Blood Transfusion Reaction in neonates management Dr Azita
Blood Transfusion Reaction in neonates & management Dr. Azita Azarkeivan Pediatric Hematology Oncology Adult Thalassemia Clinic
Complications of Transfusion n Transfusion reactions occur in 2% of units or within 24 hours of use. Most common adverse side effects are usually mild and non-life-threatening In New born and infants these complications may have some differences

Complications of Transfusion in newborn and infants n n Small Blood volume Passive transfer of maternal antibody Immature Immune system CMV , TA-GVHD
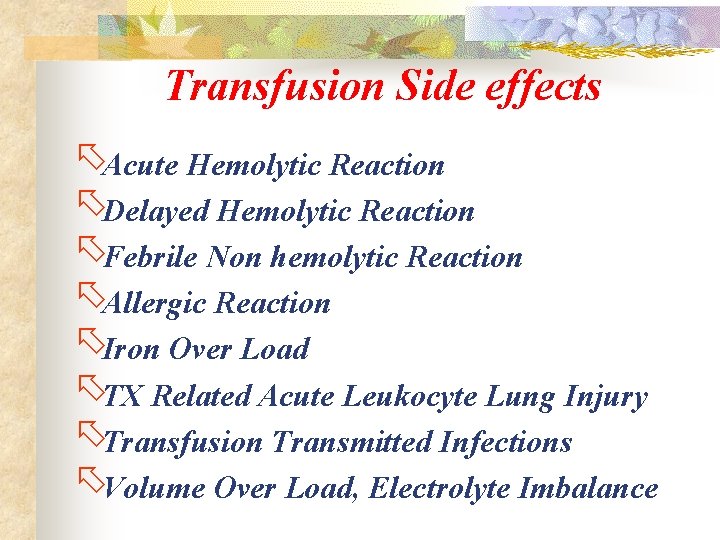
Transfusion Side effects õAcute Hemolytic Reaction õDelayed Hemolytic Reaction õFebrile Non hemolytic Reaction õAllergic Reaction õIron Over Load õTX Related Acute Leukocyte Lung Injury õTransfusion Transmitted Infections õVolume Over Load, Electrolyte Imbalance
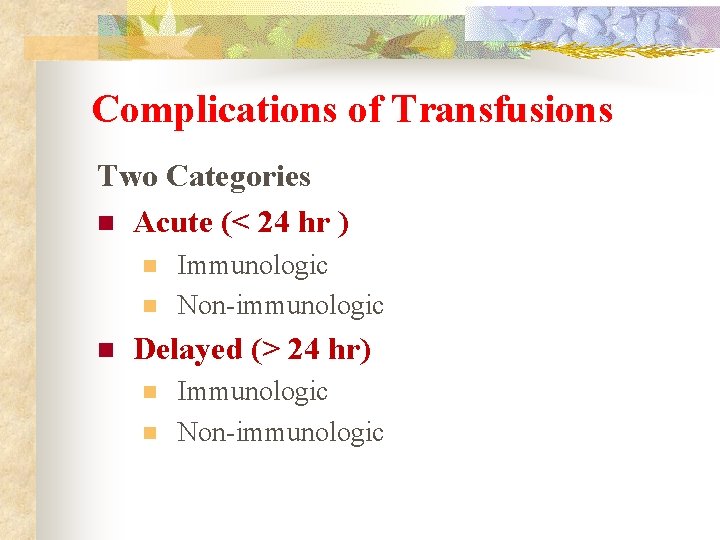
Complications of Transfusions Two Categories n Acute (< 24 hr ) n n n Immunologic Non-immunologic Delayed (> 24 hr) n n Immunologic Non-immunologic
Acute Immunologic (< 24 hr) Transfusion Reactions
Acute (< 24 hr) Immunologic n n n Hemolytic Febrile ; Fever , chills, non-hemolytic Allergic ; Urticarial , non-hemolytic Transfusion-related acute lung injury (TRALI) Anaphylactic ( Ig. A related)
Acute (< 24 hr) Immunologic Hemolytic Ø Ø Mostly ABO incompatibility A clerical error (wrong specimen, wrong patient) Sever hemolysis , In new born the ABO gp antigens not developed well and also their antibodies are not in high level Ø But The maternal antibodies may pass from mother and these antibodies may produce hemolysis in new born Ø Prevention : Correct ABO grouping of patient and blood bag Careful cross match with maternal serum
