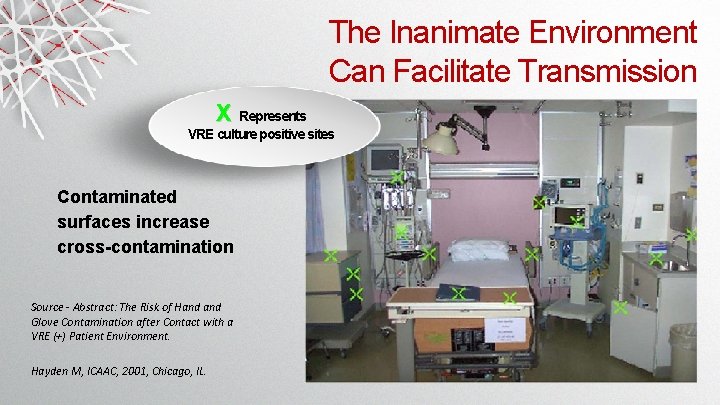
The Inanimate Environment Can Facilitate Transmission X Represents VRE culture positive sites Contaminated surfaces increase cross-contamination Source - Abstract: The Risk of Hand Glove Contamination after Contact with a VRE (+) Patient Environment. Hayden M, ICAAC, 2001, Chicago, IL.
Proper hand washing is VITAL to infection prevention! You may not realize you have germs on your hands! Hand Hygiene (cont. ) Wash your hands, even if gloves have been worn… • Before patient contact, including between different patients • AFTER contact with anything contaminated • During patient care • Before and after invasive procedure • Before and after contact with wound • Between procedures on different body parts of the same patient • Between glove changes • Immediately if skin is contaminated or if an injury occurs
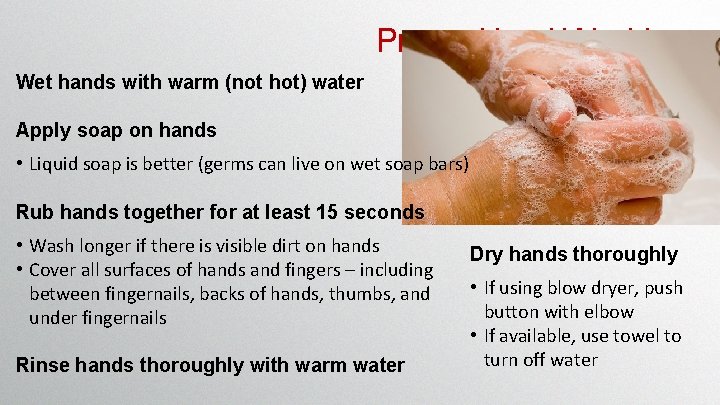
Proper Hand Washing Wet hands with warm (not hot) water Apply soap on hands • Liquid soap is better (germs can live on wet soap bars) Rub hands together for at least 15 seconds • Wash longer if there is visible dirt on hands • Cover all surfaces of hands and fingers – including between fingernails, backs of hands, thumbs, and under fingernails Rinse hands thoroughly with warm water Dry hands thoroughly • If using blow dryer, push button with elbow • If available, use towel to turn off water

WHAT SONG IS ABOUT 15 SECONDS LONG?
“Happy Birthday” Song -or“ABC” Song Source: Hand Hygiene Resource Center http: //www. handhygiene. org/
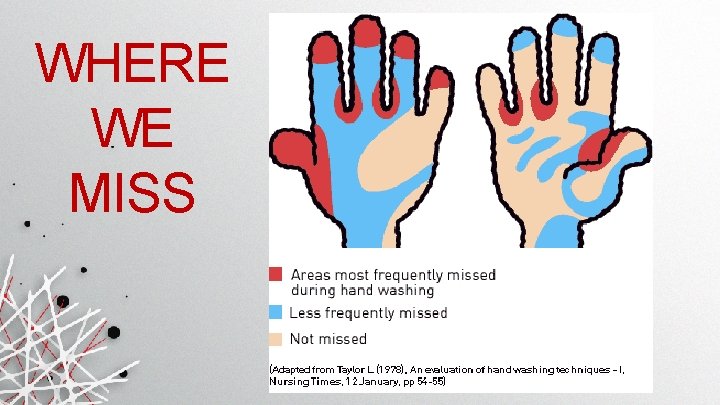
WHERE WE MISS
Hand Hygiene (cont. ) Alcohol sanitizers • 62% ethyl alcohol • Accepted as effective under certain conditions • Should not be used when there is visible dirt or grime
