Blood sample collection in children Dos and Donts
Blood sample collection in children Do’s and Don'ts Dr Swati Bhave
Preparation of Pediatric Patients • Find out – Is it the first time for the child? Find out about past experience. How did the child react ? How did the parents react ? • Explain – To parent and child about procedure (if possible with dolls or puppets) Explain need of second attempt if required
Parental co-operation • Assess - Parental ability to participate or assist you • Decide - Whether parent should be present or not • If present - Decide how will they assist : physical restrain, distraction, emotional support , explanation
How to relieve Anxiety & Fear • Collect blood away from other patients in a special room. Never in the hospital bed. This is a comfort zone • Area should be child friendly. Uniforms should be colourful • Keep equipment out of site • Ask child’s preference of hand • Allow child to select comfort object • Stop procedure if child combative • Try later or another person

Minimizing PAIN • • Topical anesthetic like AMETOP, EMLA Cost, time ( 10 -60 min) More than one site tried, allergy Sucrose or pacifier
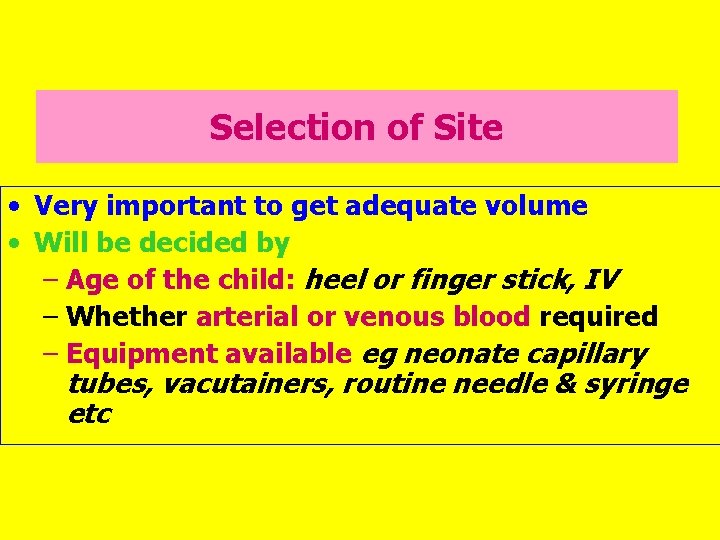
Selection of Site • Very important to get adequate volume • Will be decided by – Age of the child: heel or finger stick, IV – Whether arterial or venous blood required – Equipment available eg neonate capillary tubes, vacutainers, routine needle & syringe etc
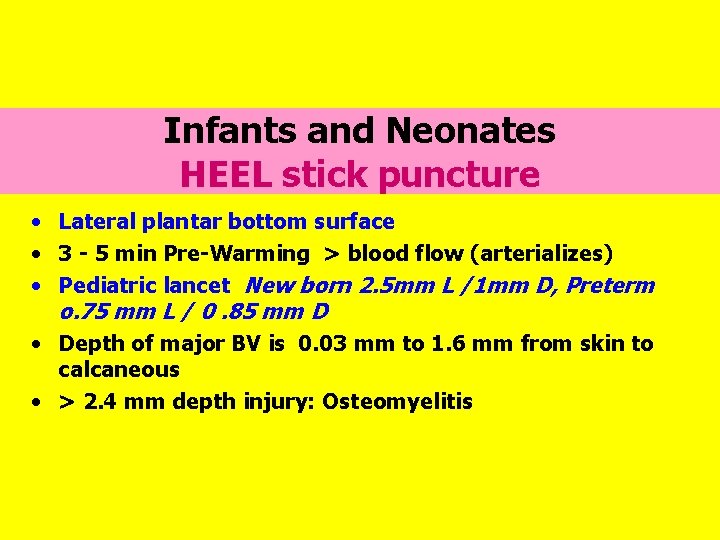