Acute (< 24 hr) Immunologic ä ä ä ä Febrile FNHTR , Rise in temperature by 2 F or 1 C HLA alloab of pt against Donor’WBC Recipient has WBC antibodies against donor WBCs contained within RBCs and Platelet products No hemolysis, Often occurs after multiple blood transfusions. In newborn and infants not very common Prevention : Use of leukoreduced product It should be to rolled out the other causes for fever for the patient Anti pyretic should use if there is no other cause
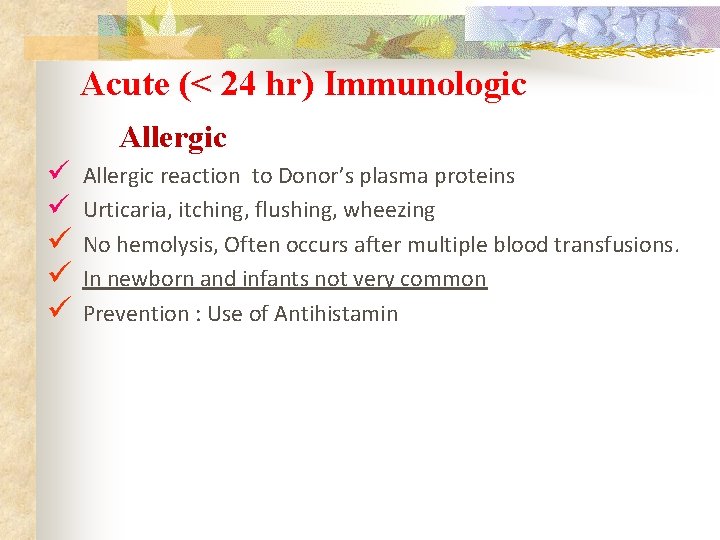
Acute (< 24 hr) Immunologic Allergic reaction to Donor’s plasma proteins Urticaria, itching, flushing, wheezing No hemolysis, Often occurs after multiple blood transfusions. In newborn and infants not very common Prevention : Use of Antihistamin
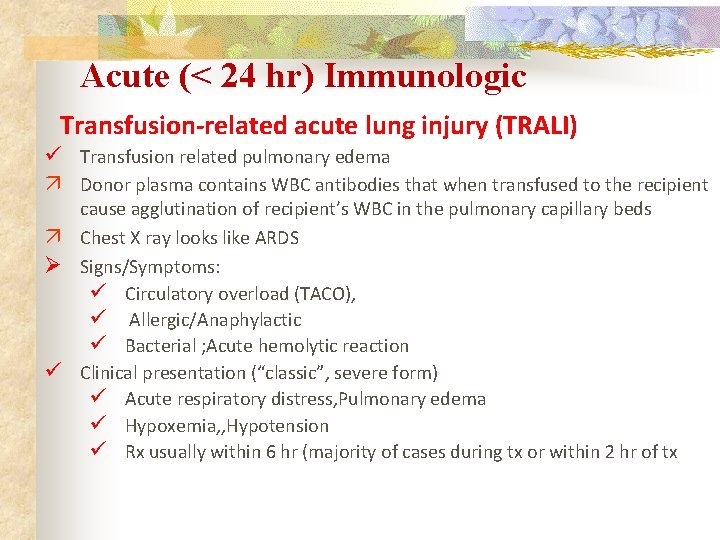
Acute (< 24 hr) Immunologic Transfusion-related acute lung injury (TRALI) Transfusion related pulmonary edema ä Donor plasma contains WBC antibodies that when transfused to the recipient cause agglutination of recipient’s WBC in the pulmonary capillary beds ä Chest X ray looks like ARDS Ø Signs/Symptoms: Circulatory overload (TACO), Allergic/Anaphylactic Bacterial ; Acute hemolytic reaction Clinical presentation (“classic”, severe form) Acute respiratory distress, Pulmonary edema Hypoxemia, , Hypotension Rx usually within 6 hr (majority of cases during tx or within 2 hr of tx