Hand Hygiene (cont. ) WASH BEFORE WASH AFTER Eating Using Toilet Caring for someone who is sick Blowing nose, coughing, or sneezing Caring for someone who is sick
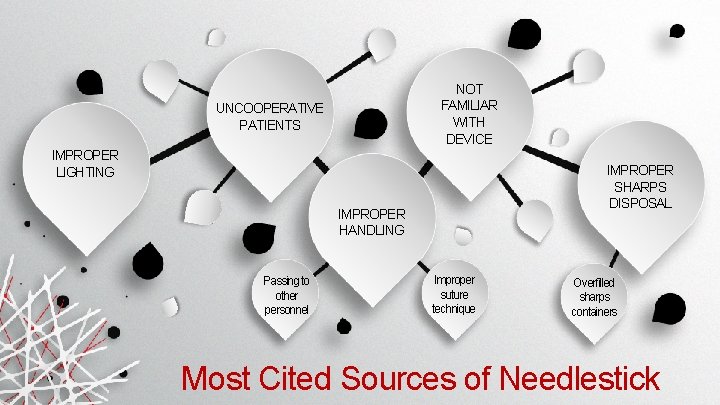
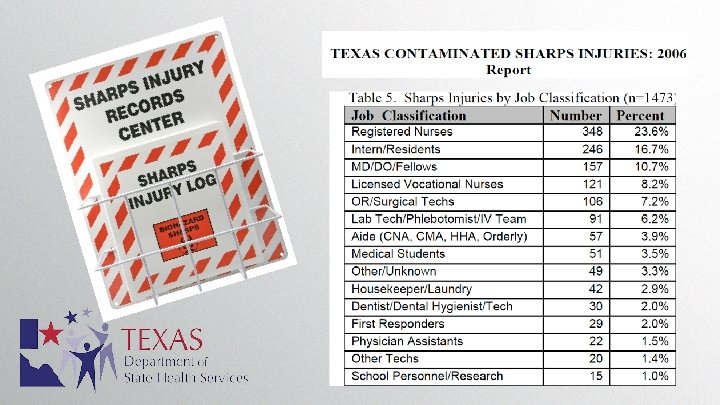
NOT FAMILIAR WITH DEVICE UNCOOPERATIVE PATIENTS IMPROPER LIGHTING IMPROPER SHARPS DISPOSAL IMPROPER HANDLING Passing to other personnel Improper suture technique Overfilled sharps containers Most Cited Sources of Needlestick
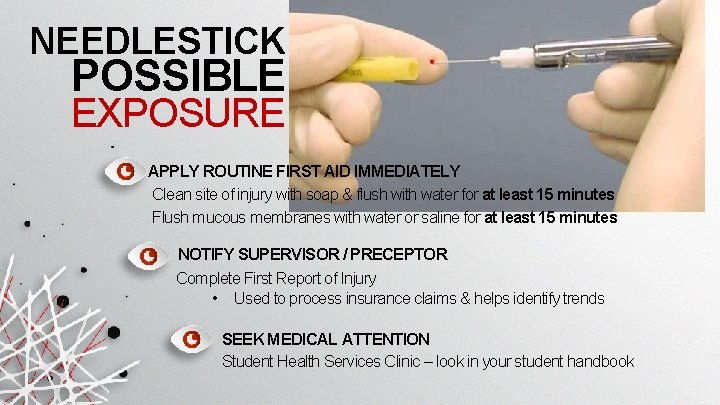
NEEDLESTICK POSSIBLE EXPOSURE APPLY ROUTINE FIRST AID IMMEDIATELY Clean site of injury with soap & flush with water for at least 15 minutes Flush mucous membranes with water or saline for at least 15 minutes NOTIFY SUPERVISOR / PRECEPTOR Complete First Report of Injury • Used to process insurance claims & helps identify trends SEEK MEDICAL ATTENTION Student Health Services Clinic – look in your student handbook
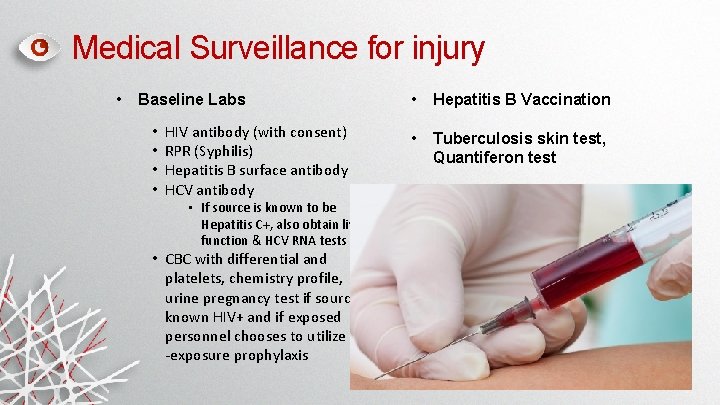
Medical Surveillance for injury • Baseline Labs • • HIV antibody (with consent) RPR (Syphilis) Hepatitis B surface antibody HCV antibody • If source is known to be Hepatitis C+, also obtain liver function & HCV RNA tests • CBC with differential and platelets, chemistry profile, urine pregnancy test if source is known HIV+ and if exposed personnel chooses to utilize post -exposure prophylaxis • Hepatitis B Vaccination • Tuberculosis skin test, Quantiferon test
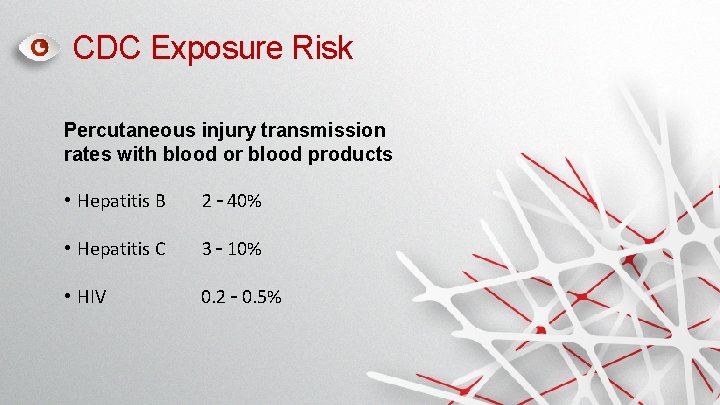
CDC Exposure Risk Percutaneous injury transmission rates with blood or blood products • Hepatitis B 2 – 40% • Hepatitis C 3 – 10% • HIV 0. 2 – 0. 5%