Infants and Neonates HEEL stick puncture • Lateral plantar bottom surface • 3 - 5 min Pre-Warming > blood flow (arterializes) • Pediatric lancet New born 2. 5 mm L /1 mm D, Preterm o. 75 mm L / 0. 85 mm D • Depth of major BV is 0. 03 mm to 1. 6 mm from skin to calcaneous • > 2. 4 mm depth injury: Osteomyelitis

Infants and Neonates HEEL stick puncture • Do not use anteromedial area or posterior curve of C • Do not use alcohol swabs to stop bleeding : stinging; Use sterile gauze for pressure • Do not use adhesive tapes : maceration and bruising of skin • Do not squeeze or milk excessively : hemolysis or dilutes blood with tissue and interstitial fluid : erroneous results • Discard first drop • Complications cellulitis, abscess, scarring, tissue loss, calcified nodules
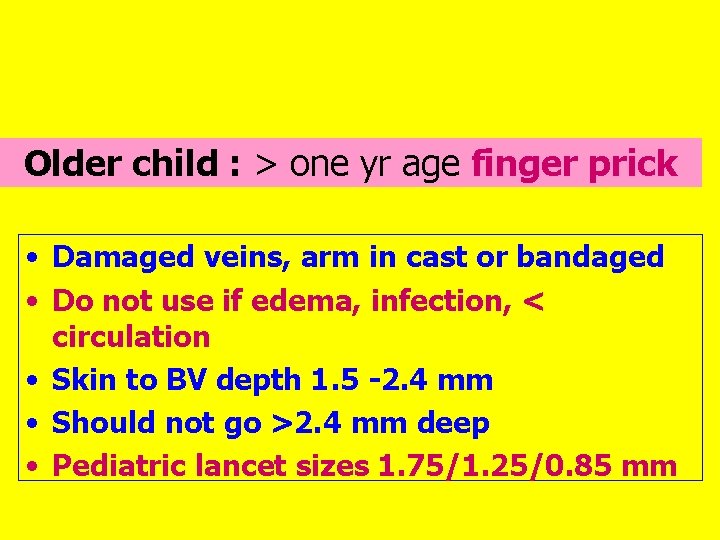
Older child : > one yr age finger prick • Damaged veins, arm in cast or bandaged • Do not use if edema, infection, < circulation • Skin to BV depth 1. 5 -2. 4 mm • Should not go >2. 4 mm deep • Pediatric lancet sizes 1. 75/1. 25/0. 85 mm

Intravenous blood collection • Site selection • Tourniquet not excessively tight • Special precautions when – Heparin lock or – IV line collection

What is required from the sample • Does the test require : whole blood , serum or plasma. • How much is the volume required : 2, 4, 5, ml etc. Pre-term 10 ml may be 5 % of total volume • What are the special bulbs or ready made tubes required : e. g. fluoride bulb for sugar, chemistry bulb for urea , EDTA for hematology etc
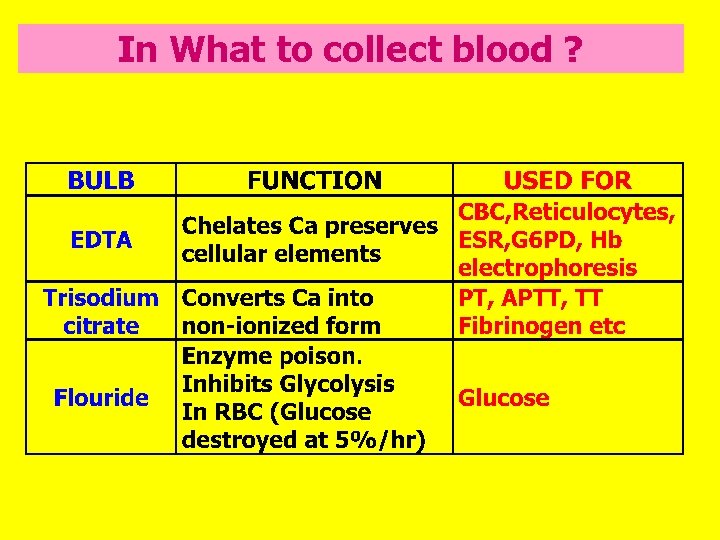
In What to collect blood ?