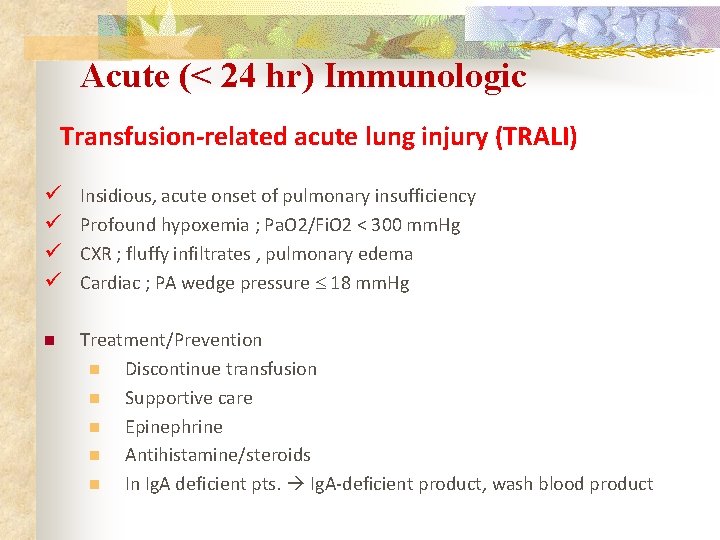
Acute (< 24 hr) Immunologic Transfusion-related acute lung injury (TRALI) Insidious, acute onset of pulmonary insufficiency Profound hypoxemia ; Pa. O 2/Fi. O 2 < 300 mm. Hg CXR ; fluffy infiltrates , pulmonary edema Cardiac ; PA wedge pressure 18 mm. Hg n Treatment/Prevention n Discontinue transfusion n Supportive care n Epinephrine n Antihistamine/steroids n In Ig. A deficient pts. Ig. A-deficient product, wash blood product

Acute Non Immunologic (< 24 hr) Transfusion Reactions
Acute (< 24 hr) Non-Immunologic n n n Circulatory overload Air embolus Hypocalcemia Hypothermia Hyperkalemia
Acute (< 24 hr) Non-Immunologic Circulatory overload Ø Ø Ø Acute pulmonary edema due to volume overload One of the most common complications of transfusion Common in newborn and infants Cardiac and pulmonary compromise Dyspnea, cyanosis, CHF during or soon after transfusion Prevention ; slow rate of transfusion , Care full estimation of volume of transfusion , Ø Treatment ; stop Tx , Use of diuretics
Acute (< 24 hr) Non-Immunologic Air Embolism Air infusion via line of product transfusion Cough, dyspnea, chest pain, shock Prevention ; Care full transfusion via the trained and well experienced Nurse Treatment ; stop Tx , Pt. placed on left side with head down , Displace air bubble from pulmonary valve
Acute (< 24 hr) Non-Immunologic Metabolic Complications ; Hypocalcemia Ø If Large volumes of product transfused rapidly ; plasma citrate Ø Ø levels may rise ; binds i. Ca+2 Citrate rapidly metabolized ; manifestations transient peripheral tingling , paresthesias, , tetanic seizure, hyperventilation, depressed cardiac function Prevention ; Control the calcium level Treatment ; Ca+2 replacement
