Blood transfusion Indications Selection of Donor criteria Cross
Blood transfusion, Indications, Selection of Donor criteria, Cross matching, Untoward Reactions, Transmissible Infections Dr Rohini Shewale
Transfusion Biology • Blood transfusion is transfusion of whole blood or components from one person to another person. • Involves two processes -Collection of blood from donor -Administration of blood to recipient
Definitions Ø WHOLE BLOOD = Unseparated blood collected into an approved container containing an anticoagulant preservative solution. Ø BLOOD PRODUCT = Any therapeutic substance prepared from human blood. Ø BLOOD COMPONENT = 1. A constituent of blood , separated from whole blood such as q Red cell concentrate q Plasma q Platelet concentrates 2. Plasma or platelets collected by apheresis 3. Cryoprecipitate prepared from fresh frozen plasma
ØCancer patients ØWomen during child birth and pregnancy

Steps • Selection of Donor as per criteria Blood collection by phlebotomy Storage of blood Donor testing for ABO and Rh grouping Testing for infectious organisms(TTD) Blood Grouping of recipient Compatibility testing Supervised Blood Transfusion
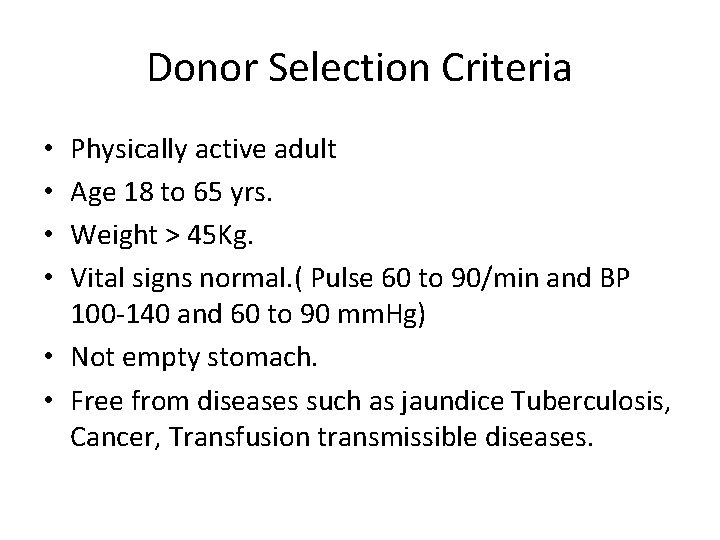
Donor Selection Criteria Physically active adult Age 18 to 65 yrs. Weight > 45 Kg. Vital signs normal. ( Pulse 60 to 90/min and BP 100 -140 and 60 to 90 mm. Hg) • Not empty stomach. • Free from diseases such as jaundice Tuberculosis, Cancer, Transfusion transmissible diseases. • •