TB Presentation & Isolation Cough Chest Pain Coughing up blood Weakness Fever and/or night sweats Weight loss
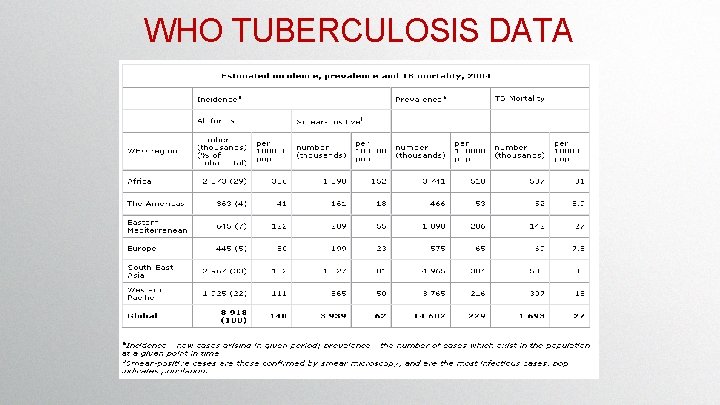
WHO TUBERCULOSIS DATA
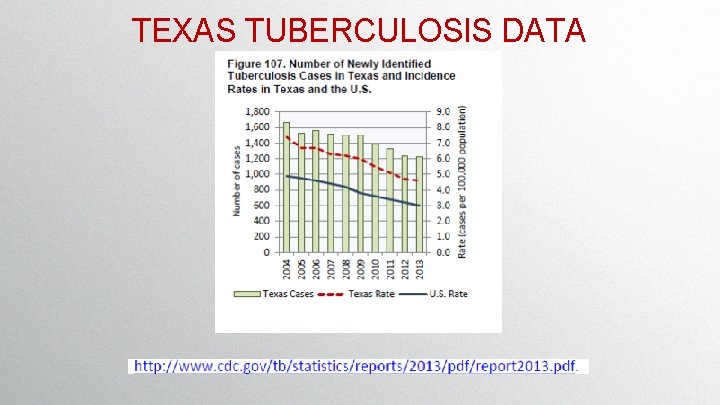
TEXAS TUBERCULOSIS DATA
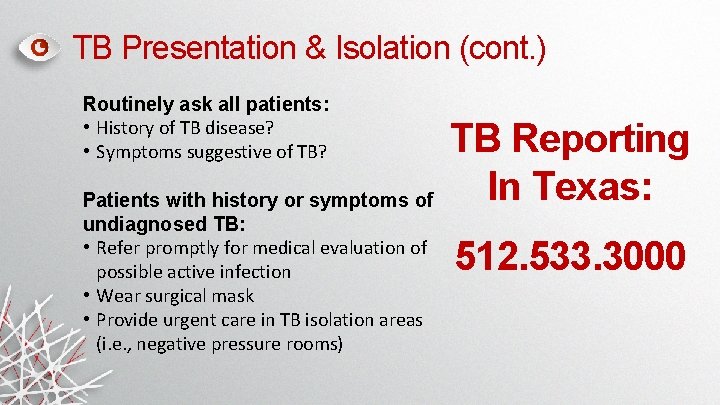
TB Presentation & Isolation (cont. ) Routinely ask all patients: • History of TB disease? • Symptoms suggestive of TB? Patients with history or symptoms of undiagnosed TB: • Refer promptly for medical evaluation of possible active infection • Wear surgical mask • Provide urgent care in TB isolation areas (i. e. , negative pressure rooms) TB Reporting In Texas: 512. 533. 3000
TB Presentation and Isolation (cont. ) REMINDER Bloodborne Pathogens can be transmitted via the following routes: • Airborne • Droplet • Contact
How to protect yourself & the patient REMEMBER Place mask on patient Use an N-95 respirator when caring for the patient (get fitted) • Routine duties • Sputum-inducing procedure Enforce cough etiquette
YOUR RIGHTS In the event of a possible exposure to bloodborne pathogens, the person is entitled to: • Confidential medical evaluation and follow-up • Documentation of routes of exposure • Identification, documentation, testing, and results of the source individual • Counseling • Evaluation of reported illness • Source patient blood draw
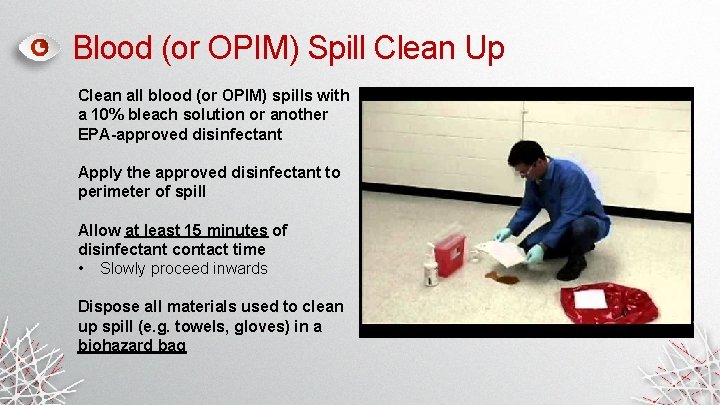
Blood (or OPIM) Spill Clean Up Clean all blood (or OPIM) spills with a 10% bleach solution or another EPA-approved disinfectant Apply the approved disinfectant to perimeter of spill Allow at least 15 minutes of disinfectant contact time • Slowly proceed inwards Dispose all materials used to clean up spill (e. g. towels, gloves) in a biohazard bag