Acute (< 24 hr) Non-Immunologic Metabolic Complications ; Hyperkalemia Ø If old ( more than 2 weeks ) product transfused ; RBC Lysis may Ø Ø increase potassium level ; Irradiation product may increase the rate of leak Cardiac arrhythmia, electrolyte imbalance Prevention ; Control the potassium level Treatment ; potassium replacement
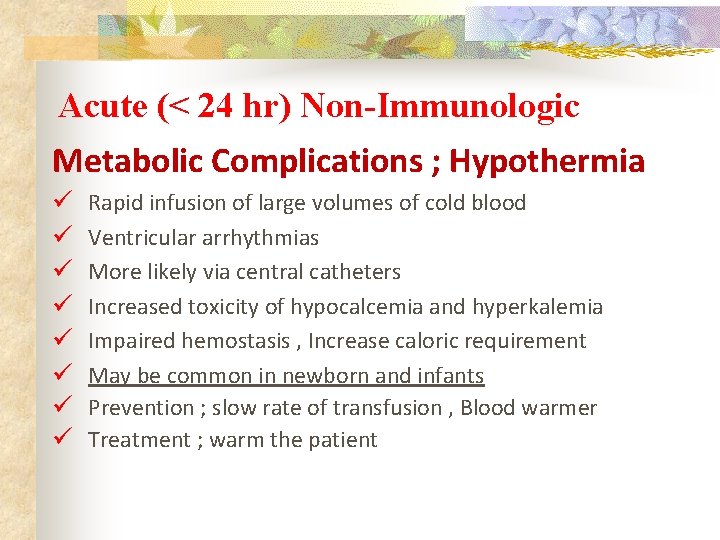
Acute (< 24 hr) Non-Immunologic Metabolic Complications ; Hypothermia Rapid infusion of large volumes of cold blood Ventricular arrhythmias More likely via central catheters Increased toxicity of hypocalcemia and hyperkalemia Impaired hemostasis , Increase caloric requirement May be common in newborn and infants Prevention ; slow rate of transfusion , Blood warmer Treatment ; warm the patient

Delayed Immunologic (> 24 hr) Transfusion Reactions
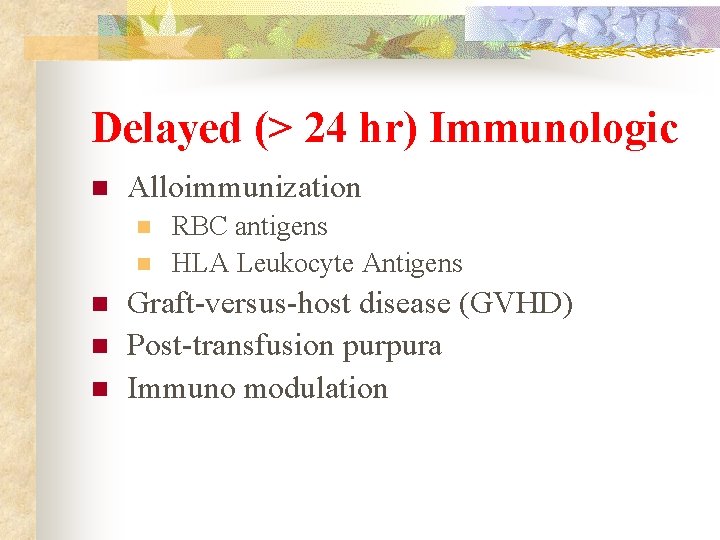
Delayed (> 24 hr) Immunologic n Alloimmunization n n RBC antigens HLA Leukocyte Antigens Graft-versus-host disease (GVHD) Post-transfusion purpura Immuno modulation
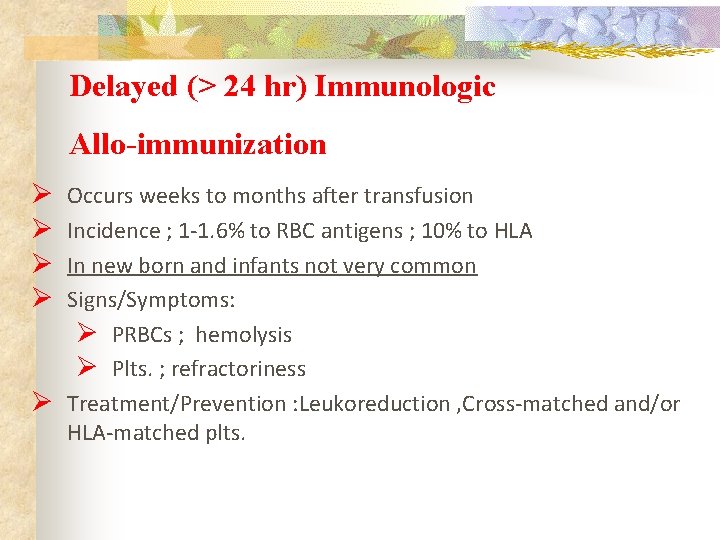
Delayed (> 24 hr) Immunologic Allo-immunization Ø Ø Occurs weeks to months after transfusion Incidence ; 1 -1. 6% to RBC antigens ; 10% to HLA In new born and infants not very common Signs/Symptoms: Ø PRBCs ; hemolysis Ø Plts. ; refractoriness Ø Treatment/Prevention : Leukoreduction , Cross-matched and/or HLA-matched plts.