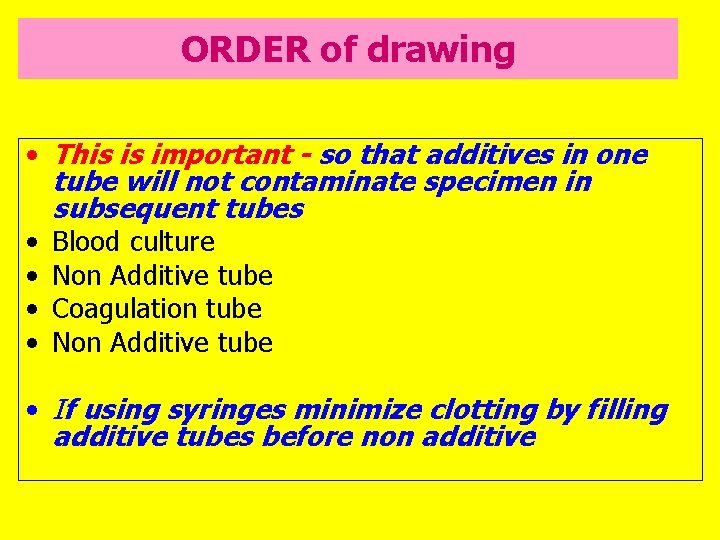
ORDER of drawing • This is important - so that additives in one tube will not contaminate specimen in subsequent tubes • Blood culture • Non Additive tube • Coagulation tube • Non Additive tube • If using syringes minimize clotting by filling additive tubes before non additive
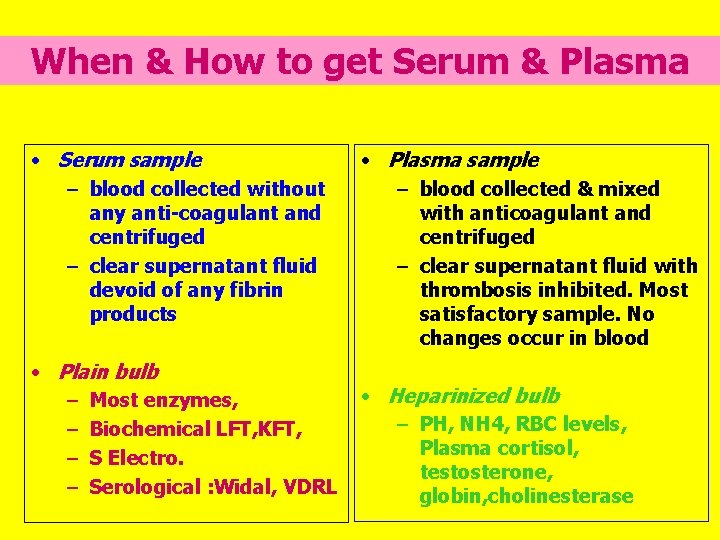
When & How to get Serum & Plasma • Serum sample – blood collected without any anti-coagulant and centrifuged – clear supernatant fluid devoid of any fibrin products • Plain bulb – Most enzymes, – Biochemical LFT, KFT, – S Electro. – Serological : Widal, VDRL • Plasma sample – blood collected & mixed with anticoagulant and centrifuged – clear supernatant fluid with thrombosis inhibited. Most satisfactory sample. No changes occur in blood • Heparinized bulb – PH, NH 4, RBC levels, Plasma cortisol, testosterone, globin, cholinesterase
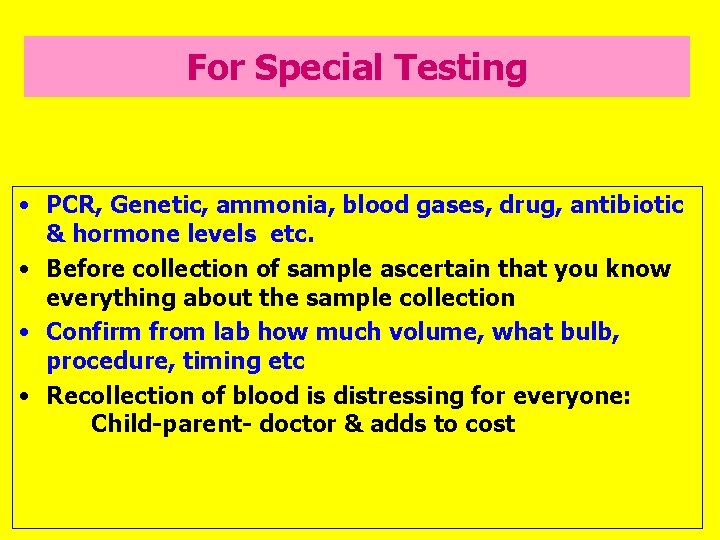