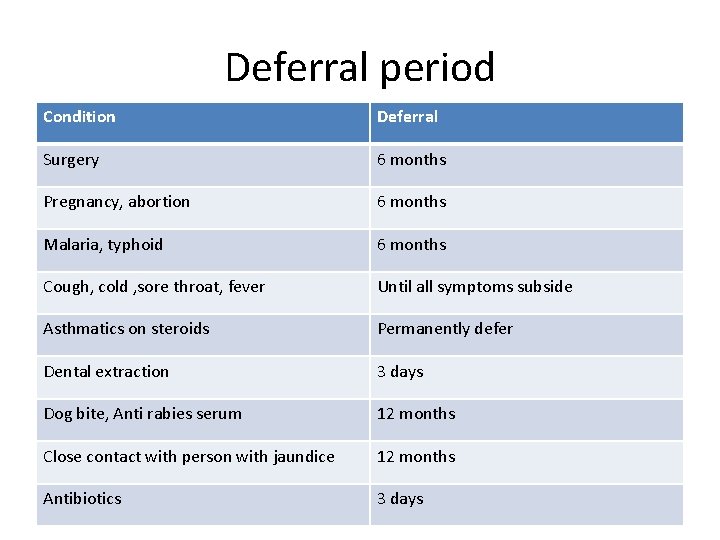
Deferral period Condition Deferral Surgery 6 months Pregnancy, abortion 6 months Malaria, typhoid 6 months Cough, cold , sore throat, fever Until all symptoms subside Asthmatics on steroids Permanently defer Dental extraction 3 days Dog bite, Anti rabies serum 12 months Close contact with person with jaundice 12 months Antibiotics 3 days
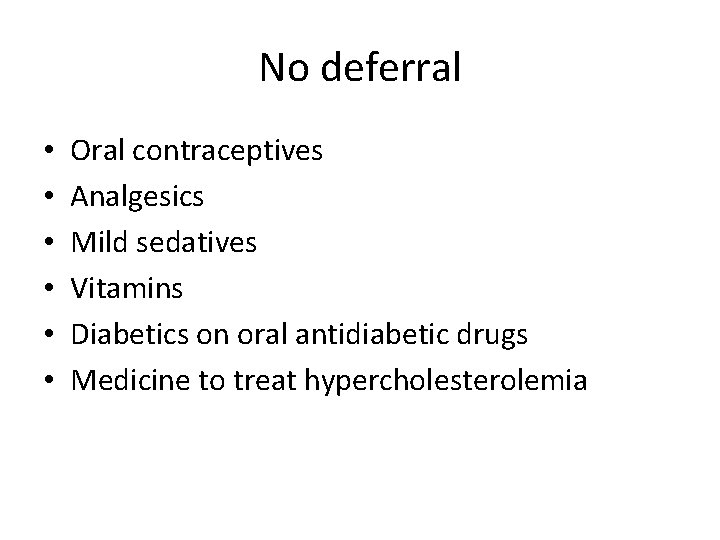
No deferral • • • Oral contraceptives Analgesics Mild sedatives Vitamins Diabetics on oral antidiabetic drugs Medicine to treat hypercholesterolemia

Blood collection by Phlebotomy Types of blood collection bags Single –Whole blood Double –Packed red cells + Plasma Triple - Packed red cells + Plasma + Platelets Quadraple - Packed red cells + plasma + Platelet + Buffy coat • Volume • 350 ml / 450 ml • • •
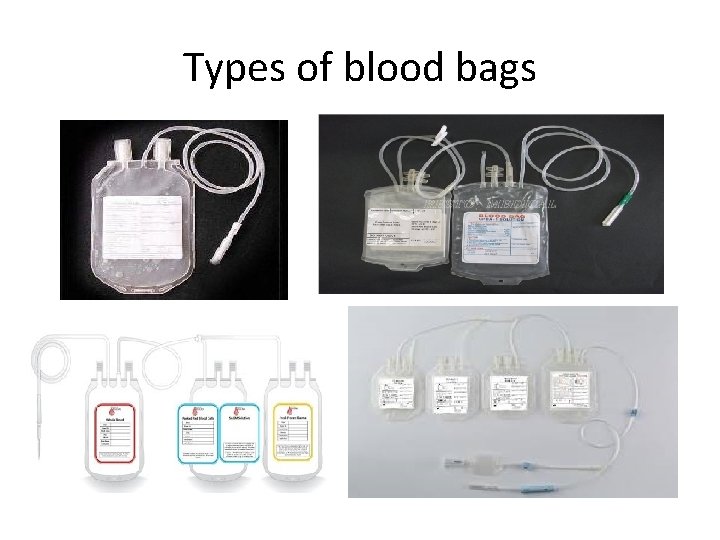
Types of blood bags
Phlebotomy(Blood collection from a donor)
Post donation care • Avoid strenuous exercise/ heavy weight lifting for that day. • Avoid direct exposure to sunlight. • Avoid driving immediately. • Avoid alcohol consumption before next meal. • Take plenty of fluids on that day. • Apply ice if pain or swelling at phlebotomy site.