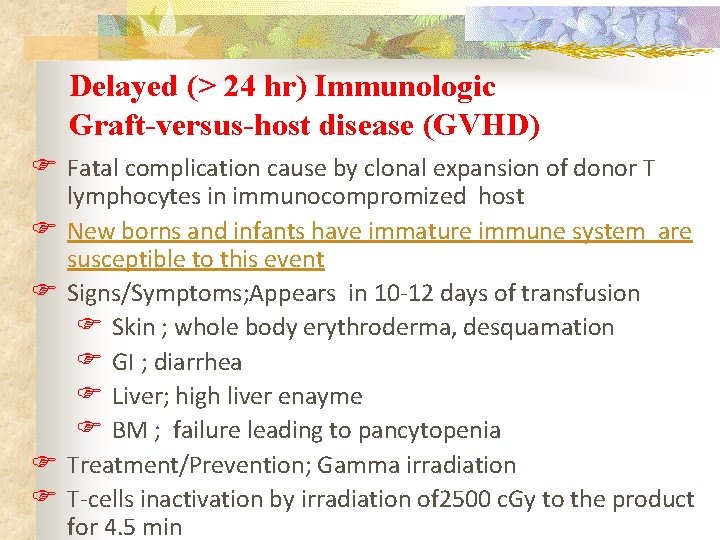
Delayed (> 24 hr) Immunologic Graft-versus-host disease (GVHD) F Fatal complication cause by clonal expansion of donor T F F lymphocytes in immunocompromized host New borns and infants have immature immune system are susceptible to this event Signs/Symptoms; Appears in 10 -12 days of transfusion F Skin ; whole body erythroderma, desquamation F GI ; diarrhea F Liver; high liver enayme F BM ; failure leading to pancytopenia Treatment/Prevention; Gamma irradiation T-cells inactivation by irradiation of 2500 c. Gy to the product for 4. 5 min
Delayed Non Immunologic (> 24 hr) Transfusion Reactions
Delayed (> 24 hr) Non-Immunologic n n Iron overload ( in repeated Tx ) Transfusion Transmitted Infections (TTI)
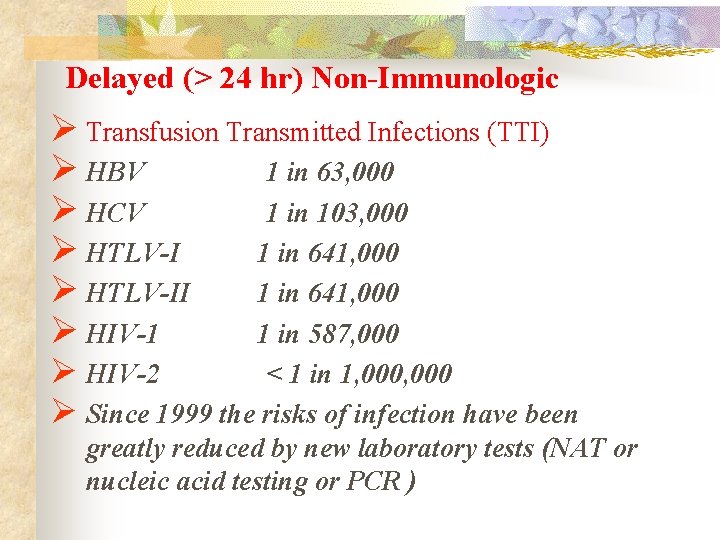
Delayed (> 24 hr) Non-Immunologic Ø Transfusion Transmitted Infections (TTI) Ø HBV 1 in 63, 000 Ø HCV 1 in 103, 000 Ø HTLV-I 1 in 641, 000 Ø HTLV-II 1 in 641, 000 Ø HIV-1 1 in 587, 000 Ø HIV-2 < 1 in 1, 000 Ø Since 1999 the risks of infection have been greatly reduced by new laboratory tests (NAT or nucleic acid testing or PCR )
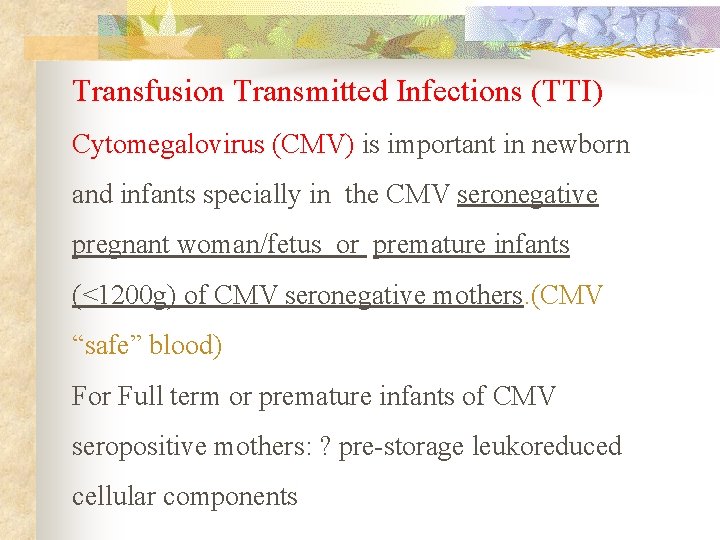
Transfusion Transmitted Infections (TTI) Cytomegalovirus (CMV) is important in newborn and infants specially in the CMV seronegative pregnant woman/fetus or premature infants (<1200 g) of CMV seronegative mothers. (CMV “safe” blood) For Full term or premature infants of CMV seropositive mothers: ? pre-storage leukoreduced cellular components
Conclusion of Tx Rx in new born and infants n n n n Small Blood volume Passive transfer of maternal antibody Immature Immune system CMV , TA-GVHD Risk of metabolic Complication Ca, K , Glucose , Hypothermia Cross match with maternal Serum Use of repeated donors CMV neg products , Irradiated product
- Slides: 29