For Special Testing • PCR, Genetic, ammonia, blood gases, drug, antibiotic & hormone levels etc. • Before collection of sample ascertain that you know everything about the sample collection • Confirm from lab how much volume, what bulb, procedure, timing etc • Recollection of blood is distressing for everyone: Child-parent- doctor & adds to cost
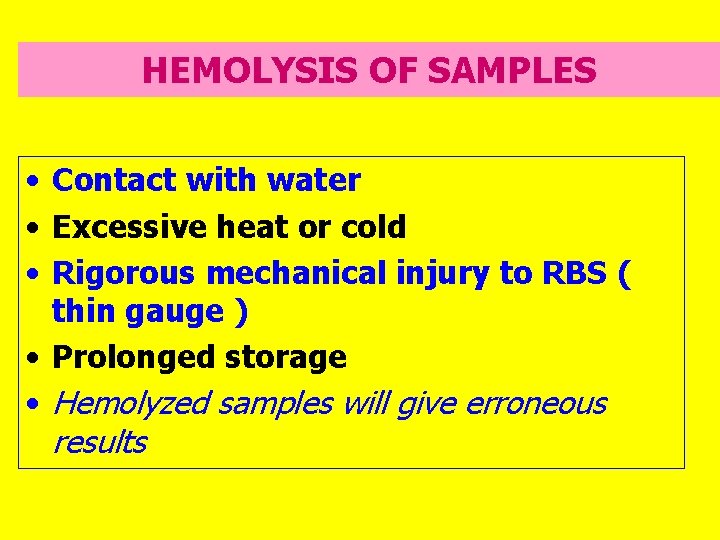
HEMOLYSIS OF SAMPLES • Contact with water • Excessive heat or cold • Rigorous mechanical injury to RBS ( thin gauge ) • Prolonged storage • Hemolyzed samples will give erroneous results
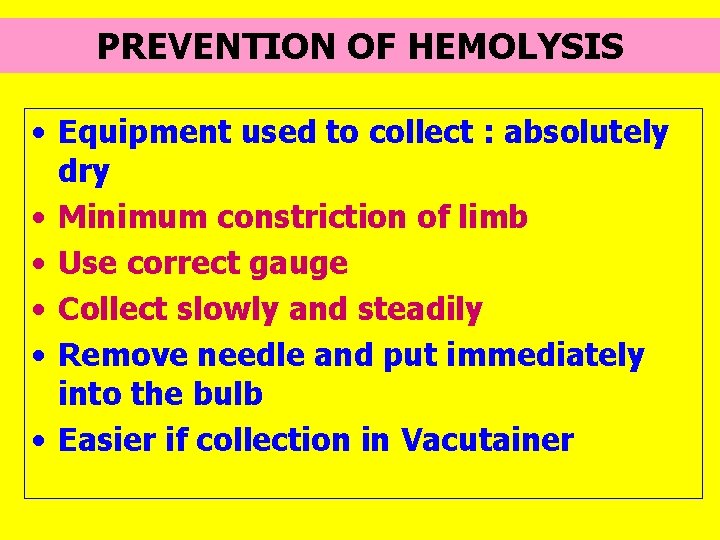
PREVENTION OF HEMOLYSIS • Equipment used to collect : absolutely dry • Minimum constriction of limb • Use correct gauge • Collect slowly and steadily • Remove needle and put immediately into the bulb • Easier if collection in Vacutainer
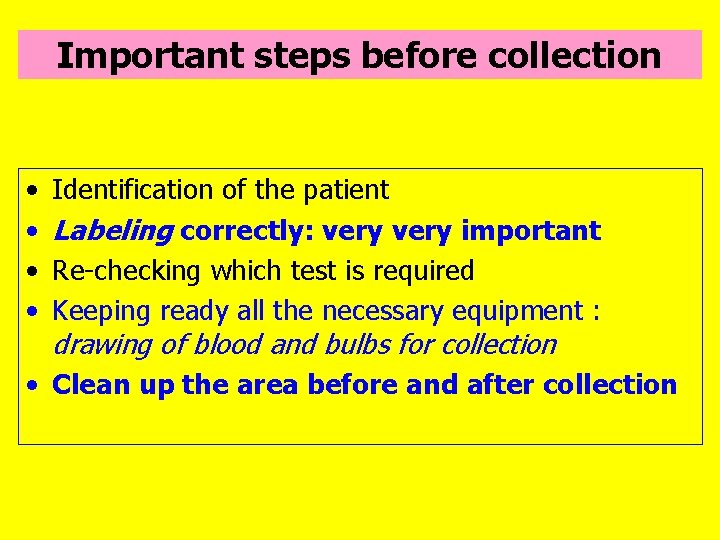
Important steps before collection • • Identification of the patient Labeling correctly: very important Re-checking which test is required Keeping ready all the necessary equipment : drawing of blood and bulbs for collection • Clean up the area before and after collection