Anticoagulants • ACD (Acid Citrate Dextrose) -21 days • CPD( Citrate Dhosphate Dextose) -21 days • CPDA( Citrate Phosphate Dextrose Adenine)135 days • SAGM( Saline Adenine Glucose Mannitol) – 42 day)
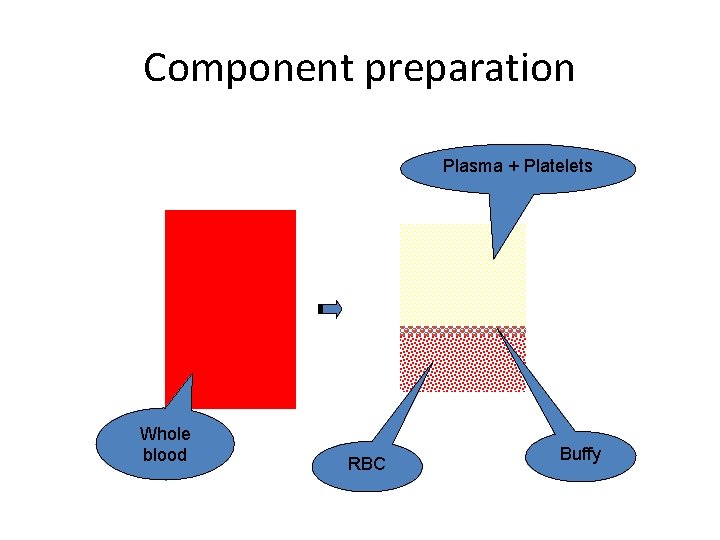
Component preparation Plasma + Platelets Whole blood RBC Buffy
Component separation • 1 st spin – Low speed centrifugation – Packed red blood cells and Platelet rich plasma • 2 nd spin – High speed centrifugation – Random donor platelet and Plasma
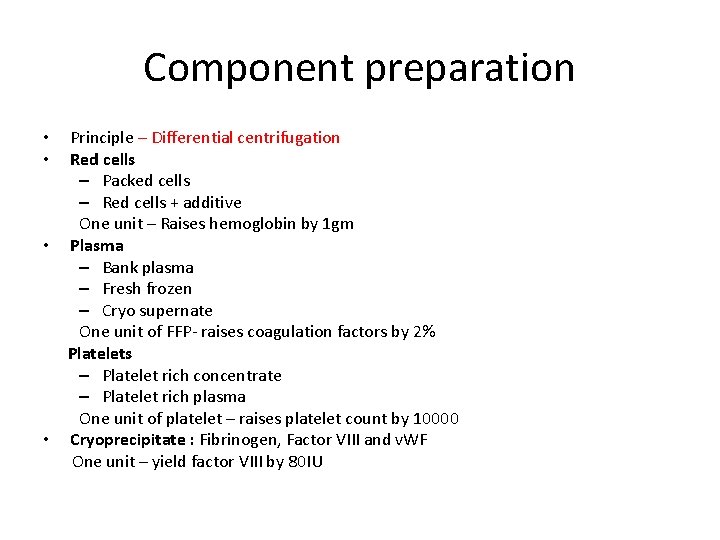
Component preparation Principle – Differential centrifugation Red cells – Packed cells – Red cells + additive One unit – Raises hemoglobin by 1 gm • Plasma – Bank plasma – Fresh frozen – Cryo supernate One unit of FFP- raises coagulation factors by 2% Platelets – Platelet rich concentrate – Platelet rich plasma One unit of platelet – raises platelet count by 10000 • Cryoprecipitate : Fibrinogen, Factor VIII and v. WF One unit – yield factor VIII by 80 IU • •

Storage of Blood/ Blood Components Storage temperature Validity Whole blood 2 to 6 ˚ C 35 /42 days Packed red cells 2 to 6 ˚ C 35 /42 days Fresh Frozen Plasma -30 to -80 ˚ C 1 year Platelet concentrates 20 to 24 ˚ C 5 days Cryoprecipitate -30 to -80 ˚ C 1 year

Blood storage cabinet Plasma freezer Platelet incubator with agitator

Storage room in blood bank

Apheresis • Apheresis – Greek word means to separate or remove. • In apheresis, blood is withdrawn from donor – mixed with anticoagulant – components separated – one or more products retained remaining blood returned to donor.