Biological Waste Disposal Place red biohazard bags inside hard-walled, leak-proof secondary containment • Do not over fill! Place sharps in an appropriate hard -walled, leak-proof sharps container • Do not recap needles! • Do not over fill (no more than ¾ full)! • Let clinic administrator or manager know if it needs to be replaced
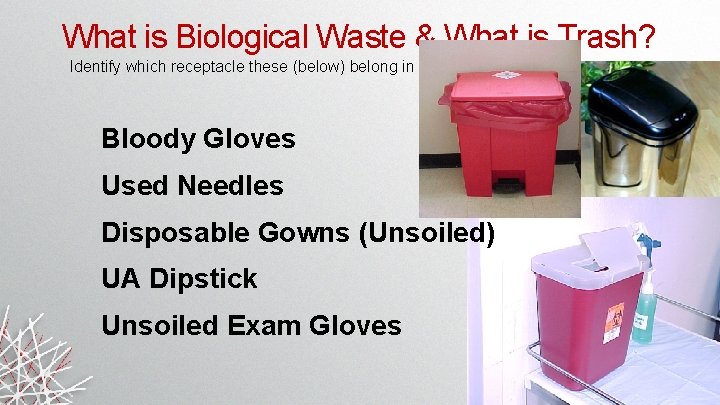
What is Biological Waste & What is Trash? Identify which receptacle these (below) belong in Bloody Gloves Used Needles Disposable Gowns (Unsoiled) UA Dipstick Unsoiled Exam Gloves

What is Biological Waste & What is Trash? Used Needles Bloody Gloves UA Dipstick Unsoiled Exam Gloves Disposable Gowns (Unsoiled)
INFORMATION RESOURCES Available resources about bloodborne pathogens • Contact your Occupational or Employee Health Clinic or report to the Institutional Emergency Department IMMEDIATELY • Biological Safety Manual (in every lab & website) • OSHA Bloodborne Pathogen Standard • Center for Disease Control • Texas Department of State Health Services
REMEMBER! You are responsible for knowing and practicing all the BBP training and safety precautions outlined in this presentation while participating in your Family Medicine preceptorship. Make sure you have your preceptors number and tell someone immediately when you are exposed to any bloodborne pathogens.
QUESTIONS? Refer to your Student Handbook Please remember: Contact your preceptor immediately following any exposures Go to the nearest Occupational or Employee Health Clinic or go to the Emergency Department for treatment

THANK YOU FOR LEARNING
- Slides: 50