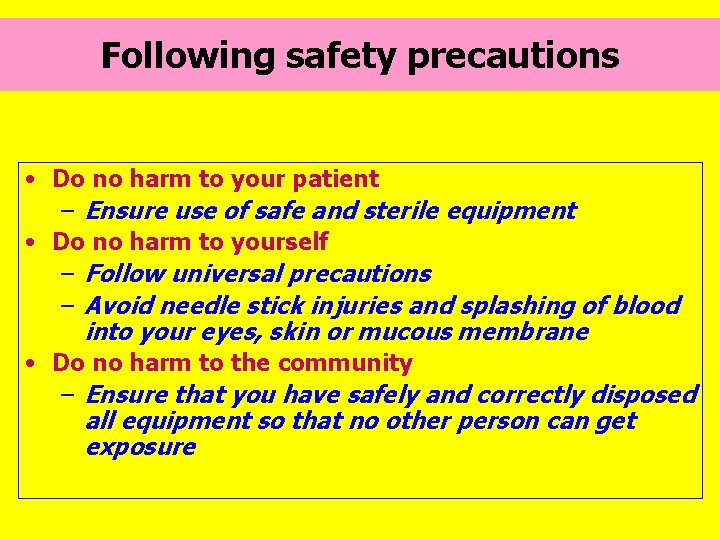
Following safety precautions • Do no harm to your patient – Ensure use of safe and sterile equipment • Do no harm to yourself – Follow universal precautions – Avoid needle stick injuries and splashing of blood into your eyes, skin or mucous membrane • Do no harm to the community – Ensure that you have safely and correctly disposed all equipment so that no other person can get exposure
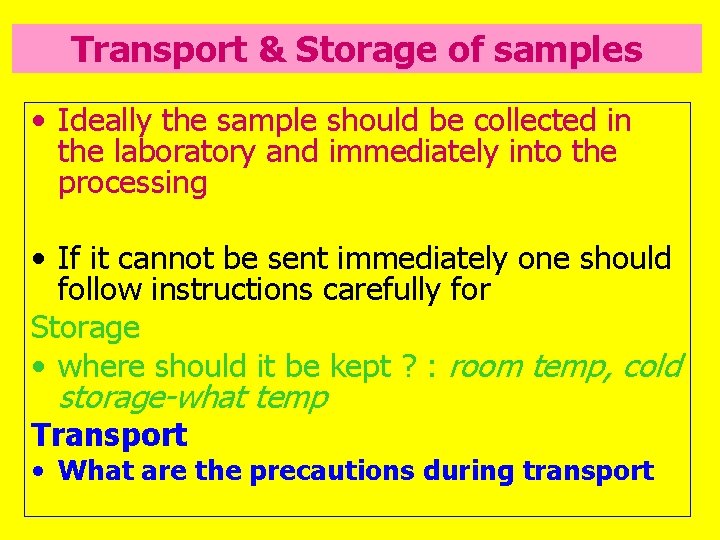
Transport & Storage of samples • Ideally the sample should be collected in the laboratory and immediately into the processing • If it cannot be sent immediately one should follow instructions carefully for Storage • where should it be kept ? : room temp, cold storage-what temp Transport • What are the precautions during transport
Summary • Blood collection in children is a traumatic and invasive procedure • All efforts should be made to reduce the discomfort • Care should be taken to avoid need for repeat puncture
- Slides: 21