Administration of blood to recipient • Request from physician • Blood grouping of patient/ recipient • Compatibility testing of patient’s sample with donor unit • Issue / supply of compatible unit
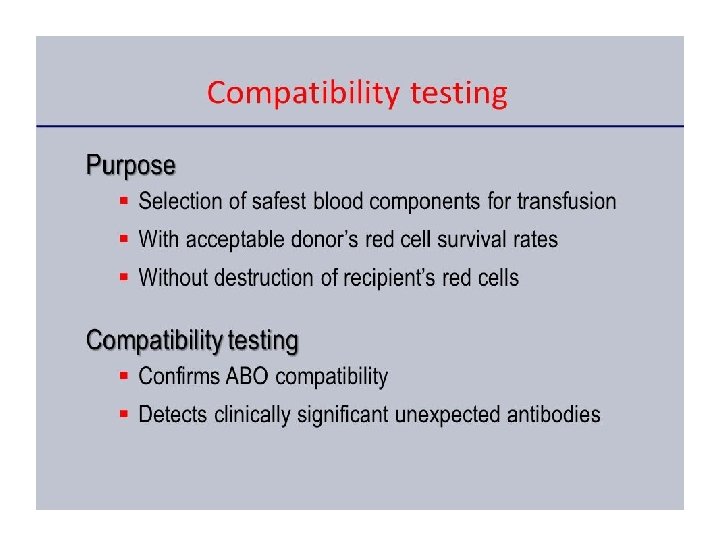
Compatibility testing • Cross matching • Two methods • 1. Major cross matching - Donor cells and recipient’s serum • 2. Minor cross matching – Donor serum and recipient’s cells

Methods of cross matching • 1. Tube technique • 2. Gel technology

Transfusion Reaction /Adverse Effects of Transfusion Ø Transfusion reaction Ø Untoward event Ø Varies from mild to life threatening Ø Majority of transfusion reactions are uneventful Ø 10% of transfusion recipients may suffer from untoward effects
Types of Transfusion Reactions Ø Immune reactions Ø Non immune reactions Ø Immediate During or within few hours of transfusion Ø Delayed Days or weeks after the transfusion
Immune Reactions Ø Haemolytic Transfusion Reactions Ø Acute Ø Delayed Ø Ø Ø Ø Febrile Non Haemolytic Transfusion Reactions Allergic / Anaphylactic reactions Allo-immunization TRALI (Transfusion Related Acute Lung Injury) TA-Gv. HD (Transfusion associated Graft vs Host Disease) PTP (Post Transfusion Purpura) Immunomodulation
Immune Transfusion Reactions Due to : Ø Patient Abs against donor Antigen or vice versa Ø Red cells Ø White cells Ø Platelets Ø Reaction to plasma proteins
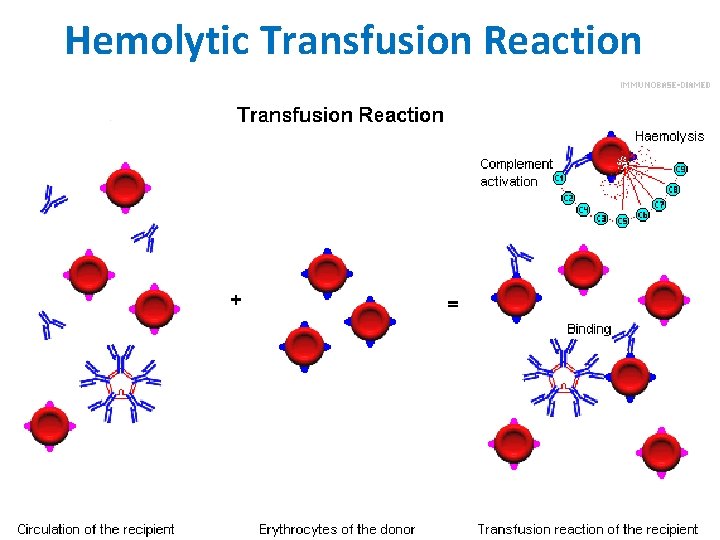
Hemolytic Transfusion Reaction
Haemolytic Transfusion Reactions Ø Increased destruction of donor red cells Ø Red cell incompatibility – ABO incompatibility Ø Accidental heating or freezing of RBC Ø Red cells in contact with water or 5% Dextrose Ø Bacterial contamination Ø Administering red cells through small gauge needle
ABO incompatible Transfusion Reactions Ø Mainly due to misidentification of the patient Ø Most occur in emergencies, in ICU, OTs Ø In unconscious & anesthetized patients ØClerical errors – commonest cause Ø Misidentification of pt / recipient Ø Wrong samples / blood packs ØTechnical errors Ø In Grouping of pt. / donor blood Ø In cross matching
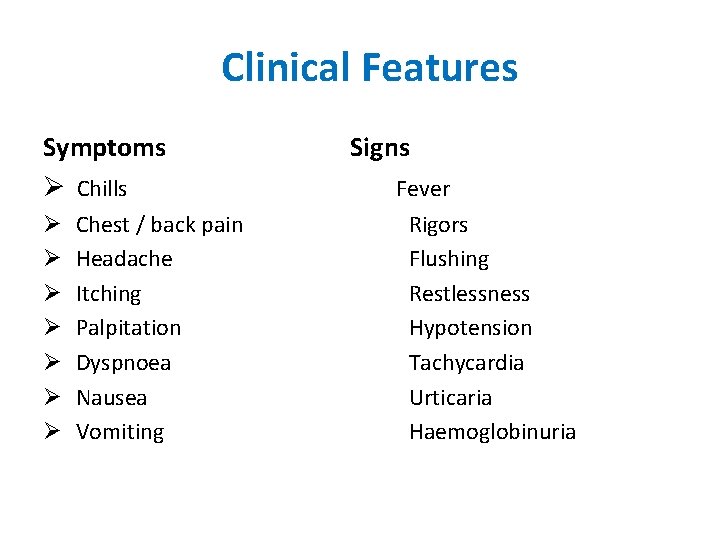
Clinical Features Symptoms Ø Chills Ø Ø Ø Ø Chest / back pain Headache Itching Palpitation Dyspnoea Nausea Vomiting Signs Fever Rigors Flushing Restlessness Hypotension Tachycardia Urticaria Haemoglobinuria
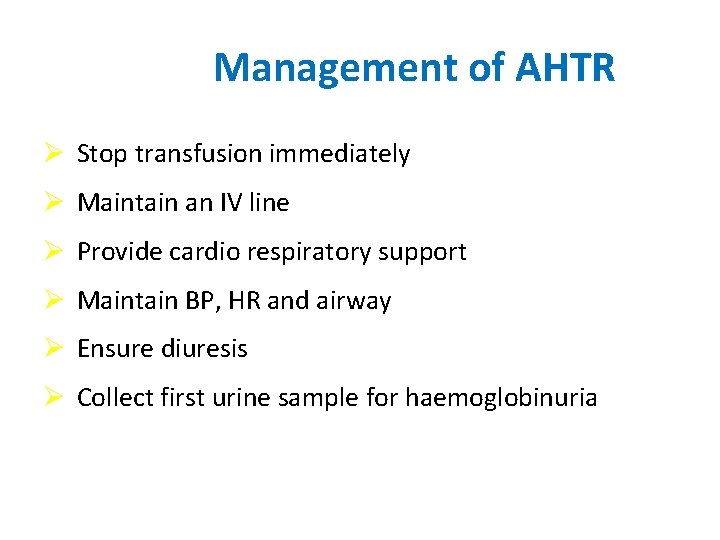
Management of AHTR Ø Stop transfusion immediately Ø Maintain an IV line Ø Provide cardio respiratory support Ø Maintain BP, HR and airway Ø Ensure diuresis Ø Collect first urine sample for haemoglobinuria
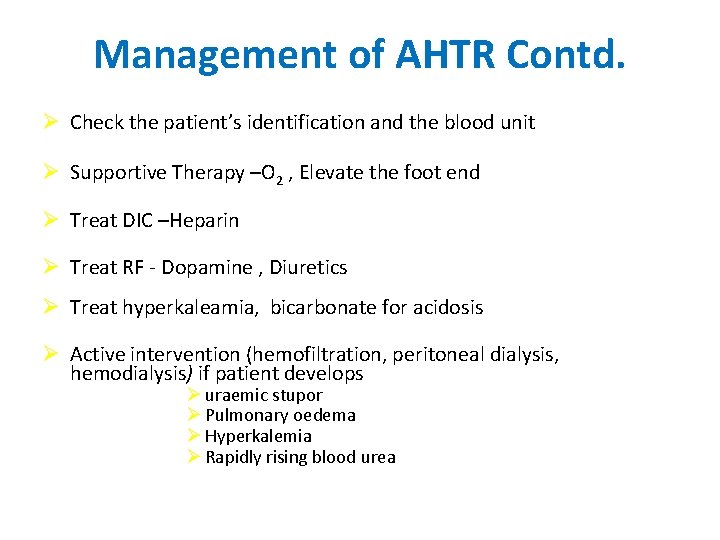
Management of AHTR Contd. Ø Check the patient’s identification and the blood unit Ø Supportive Therapy –O 2 , Elevate the foot end Ø Treat DIC –Heparin Ø Treat RF - Dopamine , Diuretics Ø Treat hyperkaleamia, bicarbonate for acidosis Ø Active intervention (hemofiltration, peritoneal dialysis, hemodialysis) if patient develops Ø uraemic stupor Ø Pulmonary oedema Ø Hyperkalemia Ø Rapidly rising blood urea
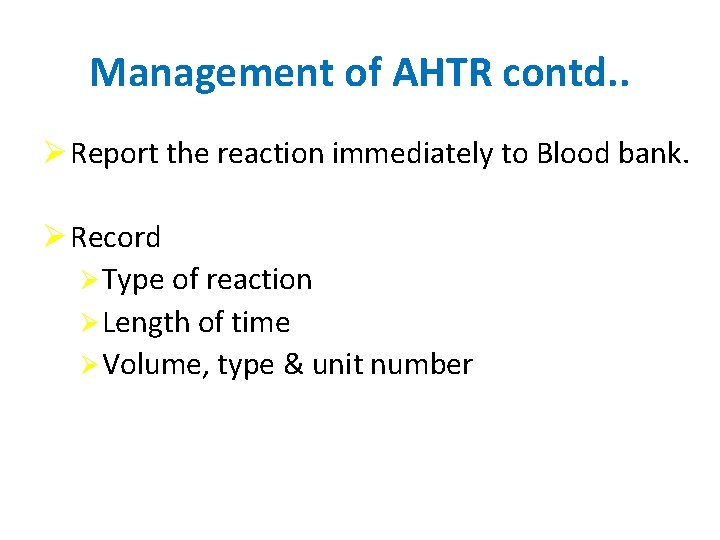
Management of AHTR contd. . Ø Report the reaction immediately to Blood bank. Ø Record Ø Type of reaction Ø Length of time Ø Volume, type & unit number
MANAGEMENT Ø Send post transfusion blood sample of patient & remaining blood unit with filled reaction form to the Blood Bank. Ø Blood sample-10 ml in plain bulb and 2 ml in EDTA bulb For DCT, Sr. urea and creatinine, Bilirubin Ø And first voided urine sample for Hb , Mb
Delayed Hemolytic Transfusion Reaction Ø Days or weeks after the blood transfusion Ø Due to secondary immune response Ø Rh or minor blood group Abs Ø Extra vascular haemolysis

Clinical Features of DHTR Ø Gradual red cell destruction Ø Occurs 5 -10 days after transfusion Ø Jaundice appear 5 -7 days after transfusion Ø Fall in Hb level Ø Prevention – Ø Screening for allo Abs Ø Selection of appropriate red cells –saline washed cells/leucoreduced red cells
Allergic / Anaphylactic Reactions Ø Mainly due to plasma proteins Ø Severity is variable Ø Mild – urticaria Ø Severe – anaphylactoid Ø Due to Ig. A deficiency Ø Occurs within minutes of commencing transfusion Ø Common in pts with repeated plasma component therapy
Non immune transfusion reactions Ø Circulatory overload Ø Heart failure, pulm. oedema Ø Iron overload Ø Iron deposit in tissues Ø Chelation - Desperrioxamine Ø Hyperkalaemia Ø Haemolysed blood Ø TTI (Transfusion Transmissible Infections) Ø Septicemia
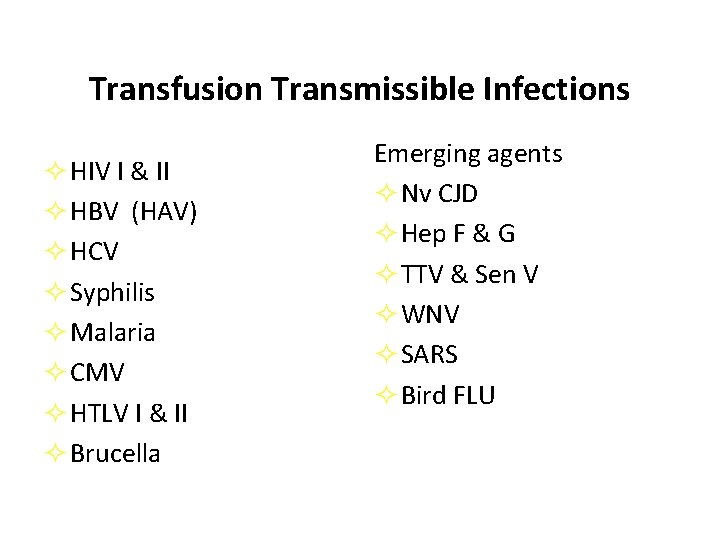
Transfusion Transmissible Infections ² HIV I & II ² HBV (HAV) ² HCV ² Syphilis ² Malaria ² CMV ² HTLV I & II ² Brucella Emerging agents ² Nv CJD ² Hep F & G ² TTV & Sen V ² WNV ² SARS ² Bird FLU
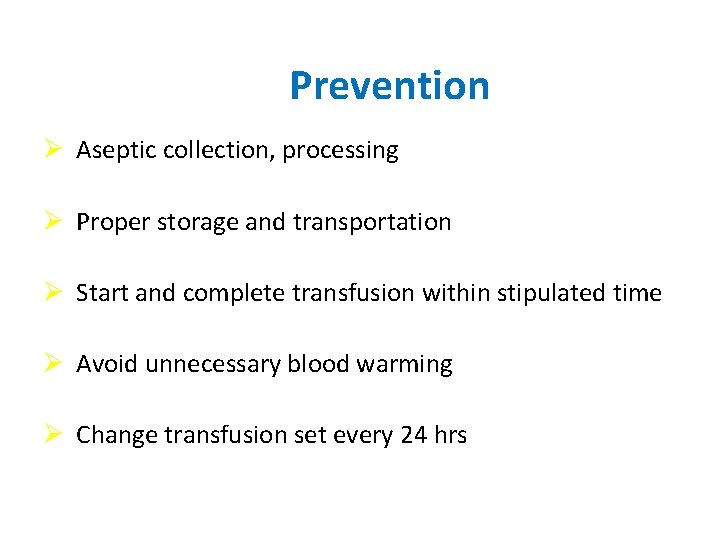
Prevention Ø Aseptic collection, processing Ø Proper storage and transportation Ø Start and complete transfusion within stipulated time Ø Avoid unnecessary blood warming Ø Change transfusion set every 24 hrs
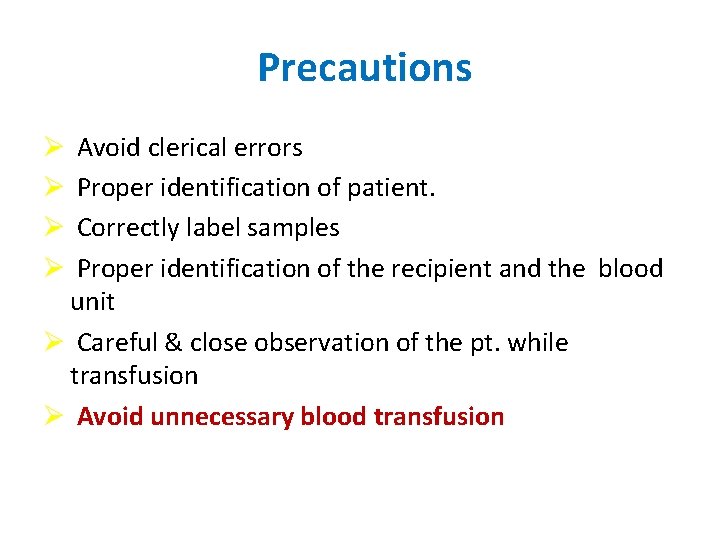
Precautions Avoid clerical errors Proper identification of patient. Correctly label samples Proper identification of the recipient and the blood unit Ø Careful & close observation of the pt. while transfusion Ø Avoid unnecessary blood transfusion Ø Ø
• THANK YOU
- Slides: 45